Abstract
Background: Reproductive years represent a major proportion of women‟s life. This review focuses on recommended nutritional considerations, physical activity pattern as well as the effect of nutrition education (NE) on behavior modification and health outcomes of women of reproductive age using either single-level, multiple-level or community-level interventions.
Methods: For this narrative review, numerous searches were conducted on databases of PubMed, Science Direct and Google Scholar search engine using the keywords women, reproductive age, NE, interventions, community-based.
Results: Even though single intervention is effective, multiple intervention programmes in addition to behavior modification components are even more successful in terms of modified behaviors and health outcomes. Moreover, community based interventions using multilevel strategies are further useful for improved health outcomes and behavior modification.
Conclusion: NE programmes have been effective in positive behavior modification measured in terms of eating pattern and health quality. Thus, it is recommended that health professionals use multiple intervention strategies at community level to ensure improved outcomes. Political support is also required to create culturally sensitive methods of delivering nutritional programmes. Finally, as policy is dependent on program cost, nutritional programmes need to combine methods of cost analysis to show cost effectiveness of supplying adequate nutrition for women throughout the lifecycle.
Keywords: Reproductive age, Behavior modification, Nutrition education, Physical activity, Intervention
Introduction
Across all cultures, a healthy baby and mother are cherished dreams and hopes of all families.1 However, besides emphasizing on pregnancy and birth outcomes, considering the different stages of women’s health, that is, during infancy, adult life, preconception period, pregnancy, lactating phase (a life course perspective) is essential to reduce risk of any pregnancy related complications and deaths as well as to eradicate disparities through enhanced health promotion and disease prevention.2For instance, an adequate nutrition before the reproductive years helps to ensure achievement of proper adolescent growth, sufficient nutrient store during reproductive years for a healthy pregnancy and an appropriate nutritional status especially to maintain skeletal health during the postmenopausal period. Hence, the need for maintaining optimal food habits throughout a woman’s lifetime is essential to optimize both her and her offspring’s health.3Women should also be exposed to health topics and encouraged to participate in health promotion programmes so as to promote healthy eating habits and thus achieve optimal nutritional status.4 Considerations include diet quality as well as body mass index (BMI).
Nutrition education (NE) is an essential consideration to optimise health of women of reproductive age in addition to pregnancy outcomes. NE programmes are important as they target at enhancing subjects’ dietary intakes by promoting behavioral changes such as food choice and cooking ability, goal-setting, motivation, and support the efforts for a change.5For instance, Dean et al. discussed that preconception nutrition-specific interventions in particular increased folic acid and multivitamins supplements among pregnant women resulted in positive pregnancy outcomes.6Furthermore, Rao demonstrated an improvement in haemoglobin level through a nutrition awareness program comprising of informal meeting sessions, cookery activities to disseminate knowledge about use of iron rich foods and kitchen garden activity.7 Recent evidence also draws attention to the need to contemplate the wide-ranging spectrum of social, cultural and economic factors, as well as the significance of engaging family members to optimize health of women of reproductive age when designing health interventions.8The objectives of this paper are:
To outline recommended healthy lifestyle behaviors such as nutrition, physical activity and alcohol consumption
To discuss the effectiveness of nutrition education programs aiming at improving diet, physical activity and overall health of women of reproductive age
Methods
For this review, scientific information from published papers was analyzed. Searches were conducted using various databases[such as Google scholar, PUBMED, Ebscohost, Google scholar, Science Direct etc.] using the following search terms: ‘women of reproductive age’, ‘pregnant’, ‘postpartum’, ‘diet’, ‘physical activity’, ‘nutrition education’ and ‘intervention’. To be able to ascertain probable relationships, scientific evidence from cross-sectional, prospective cohort and experimental studies were also considered.
Ethical issues
There is no need for ethical clearance or any issues pertaining to same as long as statistics from governmental database or related information are not being used. Study also does not deal with any sensitive information pertaining to human, invasive procedures, informed consent.
Results
Malnutrition
Nutrient-related deficiency diseases, which can result to intrauterine growth retardation and other vitamins and minerals deficiency disorders, are manifested worldwide. As postulated by Kulasekaran, women of reproductiveage are particularly susceptible to malnutrition due to various social (for example low income level and illiteracy) and biological factors.9Malnutrition is mainly a matter of concern for women of reproductive age as a poor nutritional status not only impedes her own health but the health of her offspring is also at risk.10
Obesity
Obesity is a growing threat to women of childbearing age.11In women of reproductive age, the prevalence of grade I (BMI 30–34.9 kg/m2) and grade II (BMI 35–39.9 kg/m2) obesity has doubled since 1979 and that of grade III (BMI> 40 kg/m2) obesity has increased threefold over the same period.12
Many women are likely to maintain a considerable amount of weight postpartum, predisposing them to become overweight or obese with increasing age. As discussed by Paden and Avery, the BMI of women 15 years post pregnancy can be independently associated with factors such as pre-pregnancy BMI, weight gain during pregnancy, and weight loss in the first year postpartum.13 Postpartum weight retained from earlier pregnancies is also an important factor to a high BMI among women of reproductive age.4 In an effort to encourage proper weight gain during pregnancy, the Institute of Medicine,14 developed prenatal weight gain recommendation which is guided by the woman’s pre-pregnancy BMI (Table 1).
Table 1. Recommended total weight gain in pregnant women by pre pregnancy BMI (in kg/m2)14 .
| Weight-for-height category | Recommended total gain (kg) |
| Normal (BMI: 18.5-24.9) | 11.4–15.9 |
| Overweight (BMI: 25.0-29.9) | 6.8–11.4 |
| Obese (BMI: ≥ 30) | 5.0–9.0 |
Underweight
Although health risk factors and death have been mostly associated with overweight and obesity, underweight is equally related to excess deaths.15 In many countries (e.g. in Africa and South Asia), women of reproductive age having a BMI below the normal range is widespread, where some prevalence estimates of under-nutrition are as high as 27-51%.16 Being underweight is associated with several health risks such as a poor nutritional status, heart irregularities, osteoporosis, amenorrhea, and infertility. Pregnant women with a low BMI are at a greater risk for preterm delivery, low birth weight, and fetal growth restrictions.4,17
Diet
Women of reproductive age have the same dietary requirements as the general population whereas pregnant and lactating women have additional nutritional recommendations.18 For example; another 100 kcal/day in addition to dietary intake that allows a constant pre-pregnancy weight is generally satisfactory while, in later months of pregnancy, an additional 200 kcal/day is occasionally suggested. In order to meet these guidelines, simple carbohydrates should be restricted while complex carbohydrates in the form of starches, legumes, seeds and bread should be limited to reasonable quantities. Useful protein sources can be meat, fish, cheese and dairy products (source of calcium), supplemented with small amounts of butter and vegetable fats.19
Micronutrients are critical for women’s health during reproductive years and during pregnancy as well as during adolescence and post-menopausal period.3 The adverse effects of micronutrient deficiencies on the health and birth outcome of women are well known. Although poor dietary intake is a common cause of micronutrient deficiencies, other individual causes including genetics, nutrient and drugs interactions, poor absorption, as well as certain diseases can lead to such deficits. In particular, deficiencies of calcium, iron, folate, zinc, thiamine, riboflavin, and vitamins A, D, B-6 and B-12 are very frequent and of concern among women of reproductive age.5 Possible reasons for these micronutrients deficiencies are low income level and lack of education about healthy practices like healthy eating patterns.20 Deficiencies in these indispensable nutrients increase the of predisposal to adverse pregnancy outcomes such as neural tube defects, early fetal loss, preeclampsia, and maternal mortality.3,21 The best known recommendation for women anticipating pregnancy, is 400μg of folic acid supplements per day to avert the risk of neural tube defects 16 while pregnant women need to increase their daily intake to 600μg.22
Physical activity and alcohol consumption
Along with proper diet, other lifestyle patterns such as regular physical activity (PA) and reduced alcohol consumption are also indispensable among women of reproductive age. Regular PA has to be established preconceptionally so as to prevent several complications of pregnancy.23 In addition, exercise prior to pregnancy help woman to control weight and prevent mood swings during pregnancy as well as minimize the likelihood of depression post pregnancy.13 Women are recommended to practice regular PA for 30 to 60 minutes per day for 5 or more days per week.23
The US Centers for Disease Control and Prevention published preconception references to promote knowledge of healthy lifestyles practices and to discourage health risk behaviors (e.g., cigarette smoking and alcohol consumption).24 Alcohol exposure during the prenatal period is one of the main sources of neurodevelopmental deficits among children, as well as those of fetal alcohol spectrum disorder (FASD).25 In 2007, it was recommended that women should avoid consuming more than one or two units which is equivalent to 8-16 g of alcohol, once or twice a week.18 Studies have shown that a significant number of women who are engaged in risky behaviors such as substance abuse continue to enter pregnancy, thus increasing their risk for negative pregnancy outcomes. For instance, in 2002, as reported by Atrash et al.1 11.4% of pregnant women smoked during pregnancy, while 10.1% of pregnant women and 54.9% of women with a high pregnancy risk consumed alcohol. Furthermore, Green-Raleigh 26 reported that women not planning a pregnancy were more prone to unhealthy lifestyle including cigarette smoking and alcohol consumption during pregnancy while women intending a pregnancy were keener to adopt healthy behaviors in terms of vitamin and mineral supplements.
Nutrition Education Programs during Preconception
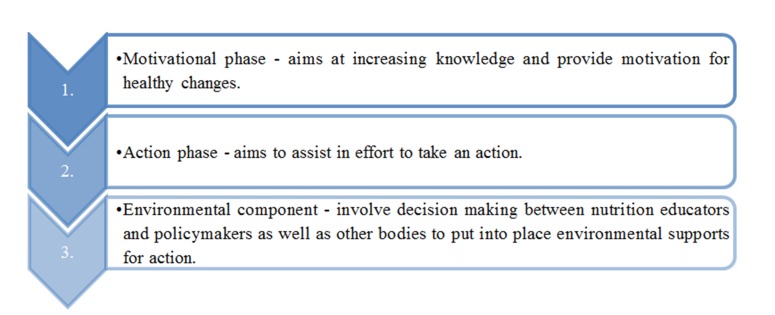
Nutrition education (NE) which consists of 3 phases (Fig.1) has been defined as “any combination of educational strategies, accompanied by environmental supports, designed to facilitate voluntary adoption of food choices and other food and nutrition-related behaviors conducive to health and well-being. NE is delivered through multiple venues and involves activities at the individual, community, and policy levels”.27
Fig.1.
Components or phases of nutrition education 27
Suitable preconception care is essential to ensure a healthy pregnancy and pregnancy outcomes.28 In order to be successful, preconception care has to consider different factors pertaining to the woman’s health. For instance, Curtis et al.29 proposed some of these considerations: a methodical risk assessment process to identify the medical, family, and reproductive health record of the woman, her nutritional status, societal constraints and/or any case of drug or substance abuse. Worldwide, the significance of preconception health and care has been supported for a healthy mother and child. Boulet et al.30 further emphasize that preconception programs and policies exist for almost three decades now, which indicate the significance of preconception intervention programs to ensure healthy pregnancy outcomes.
Importance and effectiveness of nutrition education programs during preconception
Women being an important pillar of the society especially in developing countries, women’s health should be given significant consideration which will assist in attaining the fourth and fifth goals of the millennium development program.30As put forth by Curtis et al.,29 many studies have supported the effectiveness of preconception care in terms of encouraging healthy behavioral practices, and controlling medical and other associated health risk factors to optimize both mother’s health and pregnancy outcomes.
For instance, as proposed by Bastani et al.31counseling during preconception about healthy diet and lifestyle can be the optimum time to encourage adequate daily iron and folic acid intake. NE programs endeavor to alter participants’ dietary intakes by remodeling behavioral factors, food choices and cooking skills, goal-setting, inspiration, and reinforce the change efforts.5“The CDC and its Select Panel have formulated four goals for health preconception” which are as follows:32
Improve the knowledge, attitudes, and behaviors of men and women related to preconceptional health.
Assure that all women of childbearing age in the United States receive preconception care services (i.e., evidence-based risk screening, health promotion, and interventions) that will enable them to enter pregnancy in optimal health.
Reduce risks indicated by a previous adverse pregnancy outcome through interventions during the interconceptional period that can prevent or minimize health problems for a mother and her future children.
Reduce the disparities in adverse pregnancy outcomes
Nutrition and Physical Activity Intervention Studies among Women of Reproductive Age
Sweet and Fortier33 recently discussed that although the benefits of participating in the recommended levels of physical activity and adhering to dietary recommendations have been confirmed for each separate health behavior, research indicates that “the combined effects of all diet and physical activity related behaviors that affect health directly and via their effects on obesity have a much larger total effect than any separate pathway”. The authors have also reported that multiple health behavior interventions have been effective at promoting required physical activity level and have encouraged positive dietary behaviors changes in terms of higher fruit and vegetable consumption and diminished fat intake, which have in turn, help in weight loss. However, the effectiveness of multiple health interventions is still a matter of reflection.
Nutrition interventions
A randomized control trial34 consisted of 633 women aged 18-40 years who were contemplating pregnancy within 1 year, were provided with preconception counseling (PCC). A questionnaire was sent to all women 2 months after delivery, enquiring about their pregnancy outcome and about their behavior before and during pregnancy. The authors reported that among the 211 women who received PCC, more women were initiated to folic acid supplements prior to pregnancy and reduced their alcohol consumption 3 months before pregnancy. The main limitation of this study is the small number of women attending PCC. Guelinckx et al.35evaluated the effects of an educational intervention program in Belgium among 115 obese pregnant women recruited before 15th week of gestation. The results indicated that nutrition counseling during pregnancy could improve dietary intake in terms of decreased saturated fat intake, increased protein, calcium and vegetable intake. The limitation in this study is that since the study population was not nutritionally vulnerable, it was inappropriate to consider the pregnancy outcomes. Although both studies had limitations, the major strength of these two studies is that both considered women before pregnancy and indeed found positive effects of preconception counseling on diet and other lifestyle behavior.
Steptoe et al.36 measured the effect of brief behavioral counseling in general practice on patients’ consumption of fruits and vegetables in adults from a low-income setting. Post intervention, fruit and vegetable intake increased by 1.5 and 0.9 portions per day in the behavioral and nutrition groups. An increase in the number (42% and 27%) of participants eating five or more portions a day was reported in both groups. Other intervention studies also reported an increased in the intake of fruits and vegetables after a nutrition education program among women of reproductive age.37-39The advantage of the studies by Steptoe et al.36 and Heneman et al.37 is that they demonstrated the effectiveness of the NE among low-income groups. Campbell et al.40 evaluated the effect of a tailored nutrition education CD-ROM program consisted of a targeted video soap opera, dietary assessment, and individually designed dietary feedback and strategies for change for participants in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC). The authors reported that no differential effect for dietary intake variables. Although the sample size of these studies were more or less the same, the results observed differed. The disparity observed between the four studies and that by Campbell et al.40 could be due to several limitations such as (i) the use of two different methods of data collection, (ii) use of a brief food frequency only for dietary assessment and also due to (iii) inability to evaluate the influence of other sources of nutrition education participants could have obtained during the study phase.
Multiple health behavior interventions
Previous studies assessed the combined effect of a physical activity and nutrition intervention among women of reproductive age. Two of the interventions reported a positive effect on dietary intake (e.g. replacing high fat foods with low fat alternatives such as fruits and vegetables) and physical activity level (PAL) 41,42 while the other intervention reported favorable trends in the reduction of excessive weight gain and PAL43 in the short term (4–12 months). In a prospective cohort study, Inskip et al.17 reported that out of 238 women who became pregnant during the first three months of the study period, those who intended a pregnancy were to some extent more inclined to follow recommendations as compared to those not planning a pregnancy. Approximately the same number of women from both groups was found to take fruits, vegetables and folic acid as recommended and also had reduced alcohol intake. Pregnant women were also likely to undertake strenuous exercise in the past three months.
Furthermore, Liu et al.44 demonstrated the positive influence of changes in nutrition and health knowledge, as well as enhancement of dietary behaviors in general, for example intake of fruits, vegetables, soybean and soybean products among women in intervention groups. Sweet and Fortier33 suggested that in multiple health behavior interventions, changing a particular behavior could encourage changes in other health behavior, thus further benefiting the use of multiple health behavior interventions.
Physical Activity interventions
Earlier studies investigated the influence of interventions to enhance physical activity level among women of reproductive age. Albright et al.45and Fahrenwald et al.46carried out the physical activity intervention among mothers for 8-weeks and reported an increased level of PA post the intervention. Cramp and Brawley47and Miller et al.48alongside with encouraging PA, they included ways of overcoming barriers to promote PA in the intervention. They demonstrated that the groups, who received exercise treatment in addition to the behavioral intervention, had higher PAL following the intervention. It can thus be concluded that while only exercise programs resulted in improvements to exercise participation, the inclusion of behavioral intervention produced greater improvement in overall physical activity, barrier efficacy and proximal outcome expectations. Findings from major interventions studies among women to assess effect of health intervention programs are summarized in Table 2.
Table 2 . Findings from interventions studies among women to assess effect of health intervention programmes .
| Author, Year | Location, Study population (n) | Design and measures | Outcomes |
| Nutrition interventions | |||
| Elsinga et al. 200834 | Netherlands N = 633 (women contemplating pregnancy within 1 year) Age:18-40 |
- Randomized control trial - Knowledge on pregnancy-related risk factors and preventive measures and change in their behavior before and during pregnancy |
-Knowledge of women who received preconception counseling (PCC) exceeded that of women who did not. -After PCC, significantly more women started using folic acid before pregnancy and reduced alcohol use during the first 3 months of pregnancy |
| Guelinckx et al. 201035 | Belgium N = 115 (pregnant women) |
- Randomized control trial - Dietary habits, physical activity, gestational weight gain |
-Nutrition counseling was associated with improvements in dietary intake specifically decreased saturated fat intake, increased protein, calcium and vegetable intake |
| Steptoe et al. 200336 | London, England N = 271 (61% females aged 18-70) |
- Pre-post, parallel group randomized controlled trial -Self-reported number of portions of fruits & vegetables eaten per day |
-Consumption of fruits and vegetables increased from baseline to 12 month. -The proportion of participants eating 5 or more portions/day increased by 42% and 27% in both groups. |
| Heneman et al. 200537 | California, USA N = 38 (Females aged 20-45) |
-Pre-post, randomized participants into three-group -parallel arm study -Diet change |
-The contract group had significantly increased acceptance of vegetable consumption. -They also significantly increased fruit consumption. |
| Richards et al. 200639 | South Dakota, USA N= 437 (75% females aged 18-24) |
-Pre-post, randomized control intervention -Daily consumption of fruits and vegetables at baseline and post intervention |
-Fruits & vegetables consumption increased for intervention group. -The intervention self-efficacy scores for both FV were significantly greater. |
| Ha and Caine-Bish, 200938 | Kent, Ohio, United States N = 80 (College students aged 18-24 years, 88% females) |
-3-day food records were collected, verified, and analyzed before and after the intervention. -Consumption of: total vegetable, fresh vegetable, starchy vegetable, French fries, vegetable juice, total fruit, fresh fruit, canned fruit, and fruit juice. |
-Participants significantly increased consumption of total fruits and vegetables (P<.005). -Intake of French fries decreased significantly (P<.05). |
| Campbell et al. 200440 | North Carolina N = 307 (20% were pregnant and 50% were minorities e.g. African American and other) |
-Pre- post, randomly assigned to intervention and control -Total fat and fruit and vegetable intake, knowledge -of low-fat and infant feeding choices, self-efficacy, and stages of change. |
-Intervention group members increased self-efficacy (P< .01) and scored significantly higher (P< .05) on both -low-fat and infant feeding knowledge compared with controls. -No differential effect was observed for dietary intake variables. |
| Multiple health behavior interventions | |||
| Lombard et al. 200941 | Melbourne, Australia N = 250 (mothers of young children) |
-Randomly assigned to intervention and control -Self-reported weight (both groups), measured -weight (intervention only), self-efficacy, dietary intake and physical activity |
-Both groups decreased weight; more women lost or maintained weight in the intervention group. -Increased physical activity (P> 0.05); both groups reported replacing high fat foods with low fat alternatives and self-efficacy deteriorated in the comparison group only. |
| Lombard et al. 201042 | urban Australia N = 250 (mothers of young children) |
-Cluster randomized controlled trial -Weight change and difference in weight change between the intervention group and the control group at 12 months. -Secondary outcomes were changes in serum concentrations of fasting lipids and glucose, and -changes in dietary behaviors, physical activity, and self-management behaviors. |
Women in the control group gained weight over the 12 month Difference in the intervention group compared with the control group for total cholesterol concentration (?0.35 mmol/l, ?0.70 to ?0.001), self-management behaviors (diet score 0.18, 0.13 to 0.33; physical activity score 0.24, 0.05 to 0.43). |
| Hui et al. 200643 | Winnipeg, Manitoba, Canada N = 52 (pregnant women) |
-Randomized controlled trial -Physical activity and food intake |
Physical activity levels in intervention group were greater than those in control group (P<0.01). |
| Inskip et al. 200917 | Southampton, United Kingdom N = 12 445 (non-pregnant women aged 20-34) |
-Prospective cohort study -Folic acid supplement intake, alcohol consumption, smoking, diet, and physical activity before pregnancy |
238 who became pregnant within 3 months of the study were only marginally more likely to comply with recommendations for those planning a pregnancy than those who did not become pregnant in this period. Women in both groups were equally likely to have recommended fruits, vegetables, and folic acid intake and drank four or fewer units of alcohol a week. |
| Liu et al. 2009 44 | Hubei, China N= 302 |
-randomized controlled trial nutrition and health knowledge, dietary behavior, health behavior and health problems during the postpartum period |
Women in the intervention groups exhibited significantly greater improvement in overall dietary behaviors such as consumption of fruits, vegetables, soybean and soybean products as well as nutrition and health knowledge than those in the control groups. The incidence of constipation, leg cramp or joint pain and prolonged lochia rubra was significantly lower in the intervention groups as compared with the control groups. |
| PA interventions | |||
| Albright et al. 200945 | N = 20 (Sedentary women) |
-Pretest-posttest design -Minutes per week of moderate and vigorous leisure time physical activity |
Significant increase in physical activity post intervention |
| Cramp and Brawley, 200647 | N = 57 (post natal women) | -Randomized, two-arm intervention design -Physical activity, barrier efficacy, and proximal outcome expectations |
Participants receiving group-mediated cognitive behavioral intervention increased their initial level of barrier efficacy and outcome expectations while participants receiving standard exercise treatment decreased (P< 0.05). |
| Fahrenwald et al. 200446 | United States N = 44 (low-income mothers enrolled WIC program) |
-Pre- post, randomly assigned to intervention and control -Stage of PA behavior change, PA behavior, selected TTM constructs, social support. |
The experimental group had greater PA behavior experimental group had greater improvements in all TTM constructs and social support, P<.001 |
| Miller et al. 200248 | N = 554 (mothers of preschool-aged children) | -Randomized controlled intervention trial -Adequate physical activity (PA), self-efficacy (SE) and partner support (PS) |
Women in intervention group were more likely to meet guidelines for PA than controls |
Interventions at community level
Community responsibility, specifically, continuous care between the home and different set-ups is another important consideration in the endeavor of optimizing health of women of reproductive age.49According to Barry et al.50 there is pertinent evidence that health promotion programmes consisting of behavior change strategies, home visits, and participatory campaigns can be helpful in ensuring the health of mothers during the reproductive age. Schiffman et al.51further postulate the importance of a Family-Community Care involves services which encompasses both the family and community to harmonise with the social and cultural milieu of particular communities.
This encourages the adoption of healthy lifestyle practices at family as well as community level. A study demonstrated the effectiveness of a nutrition education programme among pregnant women in Iran.52 For instance, a major increase in the nutritional knowledge level of pregnant women was noted with a rise from 3% to 31% post the nutritional education intervention, irrespective of maternal age and educational attainment.52 In line with this, a recent study shows the effectiveness of community-based efforts, in particular gathering of mothers which were intended to promote healthy behaviors, are efficient and can be extrapolated to a larger population.53 On the other hand, Perumal et al.54reported that nutrition knowledge, attitudes, and dietary score were not significantly different between women attending and not-attending antenatal care clinic attending. However, they found that regular visits to antenatal care clinics were notably related with improved health knowledge among mothers.
Conclusion
Adequate nutrition and healthy lifestyle behaviors such as physical activity and alcohol consumption are to be given significant consideration among women of reproductive age to optimize the health of their babies as well as their own health. There is strong evidence from published studies, which demonstrate that nutrition, and physical activity interventions have had a positive impact on the behaviors of women of reproductive age resulting in optimistic health outcomes. It has been found that multiple health intervention strategies have been more successful in modifying health behaviors of women of reproductive age. As demonstrated by the social ecological model, several factors may obstruct women of reproductive age in their endeavour to practice healthy behaviours. Thus, it is important that all family members should be equally involved in health promotion programmes as a support for improved dietary and physical activity practices for women. Nutrition education conducted at community level, for instance in hospitals, and area health centres contribute to positive health behavior modifications. Thus, health professionals should aim at multiple health interventions at community level to have better outcomes. Political support for a broad-based approach to nutrition should further be considered to encourage the practical application of research.
Acknowledgements
The Dept. of Health Sciences (Faculty of Science, University of Mauritius) is acknowledged for its support.
Conflict of interests
The authors declare that there is no conflict of interests.
Citation: Dunneram Y, Jeewon R. Healthy Diet and Nutrition Education Program among Women of Reproductive Age: A Necessity of Multilevel Strategies or Community Responsibility. Health Promot Perspect 2015; 5(2): 116-127.
References
- 1.Atrash HK, Johnson K, Adams M, Cordero JF, Howse J. Preconception care for improving perinatal outcomes: the time to act. Matern Child Health J . 2006;10:3–11. doi: 10.1007/s10995-006-0100-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barfield WD, Warner L. Preventing chronic disease in women of reproductive age: opportunities for health promotion and preventive services. Prev Chronic Dis. 2012;9:1–3. doi: 10.5888/pcd9.110281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bartley KA, Underwood BA, Deckelbaum RJ. A life cycle micronutrient perspective for women’s health. Am J Clin Nutr. 2005;81:1188S–1193S. doi: 10.1093/ajcn/81.5.1188. [DOI] [PubMed] [Google Scholar]
- 4.Moos MK, Dunlop AL, Jack BW, Nelson L, Coonrod DV, Long R. et al. Healthier women, healthier reproductive outcomes: recommendations for the routine care of all women of reproductive age. Am J Obstet Gynecol. 2008;199:S280–S289. doi: 10.1016/j.ajog.2008.08.060. [DOI] [PubMed] [Google Scholar]
- 5.Bhargava A, Hays J. Behavioral variables and education are predictors of dietary change in the Women’s Health Trial: feasibility study in minority populations. Prev Med. 2004;38:442–451. doi: 10.1016/j.ypmed.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Dean SV, Lassi ZS, Imam AM, Bhutta ZA. Preconception care: nutritional risks and interventions. Reprod Health. 2014;11:S3. doi: 10.1186/1742-4755-11-S3-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rao S. Potential of community based approach for prevention of anaemia among women of childbearing age from rural India. Journal of Food and Nutrition Sciences. 2014;2:270–276. doi: 10.11648/j.jfns.201402-06.15. [DOI] [Google Scholar]
- 8.Mwangome M, Prentice A, Plugge E, Nweneka C. Determinants of appropriate child health and nutrition practices among women in rural Gambia. J Health Popul Nutr. 2010;28:167–172. doi: 10.3329/jh-pn.v28i2.4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kulasekaran RA. Influence of mothers’ chronic energy deficiency on the nutritional status of preschool children in Empowered Action Group states in India. Int J Nutr Pharmacol Neurol Dis. 2012;2:198–209. doi: 10.4103/2231-0738.99471. [DOI] [Google Scholar]
- 10.Mostafa Kamal SM, Md Aynul I. Socio-economic correlates of malnutrition among married women in Bangladesh. Mal J Nutr. 2010;16:349–359. [PubMed] [Google Scholar]
- 11.Thangaratinam S, Rogozinska E, Jolly K, Glinkowski S, Roseboom T, Tomlinson JW. et al. Effects of interventions in pregnancy on maternal weight and obstetric outcomes: meta-analysis of randomized evidence. BMJ. 2012;344:1–15. doi: 10.1136/bmj.e2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dennedy MC, Dunne F. The maternal and fetal impacts of obesity and gestational diabetes on pregnancy outcome. Best Pract Res Clin Endocrinol Metab. 2010;24:573–589. doi: 10.1016/j.beem.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 13.Paden MM, Avery DM. Preconception counseling to prevent the complications of obesity during pregnancy. Am J Clin Med. 2012;9:30–35. [Google Scholar]
- 14.Tanentsapf I, Heitmann BL, Adegboye ARA. Systematic review of clinical trials on dietary interventions to prevent excessive weight gain during pregnancy among normal weight, overweight and obese women. BMC Pregnancy Childbirth. 2011;11:81. doi: 10.1186/1471-2393-11-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 16. World Health Organisation . The world health report, Chapter 4: Childhood and maternal undernutrition. Geneva: World Health Organization; 2013. [Cited 2013 Jan 13]. Available from: http://www.who.int/whr/2002/chapter4/en/index3.html.
- 17. Blössner M, De Onis M. Malnutrition: Quantifying the health impact at national and local levels. Geneva: World Health Organization; 2005. WHO Environmental Burden of Disease Series, No. 12. [cited 2013 Jan 13]. Available from: http://whqlibdoc.wh-o.int/publications/2005/9241591870.pdf.
- 18.Inskip HM, Crozier SR, Godfrey KM, Borland SE, Cooper C, Robinson SM. Women’s compliance with nutrition and lifestyle recommendations before pregnancy: general population cohort study. BMJ. 2009;338:b481. doi: 10.1136/bmj.b481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Galtier F, Raingeard I, Renard E, Boulot P, Bringer J. Optimizing the outcome of pregnancy in obese women: from pregestational to long-term management. Diabetes Metab. 2008;34:19–25. doi: 10.1016/j.diabet.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Bain LE, Awah PK, Geraldine N, Kindong NP, Sigal Y, Bernard N. et al. Malnutrition in Sub–Saharan Africa: burden, causes and prospects. Pan Afr Med J. 2013;15:120. doi: 10.11604/pamj.2013.15.120.2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Becquey E, Martin-Prevel Y. Micronutrient adequacy of women’s diet in urban Burkina Faso is low. J Nutr. 2010;140:2079S–2085S. doi: 10.3945/jn.110.123356. [DOI] [PubMed] [Google Scholar]
- 22. Brown LS. Nutrition requirements during pregnancy. In: Sharlin J, Edelstein S, editors. Essentials of life cycle nutrition. United States of America: Jones and Bartlett Publishers; 2011.
- 23.Berghella V, Buchanan E, Pereira L, Baxter JK. Preconception care. Obstet Gynecol Surv. 2010;65:119–131. doi: 10.1097/OGX.0b013e3181d0c358. [DOI] [PubMed] [Google Scholar]
- 24. Lum KJ, Sundaram R, Buck Louis GM. Women’s lifestyle behaviors while trying to become pregnant: evidence supporting preconception guidance. Am J Obstet Gynecol 2011;205:203.e1-7. doi: 10.1016/j.ajog.2011.04.030. [DOI] [PMC free article] [PubMed]
- 25.Tough S, Tofflemire K, Clarke M, Newburn-Cook C. Do women change their drinking behaviors while trying to conceive? an opportunity for preconception counseling. Clin Med Res. 2006;4:97–105. doi: 10.3121/cmr.4.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Green-Raleigh K, Lawrence JM, Chen H, Devine O, Prue C. Pregnancy planning status and health behaviors among non pregnant women in a California managed health care organization. Perspect Sex Reprod Health. 2005;37:179–183. doi: 10.1111/j.1931-2393.2005.tb00242.x. [DOI] [PubMed] [Google Scholar]
- 27.Contento IR. Nutrition education: linking research, theory, and practice. Asia Pac J Clin Nutr. 2008;17:176–179. [PubMed] [Google Scholar]
- 28.Everette M. A review of nutrition education: before, between and beyond pregnancy. Curr Womens Health Rev. 2009;5:193–200. doi: 10.2174/1573404097900-69925. [DOI] [Google Scholar]
- 29.Curtis M, Abelman S, Schulkin J, Williams JL, Fassett EM. Do we practice what we preach? A review of actual clinical practice with regards to preconception care guidelines. Matern Child Health J. 2006;10:S53–S58. doi: 10.1007/s10995-006-0112-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baheiraei A, Mirghafourvand M, Mohammadi E, Mohammad-Alizadeh Charandabi S. The experiences of women of reproductive age regarding health-promoting behaviors: a qualitative study. BMC Public Health. 2012;12:573. doi: 10.1186/1471-2458-12-573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bastani F. The effect of education on nutrition behavioral intention and self-efficacy in women. Health Scope. 2012;1:12–17. doi: 10.5812/jhs.4520. [DOI] [Google Scholar]
- 32.Moos MK. From Concept to Practice: Reflections on the Preconception Health Agenda. J Womens Health (Larchmt) 2010;19:561–567. doi: 10.1089/jwh.2009.1411. [DOI] [PubMed] [Google Scholar]
- 33.Sweet SN, Fortier MS. Improving physical activity and dietary behaviors with single or multiple health behavior interventions? a synthesis of meta-analyses and reviews. Int J Environ Res Public Health. 2010;7:1720–1743. doi: 10.3390/ijerph7041720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elsinga J, de Jong-Potjer LC , van der Pal-de Bruin KM, le Cessie S, Assendelft WJ, Buitendijk SE. The effect of preconception counseling on lifestyle and other behavior before and during pregnancy. Womens Health Issues. 2008;18:117–125. doi: 10.1016/j.whi.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 35.Guelinckx I, Devlieger R, Mullie P, Vansant G. Effect of lifestyle intervention on dietary habits, physical activity, and gestational weight gain in obese pregnant women: a randomized controlled trial. Am J Clin Nutr. 2010;91:373–380. doi: 10.3945/ajcn.200-9.28166. [DOI] [PubMed] [Google Scholar]
- 36.Steptoe A, Perkins-Porras L, McKay C, Rink E, Hilton S, Cappuccio FP. Behavioral counseling to increase consumption of fruit and vegetables in low income adults: randomized trial. BMJ. 2003;326:855. doi: 10.1136/bmj.326.7394.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heneman K, Block-Joy A, Zidenberg-Cherr S, Donohue S, Garcia L, Martin A. et al. A "contract for change" increases produce consumption in low-income women: a pilot study. J Am Diet Assoc. 2005;105:1793–1796. doi: 10.1016/j.jada.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 38.Ha EJ, Caine-Bish N. Effect of nutrition intervention using a general nutrition course for promoting fruit and vegetable consumption among college students. J Nutr Educ Behav. 2009;41:103–109. doi: 10.1016/j.jneb.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 39.Richards A, Kattelmann KK, Ren C. Motivating 18- to 24-year-olds to increase their fruit and vegetable consumption. J Am Diet Assoc. 2006;106:1405–1411. doi: 10.1016/j.jada.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 40.Campbell MK, Carbone E, Honess-Morreale L, Heisler-Mackinnon J, Demissie S, Farrell D. Randomized trial of a tailored nutrition education CD-ROM program for women receiving food assistance. J Nutr Educ Behav. 2004;36:58–66. doi: 10.1016/s1499-4046(06)60134-6. [DOI] [PubMed] [Google Scholar]
- 41.Lombard CB, Deeks AA, Ball K, Jolley D, Teede HJ. Weight, physical activity and dietary behavior change in young mothers: short term results of the HeLP-her cluster randomized controlled trial. Nutr J. 2009;8:17. doi: 10.1186/1475-2891-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lombard C, Deeks A, Jolley D, Ball K, Teede H. A low intensity, community based lifestyle programme to prevent weight gain in women with young children: cluster randomized controlled trial. BMJ. 2010;341:c3215. doi: 10.1136/bmj.c3215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hui AL, Ludwig SM, Gardiner P, Sevenhuysen G, Murray R, Morris M. et al. Community-based exercise and dietary intervention during pregnancy: a pilot study. Can J Diabetes. 2006;30:169–175. doi: 10.1016/s1499-2671(06)02010-7. [DOI] [Google Scholar]
- 44.Liu N, Mao L, Sun X, Liu L, Yao P, Chen B. The effect of health and nutrition education intervention on women's postpartum beliefs and practices: a randomized controlled trial. BMC Public Health. 2009;9:45. doi: 10.1186/1471-2458-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Albright CL, Maddock JE, Nigg CR. Increasing physical activity in postpartum multiethnic women in Hawaii: results from a pilot study. BMC Womens Health. 2009;9:4. doi: 10.1186/1472-6874-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fahrenwald NL, Atwood JR, Walker SN, Johnson DR, Berg K. A randomized pilot test of "Moms on the Move": a physical activity intervention for WIC mothers. Ann Behav Med. 2004;27:82–90. doi: 10.1207/s15324796abm2702_2. [DOI] [PubMed] [Google Scholar]
- 47.Cramp AG, Brawley LR. Moms in motion: a group-mediated cognitive-behavioral physical activity intervention. Int J Behav Nutr Phys Act. 2006;3:23. doi: 10.1186/1479-5868-3-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miller YD, Trost SG, Brown WJ. Mediators of physical activity behavior change among women with young children. Am J Prev Med. 2002;23:98–103. doi: 10.1016/S0749-3797(02)00484-1. [DOI] [PubMed] [Google Scholar]
- 49.Bahl R, Qazi S, Darmstadt GL, Martines J. Why is continuum of care from home to health facilities essential to improve perinatal survival? Semin Perinatol. 2010;34:477–485. doi: 10.1053/j.semperi.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 50.Barry D, Frew AH, Mohammed H, Desta BF, Tadesse L, Aklilu Y. et al. The effect of community maternal and newborn health family meetings on type of birth attendant and completeness of maternal and newborn care received during birth and the early postnatal period in rural Ethiopia. J Midwifery Womens Health. 2014;59:S44–S54. doi: 10.1111/jmw-h.12171. [DOI] [PubMed] [Google Scholar]
- 51.Schiffman J, Darmstadt GL, Agarwal S, Baqui AH. Community-based intervention packages for improving perinatal health in developing countries: a review of the evidence. Semin Perinatol. 2010;34:462–476. doi: 10.1053/j.semperi.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 52.Fallah F, Pourabbas A, Delpisheh A, Veisani Y, Shadnoush M. Effects of nutrition education on levels of nutritional awareness of pregnant women in western Iran. Int J Endocrinol Metab. 2013;11:175–178. doi: 10.5812/ijem.9122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Acharya A, Lalwani T, Dutta R, Rajaratnam JK, Ruducha J, Varkey LC. et al. Evaluating a large-scale community-based intervention to improve pregnancy and newborn health among the rural poor in India. Am J Public Health. 2015;105:144–152. doi: 10.2105/ajph.2014.302092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Perumal N, Cole DC, Ouédraogo HZ, Sindi K, Loechl C, Low J. et al. Health and nutrition knowledge, attitudes and practices of pregnant women attending and not-attending ANC clinics in Western Kenya: a cross-sectional analysis. BMC Pregnancy Childbirth. 2013;13:146. doi: 10.1186/1471-2393-13-146. [DOI] [PMC free article] [PubMed] [Google Scholar]