Abstract
Setting: One hundred and forty non-governmental organisations implementing human immunodeficiency virus (HIV) prevention programmes among clients, including people who inject drugs, prisoners, female sex workers, men who have sex with men and street children in Ukraine, 2010–2011.
Objective: Among enrolled clients, to assess factors associated with HIV testing, HIV retesting within a year of initial testing and HIV seroconversion.
Design: Retrospective cohort study involving record reviews.
Results: Of 192 487 clients, 42 109 (22%) underwent an initial HIV test (22% were positive). Among HIV-negative clients at baseline, 10 858 (27%) were retested within a year: 317 (3%) of these were HIV-positive. HIV testing and retesting rates were lower among prisoners (0.3%) and others (street children and partners of those in risk groups, 6%), and those who did not receive counselling or services such as condom and needle distribution. Individuals who were not counselled were more likely to seroconvert.
Conclusions: In this large cohort of high-risk groups from Eastern Europe, HIV testing was low and HIV sero-conversion was high. This is of public health concern, bringing into question the overall quality of counselling and how well it is tailored to the specific needs of various risk groups. Qualitative studies to understand the reasons for non-testing are urgently required for designing client-specific interventions.
Keywords: HIV testing, HIV prevention, most-at-risk populations, HIV seroconversion, injection drug users
Abstract
Contexte : Cent quarante organisations non gouvernementales impliquées dans la mise en œuvre de programmes de prévention du virus de l'immunodéficience humaine (VIH) pour des clients comprenant des utilisateurs de drogues injectables, des détenus, des travailleuses du sexe, des homosexuels masculins et des enfants des rues en Ukraine de 2010 à 2011.
Objectif : Evaluer les facteurs associés au dépistage du VIH, à un second dépistage dans l'année qui suit et à une séroconversion parmi les clients enrôlés.
Schéma : Etude rétrospective de cohorte par revue de dossiers.
Résultats : Sur 192 487 clients, 42 109 (22%) ont eu un test VIH initial (22% étaient positifs). Parmi les clients négatifs au départ, 10 858 (27%) ont eu un deuxième test dans l'année, dont 317 (3%) se sont révélés VIH positifs. Les taux de dépistage initial et subséquent étaient plus faibles parmi les prisonniers (0,3%) et d'autres groupes comme les enfants des rues et les partenaires de groupes à risque (6%), ainsi que ceux qui n'avaient pas bénéficié de conseil ni de services comme la distribution de préservatifs et d'aiguilles. Les sujets qui n'avaient pas bénéficié de conseil étaient plus enclins à la séroconversion.
Conclusions: Dans cette vaste cohorte de groupes à risque élevé d'Europe de l'Est, le taux de dépistage était faible et le taux de séroconversion élevé. Cette situation est préoccupante en termes de santé publique et met en doute la qualité d'ensemble du conseil et la manière dont il est adapté aux besoins spécifiques de divers groupes à risque. Il est urgent de réaliser des études qualitatives afin de comprendre les raisons du non dépistage et d'élaborer des interventions spécifiques des clients.
Abstract
Marco de referencia: Las 140 organizaciones no gubernamentales que aplican programas de prevención de la infección por el virus de la inmunodeficiencia humana (VIH) a usuarios como los consumidores de drogas inyectables, los reclusos, las trabajadoras del sexo, los hombres que tienen relaciones sexuales con hombres y los niños de la calle en Ucrania entre el 2010 y el 2011.
Objetivo: Evaluar los factores que se asocian con la práctica de la prueba diagnóstica del VIH, la repetición de la prueba un año después de la primera y la seroconversión en los usuarios inscritos.
Método: Fue este un estudio retrospectivo de cohortes con análisis de las historias clínicas.
Resultados: De los 192 487 usuarios del programa, 42 109 recibieron una primera prueba del VIH (22%); 22% fueron positivos. De las personas con un resultado negativo inicial, 10 858 repitieron la prueba un año después (27%) y 317 de ellas obtuvieron un resultado positivo (3%). Las tasas de práctica de la prueba del VIH y de repetición de la misma fueron inferiores en los reclusos (0,3%), en el grupo de otros (los niños de la calle y las parejas de personas de los grupos de riesgo, 6%) y en las personas que no recibieron asesoramiento ni servicios como la distribución de agujas o preservativos. La seroconversión fue más frecuente en las personas que no recibieron orientación.
Conclusión: En este amplio estudio de cohortes de grupos de riesgo en Europa oriental, la tasa de pruebas diagnósticas del VIH fue baja y los índices de seroconversión fueron altos. Esta situación representa un problema de salud pública y pone en tela de juicio la calidad general de los programas de asesoramiento y la forma como estos se adaptan a las necesidades específicas de los diversos grupos de riesgo. Se precisan con urgencia estudios cualitativos que analicen las razones de la falta de la prueba diagnóstica, con el fin de elaborar intervenciones que sean específicas para determinados usuarios.
Ukraine is facing a concentrated human immuno-deficiency virus (HIV) epidemic,1 with a high prevalence of HIV in most-at-risk populations (MARPs), which include people who inject drugs (PWIDs), men who have sex with men (MSM), female sex workers (FSWs), street children and sexual partners of people from risk groups.2 The scaling up of prevention activities among MARPs is a vital step in controlling and reversing the HIV epidemic. HIV prevention programmes have been in operation since 2004 to prevent such individuals from acquiring and transmitting HIV infection and to provide HIV care if they acquire infection.3 PWID, FSWs, MSM, partners of PWIDs, prisoners aged ⩾18 years and street children aged between 10 and 19 years are considered to be programme clients once they have accessed project services and received a unique client code. All clients are offered rapid HIV testing and, if found to be HIV-positive, are linked to care and support services; if found to be HIV-negative, they are advised to repeat HIV testing every 6 months.4
Despite the availability of rapid HIV tests, anecdotal evidence suggests that a large number of clients are not undergoing testing. We also assume that among clients who do undergo testing and are found to be HIV-negative at the initial test, not everyone is undergoing retesting. This can hamper early HIV diagnosis, with consequent delays in accessing HIV care and treatment, which may lead to increased morbidity, mortality and continued progression of the HIV epidemic. Ensuring that all clients with high-risk behaviour know their HIV status and have access to prevention and care-related interventions is essential to curb the HIV epidemic and achieve the ambitious global goal of ‘zero HIV infections’ by 2015 and beyond.5
There are no published longitudinal data from Ukraine on the exact proportion of clients who were tested for HIV at baseline, the proportion who undergo retesting and factors associated with HIV testing behaviour of clients, nor is there any published information on HIV seroconversion among clients who were HIV-negative at initial testing. A huge longitudinal data set has been produced as a result of programme data recording. Since 2005, Alliance-Ukraine has been using a single registration and monitoring system for prevention services, known as the SyrEx database.5 This database monitors and analyses data on the number of clients covered, distributed materials and services provided to clients.
We aimed to describe the performance of HIV prevention programmes and assess factors associated with initial HIV testing, retesting and HIV seroconversion among clients enrolled in HIV programmes in Ukraine. The specific objectives were to 1) assess the number (proportion) of clients enrolled in HIV prevention programmes who underwent HIV testing, and 2) among those who were HIV-negative at initial testing, to assess the number who underwent retesting for HIV and the number found to be HIV-positive within a year of initial testing. We also assessed specific factors (age, sex, type of high-risk group, type of service, region and number of visits) associated with initial testing, retesting and HIV seroconversion.
METHODS
Design
This was a retrospective cohort study of clients enrolled in HIV prevention programmes in Ukraine in 2010–2011.
Setting
Ukraine, with a population of 45 million, has an HIV prevalence of 0.27% in the general population. It is estimated that about 230 000 people are living with HIV in Ukraine, the majority of whom are from high-risk groups. Nearly 46% of all HIV-positive individuals registered in 2012 were PWIDs. With an estimated 310 000 PWIDs (HIV prevalence 21.6%), 80 000 FSWs (HIV prevalence 10%) and 176 000 MSM (HIV prevalence 6.4%),2 there is considerable need for HIV prevention services.
To address this need, HIV prevention programmes have been widely implemented by local and international non-governmental organisations (NGOs) in Ukraine since 2004. The International HIV/AIDS Alliance in Ukraine (Alliance-Ukraine), in partnership with key civil society and government agencies, is leading the response to HIV/AIDS in Ukraine by providing sub-grants to over 140 local NGOs to implement a comprehensive package of services for high-risk groups. This package includes education, voluntary counselling and testing (VCT) for HIV, counselling provided by outreach or social workers, including promotion of VCT (referred to here as ‘counselling’), provision of female and male condoms with lubricants, needles and syringe distribution, diagnosis and treatment of sexually transmitted infections, testing for hepatitis B and C and screening for tuberculosis.4 All services are usually provided by outreach workers, except VCT, which is provided by a physician and a nurse at outreach sites or through mobile clinics.
According to data from Alliance-Ukraine, in 2011, HIV services reached 157 011 PWIDs (54% of estimated), 28 224 FSWs (40% of estimated), 19 130 MSM (20% of estimated) and 25 497 prisoners.6
Each client is advised to undergo HIV testing after enrolment.7 HIV testing is voluntary and provided together with pre- and post-test counselling by a physician and a nurse at the outreach site. In the case of a positive HIV result, the client is advised to undergo a confirmatory test, and is referred to the AIDS centre for initiation of HIV care, including antiretroviral treatment. In the case of a negative result, the client is provided with post-test counselling and advised to undergo HIV testing at least once every 6 months or within a month of a risk-behaviour incident. Clients are advised to present to the prevention services as often as they wish.
Study population
All clients enrolled into HIV prevention programmes in the 2 years from January 2010 to December 2011 were included in this study. The data cover 24 regions. Three regions (Dnipropetrovsk region, Chernivtsi region and Sevastopol city) were excluded from analysis due to technical problems with the data set. The analysis was conducted between March and November 2013.
Data variables and data source
Information on the following variables was extracted from SyrEx for the purpose of the study: unique client code, age, sex, primary risk group, initial HIV test result and date, HIV retesting status (test result) within a year of initial test, number of visits over a year from the initial test, services provided (needle exchange/condom distribution/counselling) and region.
Data analysis
Data from SyrEx were extracted and imported into Epi-Data Version V2.2.2.180 (EpiData Association, Odense, Denmark) for analysis. All information entered in SyrEx is de-identified and uses unique codes for each client. Data were summarised in means and proportions to describe the demographic and clinical profile of the clients. Relative risks (RR) with 95% confidence intervals were calculated to assess associations with HIV testing, retesting and HIV seroconversion. The χ2 test was used to assess statistical significance (P < 0.05) and χ2 for trend to assess linear trends.
Ethics approval
Ethics approval was obtained from the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease and the Committee on Medical Ethics of the Gromashevskiy Institute of Epidemiology and Infectious Diseases of the Ukrainian National Academy of Medical Science. As this was a retrospective review of de-personalised records and involved no direct interaction with the study participants, the need for informed consent was waived by the ethics committees.
RESULTS
Characteristics of the study population
Of 192 487 clients enrolled, 71% were males; the mean age of the cohort was 30 years (standard deviation 10.64). Clients included 118 834 (62%) PWIDs, 30 371 (16%) prisoners, 19 853 (10%) FSWs, 17 036 (9%) MSM and 6392 (3.3%) others (including street children and partners of those in risk groups).
Initial human immunodeficiency virus testing and retesting within one year
The Figure shows the enrolment, initial HIV testing and retesting rates in this population. Of all the clients enrolled, 42 109 (22%) underwent an initial HIV test; 1638 (4%) of these were HIV-positive. Among 10 858 (27%) who were initially HIV-negative and retested within a year, 317 (3%) became HIV positive.
FIGURE.
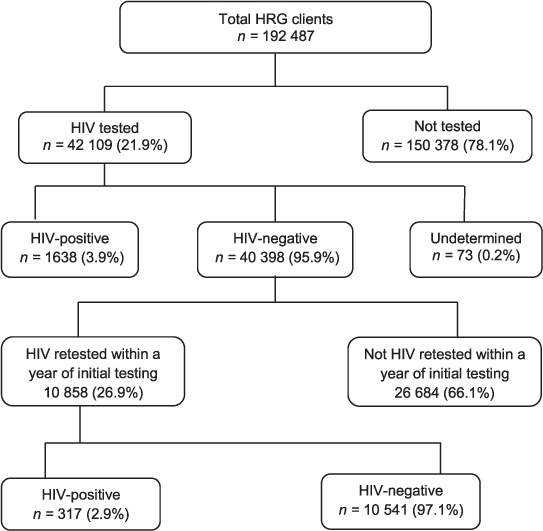
Enrolment, HIV testing and retesting and seroconversion among most at risk populations enrolled in HIV prevention programmes in Ukraine, 2010–2012. HRG = high-risk group; HIV = human immunodeficiency virus.
Factors associated with initial human immunodeficiency virus testing
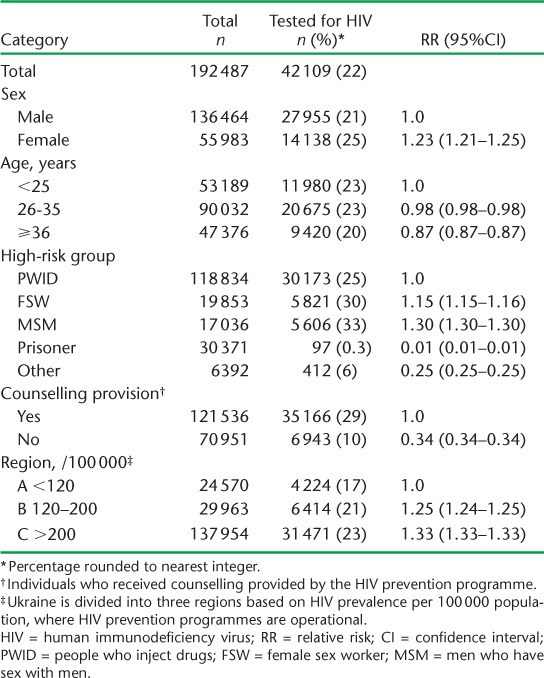
Factors associated with initial HIV testing are shown in Table 1. Despite receiving counselling from an outreach or social worker, which includes VCT promotion, only 29% of clients underwent HIV testing. The percentage of clients who received VCT was very low (10%). Females were more likely to be tested than males, although the difference was minimal (25% vs. 21%, respectively). Prisoners and others (street children and partners of those in risk groups) had the lowest proportion undergoing initial HIV testing (0.3% and 6%, respectively), while MSM had the highest (33%). Compared to PWIDs, MSM and FSWs were more likely to undergo initial HIV testing, while prisoners and others were less likely. There was a significant linear trend associated with uptake of initial HIV testing in regions of Ukraine with higher HIV prevalence (χ2 for trend 364, P < 0.0001).
TABLE 1.
Factors associated with accepting HIV testing (at baseline) among clients enrolled in HIV prevention programmes in Ukraine, 2010–2011
Factors associated with retesting for human immunodeficiency virus and seroconversion
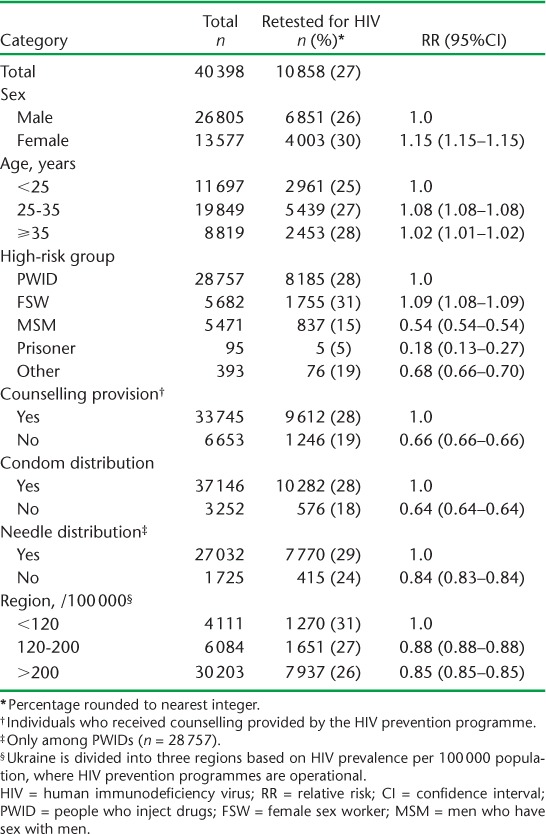
Factors associated with HIV retesting within a year of initial testing are shown in Table 2. Of 398 clients who were HIV-negative on initial HIV testing, only 10 858 (27%) were retested for HIV within a year. Higher retesting rates were found among FSWs (31%) and in PWIDs (28%), while the lowest retesting proportions were again among prisoners (5%). Provision of counselling and condom and needle distribution were associated with a higher likelihood of undergoing a second HIV test. Unlike initial HIV testing, fewer people in regions with high HIV prevalence underwent retesting (26%) than in low-prevalence regions (31%).
TABLE 2.
Factors associated with retesting for HIV within a year of initial HIV testing among clients enrolled in HIV prevention programmes in Ukraine, 2010–2011
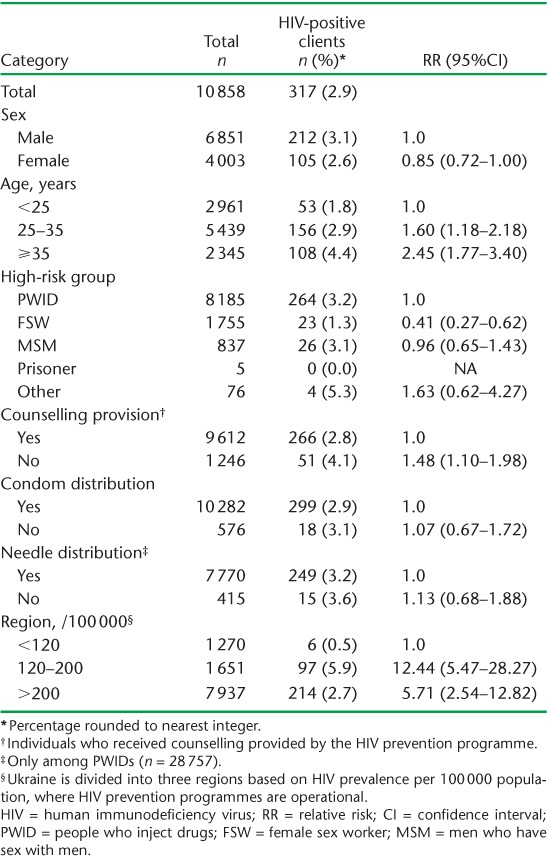
Factors associated with HIV seroconversion within one year of initial HIV testing are shown in Table 3. Individuals aged >25 years had a higher risk of HIV seroconversion than younger age groups, while FSW had a lower risk of seroconversion than PWIDs. Individuals who did not receive counselling were more likely to seroconvert than those who were counselled. Clients from regions with overall HIV prevalence ranging from 120 to 200 HIV cases per 100 000 population were 12 times more likely to become HIV-positive in 12 months than those from regions with an overall HIV prevalence of <120/100 000. Clients from regions with overall HIV prevalence >200/100 000 were five times more likely to seroconvert in 12 months. Neither condom nor syringe distribution were significantly associated with seroconversion, but this may be partly due to the fact that most clients received these services.
TABLE 3.
Factors associated with HIV seroconversion within a year of initial HIV testing among clients enrolled in HIV prevention programmes in Ukraine, 2010–2011
DISCUSSION
This study is the first attempt to analyse one of the largest cohorts of high-risk groups in an Eastern European country. It included prospective follow-up data on almost one fifth of a million vulnerable and excluded persons. This is a laudable achievement, and is an example of how NGOs can effectively contribute to HIV prevention within a hard-to-reach population where access to conventional health services is problematic and HIV transmission is intense.
A strength of this study is that it used aggregated and standardised data from 140 NGOs working with MARPs in Ukraine. Standard data collection forms were used to gather data and there was a system of quarterly monitoring, reporting and data quality control procedures in place. We thus believe that the data are robust. As the study was collected from settings where MARPs are concentrated, it is also likely to reflect the reality in the field. This is an example of how routine monitoring data collected through standardised software systems can contribute to knowledge about the HIV epidemic and the effectiveness of preventive strategies. This can be a valuable addition to knowledge produced through integrated bio-behavioural surveys and operational studies.
A discouraging finding was that only two in ten individuals underwent initial HIV testing and no more than three in ten underwent retesting within a year of the initial test—a waterfall reduced to a trickle. As HIV testing is a critical path to offering prevention and care to MARPs, this is of serious public health concern, and HIV prevention programmes must rethink their outreach HIV testing strategies.
Several findings of this study are of public health importance. First, HIV positivity among those initially tested for HIV was 3.9%, which seems low in a context where groups such as PWIDs and FSWs are known to have a high prevalence, of 22% and 10%, respectively.8,9 The reasons may be that those who know their HIV status do not attend for HIV testing and that many who feel they might be HIV-positive avoid HIV testing sites due to fear of breaching confidentiality and peer stigmatisation.
On the other hand, HIV prevalence among those who underwent retesting within 12 months was 2.9%; this seems high, and may indicate continuing high-risk behaviour and recent HIV outbreaks. As overall retesting rates are low, it is also possible that those who return for testing are more likely to have risk behaviours. Regions with average HIV prevalence in the general population have higher seroconversion rates than those with high prevalence. This may be explained by a higher concentration and longer history of HIV prevention programmes in high-prevalence regions, which may have had a positive influence in reducing clients' risk behaviour over time. Network-related mechanisms may also influence seroconversion.10 This finding suggests that HIV prevention should be strengthened in regions with average HIV prevalence.
Second, even among those who underwent HIV counselling, only three in ten individuals underwent initial HIV testing. This undermines the effectiveness of counselling in terms of HIV testing promotion. We might need to deal with HIV testing stigmatisation and breach of confidentiality, as well as other fears about the use of HIV services.11 Offering psychological support and sex- and age-specific services as part of the essential package of care and client-tailored counselling may be required to improve HIV testing in general. This is a critical area requiring a review of counselling approaches.
Third, prisoners and others (street children and partners of high-risk groups) had a significantly lower likelihood of being tested and retested, and this may reflect difficulties related to access. It is difficult to reach prisoners due to administrative barriers and punitive laws. Closer collaboration with prison authorities and informal prison community leaders is essential. Educational programmes focusing on the benefits of HIV testing and early treatment initiation as well stigma reduction campaigns might improve testing rates in prisons, but this needs to be evaluated in an operational setting. The migratory nature of street children is a serious challenge; psychological difficulties and the legal restrictions related to working with underage groups may influence the effectiveness of counselling messages. This warrants specific qualitative research to tailor prevention in this sub-group.
Fourth, FSWs were more likely to undergo initial HIV testing and retesting and were less likely to seroconvert than PWIDs. This may be because ongoing HIV prevention activities, and in particular the organisation of HIV testing, are better suited to FSWs than PWIDs. FSWs reportedly prioritise their health and express a need for testing services.12 HIV testing should be adapted to increase uptake by PWIDs. The observed higher seroconversion among PWIDs may be the result of ongoing HIV transmission through sharing contaminated needles, and continued attention to safer injecting practices is required, despite encouraging data that 95.5% of PWIDs had used sterile equipment for their last injection.9
Finally, it is well known that HIV testing in MARPs requires multiple approaches, including night-time (moonlight) testing, mobile outreach, community engagement, activism and advocacy.13 In many cases, this is actually taking place on the ground, but the data suggest that effectiveness is still low. Current approaches may thus need to be reviewed and further adapted.
One of the main limitations of this study is that we do not have data on the HIV status of those who did not retest for HIV. In addition, retesting rates are low and seroconversion rates may not be generalisable. Data on risk group characteristics are also limited and do not include additional risk information, such as injecting drug use and engagement in sex work, which might have an effect on HIV seroconversion.
In conclusion, achieving the UNAIDS objective of ‘getting to zero’ new HIV infections by 2015 and beyond requires priority actions targeting high-risk group populations. Failing to address this will lead to continued intense HIV transmission within high-risk groups, and a risk of transmission to the general population, a trend that is already visible in Ukraine.
This study shows that only a very limited proportion of MARPs in Ukraine currently undergo HIV testing, and that HIV seroconversion rates are substantial, indicating the need for urgent attention and focused interventions. Several challenges have been identified and ways forward suggested.
Acknowledgments
This research was supported through an operational research course that was jointly developed and run by International Union Against Tuberculosis and Lung Disease (The Union), SouthEast Asia Office, Delhi, India; the Centre for Operational Research, The Union, Paris, France; and the Operational Research Unit (LUXOR), Médecins Sans Frontières, Brussels Operational Centre, Luxembourg. This course is under the umbrella of the World Health Organization (WHO-TDR) SORT IT (Structured Operational Research and Training Initiative) programme for capacity building in low- and middle-income countries. Funding for the course was from an anonymous donor and the Department for International Development, UK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflict of interest: none declared.
References
- 1.Ministry of Health of Ukraine. Ukraine harmonized AIDS response progress report. Kyiv, Ukraine: Ministry of Health; 2012. January 2010–December 2011. [Google Scholar]
- 2.HIV-infection in Ukraine. Kyiv, Ukraine: Ministry of Health; 2012. Bulletin 38. [Google Scholar]
- 3.Bergmann H, Stash S. Promising approaches to combination HIV prevention programming in concentrated epidemics. Boston, MA, USA: John Snow, Inc; 2010. AIDSTAR-One. [Google Scholar]
- 4.International HIV/AIDS Alliance in Ukraine. Annual Report for 2012. Kyiv, Ukraine: International HIV/AIDS Alliance in Ukraine; 2013. [Google Scholar]
- 5.UNAIDS. 2011–2015 Strategy. Getting to zero. Geneva, Switzerland: UNAIDS; 2010. http://www.unaids.org/en/aboutunaids/unaidsstrategygoalsby2015/ Accessed April 2014. [Google Scholar]
- 6.World Health Organization. WHO report 2007. Global tuberculosis control: surveillance, planning, financing. Geneva, Switzerland: WHO; 2007. WHO/HTM/TB/2007.376. [Google Scholar]
- 7.International HIV/AIDS Alliance in Ukraine. Annual Report for 2011. Kyiv, Ukraine: International HIV/AIDS Alliance in Ukraine; 2012. [Google Scholar]
- 8.International HIV/AIDS Alliance in Ukraine. Counselling and testing for HIV using rapid tests in prevention projects among groups at risk of HIV infection. Kyiv, Ukraine: International HIV/AIDS Alliance in Ukraine; 2012. [Google Scholar]
- 9.International HIV/AIDS Alliance in Ukraine. Behaviour monitoring and HIV-infection prevalence among commercial sex workers as a component of second generation surveillance. Kyiv, Ukraine: International HIV/AIDS Alliance in Ukraine; 2012. [Google Scholar]
- 10.Balakiryeva O, Bondar T, Sereda Y, Sazonova Y. Behaviour monitoring and HIV prevalence among injecting drug users as a component of second generation sentinel surveillance. Kyiv, Ukraine: International HIV/AIDS Alliance in Ukraine; 2012. [Google Scholar]
- 11.Friedman S R, Kottiri B J, Neaigus A, Curtis R, Vermund S H, Des Jarlais D C. Network-related mechanisms may help explain long-term HIV-1 seropreva-lence levels that remain high but do not approach population-group saturation. Am J Epidemiol. 2000;152:913–922. doi: 10.1093/aje/152.10.913. [DOI] [PubMed] [Google Scholar]
- 12.Mateu-Helabert P, Shulga L, Dvinskykh N, Varban M Summary of results of the ethnographic study of the lifestyle and principal behavioral models of the injecting drug users in Kyiv. Kyiv, Ukraine: International HIV/AIDS Alliance in Ukraine; 2013. [Google Scholar]
- 13.International HIV/AIDS Alliance in Ukraine. Ethnographic survey of the sex business in specific regions of Ukraine. Kyiv, Ukraine: International HIV/AIDS Alliance in Ukraine; 2013. [Google Scholar]
- 14.World Health Organization. Service delivery approaches to HIV testing and counselling (HTC): a strategic policy framework. Geneva, Switzerland: WHO; 2012. http://www.who.int/hiv/pub/vct/htc_framework/en/ Accessed April 2014. [Google Scholar]


