Abstract
Background:
Prolonged hospitalization in the intensive care unit (ICU) can impose long-term psychological effects on patients. One of the most significant psychological effects from prolonged hospitalization is delirium.
Objectives:
The aim of this study was to assess the effect of prolonged hospitalization of patients and subsequent delirium in the intensive care unit.
Patients and Methods:
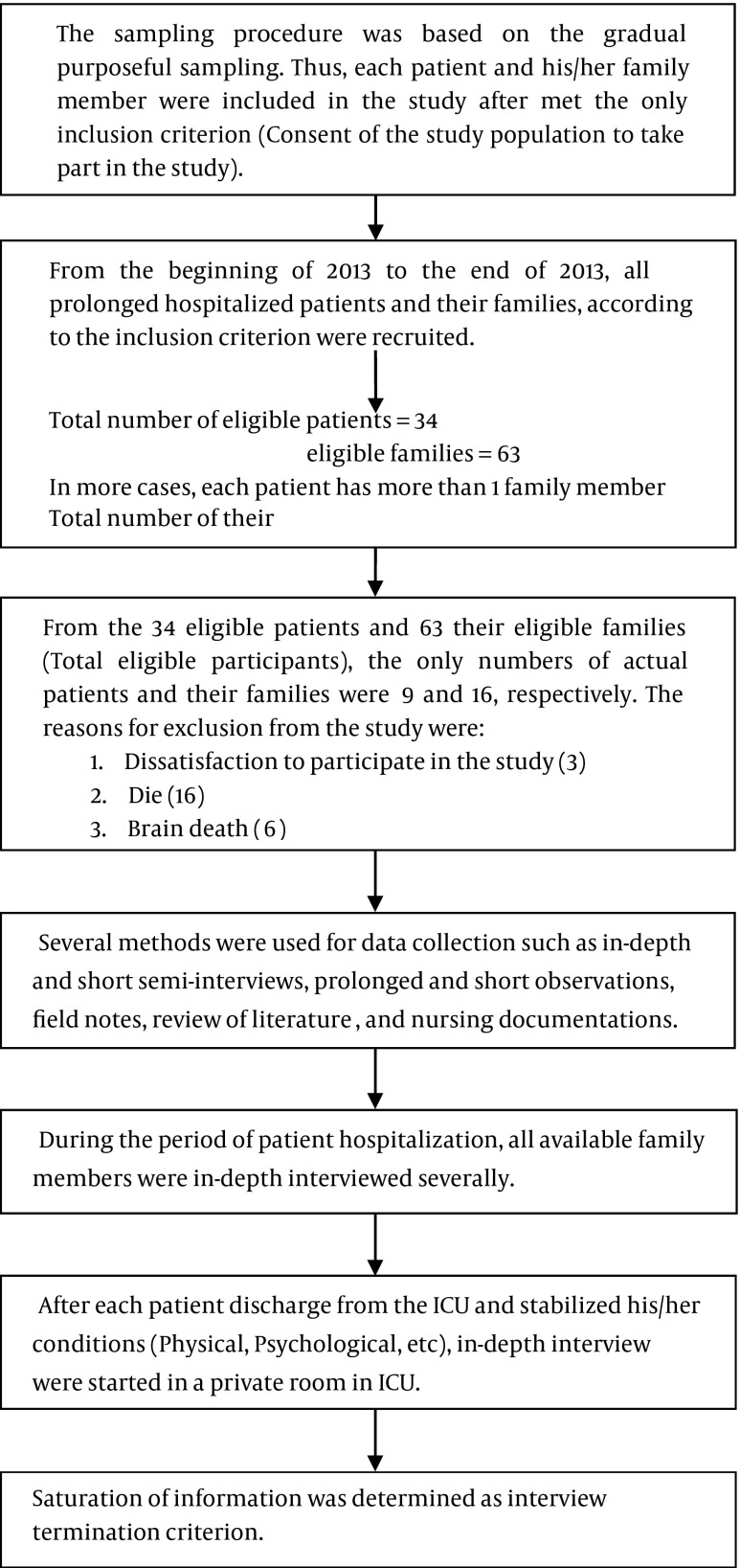
This conventional content analysis study was conducted in the General Intensive Care Unit of the Shariati Hospital of Tehran University of Medical Sciences, from the beginning of 2013 to 2014. All prolonged hospitalized patients and their families were eligible participants. From the 34 eligible patients and 63 family members, the final numbers of actual patients and family members were 9 and 16, respectively. Several semi-structured interviews were conducted face-to-face with patients and their families in a private room and data were gathered.
Results:
Two main themes from two different perspectives emerged, 'patients' perspectives' (experiences during ICU hospitalization) and 'family members' perspectives' (supportive-communicational experiences). The main results of this study focused on delirium, Patients' findings were described as pleasant and unpleasant, factual and delusional experiences.
Conclusions:
Family members are valuable components in the therapeutic process of delirium. Effective use of family members in the delirium caring process can be considered to be one of the key non-medical nursing components in the therapeutic process.
Keywords: Delirium, Intensive Care Units, Iran
1. Background
Prolonged hospitalization in an intensive care unit (ICU) can have long-term psychological effects on patients (1). One of the most significant psychological effects resulting from prolonged hospitalization is delirium. Delirium is a common and frequently underestimated syndrome characterized by acute fluctuations in the patient's mental status which is comprised of: confusion, inattention, and disorganized thinking (2-8). The incidence of delirium in ICU patients ranges from 16% to 92%, and patients diagnosed with delirium are at increased risk from adverse inpatient events such as: falls, inadvertent removal of lines and catheters, pneumonia, pressure ulcers, and adverse drug reactions associated with the treatment of agitation or insomnia (9-11). Overall, delirium contributes to higher mortality and morbidity rates, prolonged stay in the ICU and hospital, increased health care costs, increased need for nursing home care after discharge (12-16), and increased risk of cognitive impairment (17, 18).
Delirium has a long lasting impact on patients. Not only does it acutely traumatize the patient through frightening experiences, it also contributes to higher incidences of posttraumatic stress disorder (PTSD), anxiety, and depression after ICU discharge (17). Studies evaluating delirium risk factors in ICU patients are limited (19-21). Risk factors for delirium have been categorized into predisposing and precipitating factors. Predisposing factors are present prior to a patient's admission to the ICU, while precipitating factors take place during the course of hospitalization. Precipitating factors are further classified into those directly connected to the critical illness, and those connected to therapeutic interventions.
Three sub-types of delirium have been described namely; hyperactive, hypoactive and mixed. Hyperactive delirium is defined by agitation, restlessness and attempts to remove invasive medical devices. Hypoactive delirium is described by withdrawal, flat affect, apathy, lethargy and decreased responsiveness. Mixed delirium is a fluctuation of the patient’s symptoms between hyperactive and hypoactive states (22, 23).
2. Objectives
The aim of this study was to assess delirium in patient with prolonged hospitalization in the ICU and its effect on them and their families.
3. Patients and Methods
3.1. Study Design
A conventional content analysis approach was utilized for data gathering and analysis. This approach authorized the researcher to describe and explain the data and to develop the dominant and major themes of the participant's experience. The qualitative content analysis used in the present study is based on methods described by Graneheim and Lundman, which are described in the following steps (24): 1. Transcription of the interviews was carried out and the transcribed texts were read several times; 2. Important texts were divided into meaning units, then these meaning units were categorized as condensed units; 3. Condensed units were categorized as subcategories; 4. According to the similarities and differences, the subcategories were divided into categories; 5. Final categories were themes developed according to their similarities and differences and formulated as an expression of the latent content of the text.
3.2. Ethical Considerations
The study was approved by the Baqiyatallah University of Medical Sciences, Nursing Faculty and Sina Trauma Research Center of Tehran University of Medical Sciences (TUMS), Tehran, Iran. The ethical considerations were related to the participants’ autonomy, confidentiality, and anonymity, during the study period and its publication. The participants were informed of the aim, the design of the study, and the voluntary nature of their participation. Moreover, tape recording permission and informed consent were attained from each participant who agreed to be included in the study.
3.3. Participants and Setting
The study was conducted in the General Intensive Care Unit (GICU) of TUMS, Tehran, Iran, from the beginning of 2013 to 2014. The ICU ward had 12 active beds with an average of 5-8 bed turnovers each week. Patients' hospitalization is normally three to ten days, however, in some situations hospitalization is prolonged. Routinely, for PHPs (prolonged hospitalized patients), the criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) and CAM (Confusion Assessment Method) were completed to assess potential delirium (Table 1). In the majority of cases, according to the criteria from the DSM-IV, our patients demonstrated delirious criteria. Because the purpose of our study was to explore the experiences of patients and their families from prolonged hospitalization, so we established a panel of expert ICU clinicians (two subspecialties in pulmonary diseases, two anesthesiologists, two neurologists, and two ICU nurses). We included patients and their families in this interview who had had more than 50-day hospitalization and at least 20-day (multiple days) of delirium.
Table 1. Diagnosis of Delirium a,b.
| DSM-IV-TR | CAM-ICU |
|---|---|
| Disturbed consciousness (eg, decreased ability to focus, sustain, or shift attention) | Feature 1: acute onset |
| Changes in cognition (eg, memory deficit, language disturbance) or accounted for by preexisting dementia | Feature 2: inattention |
| Disturbance develops over a short period of time and fluctuates | Feature 3: disorganized thinking |
| Evidence supports that the disturbance is directly caused by the patient's general medical condition | Feature 4: altered level of consciousness |
a Abbreviations: CAM, Confusion Assessment Method; DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision; ICU, intensive care unit.
b The patient exhibited signs that fulfilled all four criteria as described by DSM-IV-TR (left column). The diagnosis was also confirmed (right column) by the CAM-ICU, which requires the presence of features 1 and 2, and of either 3 or 4.
PHPs and their families comprised the participants in this study. All parts of the study were reviewed according to the consolidated criteria for reporting qualitative research (COREQ) statement (Figure 1) (25). The number of patients and their families assessed were 9 and 16, respectively.
Figure 1. Fellow Chart of Patients and Their Families' Recruitment and Interview.
3.4. Data Collection
Patients and their family members were interviewed several times (Table 2, Figure 1). The semi-structured interviews were conducted in a private room and face-to-face. In all interview sessions, AVA (first author) and AE (second author) directly managed the interview. Each interview took between 45 and 90 minutes. Interviews commenced with a general open ended question and then continued with supplementary queries that further expanded the participants' responses regarding their experiences from prolonged hospitalization. The participants were given the opportunity, and encouraged to talk about their experiences or what was on their mind about the study-related issues. The data gathering and analysis were carried out simultaneously. Information saturation was determined as the interview termination criterion.
Table 2. Profiles of the Interviewed Participants.
| Participant's number | Patient1 | Patient2 | Patient3 | Patient4 | Patient5 | Patient6 | Patient7 | Patient8 | Patient9 |
|---|---|---|---|---|---|---|---|---|---|
| Number of interviews | 3 | 2 | 2 | 2 | 1 | 4 | 3 | 2 | 3 |
| Average of total interview times, min | 213 | 123 | 120 | 187 | 103 | 189 | 187 | 124 | 301 |
| Number of interviewed family members | 2 | 1 | 5 | 2 | 1 | 1 | 1 | 1 | 2 |
| Average of total interview times, min | 69 | 76 | 298 | 129 | 89 | 45 | 50 | 65 | 79 |
3.5. Data Analysis
Max-Q-Data software (Version 2010, Marie-Elisabeth-Lüders-Straße 1 10625, Berlin, Germany) was used to assist with the storage, searching, initial and final coding of the qualitative data. Analysis of each interview was done by the researchers independently. In areas where the three did not agree, the definitions were explained and discussions continued until a consensus was achieved. Concerning the trustworthiness of the data, credibility was determined through member checking and prolonged engagement. Extended engagement with the participants within the research field also helped the first author to gain the participants' trust and provided a better understanding of the research fields. Member checking was conducted by asking the participants to ascertain the preliminary findings from the earlier interviews. The rigor of the study was improved by asking ten participants (five family members and five patients) to compare the results of the study with their own experiences. Four expert supervisors and three other doctoral students of nursing conducted the peer checking.
4. Results
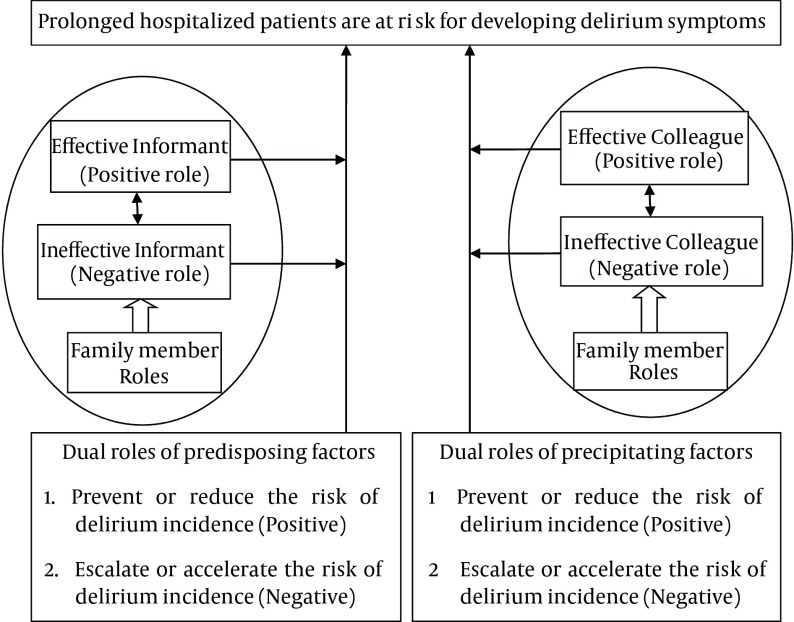
During the data analysis, two main themes from two different perspectives emerged namely,'patients’ perspectives' (experiences during ICU hospitalization), and 'family members’ perspectives' (supportive-communicative experiences). Although the main study findings was delirium, the patients also described pleasant and unpleasant, factual and delusional experiences, which introduced the concepts of intensive care delirium in an Iranian context (Table 3). Moreover, the family members' perspectives were in agreement with the predisposing and precipitating factors found for the patients' delirium (Figure 2). These results are explained below according to the participants’ interviews.
Table 3. Patients' Experiences from Delirium.
| Patients’ Experiences | Categories | Subcategories |
|---|---|---|
| Pleasant experiences | Life saving experiences | Breathing ability, Removal of secretions, Absence of bleeding, Attention by medical staff |
| Relieving bodily experiences | Being able to communicate, Ability to sleep, Being unrestricted in the bed, Moving in bed, Painless intensive interventions | |
| Relieving bodily sensations | Pain relief, Thirst relief, Feeling of security and safety, Being cared for, Pleasant dreams and hallucination | |
| Unpleasant experiences | Life threatening experiences | Severe bleeding, High levels and suffocating secretions, Inability to breathe, Shock and chaos |
| Jeopardized bodily experiences | Sleep disturbance, Disturbed communication, Restricted to bed, Intensive care interventions | |
| Annoying and distressful bodily sensations | Having pain, Being thirsty, Being hungry, Being dizzy and vertiginous, Restless in body, Fear of dying, Panic, Anxiety, Hallucinations |
Figure 2. Flow Chart of Mutual Interactions Between Family Member's Roles, Predisposing and Precipitating Risk Factors in Delirium.
4.1. Patients' Perspective (Experiences During Hospitalization in ICU)
All patients declared factual and delusional experiences during their hospitalization in the ICU. Each experience had two aspects; pleasant and unpleasant. The patients' experiences are shown in Table 3, but some of the most common experiences are presented as follow: According to patients who experienced sleep problems, hearing a familiar voice could effectively contribute to their ability to sleep in an unfamiliar environment.
In this regard, it is notable that every other night, the nursing personnel routinely held a Quran recitation for all hospitalized patients, especially PHPs. It was also noted that all of our patients were Muslims and believed that reading the Quran helped them to regain their health, and they were committed to the Quran recitation. Some of the patients expressed hearing special alarms as unpleasant factual recalls.
On the other hand, delusional experiences constituted the majority of patients' recalls.
4.2. Family Member's Perspective (Supportive-Communicational Experiences)
From the family members' perspective who visited their patients during the lengthy hospitalization period, having satisfactory communication and reasonable support were very significant. In other words, both of these factors are predisposing and precipitating factors of delirium prevention. By establishing satisfactory communication, all family members strongly believed that the caring personnel should develop a professional-therapeutic communication with family members. Furthermore, given such a relationship, family members can then more easily confide in them. The results of these professional-therapeutic relationships are definitely beneficial for the patients as they share a common goal. Professional personnel also need to have more specific information about the patient status before hospitalization, as often pertinent information is not recorded in the patient's chart. This information is important as it enables better management of the patient's condition, and the only source of this kind of information is from their family members.
Using these types of information has two effects. One effect refers to the predisposing factors; because the patient can more easily undergo the necessary treatments, without any interruptions or changes required in the process. The other effect refers to precipitating factors; because no unnecessary drugs need to be added to the patient's medication regimen and as far as possible, adverse drug effects and toxicity can be prevented.
In addition, it should also be noted that family members make up the free labor force behind ICU doors. These enthusiastic and unpaid workers volunteer themselves in order to improve the quality of care that their family member needs. Moreover, to create these effective therapeutic elements, family members are undeniably essential components. Through good communication with family members, the majority of the patient's habits and mannerisms can be understood more clearly. Some of these habits and mannerisms are very important as they enable better management of the patient's condition. Developing a good relationship between the patient's nurse and family members can be seen as a positive factor in decreasing the development of delirium.
5. Discussion
5.1. Patients' Perspective (Experiences During Hospitalization in ICU)
The information in each patient's interview was loaded with their experiences, and also contained a high frequency of delusional ones. Generally, there are three main reasons that can explain the factual and delusional experiences of the patients interviewed.
The majority of the patients in this study were Muslim and according to their religion (Islam), prayer must be done three times each day; but hospitalized patients could not and this inability had a very dismaying role during their hospitalization that transformed into delusional episodes where they felt that they were being scrutinized by the Guardians of Limbo.
Therapeutic procedures were interpreted as torture in different ways, including; physical, emotional, semantic, and perceptual, which is in accordance with the results of the literature review (26).
Other delusional and factual experiences were related to physical restriction (restraint of the limbs). Two patients declared that restraining their limbs was their worst memory of their ICU hospitalization. This finding is in accord with other studies (1). Other patients expressed that physical restriction was the best way to control them from the nurses' perspective, because that assured them that the patients couldn't pull out their therapeutic devices, however, the patient's assessment of their quality of nursing care was significantly decreased.
It is important to note that the perception of different experiences was dependent on the patients' level of consciousness, as the experiences have two aspects. One aspect was pleasant while the other was unpleasant. Although some of the unpleasant experiences were necessary for the patients' treatment, if the patients had a high level of consciousness they were able to understand the necessity of these procedures. In addition, the physical condition of the patient was also important, because patients who have prolonged hospital stays often have unpleasant experiences in the early days of their hospitalization, but as their physical situations improves, their perception of the ICU environment and its happenings, become increasingly pleasant. According to Table 3, each unpleasant experience has a corresponding pleasant one. For example, a life threatening experience is ameliorated by a lifesaving experience.
5.2. Family Members' Perspective
The major concern of patient's families was to communicate with the ICU personnel for the purpose of receiving informing about the patient's therapeutic progress. All family members believed that caring team personnel must involve the family from the beginning to the end of the therapeutic process. Accordingly, some family members were more enthusiastic in being involved with providing related care for the patient, while others may not. It is important that ICU personnel differentiate between the involvement of family members as a significant part of the caring process and informing them of the patient's status. This also includes the patient's prognosis, the impact of medical procedures on the patient's recovery, actual and potential complications of the medical processes, anticipated care needs after hospitalization and alternatives to the continuation of care. These findings are congruent with other studies (27). Although having this information is the right of the patient's family members. The most important reason for this is that 76% of spouses/caregivers and 73% of nurses reported severe distress related to a patient's delirium. Mean distress levels were significantly higher for spouses/caregivers than for nurses caring for the patients and even for the patients themselves (28).
According to Figure 2, family members have a very important role to play in the development of delirium symptoms in the patients. The informant role consists of two aspects across a broad spectrum (very effective informant to very ineffective informant). Effective and ineffective indexes refer to the ability of family members to convey and communicate their concerns to the nursing personnel about the patient's condition and also to provide important information for medical personnel such as real past medical history, real past drug history (herbal and non-herbal drugs), special habits and manners especially those that relate to the present illnesses.
Another role of family members is a collegial one. In this role, family members should aspire to cooperate with nursing personnel. In the first instance, from a nursing personnel's perspective, without family members' activities in the therapeutic process, there would be an increase in the workload of the nursing personnel. The support and assistance that family member's deliver to their loved ones is a valuable adjunct in the therapeutic process. Furthermore, increased endeavors of family members in the care of the patient enhanced the nursing personnel's level of satisfaction.
According to Figure 2, medical staff and family members have mutual behaviors in caring for delirious patients and it is advantageous for the patient if they can cooperate with each other. There are two aspects involved: one is related to the nurses' care of the delirious patients, while the other is related to the family members.
In regard to the nurses, some of the literature states that there is an increased workload on medical personnel and conflicts can arise between meeting the adequate care needs of the delirious patients, while not neglecting their other patients, in addition there is a requirement to comfort patients, while also maintaining their safety (29, 30). Moreover, previous studies have emphasized the difficulty of trying to manage and understand the patients' experience, when there is a lack of trust and unpredictable behavior (31, 32). The previously mentioned researches recommend a dichotomy between trying to understand the patient's experience, with providing basic care and maintaining patient safety, and to use that understanding as a therapeutic tool.
For family members, Morita et al. (33) carried out a qualitative analysis of interviews with 20 bereaved family members of cancer patients, who had developed delirium during the last two weeks before their death. Many families were distressed by the delirium and felt it reflected pain, mental distress, or anxiety about death in their loved ones; others felt the delirium was a relief from their suffering. The same research group (34) re-examined this issue in a multicenter questionnaire survey of 560 bereaved family members of cancer patients, who had experienced delirium before their death. More than two thirds of the 242 respondents recognized all of the delirium symptoms, other than somnolence. Many felt that there were deficits in the medical care provided, with a need for more explanation about delirium and for the medical staff to be less distant and to show greater respect for the patients' subjective world.
To sum up, it should be noted that family members are very valuable components in the therapeutic process of delirium; and medical personnel, especially nurses, should pay attention to these valuable and worthwhile components.
5.3. Implication For health Policy
Predisposing and precipitating risk factors for delirium have equal importance, and family members play an important role in preventing and reducing these episodes. Furthermore, encouraging family members to provide primary care for patients has several useful outcomes which result in reducing the incidence of PTSD in patients.
Acknowledgments
The authors would like to thank all patients and their family members for agreeing to participate in our study. Furthermore, our thanks go to the Sina Trauma Research Center and Baqiyatallah University of Medical Sciences for their financial support of this study.
Footnotes
Authors’ Contributions:Study conception and design: Amir Vahedian-Azimi, Abbas Ebadi, Soheil Saadat and Fazlollah Ahmadi; data collection and analysis: Amir Vahedian-Azimi, Abbas Ebadi, Soheil Saadat and Fazlollah Ahmadi; drafting of the manuscript: Amir Vahedian-Azimi, Abbas Ebadi, Soheil Saadat and Fazlollah Ahmadi; critical revisions to the paper for important intellectual content and English editing: Amir Vahedian-Azimi, Abbas Ebadi, Soheil Saadat and Fazlollah Ahmadi.
Funding/Support:This research received funding from two centers: Sina Trauma Research Center and Baqiyatallah University of Medical Sciences.
References
- 1.Mishra RK, Alalawi R, Raj R, Nugent KM. Prolonged acute care in a 52-year-old man with respiratory failure: lessons learned from 70-day intensive care unit hospitalization. J Crit Care. 2011;26(5):532.e9-532.e16. doi: 10.1016/j.jcrc.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Grandi C, Tomasi CD, Fernandes K, Stertz L, Kapczinski F, Quevedo J, et al. Brain-derived neurotrophic factor and neuron-specific enolase, but not S100beta, levels are associated to the occurrence of delirium in intensive care unit patients. J Crit Care. 2011;26(2):133–7. doi: 10.1016/j.jcrc.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Taipale PG, Ratner PA, Galdas PM, Jillings C, Manning D, Fernandes C, et al. The association between nurse-administered midazolam following cardiac surgery and incident delirium: an observational study. Int J Nurs Stud. 2012;49(9):1064–73. doi: 10.1016/j.ijnurstu.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Mattar I, Chan MF, Childs C. Risk Factors for Acute Delirium in Critically Ill Adult Patients: A Systematic Review. Int Scholar Res Notices . 2013;2013:1–10. doi: 10.5402/2013/910125. [DOI] [Google Scholar]
- 5.Rice KL, Bennett M, Gomez M, Theall KP, Knight M, Foreman MD. Nurses' recognition of delirium in the hospitalized older adult. Clin Nurse Spec. 2011;25(6):299–311. doi: 10.1097/NUR.0b013e318234897b. [DOI] [PubMed] [Google Scholar]
- 6.Godfrey M, Smith J, Green J, Cheater F, Inouye SK, Young JB. Developing and implementing an integrated delirium prevention system of care: a theory driven, participatory research study. BMC Health Serv Res. 2013;13:341. doi: 10.1186/1472-6963-13-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Milisen K, Cremers S, Foreman MD, Vandevelde E, Haspeslagh M, Geest SD, et al. The Strain of Care for Delirium Index: a new instrument to assess nurses' strain in caring for patients with delirium. Int J Nurs Stud. 2004;41(7):775–83. doi: 10.1016/j.ijnurstu.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Tsuruta R, Nakahara T, Miyauchi T, Kutsuna S, Ogino Y, Yamamoto T, et al. Prevalence and associated factors for delirium in critically ill patients at a Japanese intensive care unit. Gen Hosp Psychiatry. 2010;32(6):607–11. doi: 10.1016/j.genhosppsych.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 9.Pisani MA, Murphy TE, Araujo KL, Van Ness PH. Factors associated with persistent delirium after intensive care unit admission in an older medical patient population. J Crit Care. 2010;25(3):540 e1–7. doi: 10.1016/j.jcrc.2010.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neagoe AD. Delirium with manic and psychotic features associated with amantadine. Gen Hosp Psychiatry. 2013;35(6):680 e7–8. doi: 10.1016/j.genhosppsych.2013.03.023. [DOI] [PubMed] [Google Scholar]
- 11.Sadananda SK, Narayanaswamy JC, Srinivasaraju R, Math SB. Delirium during the course of electroconvulsive therapy in a patient on lithium carbonate treatment. Gen Hosp Psychiatry. 2013;35(6):678 e1–2. doi: 10.1016/j.genhosppsych.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 12.Hall RJ, Meagher DJ, MacLullich AM. Delirium detection and monitoring outside the ICU. Best Pract Res Clin Anaesthesiol. 2012;26(3):367–83. doi: 10.1016/j.bpa.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Devlin JW, Al-Qadhee NS, Skrobik Y. Pharmacologic prevention and treatment of delirium in critically ill and non-critically ill hospitalised patients: a review of data from prospective, randomised studies. Best Pract Res Clin Anaesthesiol. 2012;26(3):289–309. doi: 10.1016/j.bpa.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Shehabi Y, Riker RR, Bokesch PM, Wisemandle W, Shintani A, Ely EW, et al. Delirium duration and mortality in lightly sedated, mechanically ventilated intensive care patients. Crit Care Med. 2010;38(12):2311–8. doi: 10.1097/CCM.0b013e3181f85759. [DOI] [PubMed] [Google Scholar]
- 15.George C, Nair JS, Ebenezer JA, Gangadharan A, Christudas A, Gnanaseelan LK, et al. Validation of the Intensive Care Delirium Screening Checklist in nonintubated intensive care unit patients in a resource-poor medical intensive care setting in South India. J Crit Care. 2011;26(2):138–43. doi: 10.1016/j.jcrc.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Mistraletti G, Pelosi P, Mantovani ES, Berardino M, Gregoretti C. Delirium: clinical approach and prevention. Best Pract Res Clin Anaesthesiol. 2012;26(3):311–26. doi: 10.1016/j.bpa.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 17.Nouwen MJ, Klijn FA, van den Broek BT, Slooter AJ. Emotional consequences of intensive care unit delirium and delusional memories after intensive care unit admission: a systematic review. J Crit Care. 2012;27(2):199–211. doi: 10.1016/j.jcrc.2011.07.074. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Z, Pan L, Ni H. Impact of delirium on clinical outcome in critically ill patients: a meta-analysis. Gen Hosp Psychiatry. 2013;35(2):105–11. doi: 10.1016/j.genhosppsych.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 19.Mattoo SK, Grover S, Gupta N. Delirium in general practice. Indian J Med Res. 2010;131:387–98. [PubMed] [Google Scholar]
- 20.Bruno JJ, Warren ML. Intensive care unit delirium. Crit Care Nurs Clin North Am. 2010;22(2):161–78. doi: 10.1016/j.ccell.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 21.Sharma A, Malhotra S, Grover S, Jindal SK. Incidence, prevalence, risk factor and outcome of delirium in intensive care unit: a study from India. Gen Hosp Psychiatry. 2012;34(6):639–46. doi: 10.1016/j.genhosppsych.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 22.van den Boogaard M, Schoonhoven L, van der Hoeven JG, van Achterberg T, Pickkers P. Incidence and short-term consequences of delirium in critically ill patients: A prospective observational cohort study. Int J Nurs Stud. 2012;49(7):775–83. doi: 10.1016/j.ijnurstu.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 23.Vasilevskis EE, Han JH, Hughes CG, Ely EW. Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol. 2012;26(3):277–87. doi: 10.1016/j.bpa.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 26.Samuelson KA. Unpleasant and pleasant memories of intensive care in adult mechanically ventilated patients--findings from 250 interviews. Intensive Crit Care Nurs. 2011;27(2):76–84. doi: 10.1016/j.iccn.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 27.Nelson JE, Kinjo K, Meier DE, Ahmad K, Morrison RS. When critical illness becomes chronic: informational needs of patients and families. J Crit Care. 2005;20(1):79–89. doi: 10.1016/j.jcrc.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 28.O'Malley G, Leonard M, Meagher D, O'Keeffe ST. The delirium experience: a review. J Psychosom Res. 2008;65(3):223–8. doi: 10.1016/j.jpsychores.2008.05.017. [DOI] [PubMed] [Google Scholar]
- 29.Grover S, Shah R. Distress due to delirium experience. Gen Hosp Psychiatry. 2011;33(6):637–9. doi: 10.1016/j.genhosppsych.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 30.Eeles EM, Pandy S, Ray JL. Delirium: a disorder of consciousness? Med Hypotheses. 2013;80(4):399–404. doi: 10.1016/j.mehy.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 31.Tsuruta R, Oda Y, Shintani A, Nunomiya S, Hashimoto S, Nakagawa T, et al. Delirium and coma evaluated in mechanically ventilated patients in the intensive care unit in Japan: A multi-institutional prospective observational study. J Crit Care. 2014;29(3):472 e1–5. doi: 10.1016/j.jcrc.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 32.Hosie A, Agar M, Lobb E, Davidson PM, Phillips J. Palliative care nurses' recognition and assessment of patients with delirium symptoms: A qualitative study using critical incident technique. Int J Nurs Stud. 2014 doi: 10.1016/j.ijnurstu.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 33.Morita T, Namba M, Akechi T, Ikenaga M, Inoue S, Kohara H, et al. Terminal delirium: recommendations from bereaved families' experiences. J Pain Symptom Manage. 2007;34(6):579–89. doi: 10.1016/j.jpainsymman.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 34.Namba M, Morita T, Imura C, Kiyohara E, Ishikawa S, Hirai K. Terminal delirium: families' experience. Palliat Med. 2007;21(7):587–94. doi: 10.1177/0269216307081129. [DOI] [PubMed] [Google Scholar]