We evaluated changes in rates of new HIV diagnoses in Canada. Our analyses were based on Health Canada data obtained for the period 1995 to 2011. British Columbia, of all Canadian jurisdictions, has had the largest decline in the rate of HIV new diagnoses and in lifetime costs averted over the study period.
Highly active antiretroviral therapy (HAART) has been shown to reduce viral load at both the individual and community levels, thus significantly extending the lives of persons living with HIV and markedly reducing the risk of HIV transmission [1-4]. Population-based studies in San Francisco, Taiwan and British Columbia, Canada have further shown HAART to reduce new infections by up to 60% [5-7]. We have previously shown that each 10% increase in HAART coverage is associated with a decrease in the rate of new HIV diagnoses of 8% [95% confidence interval (CI) 2.4, 13.3%] [7]. HIV treatment is now accepted as one of the most promising tools to curb the impact of HIV/AIDS, as it at once it is highly effective in terms of preventing HIV/AIDS morbidity and mortality as well as HIV transmission [8,9].
A previous analysis of annual trends in new HIV diagnoses per capita revealed substantial regional disparities in the burden of HIV/AIDS in Canada [7]. In the present analysis, we examined longitudinal rates of new HIV diagnoses by province and territory in Canada. In particular, we compared British Columbia against the rest of the Canadian provinces and territories, in view of the continued expansion of HAART coverage in British Columbia (from 1996 to 2011). Counts of new HIV cases by province and territory from 1995 to 2011 were obtained from Health Canada [10], while corresponding censual and inter-censual population figures were obtained from Statistics Canada [11]. Trends in new diagnoses were assessed using linear regression to fit a trend line through the respective data points for each province or territory.
In Canada, there are an estimated 71 300 (range 58 600-84 000) individuals infected with HIV, of whom 54 700 (44 400–65 000) are men [10]. The majority reside in Ontario, Quebec and British Columbia and their routes of infection are men who have sex with men (MSM) (46.7%), heterosexual contact (34.5%) or injecting drug use (16.9%) [7,10]. In British Columbia, the proportion of injecting drug users is considerably higher at 31.1%, although MSM still represent the majority of those infected (42.3%) in the province [10].
A total of 41 456 new HIV diagnoses occurred in Canada from 1995 to 2011, with the number decreasing by 24% from 2948 in 1995 to 2221 in 2011 and per capita rates decreasing from 10.06 to 6.44 per 100 000 population over the same time period. As shown in Figure 1, the majority of these new HIV diagnoses occurred in Ontario (17793; 42.9%), Quebec (7312; 17.6%) and British Columbia (9589; 23.1%). British Columbia had the largest decrease in new HIV diagnoses, from 18.05 to 6.49 per 100 000 population (2.78-fold; P < 0.001), with rates originally being higher than those in all other provinces and territories and now being lower than those in Ontario, Manitoba and Saskatchewan. Annual rates of new HIV diagnoses have also declined in Ontario, Quebec and the Atlantic Provinces. The largest decline was in the Atlantic Provinces (2.32-fold; P = 0.003), followed by Ontario (1.71-fold; P = 0.031) and Quebec (1.44-fold; P = 0.002). However, in Saskatchewan rates increased nearly 8-fold from 2.76 to 16.17 per 100 000 population (P < 0.001), while in Manitoba they increased from 4.52 to 6.53 per 100 000 population over the study period. The majority of the increase in new HIV diagnoses in Saskatchewan and Manitoba was attributable to an increase in new infections among First Nations peoples [12,13]. Rates in Alberta and in the Territories (not shown in Fig. 1 because of small numbers) have remained constant over the study period.
Fig. 1.
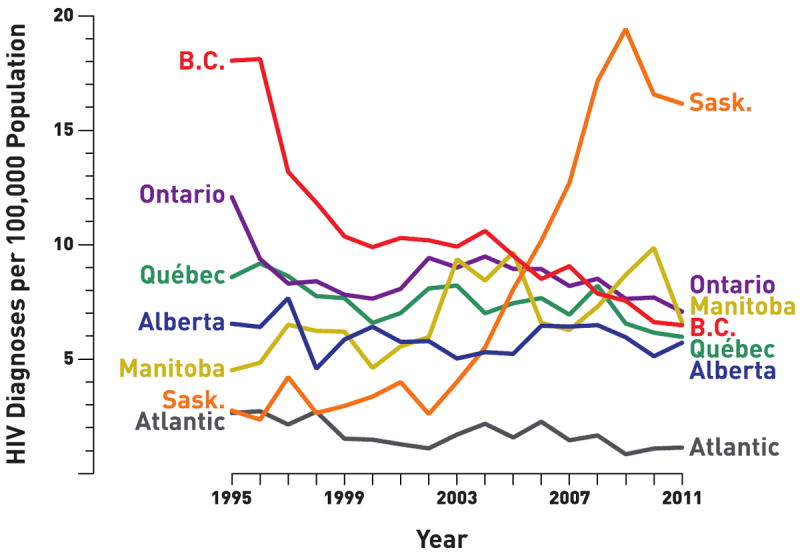
Rates of new HIV infections in Canada, by province or region, from 1995 to 2011. Atlantic, Atlantic Provinces; BC, British Columbia; Sask., Saskatchewan.
In a previous article, we estimated the number of averted cases of HIV infection in Canada that would have occurred if the rates in 1995 had remained constant until 2008 [7]. Based on the latest estimates of lifetime costs of HIV-positive individuals accessing treatment (present cost $CDN 396 000 per person) [14], British Columbia averted $CND 3.06 million per 100 000 population in lifetime costs for averted cases of HIV infection since 1996 compared with $CND 1.38 million and $CND 432 000 per 100 000 population, respectively, for Ontario and Quebec. In contrast, Saskatchewan and Manitoba may have incurred an additional cost of $CND 2.06 million and $CND 956 000 per 100 000 population, respectively, for the increment in new cases since 1996.
British Columbia has had the largest decline in the rate of HIV new diagnoses and in lifetime costs averted of all Canadian jurisdictions over the study period. Relatively smaller decreases in rates were also observed in Atlantic Provinces, Ontario, and Quebec. However, notable increases in rates were observed in Manitoba and Saskatchewan. The decline in new cases, observed in BC and elsewhere, may be at least partially attributed to the accelerated expansion of HAART coverage [8,9,15] and will contribute to a significant reduction in future costs associated with these averted cases. Further efforts are needed to optimize the potential impact of Treatment as Prevention in the whole of Canada.
References
- 1.Antiretroviral Cohort Collaboration. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372:293–299. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wood E, Kerr T, Marshall BDL, et al. Longitudinal community plasma HIV-1 RNA concentrations and incidence of HIV-1 among injecting drug users: prospective cohort study. BMJ. 2009;338:b1649. doi: 10.1136/bmj.b1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 Infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Attia S, Egger M, Müller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS. 2009;23:1397–1404. doi: 10.1097/QAD.0b013e32832b7dca. [DOI] [PubMed] [Google Scholar]
- 5.Porco TC, Martin JN, Page-Shafer KA, et al. Decline in HIV infectivity following the introduction of highly active antiretroviral therapy. AIDS. 2004;18:81–88. doi: 10.1097/01.aids.0000096872.36052.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fang CT, Hsu HM, Twu SJ, et al. Decreased HIV transmission after a policy of providing free access to highly active antiretroviral therapy in Taiwan. J Infect Dis. 2004;190:879–885. doi: 10.1086/422601. [DOI] [PubMed] [Google Scholar]
- 7.Hogg RS, Heath K, Lima VD, et al. Disparities in the burden of HIV/AIDS in Canada. PloS ONE. 2012;7:e47260. doi: 10.1371/journal.pone.0047260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montaner JS, Hogg R, Wood E, et al. The case for expanding access to highly active antiretroviral therapy to curb the growth of the HIV epidemic. Lancet. 2006;368:531–536. doi: 10.1016/S0140-6736(06)69162-9. [DOI] [PubMed] [Google Scholar]
- 9.Montaner J. Treatment as prevention-a double hat-trick. Lancet. 2011;378:208–209. doi: 10.1016/S0140-6736(11)60821-0. [DOI] [PubMed] [Google Scholar]
- 10.Public Health Agency of Canada. HIV and AIDS in Canada. Ottawa, ON: Surveillance and Risk Assessment Division, Centre for Communicable Diseases and Infection Control, PHAC; 2012. Surveillance Report to December 31, 2011. [Google Scholar]
- 11. [6 August 2013];Statistics Canada Table 051-0001: estimates of population, by age group and sex for July 1, Canada, provinces and territories, annual (persons unless otherwise noted) Available at http://cansim2.statcan.gc.ca/cgi-win/cnsmcgi.exe?Lang=E&RootDir=CII/&ResultTemplate=CII/CII___&Array_Pick=1&ArrayId=0510001.
- 12.Public Health Agency of Canada. Estimates of HIV Prevalence and Incidence in Canada, 2011. Ottawa, ON: Surveillance and Risk Assessment Division, Centre for Communicable Diseases and Infection Control, PHAC; 2012. [Google Scholar]
- 13.Saskatchewan Ministry of Health. [6 August 2013];Saskatchewan’s HIV Strategy 2010–2014. Available at www.health.gov.sk.ca/hiv-strategy-2010-2014.
- 14.Sloan CE, Champenois K, Choisy P, et al. Cost-Effectiveness of Preventing AIDS Complications (CEPAC) investigators. Newer drugs and earlier treatment: impact on lifetime cost of care for HIV-infected adults. AIDS. 2012;26:45–56. doi: 10.1097/QAD.0b013e32834dce6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Montaner JSG, Lima VD, Barrios R, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet. 2010;376:532–539. doi: 10.1016/S0140-6736(10)60936-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


