Abstract
Several mechanisms facilitate the progression of hormone-sensitive prostate cancer to castration-resistant prostate cancer (CRPC). At present, the approved chemotherapies for CRPC include systemic drugs (docetaxel and cabazitaxel) and agents that target androgen signaling, including enzalutamide and abiraterone. While up to 30% of patients have primary resistance to these treatments, each of these drugs confers a significant survival benefit for many. Over time, however, all patients inevitably develop resistance to treatment and their disease will continue to progress. Several key mechanisms have been identified that give rise to drug resistance. Expression of constitutively active variants of the androgen receptor, such as AR-V7, intracrine androgens and overexpression of androgen synthesis enzymes like AKR1C3, and increased drug efflux through ABCB1 are just some of the many discovered mechanisms of drug resistance. Treatment strategies are being developed to target these pathways and reintroduce drug sensitivity. Niclosamide has been discovered to reduce AR-V7 activity and synergized to enzalutamide. Indomethacin has been explored to inhibit AKR1C3 activity and showed to be able to reverse resistance to enzalutamide. ABCB1 transport activity can be mitigated by the phytochemical apigenin and by antiandrogens such as bicalutamide, with each improving cellular response to chemotherapeutics. By better understanding the mechanisms by which drug resistance develops improved treatment strategies will be made possible. Herein, we review the existing knowledge of CRPC therapies and resistance mechanisms as well as methods that have been identified which may improve drug sensitivity.
Keywords: Drug resistance, castration resistant, prostate cancer, treatment strategies
Introduction
Prostate cancer is the most commonly diagnosed cancer and second leading cause of cancer related deaths in men; attributing to over 29,000 deaths in 2014 in the United States alone [1,2]. Additionally, 14% of all newly diagnosed cancers in the United Sates are prostate cancer and 15% of men will be diagnosed with this disease in their lifetime [3]. Initial treatments for prostate cancer focus on the use of androgen deprivation therapies (ADT) to reduce levels of circulating androgens in order to stop tumor growth. ADT is achieved either surgically via bilateral orchiectomy to inhibit androgen synthesis by the testes or with medical castration using drugs including gonadotropin-releasing hormone (GnRH) agonists, GnRH antagonists, and anti-androgens to reduce circulating levels of androgen and reduce androgen receptor (AR) activation. Unfortunately, after 2-3 years of ADT, patient’s often progress to castration-resistant prostate cancer (CRPC) at which point therapeutic choices are limited but continuously being improved upon [4].
CRPC, previously hormone-resistant prostate cancer, is defined as progression of disease in the presence of castrate levels of circulating testosterone [5,6]. It is hallmarked by hyper-activation and/or overexpression of the AR resulting in the transcription of downstream target genes and tumor progression despite only castrate levels of androgen being present in the patient. Dysregulated mechanisms that contribute to the development of CRPC from hormone-sensitive prostate cancer have been extensively investigated and can be broken up into five general categories: AR amplification and mutation, AR co-activator and co-repressor modifications, aberrant activation and/or post-translational modification, altered steroidogenesis, and AR splice variants. Each of these five broad classifications have the end result of increased AR activation whether due to increasing the amount of androgen, enhancing the response to existing androgen, sensitizing the AR to non-classical ligands, allowing the AR to activate in the absence of ligand, or a myriad of other mechanisms [7-11].
Chemotherapeutics currently available for the treatment of CRPC include systemic therapies, such as docetaxel and cabazitaxel, as well as drugs like enzalutamide and abiraterone which target AR activation either directly or indirectly (Figure 1). Sadly, primary resistance to these treatments is not uncommon. Up to one third of patients receiving abiraterone and one fourth of patients receiving enzalutamide fail to respond to initial treatment with these drugs [12,13]. Even patients who initially benefit from treatment develop drug resistance within 24 months of initial exposure.
Figure 1.
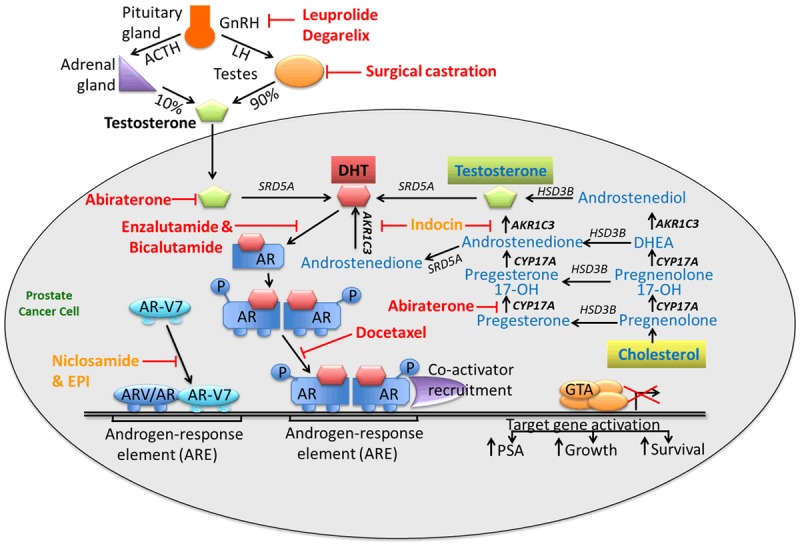
An overview of approved and experimental treatment strategies for CRPC targeting the androgen axis. Currently approved therapies are written in red while experimental therapies are in orange.
The aim of this review is to outline current methodologies used in the treatment of CRPC with a focus on mechanisms that become dysregulated as prostate cancer patients develop resistance to these chemotherapeutics. Developmental strategies showing promise for overcoming acquired resistance will be highlighted.
Docetaxel and cabazitaxel
Until recently, the primary treatment for CRPC has been docetaxel since it was approved in 2004 however newer drugs such as enzalutamide and abiraterone have overtaken its use as the first-line treatment. Data from the CHAARTED trial, however, demonstrate that docetaxel as an initial treatment for hormone-naïve prostate cancer in conjunction with ADT in patients with high volume or visceral metastases provided a 17-month survival advantage over androgen ablation [14].
Docetaxel is an anti-mitotic chemotherapeutic used for the treatment of several other varieties of cancer including cancers of the breast, lung, and stomach. In the treatment of prostate cancer, docetaxel is often used in combination with prednisone and functions by binding to free tubulin within cells promoting the formation of stable microtubules preventing depolymerization which results in inhibition of mitosis and consequent induction of apoptosis [15-17]. Furthermore, docetaxel has been shown to reduce AR expression in CRPC cells [18].
Cabazitaxel is a newer FDA approved taxane used for the treatment of CRPC in patients who have failed docetaxel chemotherapy. Compared to mitoxantrone, the TROPIC clinical trial observed cabazitaxel to have a 2.4 month survival benefit in patients with metastatic CRPC whose disease had progressed on docetaxel [19]. While both taxanes function through tubulin binding, cabazitaxel has unique mechanisms of action and therefor resistance compared to docetaxel [20]. Unlike docetaxel, cabazitaxel has low affinity for the MDRP ABCB1, a fact that led to its selection as a chemotherapeutic [21,22].
Docetaxel resistance
Resistance to docetaxel treatment is well characterized and arises due to a number of different mechanisms. Many of these mechanisms are related to aberrant regulation of molecules involved in cell survival and death. Overexpression or activation of signal transducers and activator of transcription (Stat) 1, Stat3, clusterin, heat shock proteins (HSP), and nuclear factor kappa B (NF-κB), among others, are associated with docetaxel resistance [23-28]. Furthermore, Vidal et al. observed that GATA2 upregulation and the resultant increase in IGF2 and activation of downstream targets promoted docetaxel resistance in murine models [29]. Conversely, reduced activity or expression of wild type p53 is linked to insensitivity to docetaxel [30].
Overexpression of inflammation associated molecules has also been demonstrated to cause resistance to docetaxel. Interleukin (IL) 6 enhances proliferation and inhibits apoptosis of prostate cancer cells. Secretion of this cytokine is inversely correlated to docetaxel response in CRPC patients, and increased IL-6 is due in part to increased levels of NF-κB [24,31]. Similarly, increased expression levels of IL-8, chemokine ligand 2 (CCL2), transforming growth factor-β1 (TGF-β1) and macrophage inhibitory cytokine-1 (MIC-1) have all been tied to promoting docetaxel resistance [32-36].
Increased expression of β-tubulin isoforms has also been linked to docetaxel resistance. In particular, taxanes have reduced efficiency for binding to the class III β-tubulin isoform [37,38]. Studies have also found increased expression of class IV β-tubulin and mutations to class 1 β-tubulin causing impaired polymerization in docetaxel resistant cells [39,40].
Another class of molecules dysregulated in docetaxel resistance is multidrug resistance proteins (MDRP). MDRP, such as P-glycoprotein, function as pumps to excrete drugs, including docetaxel, into the extracellular fluid. This reduces the drugs ability to target cells and leads to drug resistance. In vitro analyses of docetaxel-resistant cells have revealed that overexpression and phosphorylation of breast cancer resistance protein (BCRP) induces docetaxel resistance [41]. Additionally, expression of P-glycoprotein (P-gp, MDR1 or ABCB1) is significantly increased in docetaxel-resistant compared to docetaxel-sensitive DU145, CWR22RV1 and C4-2B parental cell lines [27,42].
Thadani-Mulero et al. observed that androgen receptor splice variants (which will be discussed in further detail later) can influence sensitivity to docetaxel. They found that the AR variant ARV-567 was sensitive to microtubule stabilization induced by taxanes whereas AR-V7 was unaffected. Furthermore, AR-V7 expressing tumor xenografts were resistant to docetaxel therapy while ARV-567 expressing xenografts where highly sensitive to docetaxel [43].
Overcoming docetaxel resistance
A number of experimental strategies have been explored for reintroducing docetaxel sensitivity. Unfortunately, while many methods have been effective in in vitro and in vivo models, clinical data to support these findings are either lacking or have shown little efficacy in later phase prostate cancer trials. One line of attack is to mediate expression of up-regulated pro-survival and pro-inflammatory molecules found to be associated with increased resistance. Inhibition of NF-κB with BAY 11-7082 in docetaxel resistant cell lines resulted in re-sensitization of these cells to docetaxel treatment [27]. Niu et al. found that the natural anti-inflammatory compound Marchantin M, found in liverwort plants, was capable of reducing IL-6 and TNFα expression and inactivating NF-κB and resulted in increased docetaxel sensitivity in prostate cancer cells [44]. Furthermore, inhibition of IGF1R expression, a molecule involved in the GATA2-IGF2 signaling axis, using the selective IGF1R/INSR inhibitor OSI-906 was observed to improve both docetaxel and cabazitaxel sensitivity in resistant cell lines [29].
Targeting ABCB1 efflux pathways and β-tubulin isoforms are two other methods researchers have investigated for resensitizing cells to docetaxel. To this effect, phase I and II clinical trials have investigated the efficacy for using MDRP inhibiting drugs, such as elacridar, in combination with chemotherapy. While phase I trials showed promise, only minimal clinical activity was observed in phase II trials [45,46]. Interestingly, Zhu et al. observed that treatment of docetaxel resistant C4-2B cells with the dietary flavone apigenin overcomes ABCB1 mediated docetaxel resistance and resensitizes cells to drug treatment by inhibiting ABCB1 expression and likely reducing drug efflux [42]. ABCB1 efflux activity was also found to be inhibited by the anti-androgens enzalutamide and bicalutamide. Co-treatment with bicalutamide and docetaxel in both AR-positive and AR-negative docetaxel resistant mouse xenograft models was observed to significantly reduce tumor growth, suggesting that this effect is independent of AR status [47]. In regards to β-tubulin, the synthetic estrogen diethylstilbestrol has been demonstrated to suppress expression of β-tubulin isoform IVa and was observed to enhance tumor growth inhibition in combination with docetaxel in prostate cancer xenograft models [48]. Other groups have found that the N-terminal domain of the AR interacts with tubulin [49]. Targeting this domain with the small-molecule inhibitor EPI in conjunction with docetaxel therapy improved docetaxel effectiveness and reduced the number of cells displaying the epithelial-mesenchymal-transition (EMT) phenotype [50].
The use of nanoparticles for docetaxel delivery into cells has also been associated with improved docetaxel sensitivity. Several classes of nanoparticles have been developed, including liposomes, polymeric micelles, and nanoconjugates. The overarching goals of using these particles are to increase specificity for cancer cells, and improve drug retention and absorption while reducing non-specific toxicity in the patient. The use of nanoparticles has been found to reduce docetaxel efflux, either by avoiding efflux or by inhibiting increased expression of MDRP observed in the presence of free docetaxel [51-53]. Additionally, compared to free docetaxel, magneto-liposome bound docetaxel has been shown to inhibit activation of receptor tyrosine kinase pathways including EGFR, PI3K and Erk1/2 mediated MAP kinase, suggesting that the bound drug has improved anti-proliferative efficacy and renders cells more sensitive to treatment [54]. The majority of these studies, however, has been conducted in cancer models other than prostate cancer and serve as proof-of-principle for nanoparticle action in prostate cancer docetaxel resistance.
Cabazitaxel resistance
Due to its more recent emergence as a chemotherapeutic in CRPC, less is known about the development of cabazitaxel resistance compared to other drugs. Similarly to docetaxel, interfering with tubulin expression can influence cabazitaxel sensitivity. Specifically, Galletti et al. found that ETS-related gene (ERG) overexpression in prostate cells leads to cabazitaxel resistance both in vitro and in vivo [55]. They determined that cytoplasmic expression of ERG interacts with β-tubulin and tubulin dimers and that interruption of this interaction restores cabazitaxel sensitivity. Other studies investigating cabazitaxel resistance have found that CRPC tumors expressing low levels of retinoblastoma had improved cabazitaxel response [20].
Anti-androgens
Abiraterone acetate
Unlike docetaxel and cabazitaxel, abiraterone acetate (Zytiga) functions as an anti-androgen. Progression to CRPC includes the ability of prostate cancer cells to utilize the 5α-dione pathway to bypass testosterone in the steroidogenesis pathway, leading to production of dihydrotestosterone (DHT). Despite this, CRPC cells still rely on adrenal androgens which get converted to androstenedione by 3βHSD in the prostate or adrenal gland. DHT is then formed from the androstenedione. Abiraterone works by preventing the formation of androgen precursors required for androgen production in prostate tumors. Specifically, abiraterone reduces circulating androgen levels by inhibiting CYP17A1. Inhibition of CYP17A1 blocks the conversion of pregnenolone to DHT resulting in significant loss of androgen production in peripheral tissues and loss of production of precursors needed for intratumoral androgen synthesis. Recent studies suggest that the potency of abiraterone is increased by conversion to the more active Δ4-abiraterone (D4A) and that this D4A is responsible in part for the clinical activity of abiraterone. In vivo and clinical data demonstrate the conversion of abiraterone to D4A and further show that D4A inhibits CYP17A1, 3βHSD and SRD5A. Additionally, D4A was shown to have improved inhibition of tumor xenograft growth compared to abiraterone [56].
In patients who had progressed after docetaxel therapy, the phase III trial COU-AA-301 demonstrated a 3.9 month survival benefit of abiraterone/prednisone over placebo/prednisone and the subsequent COU-AA-302 trial showed a 4.4 month survival benefit with abiraterone in chemotherapy-naive CRPC patients [12,57,58]. Unfortunately, one-third of all patients display primary resistance to abiraterone treatment, and all patients with initial response progressed by 15 months of abiraterone chemotherapy [12].
Abiraterone resistance
Resistance to abiraterone in patients is tied to re-activation of androgen synthesis in prostate cancer cells. Up-regulation of and mutations to enzymes involved in the steroidogenesis pathway are likely contributors to both CRPC progression and abiraterone resistance. Mostaghel et al. detected a 1.3-4.5 fold increase in enzymes involved in steroidogenesis in abiraterone treated LuCaP cell lines, including CYP17A1, AKR1C3, HSD17B3, and SDR5A2 [59]. Additionally, Chang et al. observed the 1245C mutation in HSD3B1 in abiraterone-resistant xenograft models [60]. IL-6 has also been identified as a mediator of increased expression of steroidogenic enzymes, including HSD3B2 and AKR1C3 [61]. AKR1C3 in particular is an important enzyme in the steroidogenesis pathway. Its activation contributes to CRPC drug resistance in patients treated with both abiraterone and enzalutamide and it has been suggested as a biomarker for assessing prostate cancer progression [62,63].
In addition to alterations in steroidogenesis, AR activation by ligands other than androgen may also play a role in abiraterone resistance. Glucocorticoids are often used to reduce side effects associated with abiraterone treatment, however this group of compounds has been demonstrated to activate mutated AR and instigate androgen-independent growth of prostate cancer cells [64]. Furthermore, androgen precursors have been found to accumulate with abiraterone treatment and some of these have been identified to bind mutated AR and instigate downstream signaling [65-67].
Enzalutamide
Similar to abiraterone, enzalutamide (Xtandi, ENZA, MDV-3100) also functions by reducing AR activity, albeit via a separate mechanism. Enzalutamide is a competitive inhibitor of ligand binding to the AR. Additionally, it inhibits AR translocation to the nucleus, co-activator recruitment, AR binding to DNA and activation of AR target genes [68]. Enzalutamide has greater affinity for the AR compared to earlier anti-androgens, such as bicalutamide and flutamide, and is subsequently more effective than its predecessors. Data from the AFFIRM trial demonstrated that enzalutamide treated CRPC patients who failed docetaxel treatment had nearly 5 months improved survival compared to placebo treated individuals [13]. Furthermore, the PREVAIL trial found the enzalutamide was also effective in pre-chemotherapy hormone-naïve prostate cancer patients [69]. Primary resistance to enzalutamide was observed in 25% of patients in the AFFIRM trial in whom progression occurred within 3 months of treatment and by 24 months, all patients had progressed in their disease despite enzalutamide therapy [70].
Enzalutamide resistance
As cells develop enzalutamide resistance, several key dysregulated mechanisms have been brought to light. Among these are alterations in steroidogenesis, glucose metabolism, and autophagy. Specifically, Liu et al. observed enzalutamide resistant prostate cancer cells had upregulated expression of androgen and its precursors including cholesterol, DHEA and progesterone. Additionally, this study found that genes involved in steroid biosynthesis where significantly over-expressed compared to enzalutamide-sensitive parental cells and that of these AKR1C3 proved to be of particular importance being as overexpression of this enzyme alone was sufficient to desensitize normally responsive cells to enzalutamide treatment [63].
Point mutations to the AR in the regions coding for the ligand binding domain are also implicated in enzalutamide resistance and it is estimated that 10-30% of CRPC patients have AR mutations [71]. Many of these mutations result in gain-of-function that increase coactivator improvement, alter ligand specificity and affinity. Interestingly, some of these mutations instigate ligand binding specificity to switch from agonist to antagonist activation. In particular, the Phe876Leu mutation in the AR has been associated with enzalutamide activating the AR however further study into this mutation is required to determine clinical significance [72,73].
Other molecular pathways have also been tied to enzalutamide resistance. Studies have determined that overexpression of p52 confers enzalutamide resistance and that this may be due in part to changes in glucose metabolism and expression of AR splice variants, which will be discussed shortly [74-76]. Others have observed that constitutive Stat3 activation due to IL-6 overexpression also induces insensitivity to enzalutamide [77].
AR splice variants
AR variants are truncated versions of the wild type AR and are often ligand-independent and constitutively active. AR variants may be generated by genome rearrangement and alternative splicing involving splicing factors such as hnRNPAs [78,79]. Generally, the C-terminal ligand-binding domain is the portion of the AR that is lost, however at least one variant is known to be truncated at the N-terminus resulting in a loss of the DNA binding domain [80-84]. The functional implications of AR variants are not yet fully understood, due in part to the lack of variant specific antibodies, and the role of these variants in CRPC is still being established. CWR22Rv1 cells in have nearly equal expression of full length AR and AR variants however most CRPC cell lines exhibit AR variant expression at some level. Additionally, bone metastases have higher AR variant expression compared to hormone-sensitive prostate cancer and AR variant expression is associated with poorer prognosis and the development of CRPC [85].
Both abiraterone and enzalutamide resistance have been tied to expression AR splice variants [76,86,87]. Among the identified splice variants, variant 7 (AR-V7) in particular has been implicated in drug resistance. Antonarakis et al. demonstrated that AR-V7 expression in patients treated with enzalutamide or abiraterone correlated to a significantly lower PSA response, shorter progression-free and overall survival compared to men without AR-V7 [88]. No changes in PSA response or progression-free survival were observed in patients treated with docetaxel regardless of AR-V7 expression suggesting that AR-V7 positive patients may be less susceptible to primary taxane drug resistance [89].
Overcoming abiraterone and enzalutamide resistance
Proposed methods for reintroducing sensitivity to abiraterone and enzalutamide include mediating dysregulated pathways and avoiding AR activation. Liu et al. found that inhibition of AKR1C3 enzymatic activity with indomethacin, a nonsteroidal anti-inflammatory drug, restored enzalutamide sensitivity in resistant prostate cancer cells and suggests that targeting intracrine androgens improves enzalutamide therapy [63]. In a separate study, enzalutamide sensitivity was also restored by inhibiting Stat3 activity using both siRNA and the Stat3 inhibitor AG490 resulting in increased apoptosis and inhibition of prostate cancer cell growth [77]. Others have demonstrated that cells can be resensitized to enzalutamide treatment when administered together with autophagy inhibitors: co-treatment of resistant CRPC cells with enzalutamide and either metformin or clomipramine had greater effect on reducing tumor volume compared to enzalutamide alone in murine models [90]. This has led to the approval for ongoing clinical trials investigating the combinatory effects of metformin with enzalutamide in CRPC patients.
Targeting AR variant expression is effective at reintroducing drug sensitivity and decreasing CRPC tumor growth. The FDA approved anti-helminthic drug, niclosamide, has been identified as an AR-V7 inhibitor via several mechanisms including increased AR-V7 protein degradation and reduced recruitment of AR-V7 to promoter regions of target genes resulting in reduced transcriptional activity. The AR-V7 degradation induced by niclosamide was determined to be the result of proteasome-dependent pathways due to the fact that MG132, a 26S proteasome inhibitor, reduced niclosamide-mediated inhibition of AR-V7 protein expression. Furthermore, enzalutamide resistant C4-2B cells expressing AR-V7 displayed a significant dose-dependent cytotoxic effect to niclosamide and when used in combination with enzalutamide had an additive response [91]. On top of its action as an AR-V7 inhibitor, niclosamide has been determined to improve enzalutamide sensitivity by modulating Stat3 activity by inhibiting its phosphorylation and reducing Stat3 target gene expression and abrogating recruitment of AR to the PSA promoter [92]. A recent study by Nadiminty et al. also tied AR-V7 downregulation to enzalutamide resensitization; by downregulating the splice factor hnRNPA1, they were able to decrease AR-V7 expression which sensitized resistant cells to enzalutamide treatment [79]. Another drug, ASC-J9, was found to degrade of both full length and AR-V3 by and associated with a decrease in CWR22Rv1 xenograft tumor growth [93].
While AR-V7 lacks the ligand binding domain, it and other constitutively active variants of the AR retain the N-terminus. Drugs have been developed that target this region of the AR, including EPI and derivatives thereof, and these too have been observed to inhibit prostate cancer cell growth. EPI is known to covalently bind the N-terminal domain of both AR and its variants and inhibit transcriptional activity. In vivo administration of EPI in prostate cancer xenograft models was observed to reduce tumor growth [94,95]. Niphatenones are another class of drugs that target the N-terminal domain of the AR. While niphatenone treatment was found to inhibit transactivation of AR and its variants, it was also observed to promote glutathione adduct formation and therefore may not be as viable for prostate cancer therapy as alternatives [96].
In addition to therapies aiming to improve the efficacy of existing drugs, novel agents are also being developed and investigated. Drug-seq technology screens genome-wide binding of potential therapeutic agents in various physiological conditions to identify probable therapeutic benefits. This technique identified SD-70, a synthetic chemical, as an inhibitor of prostate cancer translocation and it has further been determined to have in vitro cytotoxic effect on hormone-sensitive LNCaP cells, C42B and drug-resistant C42B cells, and in vivo efficacy in a CWR22Rv1 mouse xenograft model [97].
Cross resistance
With the increase in available chemotherapeutics, cross-resistance has become evident and limits the effective agents in patients who have failed prior therapy. Cross-resistance does not seem to be limited to one class of therapeutics but rather involves all approved CRPC treatments. In a study observing 310 patients with metastatic CRPC, Cheng et al. observed that prior exposure to abiraterone or docetaxel had reduced response to subsequent enzalutamide treatment. Additionally, PSA decline and PSA progression-free survival were diminished in patients previously treated with abiraterone or, to a lesser degree, docetaxel [98]. Other groups have observed similar trends in patients treated with docetaxel following abiraterone treatment and in those receiving enzalutamide post-docetaxel [99-101]. Interestingly, cabazitaxel appears to have less cross-resistance with AR targeted therapies than docetaxel [102,103]. This may be due to the innate differences in mechanisms of action between these two taxanes including the higher affinity of docetaxel for MDRP and the increased impact of cabazitaxel on cell cycle pathways and chromatin organization [20]. The reduction in docetaxel efficiency observed following AR targeted therapies suggests that taxane therapy may have a role in AR axis modulation. It is important to note, however, that this cross-resistance occurs regardless of the order in which docetaxel and AR targeted therapies are administered.
The emergence of cross-resistance in prostate cancer highlights the necessity for identifying molecules that inhibit resistance pathways that can be used as co-treatments with existing therapies to improve clinical outcome.
Conclusion
CRPC is a complex disease characterized by progression despite the availability of multiple currently approved therapies targeting different pathways. Chemo-resistance to these drugs develops over time through a multitude of dysregulated pathways and aberrant AR activation. Intense, ongoing research is dedicated to discerning these pathways and ways to target them to improve drug sensitivity. The more complete understanding of these mechanisms of resistance will enable the development of improved treatment strategies to overcome this resistance.
Acknowledgements
This work is supported in part by grants NIH/NCI CA140468, CA168601, CA179970 (A.C. Gao), US Department of Veterans Affairs, Office of Research and Development VA Merits I01 BX002653 (A.C. Gao), and by resources from the VA Northern California Health Care System, Sacramento, California.
References
- 1.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374–1403. doi: 10.1016/j.ejca.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 3.Howlader N, Mariotto AB, Woloshin S, Schwartz LM. Providing clinicians and patients with actual prognosis: cancer in the context of competing causes of death. J Natl Cancer Inst Monogr. 2014;2014:255–264. doi: 10.1093/jncimonographs/lgu022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris WP, Mostaghel EA, Nelson PS, Montgomery B. Androgen deprivation therapy: progress in understanding mechanisms of resistance and optimizing androgen depletion. Nat Clin Pract Urol. 2009;6:76–85. doi: 10.1038/ncpuro1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cookson MS, Roth BJ, Dahm P, Engstrom C, Freedland SJ, Hussain M, Lin DW, Lowrance WT, Murad MH, Oh WK, Penson DF, Kibel AS. Castration-resistant prostate cancer: AUA Guideline. J Urol. 2013;190:429–438. doi: 10.1016/j.juro.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Saad F, Hotte SJ. Guidelines for the management of castrate-resistant prostate cancer. Can Urol Assoc J. 2010;4:380–384. doi: 10.5489/cuaj.10167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steketee K, Timmerman L, Ziel-van der Made AC, Doesburg P, Brinkmann AO, Trapman J. Broadened ligand responsiveness of androgen receptor mutants obtained by random amino acid substitution of H874 and mutation hot spot T877 in prostate cancer. Int J Cancer. 2002;100:309–317. doi: 10.1002/ijc.10495. [DOI] [PubMed] [Google Scholar]
- 8.Dehm SM, Schmidt LJ, Heemers HV, Vessella RL, Tindall DJ. Splicing of a novel androgen receptor exon generates a constitutively active androgen receptor that mediates prostate cancer therapy resistance. Cancer Res. 2008;68:5469–5477. doi: 10.1158/0008-5472.CAN-08-0594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang KH, Ercole CE, Sharifi N. Androgen metabolism in prostate cancer: from molecular mechanisms to clinical consequences. Br J Cancer. 2014;111:1249–1254. doi: 10.1038/bjc.2014.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang KH, Li R, Papari-Zareei M, Watumull L, Zhao YD, Auchus RJ, Sharifi N. Dihydrotestosterone synthesis bypasses testosterone to drive castration-resistant prostate cancer. Proc Natl Acad Sci U S A. 2011;108:13728–13733. doi: 10.1073/pnas.1107898108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shtivelman E, Beer TM, Evans CP. Molecular pathways and targets in prostate cancer. Oncotarget. 2014;5:7217–7259. doi: 10.18632/oncotarget.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, Chi KN, Jones RJ, Goodman OB Jr, Saad F, Staffurth JN, Mainwaring P, Harland S, Flaig TW, Hutson TE, Cheng T, Patterson H, Hainsworth JD, Ryan CJ, Sternberg CN, Ellard SL, Fléchon A, Saleh M, Scholz M, Efstathiou E, Zivi A, Bianchini D, Loriot Y, Chieffo N, Kheoh T, Haqq CM, Scher HI COU-AA-301 Investigators. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364:1995–2005. doi: 10.1056/NEJMoa1014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, de Wit R, Mulders P, Chi KN, Shore ND, Armstrong AJ, Flaig TW, Fléchon A, Mainwaring P, Fleming M, Hainsworth JD, Hirmand M, Selby B, Seely L, de Bono JS AFFIRM Investigators. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–1197. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 14.Sweeney CJ. ECOG: CHAARTED--ChemoHormonal therapy versus androgen ablation randomized trial for extensive disease in prostate cancer. Clin Adv Hematol Oncol. 2006;4:588–590. [PubMed] [Google Scholar]
- 15.Dagher R, Li N, Abraham S, Rahman A, Sridhara R, Pazdur R. Approval summary: Docetaxel in combination with prednisone for the treatment of androgen-independent hormone-refractory prostate cancer. Clin Cancer Res. 2004;10:8147–8151. doi: 10.1158/1078-0432.CCR-04-1402. [DOI] [PubMed] [Google Scholar]
- 16.McGrogan BT, Gilmartin B, Carney DN, McCann A. Taxanes, microtubules and chemoresistant breast cancer. Biochim Biophys Acta. 2008;1785:96–132. doi: 10.1016/j.bbcan.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Shelanski ML, Gaskin F, Cantor CR. Microtubule assembly in the absence of added nucleotides. Proc Natl Acad Sci U S A. 1973;70:765–768. doi: 10.1073/pnas.70.3.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuroda K, Liu H, Kim S, Guo M, Navarro V, Bander NH. Docetaxel down-regulates the expression of androgen receptor and prostate-specific antigen but not prostate-specific membrane antigen in prostate cancer cell lines: implications for PSA surrogacy. Prostate. 2009;69:1579–1585. doi: 10.1002/pros.21004. [DOI] [PubMed] [Google Scholar]
- 19.de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, Gravis G, Bodrogi I, Mackenzie MJ, Shen L, Roessner M, Gupta S, Sartor AO TROPIC Investigators. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147–1154. doi: 10.1016/S0140-6736(10)61389-X. [DOI] [PubMed] [Google Scholar]
- 20.de Leeuw R, Berman-Booty LD, Schiewer MJ, Ciment SJ, Den RB, Dicker AP, Kelly WK, Trabulsi EJ, Lallas CD, Gomella LG, Knudsen KE. Novel actions of next-generation taxanes benefit advanced stages of prostate cancer. Clin Cancer Res. 2015;21:795–807. doi: 10.1158/1078-0432.CCR-14-1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mita AC, Figlin R, Mita MM. Cabazitaxel: more than a new taxane for metastatic castrate-resistant prostate cancer? Clin Cancer Res. 2012;18:6574–6579. doi: 10.1158/1078-0432.CCR-12-1584. [DOI] [PubMed] [Google Scholar]
- 22.Tsao CK, Cutting E, Martin J, Oh WK. The role of cabazitaxel in the treatment of metastatic castration-resistant prostate cancer. Ther Adv Urol. 2014;6:97–104. doi: 10.1177/1756287214528557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gan L, Wang J, Xu H, Yang X. Resistance to docetaxel-induced apoptosis in prostate cancer cells by p38/p53/p21 signaling. Prostate. 2011;71:1158–1166. doi: 10.1002/pros.21331. [DOI] [PubMed] [Google Scholar]
- 24.Domingo-Domenech J, Oliva C, Rovira A, Codony-Servat J, Bosch M, Filella X, Montagut C, Tapia M, Campas C, Dang L, Rolfe M, Ross JS, Gascon P, Albanell J, Mellado B. Interleukin 6, a nuclear factor-kappaB target, predicts resistance to docetaxel in hormone-independent prostate cancer and nuclear factor-kappaB inhibition by PS-1145 enhances docetaxel antitumor activity. Clin Cancer Res. 2006;12:5578–5586. doi: 10.1158/1078-0432.CCR-05-2767. [DOI] [PubMed] [Google Scholar]
- 25.Patterson SG, Wei S, Chen X, Sallman DA, Gilvary DL, Zhong B, Pow-Sang J, Yeatman T, Djeu JY. Novel role of Stat1 in the development of docetaxel resistance in prostate tumor cells. Oncogene. 2006;25:6113–6122. doi: 10.1038/sj.onc.1209632. [DOI] [PubMed] [Google Scholar]
- 26.Zemskova M, Sahakian E, Bashkirova S, Lilly M. The PIM1 kinase is a critical component of a survival pathway activated by docetaxel and promotes survival of docetaxel-treated prostate cancer cells. J Biol Chem. 2008;283:20635–20644. doi: 10.1074/jbc.M709479200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Neill AJ, Prencipe M, Dowling C, Fan Y, Mulrane L, Gallagher WM, O’Connor D, O’Connor R, Devery A, Corcoran C, Rani S, O’Driscoll L, Fitzpatrick JM, Watson RW. Characterisation and manipulation of docetaxel resistant prostate cancer cell lines. Mol Cancer. 2011;10:126. doi: 10.1186/1476-4598-10-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Codony-Servat J, Marin-Aguilera M, Visa L, Garcia-Albeniz X, Pineda E, Fernandez PL, Filella X, Gascon P, Mellado B. Nuclear factor-kappa B and interleukin-6 related docetaxel resistance in castration-resistant prostate cancer. Prostate. 2013;73:512–521. doi: 10.1002/pros.22591. [DOI] [PubMed] [Google Scholar]
- 29.Vidal SJ, Rodriguez-Bravo V, Quinn SA, Rodriguez-Barrueco R, Lujambio A, Williams E, Sun X, de la Iglesia-Vicente J, Lee A, Readhead B, Chen X, Galsky M, Esteve B, Petrylak DP, Dudley JT, Rabadan R, Silva JM, Hoshida Y, Lowe SW, Cordon-Cardo C, Domingo-Domenech J. A targetable GATA2-IGF2 axis confers aggressiveness in lethal prostate cancer. Cancer Cell. 2015;27:223–239. doi: 10.1016/j.ccell.2014.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu C, Zhu Y, Lou W, Nadiminty N, Chen X, Zhou Q, Shi XB, deVere White RW, Gao AC. Functional p53 determines docetaxel sensitivity in prostate cancer cells. Prostate. 2013;73:418–427. doi: 10.1002/pros.22583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zerbini LF, Wang Y, Cho JY, Libermann TA. Constitutive activation of nuclear factor kappaB p50/p65 and Fra-1 and JunD is essential for deregulated interleukin 6 expression in prostate cancer. Cancer Res. 2003;63:2206–2215. [PubMed] [Google Scholar]
- 32.Singh RK, Lokeshwar BL. Depletion of intrinsic expression of Interleukin-8 in prostate cancer cells causes cell cycle arrest, spontaneous apoptosis and increases the efficacy of chemotherapeutic drugs. Mol Cancer. 2009;8:57. doi: 10.1186/1476-4598-8-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qian DZ, Rademacher BL, Pittsenbarger J, Huang CY, Myrthue A, Higano CS, Garzotto M, Nelson PS, Beer TM. CCL2 is induced by chemotherapy and protects prostate cancer cells from docetaxel-induced cytotoxicity. Prostate. 2010;70:433–442. doi: 10.1002/pros.21077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shiota M, Kashiwagi E, Yokomizo A, Takeuchi A, Dejima T, Song Y, Tatsugami K, Inokuchi J, Uchiumi T, Naito S. Interaction between docetaxel resistance and castration resistance in prostate cancer: implications of Twist1, YB-1, and androgen receptor. Prostate. 2013;73:1336–1344. doi: 10.1002/pros.22681. [DOI] [PubMed] [Google Scholar]
- 35.Marin-Aguilera M, Codony-Servat J, Kalko SG, Fernandez PL, Bermudo R, Buxo E, Ribal MJ, Gascon P, Mellado B. Identification of docetaxel resistance genes in castration-resistant prostate cancer. Mol Cancer Ther. 2012;11:329–339. doi: 10.1158/1535-7163.MCT-11-0289. [DOI] [PubMed] [Google Scholar]
- 36.Mimeault M, Johansson SL, Batra SK. Marked improvement of cytotoxic effects induced by docetaxel on highly metastatic and androgen-independent prostate cancer cells by downregulating macrophage inhibitory cytokine-1. Br J Cancer. 2013;108:1079–1091. doi: 10.1038/bjc.2012.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ploussard G, Terry S, Maille P, Allory Y, Sirab N, Kheuang L, Soyeux P, Nicolaiew N, Coppolani E, Paule B, Salomon L, Culine S, Buttyan R, Vacherot F, de la Taille A. Class III beta-tubulin expression predicts prostate tumor aggressiveness and patient response to docetaxel-based chemotherapy. Cancer Res. 2010;70:9253–9264. doi: 10.1158/0008-5472.CAN-10-1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Terry S, Ploussard G, Allory Y, Nicolaiew N, Boissiere-Michot F, Maille P, Kheuang L, Coppolani E, Ali A, Bibeau F, Culine S, Buttyan R, de la Taille A, Vacherot F. Increased expression of class III beta-tubulin in castration-resistant human prostate cancer. Br J Cancer. 2009;101:951–956. doi: 10.1038/sj.bjc.6605245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hara T, Ushio K, Nishiwaki M, Kouno J, Araki H, Hikichi Y, Hattori M, Imai Y, Yamaoka M. A mutation in beta-tubulin and a sustained dependence on androgen receptor signalling in a newly established docetaxel-resistant prostate cancer cell line. Cell Biol Int. 2010;34:177–184. doi: 10.1042/CBI20090030. [DOI] [PubMed] [Google Scholar]
- 40.Makarovskiy AN, Siryaporn E, Hixson DC, Akerley W. Survival of docetaxel-resistant prostate cancer cells in vitro depends on phenotype alterations and continuity of drug exposure. Cell Mol Life Sci. 2002;59:1198–1211. doi: 10.1007/s00018-002-8498-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xie Y, Xu K, Linn DE, Yang X, Guo Z, Shimelis H, Nakanishi T, Ross DD, Chen H, Fazli L, Gleave ME, Qiu Y. The 44-kDa Pim-1 kinase phosphorylates BCRP/ABCG2 and thereby promotes its multimerization and drug-resistant activity in human prostate cancer cells. J Biol Chem. 2008;283:3349–3356. doi: 10.1074/jbc.M707773200. [DOI] [PubMed] [Google Scholar]
- 42.Zhu Y, Liu C, Nadiminty N, Lou W, Tummala R, Evans CP, Gao AC. Inhibition of ABCB1 expression overcomes acquired docetaxel resistance in prostate cancer. Mol Cancer Ther. 2013;12:1829–1836. doi: 10.1158/1535-7163.MCT-13-0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thadani-Mulero M, Portella L, Sun S, Sung M, Matov A, Vessella RL, Corey E, Nanus DM, Plymate SR, Giannakakou P. Androgen receptor splice variants determine taxane sensitivity in prostate cancer. Cancer Res. 2014;74:2270–2282. doi: 10.1158/0008-5472.CAN-13-2876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Niu L, Deng J, Zhu F, Zhou N, Tian K, Yuan H, Lou H. Anti-inflammatory effect of Marchantin M contributes to sensitization of prostate cancer cells to docetaxel. Cancer Lett. 2014;348:126–134. doi: 10.1016/j.canlet.2014.03.019. [DOI] [PubMed] [Google Scholar]
- 45.van Zuylen L, Sparreboom A, van der Gaast A, Nooter K, Eskens FA, Brouwer E, Bol CJ, de Vries R, Palmer PA, Verweij J. Disposition of docetaxel in the presence of P-glycoprotein inhibition by intravenous administration of R101933. Eur J Cancer. 2002;38:1090–1099. doi: 10.1016/s0959-8049(02)00035-7. [DOI] [PubMed] [Google Scholar]
- 46.Fracasso PM, Goldstein LJ, de Alwis DP, Rader JS, Arquette MA, Goodner SA, Wright LP, Fears CL, Gazak RJ, Andre VA, Burgess MF, Slapak CA, Schellens JH. Phase I study of docetaxel in combination with the P-glycoprotein inhibitor, zosuquidar, in resistant malignancies. Clin Cancer Res. 2004;10:7220–7228. doi: 10.1158/1078-0432.CCR-04-0452. [DOI] [PubMed] [Google Scholar]
- 47.Zhu Y, Liu C, Armstrong C, Lou W, Sandher A, Gao AC. Anti-androgens inhibit ABCB1 efflux and ATPase activity and reverse docetaxel resistance in advanced prostate cancer. Clin Cancer Res. 2015 doi: 10.1158/1078-0432.CCR-15-0269. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Montgomery RB, Bonham M, Nelson PS, Grim J, Makary E, Vessella R, Stahl WL. Estrogen effects on tubulin expression and taxane mediated cytotoxicity in prostate cancer cells. Prostate. 2005;65:141–150. doi: 10.1002/pros.20246. [DOI] [PubMed] [Google Scholar]
- 49.Zhu ML, Horbinski CM, Garzotto M, Qian DZ, Beer TM, Kyprianou N. Tubulin-targeting chemotherapy impairs androgen receptor activity in prostate cancer. Cancer Res. 2010;70:7992–8002. doi: 10.1158/0008-5472.CAN-10-0585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Martin SK, Banuelos CA, Sadar MD, Kyprianou N. N-terminal targeting of androgen receptor variant enhances response of castration resistant prostate cancer to taxane chemotherapy. Mol Oncol. 2014 doi: 10.1016/j.molonc.2014.10.014. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Muthu MS, Kulkarni SA, Raju A, Feng SS. Theranostic liposomes of TPGS coating for targeted co-delivery of docetaxel and quantum dots. Biomaterials. 2012;33:3494–3501. doi: 10.1016/j.biomaterials.2012.01.036. [DOI] [PubMed] [Google Scholar]
- 52.Yamamoto Y, Yoshida M, Sato M, Sato K, Kikuchi S, Sugishita H, Kuwabara J, Matsuno Y, Kojima Y, Morimoto M, Horiuchi A, Watanabe Y. Feasibility of tailored, selective and effective anticancer chemotherapy by direct injection of docetaxel-loaded immunoliposomes into Her2/neu positive gastric tumor xenografts. Int J Oncol. 2011;38:33–39. [PubMed] [Google Scholar]
- 53.Ho KS, Aman AM, Al-awar RS, Shoichet MS. Amphiphilic micelles of poly(2-methyl-2-carboxytrimethylene carbonate-co-D,L-lactide)-graft-poly(ethylene glycol) for anti-cancer drug delivery to solid tumours. Biomaterials. 2012;33:2223–2229. doi: 10.1016/j.biomaterials.2011.11.072. [DOI] [PubMed] [Google Scholar]
- 54.Kobayashi D, Kawai N, Sato S, Naiki T, Yamada K, Yasui T, Tozawa K, Kobayashi T, Takahashi S, Kohri K. Thermotherapy using magnetic cationic liposomes powerfully suppresses prostate cancer bone metastasis in a novel rat model. Prostate. 2013;73:913–922. doi: 10.1002/pros.22637. [DOI] [PubMed] [Google Scholar]
- 55.Galletti G, Matov A, Beltran H, Fontugne J, Miguel Mosquera J, Cheung C, MacDonald TY, Sung M, O’Toole S, Kench JG, Suk Chae S, Kimovski D, Tagawa ST, Nanus DM, Rubin MA, Horvath LG, Giannakakou P, Rickman DS. ERG induces taxane resistance in castration-resistant prostate cancer. Nat Commun. 2014;5:5548. doi: 10.1038/ncomms6548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li Z, Bishop AC, Alyamani M, Garcia JA, Dreicer R, Bunch D, Liu J, Upadhyay SK, Auchus RJ, Sharifi N. Conversion of abiraterone to D4A drives anti-tumour activity in prostate cancer. Nature. 2015;523:347–51. doi: 10.1038/nature14406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, Fizazi K, Mainwaring P, Piulats JM, Ng S, Carles J, Mulders PF, Basch E, Small EJ, Saad F, Schrijvers D, Van Poppel H, Mukherjee SD, Suttmann H, Gerritsen WR, Flaig TW, George DJ, Yu EY, Efstathiou E, Pantuck A, Winquist E, Higano CS, Taplin ME, Park Y, Kheoh T, Griffin T, Scher HI, Rathkopf DE. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368:138–148. doi: 10.1056/NEJMoa1209096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ryan CJ, Smith MR, Fizazi K, Saad F, Mulders PF, Sternberg CN, Miller K, Logothetis CJ, Shore ND, Small EJ, Carles J, Flaig TW, Taplin ME, Higano CS, de Souza P, de Bono JS, Griffin TW, De Porre P, Yu MK, Park YC, Li J, Kheoh T, Naini V, Molina A, Rathkopf DE. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomised, double-blind, placebocontrolled phase 3 study. Lancet Oncol. 2015;16:152–160. doi: 10.1016/S1470-2045(14)71205-7. [DOI] [PubMed] [Google Scholar]
- 59.Mostaghel EA, Marck BT, Plymate SR, Vessella RL, Balk S, Matsumoto AM, Nelson PS, Montgomery RB. Resistance to CYP17A1 inhibition with abiraterone in castration-resistant prostate cancer: induction of steroidogenesis and androgen receptor splice variants. Clin Cancer Res. 2011;17:5913–5925. doi: 10.1158/1078-0432.CCR-11-0728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cai C, Chen S, Ng P, Bubley GJ, Nelson PS, Mostaghel EA, Marck B, Matsumoto AM, Simon NI, Wang H, Chen S, Balk SP. Intratumoral de novo steroid synthesis activates androgen receptor in castration-resistant prostate cancer and is upregulated by treatment with CYP17A1 inhibitors. Cancer Res. 2011;71:6503–6513. doi: 10.1158/0008-5472.CAN-11-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chun JY, Nadiminty N, Dutt S, Lou W, Yang JC, Kung HJ, Evans CP, Gao AC. Interleukin-6 regulates androgen synthesis in prostate cancer cells. Clin Cancer Res. 2009;15:4815–4822. doi: 10.1158/1078-0432.CCR-09-0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tian Y, Zhao L, Zhang H, Liu X, Zhao L, Zhao X, Li Y, Li J. AKR1C3 overexpression may serve as a promising biomarker for prostate cancer progression. Diagn Pathol. 2014;9:42. doi: 10.1186/1746-1596-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu C, Lou W, Zhu Y, Yang JC, Nadiminty N, Gaikwad NW, Evans CP, Gao AC. Intracrine Androgens and AKR1C3 Activation Confer Resistance to Enzalutamide in Prostate Cancer. Cancer Res. 2015;75:1413–1422. doi: 10.1158/0008-5472.CAN-14-3080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhao XY, Malloy PJ, Krishnan AV, Swami S, Navone NM, Peehl DM, Feldman D. Glucocorticoids can promote androgen-independent growth of prostate cancer cells through a mutated androgen receptor. Nat Med. 2000;6:703–706. doi: 10.1038/76287. [DOI] [PubMed] [Google Scholar]
- 65.Grigoryev DN, Long BJ, Njar VC, Brodie AH. Pregnenolone stimulates LNCaP prostate cancer cell growth via the mutated androgen receptor. J Steroid Biochem Mol Biol. 2000;75:1–10. doi: 10.1016/s0960-0760(00)00131-x. [DOI] [PubMed] [Google Scholar]
- 66.Culig Z, Hobisch A, Cronauer MV, Cato AC, Hittmair A, Radmayr C, Eberle J, Bartsch G, Klocker H. Mutant androgen receptor detected in an advanced-stage prostatic carcinoma is activated by adrenal androgens and progesterone. Mol Endocrinol. 1993;7:1541–1550. doi: 10.1210/mend.7.12.8145761. [DOI] [PubMed] [Google Scholar]
- 67.Attard G, Reid AH, Auchus RJ, Hughes BA, Cassidy AM, Thompson E, Oommen NB, Folkerd E, Dowsett M, Arlt W, de Bono JS. Clinical and biochemical consequences of CYP17A1 inhibition with abiraterone given with and without exogenous glucocorticoids in castrate men with advanced prostate cancer. J Clin Endocrinol Metab. 2012;97:507–516. doi: 10.1210/jc.2011-2189. [DOI] [PubMed] [Google Scholar]
- 68.Sternberg CN, Petrylak DP, Madan RA, Parker C. Progress in the treatment of advanced prostate cancer. Am Soc Clin Oncol Educ Book. 2014:117–131. doi: 10.14694/EdBook_AM.2014.34.117. [DOI] [PubMed] [Google Scholar]
- 69.Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, Iversen P, Bhattacharya S, Carles J, Chowdhury S, Davis ID, de Bono JS, Evans CP, Fizazi K, Joshua AM, Kim CS, Kimura G, Mainwaring P, Mansbach H, Miller K, Noonberg SB, Perabo F, Phung D, Saad F, Scher HI, Taplin ME, Venner PM, Tombal B PREVAIL Investigators. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–433. doi: 10.1056/NEJMoa1405095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sternberg CN, de Bono JS, Chi KN, Fizazi K, Mulders P, Cerbone L, Hirmand M, Forer D, Scher HI. Improved outcomes in elderly patients with metastatic castration-resistant prostate cancer treated with the androgen receptor inhibitor enzalutamide: results from the phase III AFFIRM trial. Ann Oncol. 2014;25:429–434. doi: 10.1093/annonc/mdt571. [DOI] [PubMed] [Google Scholar]
- 71.Waltering KK, Urbanucci A, Visakorpi T. Androgen receptor (AR) aberrations in castra tion-resistant prostate cancer. Mol Cell Endocrinol. 2012;360:38–43. doi: 10.1016/j.mce.2011.12.019. [DOI] [PubMed] [Google Scholar]
- 72.Eisermann K, Wang D, Jing Y, Pascal LE, Wang Z. Androgen receptor gene mutation, rearrangement, polymorphism. Transl Androl Urol. 2013;2:137–147. doi: 10.3978/j.issn.2223-4683.2013.09.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Korpal M, Korn JM, Gao X, Rakiec DP, Ruddy DA, Doshi S, Yuan J, Kovats SG, Kim S, Cooke VG, Monahan JE, Stegmeier F, Roberts TM, Sellers WR, Zhou W, Zhu P. An F876L mutation in androgen receptor confers genetic and phenotypic resistance to MDV3100 (enzalutamide) Cancer Discov. 2013;3:1030–1043. doi: 10.1158/2159-8290.CD-13-0142. [DOI] [PubMed] [Google Scholar]
- 74.Tran C, Ouk S, Clegg NJ, Chen Y, Watson PA, Arora V, Wongvipat J, Smith-Jones PM, Yoo D, Kwon A, Wasielewska T, Welsbie D, Chen CD, Higano CS, Beer TM, Hung DT, Scher HI, Jung ME, Sawyers CL. Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science. 2009;324:787–790. doi: 10.1126/science.1168175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cui Y, Nadiminty N, Liu C, Lou W, Schwartz CT, Gao AC. Upregulation of glucose metabolism by NF-kappaB2/p52 mediates enzalutamide resistance in castration-resistant prostate cancer cells. Endocr Relat Cancer. 2014;21:435–442. doi: 10.1530/ERC-14-0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nadiminty N, Tummala R, Liu C, Yang J, Lou W, Evans CP, Gao AC. NF-kappaB2/p52 induces resistance to enzalutamide in prostate cancer: role of androgen receptor and its variants. Mol Cancer Ther. 2013;12:1629–1637. doi: 10.1158/1535-7163.MCT-13-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu C, Zhu Y, Lou W, Cui Y, Evans CP, Gao AC. Inhibition of constitutively active Stat3 reverses enzalutamide resistance in LNCaP derivative prostate cancer cells. Prostate. 2014;74:201–209. doi: 10.1002/pros.22741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Li Y, Alsagabi M, Fan D, Bova GS, Tewfik AH, Dehm SM. Intragenic rearrangement and altered RNA splicing of the androgen receptor in a cell-based model of prostate cancer progression. Cancer Res. 2011;71:2108–2117. doi: 10.1158/0008-5472.CAN-10-1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nadiminty N, Tummala R, Liu C, Lou W, Evans CP, Gao AC. NF-κB2/p52:c-Myc:hnRNPA1 Pathway Regulates Expression of Androgen Receptor Splice Variants and Enzalutamide Sensitivity in Prostate Cancer. Mol Cancer Ther. 2015;14:1884–1895. doi: 10.1158/1535-7163.MCT-14-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dehm SM, Tindall DJ. Alternatively spliced androgen receptor variants. Endocr Relat Cancer. 2011;18:R183–196. doi: 10.1530/ERC-11-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Guo Z, Yang X, Sun F, Jiang R, Linn DE, Chen H, Chen H, Kong X, Melamed J, Tepper CG, Kung HJ, Brodie AM, Edwards J, Qiu Y. A novel androgen receptor splice variant is up-regulated during prostate cancer progression and promotes androgen depletion-resistant growth. Cancer Res. 2009;69:2305–2313. doi: 10.1158/0008-5472.CAN-08-3795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hu R, Dunn TA, Wei S, Isharwal S, Veltri RW, Humphreys E, Han M, Partin AW, Vessella RL, Isaacs WB, Bova GS, Luo J. Ligand-independent androgen receptor variants derived from splicing of cryptic exons signify hormone-refractory prostate cancer. Cancer Res. 2009;69:16–22. doi: 10.1158/0008-5472.CAN-08-2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sun S, Sprenger CC, Vessella RL, Haugk K, Soriano K, Mostaghel EA, Page ST, Coleman IM, Nguyen HM, Sun H, Nelson PS, Plymate SR. Castration resistance in human prostate cancer is conferred by a frequently occurring androgen receptor splice variant. J Clin Invest. 2010;120:2715–2730. doi: 10.1172/JCI41824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yang X, Guo Z, Sun F, Li W, Alfano A, Shimelis H, Chen M, Brodie AM, Chen H, Xiao Z, Veenstra TD, Qiu Y. Novel membrane-associated androgen receptor splice variant potentiates proliferative and survival responses in prostate cancer cells. J Biol Chem. 2011;286:36152–36160. doi: 10.1074/jbc.M111.265124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hornberg E, Ylitalo EB, Crnalic S, Antti H, Stattin P, Widmark A, Bergh A, Wikstrom P. Expression of androgen receptor splice variants in prostate cancer bone metastases is associated with castration-resistance and short survival. PLoS One. 2011;6:e19059. doi: 10.1371/journal.pone.0019059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Joseph JD, Lu N, Qian J, Sensintaffar J, Shao G, Brigham D, Moon M, Maneval EC, Chen I, Darimont B, Hager JH. A clinically relevant androgen receptor mutation confers resistance to second-generation antiandrogens enzalutamide and ARN-509. Cancer Discov. 2013;3:1020–1029. doi: 10.1158/2159-8290.CD-13-0226. [DOI] [PubMed] [Google Scholar]
- 87.Li Y, Chan SC, Brand LJ, Hwang TH, Silverstein KA, Dehm SM. Androgen receptor splice variants mediate enzalutamide resistance in castration-resistant prostate cancer cell lines. Cancer Res. 2013;73:483–489. doi: 10.1158/0008-5472.CAN-12-3630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Antonarakis ES, Lu C, Wang H, Luber B, Nakazawa M, Roeser JC, Chen Y, Mohammad TA, Chen Y, Fedor HL, Lotan TL, Zheng Q, De Marzo AM, Isaacs JT, Isaacs WB, Nadal R, Paller CJ, Denmeade SR, Carducci MA, Eisenberger MA, Luo J. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N Engl J Med. 2014;371:1028–1038. doi: 10.1056/NEJMoa1315815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Antonarakis ES, Lu C, Chen Y, Luber B, Wang H, Nakazawa M, De Marzo AM, Isaacs WB, Nadal R, Paller CJ, et al. ASCO Genitourinary Cancers Symposium. vol. 33 (suppl 7; abstr 138) Orlando, FL, USA: Journal of Clinical Oncology; 2015. AR splice variant 7 (AR-V7) and response to taxanes in men with metastatic castration-resistant prostate cancer (mCRPC) [Google Scholar]
- 90.Nguyen HG, Yang JC, Kung HJ, Shi XB, Tilki D, Lara PN Jr, DeVere White RW, Gao AC, Evans CP. Targeting autophagy overcomes Enzalutamide resistance in castration-resistant prostate cancer cells and improves therapeutic response in a xenograft model. Oncogene. 2014;33:4521–4530. doi: 10.1038/onc.2014.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liu C, Lou W, Zhu Y, Nadiminty N, Schwartz CT, Evans CP, Gao AC. Niclosamide inhibits androgen receptor variants expression and overcomes enzalutamide resistance in castration-resistant prostate cancer. Clin Cancer Res. 2014;20:3198–3210. doi: 10.1158/1078-0432.CCR-13-3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Liu C, Lou W, Armstrong C, Zhu Y, Evans CP, Gao AC. Niclosamide suppresses cell migration and invasion in enzalutamide resistant prostate cancer cells via Stat3-AR axis inhibition. Prostate. 2015;75:1341–1353. doi: 10.1002/pros.23015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yamashita S, Lai KP, Chuang KL, Xu D, Miyamoto H, Tochigi T, Pang ST, Li L, Arai Y, Kung HJ, Yeh S, Chang C. ASC-J9 suppresses castration-resistant prostate cancer growth through degradation of full-length and splice variant androgen receptors. Neoplasia. 2012;14:74–83. doi: 10.1593/neo.111436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Myung JK, Banuelos CA, Fernandez JG, Mawji NR, Wang J, Tien AH, Yang YC, Tavakoli I, Haile S, Watt K, McEwan IJ, Plymate S, Andersen RJ, Sadar MD. An androgen receptor N-terminal domain antagonist for treating prostate cancer. J Clin Invest. 2013;123:2948–2960. doi: 10.1172/JCI66398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Andersen RJ, Mawji NR, Wang J, Wang G, Haile S, Myung JK, Watt K, Tam T, Yang YC, Banuelos CA, Williams DE, McEwan IJ, Wang Y, Sadar MD. Regression of castrate-recurrent prostate cancer by a small-molecule inhibitor of the amino-terminus domain of the androgen receptor. Cancer Cell. 2010;17:535–546. doi: 10.1016/j.ccr.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 96.Banuelos CA, Lal A, Tien AH, Shah N, Yang YC, Mawji NR, Meimetis LG, Park J, Kunzhong J, Andersen RJ, Sadar MD. Characterization of niphatenones that inhibit androgen receptor N-terminal domain. PLoS One. 2014;9:e107991. doi: 10.1371/journal.pone.0107991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jin C, Yang L, Xie M, Lin C, Merkurjev D, Yang JC, Tanasa B, Oh S, Zhang J, Ohgi KA, Zhou H, Li W, Evans CP, Ding S, Rosenfeld MG. Chem-seq permits identification of genomic targets of drugs against androgen receptor regulation selected by functional phenotypic screens. Proc Natl Acad Sci U S A. 2014;111:9235–9240. doi: 10.1073/pnas.1404303111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cheng HH, Gulati R, Azad A, Nadal R, Twardowski P, Vaishampayan UN, Agarwal N, Heath EI, Pal SK, Rehman HT, Leiter A, Batten JA, Montgomery RB, Galsky MD, Antonarakis ES, Chi KN, Yu EY. Activity of enzalutamide in men with metastatic castration-resistant prostate cancer is affected by prior treatment with abiraterone and/or docetaxel. Prostate Cancer Prostatic Dis. 2015;18:122–7. doi: 10.1038/pcan.2014.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schweizer MT, Zhou XC, Wang H, Bassi S, Carducci MA, Eisenberger MA, Antonarakis ES. The influence of prior abiraterone treatment on the clinical activity of docetaxel in men with metastatic castration-resistant prostate cancer. Eur Urol. 2014;66:646–652. doi: 10.1016/j.eururo.2014.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mezynski J, Pezaro C, Bianchini D, Zivi A, Sandhu S, Thompson E, Hunt J, Sheridan E, Baikady B, Sarvadikar A, Maier G, Reid AH, Mulick Cassidy A, Olmos D, Attard G, de Bono J. Antitumour activity of docetaxel following treatment with the CYP17A1 inhibitor abiraterone: clinical evidence for cross-resistance? Ann Oncol. 2012;23:2943–2947. doi: 10.1093/annonc/mds119. [DOI] [PubMed] [Google Scholar]
- 101.Nadal R, Zhang Z, Rahman H, Schweizer MT, Denmeade SR, Paller CJ, Carducci MA, Eisenberger MA, Antonarakis ES. Clinical activity of enzalutamide in Docetaxel-naive and Docetaxel-pretreated patients with metastatic castration-resistant prostate cancer. Prostate. 2014;74:1560–1568. doi: 10.1002/pros.22874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.van Soest RJ, de Morree ES, Kweldam CF, de Ridder CM, Wiemer EA, Mathijssen RH, de Wit R, van Weerden WM. Targeting the androgen receptor confers in vivo cross-resistance between enzalutamide and docetaxel, but not cabazitaxel, in castration-resistant prostate cancer. Eur Urol. 2015;67:981–5. doi: 10.1016/j.eururo.2014.11.033. [DOI] [PubMed] [Google Scholar]
- 103.Al Nakouzi N, Le Moulec S, Albiges L, Wang C, Beuzeboc P, Gross-Goupil M, de La Motte Rouge T, Guillot A, Gajda D, Massard C, Gleave M, Fizazi K, Loriot Y. Cabazitaxel remains active in patients progressing after docetaxel followed by novel androgen receptor pathway targeted therapies. Eur Urol. 2015;68:228–35. doi: 10.1016/j.eururo.2014.04.015. [DOI] [PubMed] [Google Scholar]


