Abstract
Purpose
To determine the mechanisms of vertical fusional vergence in patients with “congenital unilateral superior oblique paresis” (SOP) and to discuss the implications of these mechanisms.
Methods
Eleven patients were examined with our eye-tracking haploscope.
Results
Three different fusion mechanisms were found, producing significantly different cyclovergence to vertical vergence ratios (P < 0.05): primary use of the vertical rectus muscles in seven patients (ratio: 0.36 ± 1.6), primary use of the oblique muscles in one patient (0.04), and use of the superior oblique muscle in the higher eye and the superior rectus muscle in the lower eye in three patients (1.15 ± 0.32). Lancaster red-green testing showed alignment differences among these groups, primarily differences in amount of subjective extorsion between the two eyes in straight-ahead gaze: The patient with oblique-muscle–mediated fusion showed essentially no subjective extorsion (0.5°), the patients with vertical-rectus-muscle–mediated vertical fusion showed a mean ± SD subjective extorsion of 3.6° ± 1.4°, and the patients with the mixed (oblique/rectus) fusion mechanism showed 7.0° ± 1.7° (P < 0.05).
Conclusions
The choice of fusion mechanism may be a function of how much intorting effect is needed. Use of the oblique muscles bilaterally causes the least intorting effect, use of the vertical rectus muscles bilaterally adds more intorting effect, and activation of the “paretic” superior oblique muscle in the higher eye and the superior rectus muscle in the lower eye provides the greatest intorting effect. Subclassifying “congenital SOP” in this way (in which the “paretic” muscle may remain functional in many cases) may help guide its optimal surgical correction.
Keywords: vertical fusional vergence, superior oblique paresis, video-oculography
Patients with “congenital unilateral superior oblique paresis” use one of three mechanisms of vertical fusional vergence to overcome their hyperdeviation. The choice of fusion mechanism may be a function of how much intorting effect is needed and may help guide the optimal surgical approach.
By analysis of the accompanying torsional movement of an eye during vertical movement, one can judge the relative contribution of the oblique muscles versus the vertical rectus muscles to that vertical movement. Such analyses have suggested that the oblique extraocular muscles play a predominant role in vertical fusional vergence in healthy individuals.1–4 Vertical fusional vergence induced by prism-produced vertical disparity in healthy subjects, and assessed using manual video-oculography, was associated with a cycloversion of the eyes (torsion of both eyes in the same direction), with the downward-moving eye intorting and the upward-moving eye extorting.1 This movement pattern suggested that the oblique muscles were largely responsible for disparity-induced vertical vergence movements. This movement pattern was largely confirmed in healthy subjects using scleral search coil recordings, with the caveat that part of the cycloversion response was in the form of torsional nystagmus.2 Subsequent studies using an afterimage technique3 and automated video-oculography4 further supported the above findings in healthy subjects and supported the idea that the oblique muscles were the primary mediators of normal vertical fusional vergence.3,4
The fourth cranial nerve, which innervates only the superior oblique muscle, can be damaged from blunt head trauma. This causes a characteristic ocular motility pattern, with elevation and extorsion of the higher eye and a compensatory head tilt away from the higher eye, which we call acquired fourth nerve paresis/palsy or superior oblique paresis/palsy (SOP). A very similar ocular motility pattern of misalignment, however, with no such trauma, can occur in any decade of life and is of uncertain etiology. The historically presumed cause has been an inborn weakness (“paresis”) of the superior oblique muscle not manifest until later in life (therefore historically termed “congenital” SOP). Magnetic resonance imaging studies, however, have shown that many patients with apparent congenital SOP have superior oblique muscles with normal cross-sectional area and normal contractility,5,6 suggesting other causes for “congenital” SOP in many cases.7,8
Because of different mechanisms likely involved in the genesis of the ocular motility pattern known as SOP, one should not be surprised if patients use different vertical vergence mechanisms to compensate for such deviations when small enough to allow motor fusion. The particular mechanism used may also correlate with surgical outcome, and thus may influence the best approach for surgical correction.
Indeed, different mechanisms of vertical fusional vergence, not predominately relying on the oblique muscles, were found by Mudgil and colleagues9 in patients with various forms of “SOP.” Using scleral search coil eye movement recordings, they identified three different patterns of vertical fusional vergence during attempted fusion in patients with unilateral SOP. The predominant pattern, involving extorsion of the downward-moving eye and intorsion of the upward-moving eye, suggested a predominant role of the vertical rectus muscles. This was found in all of their patients with true, acquired SOP, but in only one-third of patients with “congenital” SOP.9
The purpose of this study was to investigate cyclovertical eye movement patterns during vertical fusion in patients with “congenital unilateral SOP” using our custom eye-tracking haploscope,4,10,11 and to investigate the value of classifying “congenital SOP” by the type of compensatory fusion used, in hopes of guiding the approach used for surgical correction.
Methods
Eleven patients (age 20–63 years) diagnosed with “congenital unilateral SOP,” without previous eye muscle surgery, participated in this study, which was approved by the Johns Hopkins University Institutional Review Board and adhered to the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects after explaining the nature and possible consequences of the study.
Eye Movement Recordings
In all patients, before surgery, vertical fusional vergence was assessed with our eye-tracking haploscope (frame rate ≈15 Hz, accuracy ≤ 0.358, precision ≤ 0.2°),4,10,11 which we fabricated from an old Bausch and Lomb arc perimeter (Bausch and Lomb, Rochester, NY, USA) presenting a separate image to each eye of the patient. Concentric circle targets without torsional cues, subtending greater than 54 degrees of visual angle, were mounted on the two arms of the arc perimeter and viewed in two 45-degree mirrors at a near viewing distance of 33 cm. Tilting the arc perimeter arms introduced vertical disparity between the two targets. Two webcams (240 × 320 pixel resolution, equipped with close-up lenses10), connected to a desktop computer, recorded horizontal, vertical, and torsional eye movements, binocularly, through the use of pupil-based and iris-crypt–based video-oculography10 as well as horizontal, vertical, and torsional in-plane head movements by means of video-based monitoring of black adhesive dots with a white border placed near the patient's inner canthi,11 all in near infrared light. Data were acquired and analyzed using custom MATLAB software (Mathworks, Inc., Natick, MA, USA), interfacing with commercial eye-tracking software IRIS (Chronos Vision, Berlin, Germany). For a more detailed description of our eye-tracking apparatus and method, please refer to Refs. 10 and 11.
Patients were examined with the targets aligned with no vertical disparity except when the patient complained of diplopia. In that case, the targets were realigned (using a lever to tilt the arc perimeter's arms, thus bringing one target upward and the other one downward), so that the patient could barely fuse them in straight-ahead gaze with the head upright. Eye movements were recorded during alternating binocular and monocular viewing sessions by covering and then uncovering one target or the other (haploscopic cover testing4) while the patients were instructed to look straight ahead and attempt fusion when both targets were visible. Haploscopic cover testing was performed with head straight and when tilted 45 degrees to the left and right so as to obtain positions that could facilitate fusion and thereby ensure detection of measureable values for vertical vergence and accompanying torsional movements, from which we determined the fusion mechanism used.
More precisely, we analyzed the directions of simultaneous vertical and torsional movements of each eye to identify which pairs of muscles were primarily acting during fusion. For example, if the higher eye is moving downward and simultaneously intorting with vertical fusional vergence, the superior oblique muscle is the primary mover, but if it is moving downward and simultaneously extorting, it is the inferior rectus muscle that is the primary mover for that eye.
We also calculated a cyclovergence to vertical vergence ratio by computing the absolute value of the change in torsional deviation (the difference between the right and left eye torsional position) from before to after fusion divided by the change in vertical deviation from before to after fusion.
Zero reference positions for horizontal, vertical, and torsional tracings were determined at the beginning of each recording with the targets aligned and head upright, by covering each eye (target) in turn, and having the other viewing eye fixate on the center of the uncovered target pattern. An absolute zero torsional position could not be defined, but it was the relative changes in torsion that we were investigating in this study.
Lancaster Red-Green Testing
In addition, all patients underwent Lancaster red-green testing12 in the nine diagnostic positions of gaze after a 30- to 60-minute patch test to reduce the effect of vergence adaptation.13
The Lancaster red-green test maps not only horizontal and vertical but also torsional ocular deviations. During the test, the patient is seated 1 m in front of a rectilinear grid of black dots marked on the wall (the distance between consecutive dots corresponds to 15 prism diopters straight ahead), wears dissociative red-green goggles, and holds a special red linear streak flashlight, while the examiner holds a green streak flashlight. The eye covered by the red filter thus sees only the red streak, whereas the eye covered by the green filter only sees the green streak. The examiner initially orients the green streak on the central dot corresponding to straight-ahead gaze. The patient is asked to superimpose the red streak on the green streak on the wall. The separation and inclination between the streaks indicates the deviation and subjective degree of torsion between the eyes respectively. This procedure is repeated in each of the nine diagnostic positions of gaze. This simulates a red laser beam projecting out from the right fovea and a green laser beam projecting out from the left fovea, mapping the subjective vertical projections of the foveas onto the wall. The results are plotted on a piece of paper, recording ocular deviations at each diagnostic position.
From the Lancaster red-green plot, we estimated the amounts of vertical deviation in up-and-in gaze of the paretic eye (elevation and adduction), up-and-out gaze, down-and-in gaze, and down-and-out gaze (depression and abduction), as well as the amount of subjective extorsion between the two eyes in straight-ahead gaze. The latter was measured with the help of a protractor after manually extending the recorded red and green streaks (with a precision of approximately ±0.2°14).
Surgery
Furthermore, results from exaggerated forced ductions performed at surgery were assessed in all but one patient (the only one not seen by the second author), specifically obtaining an estimate of the tightness of the oblique muscles by placing them on maximum stretch.15 Such exaggerated traction testing allows a graded evaluation of oblique muscle tightness on a scale from 0 to 4+, with normal superior oblique muscle tightness averaging approximately 1.5+ and normal inferior oblique muscle tightness averaging approximately 1.0+.15
The choice of surgical approach was not influenced by the results of the eye movement recordings because the analyses of the recordings had usually not been completed by the time of surgery.
Results
Eye Movement Recordings
The following results are summarized in the Table. Three different patterns of torsional eye movements were identified in our patients when overcoming their hyperdeviation with vertical fusional vergence with head straight or tilted. In seven patients, vertical fusional vergence was accompanied by a cycloversion toward the side of the higher eye. The opposite mechanism was observed in one patient: vertical fusional vergence accompanied by a cycloversion away from the side of the higher eye. The remaining three patients showed vertical fusional vergence to be associated with a cyclovergence, with both the higher eye intorting and the lower eye intorting.
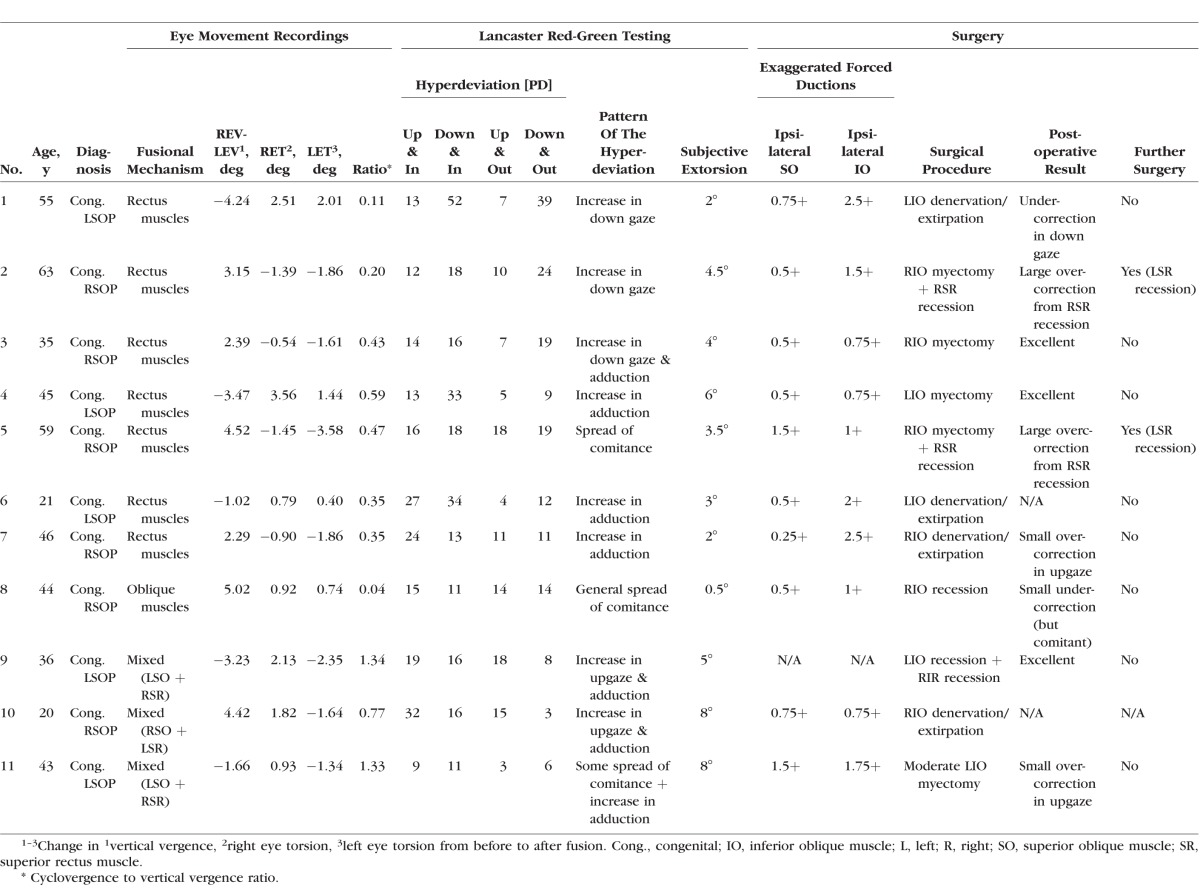
Table.
Summary of SOP Patient Data
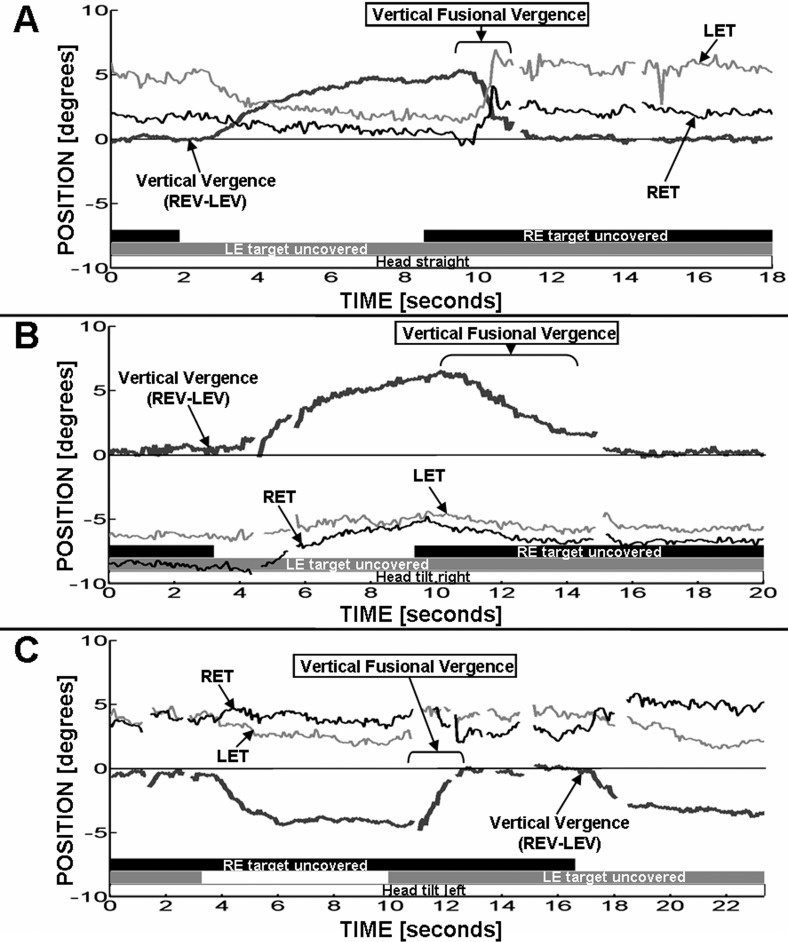
Typical examples of video-oculographic recordings during haploscopic cover testing in our patients are illustrated in Figure 1. Figure 1A depicts a patient with “congenital right SOP,” showing vertical fusional vergence associated with cycloversion toward the side of the higher eye (which was found in 7 of the 11 patients). When the right eye's target is covered, at approximately 2 seconds, the underlying right hyperdeviation develops (upward vergence trace). After the cover is then removed from the right eye's target, at approximately 8 seconds, both eyes are then viewing, and vertical fusional vergence occurs (the right eye relatively depresses while the left eye relatively elevates), accompanied by clockwise cycloversion to the right (extorsion of the right eye and intorsion of the left eye), that is, a cycloversion toward the side of the higher eye. This pattern of simultaneous vertical and torsional eye movements, with the higher eye depressing and extorting with vertical fusional vergence, and with the lower eye elevating and intorting (Fig. 1A), indicates increased action of the higher eye's inferior rectus muscle and the lower eye's superior rectus muscle (the “vertical rectus muscle mechanism”), with of course simultaneous inhibition of their direct antagonists.
Figure 1.
Video-oculographic recordings from patients with “congenital SOP,” showing vertical fusional vergence associated with (A) cycloversion toward the side of the higher, right eye (which was the pattern found in 7 of the 11 patients; patient 5 shown), and (B) cycloversion away from the side of the higher, right eye (the pattern found in one patient: patient 8), and (C) cyclovergence, with the higher, left eye torting away from, and the lower, right eye torting toward, the side of the higher, left eye (the pattern found in 3 of the 11 patients; patient 9 shown). Vertical vergence (thick black trace) is shown, with positive representing the right eye higher than the left. Upward deflections of right eye torsion (thin black trace) and left eye torsion (thin gray trace) represent clockwise eye movements from the subject's perspective looking forward (extorsion of the right eye and intorsion of the left eye). LEV, left eye vertical; REV, right eye vertical; LET, left eye torsion; RET, right eye torsion. Gaps in the recordings indicate blink artifacts that have been removed for clarity. The vergence tracings have been zeroed at the resting, fusing position with both eyes open for clarity.
Figure 1B illustrates another patient with “congenital right SOP,” showing vertical fusional vergence associated with a cycloversion away from the side of the higher eye (found in 1 of the 11 patients). When the right eye's target is covered at approximately 3 seconds, the underlying right hyperdeviation develops. After the cover is then removed from the right eye's target, at approximately 9 seconds, both eyes are viewing, and vertical fusional vergence occurs, accompanied by cycloversion away from the side of the higher eye (intorsion of the higher, right eye and extorsion of the lower, left eye). This pattern of simultaneous vertical and torsional eye movements, with the higher eye depressing and intorting, and with the lower eye elevating and extorting (Fig. 1B), indicates increased action of the higher eye's superior oblique muscle and the lower eye's inferior oblique muscle (the “oblique muscle mechanism”).
Figure 1C depicts another patient, with “congenital left SOP,” who showed a cyclovergence accompanying the vertical fusional vergence, with the higher left eye torting away from, and the lower right eye torting toward the side of the higher eye (found in 3 of the 11 patients). When the left eye's target is covered at approximately 3 seconds, the underlying left hyperdeviation develops (downward vergence trace). After the cover is then removed from the left eye's target, at approximately 10 seconds, both eyes are viewing, and vertical fusional vergence occurs, accompanied by a cyclovergence, with both eyes intorting (intorsion of the higher, left eye and intorsion of the lower, right eye). This pattern of simultaneous vertical and torsional eye movements, with the higher eye depressing and intorting, and with the lower eye elevating and intorting (Fig. 1C), indicates increased action of the higher left eye's superior oblique muscle and the lower right eye's superior rectus muscle (the “mixed mechanism”). When the left eye's target is again covered at approximately 17 seconds, the underlying left hyperdeviation develops again, now with both eyes extorting.
These three groups of patients with “congenital SOP” showed a statistically significant difference in their cyclovergence to vertical vergence ratio (Kruskal-Wallis test: H = 7.27[2, n = 11], P < 0.05). The patients who primarily used their vertical rectus muscles for vertical fusional vergence had a mean ± SD cyclovergence to vertical vergence ratio of 0.36 ± 0.16, whereas the patient with oblique-muscle–mediated fusion had a cyclovergence to vertical vergence ratio of 0.04, and the patients with the mixed (oblique/rectus) mechanism of vertical fusional vergence had a mean ± SD cyclovergence to vertical vergence ratio of 1.15 ± 0.32.
Lancaster Red-Green Testing
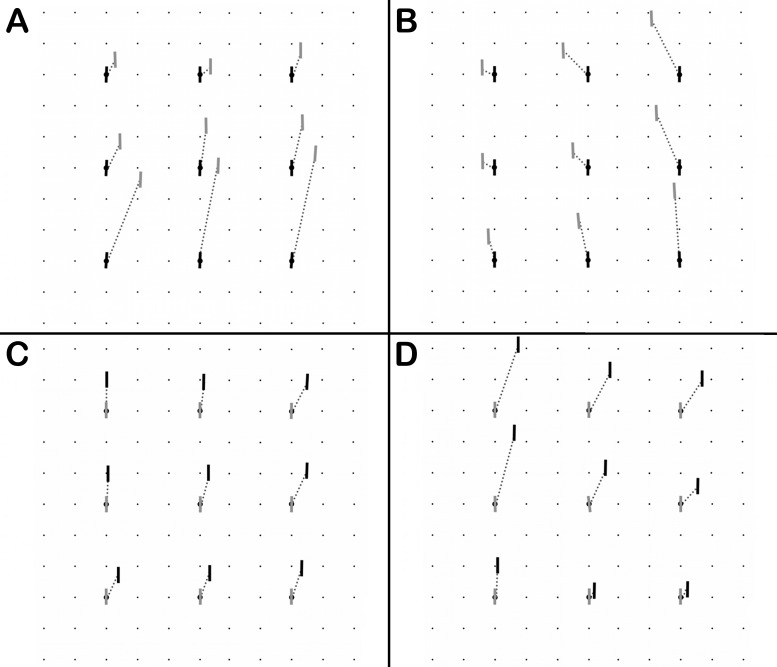
Among the three groups of patients, there was also a statistically significant difference in the subjective extorsion between the two eyes in straight-ahead gaze (Kruskal-Wallis test: H = 6.41[2, n = 11], P < 0.05). For example, the patients who primarily used their vertical rectus muscles for vertical fusional vergence showed a mean ± SD subjective extorsion between the two eyes of 3.6 ± 1.4 degrees, whereas the patient with oblique-muscle–mediated fusion showed 0.5 degree of subjective extorsion between the two eyes, and the patients with the mixed (oblique/rectus) mechanism of vertical fusional vergence showed a mean ± SD subjective extorsion between the two eyes of 7.0 ± 1.7 degrees. Typical examples of Lancaster red-green plots from our patients are illustrated in Figure 2.
Figure 2.
Lancaster red-green plots from patients with “congenital SOP.” The black lines correspond to the projections of the subjective vertical meridians of the right eye onto the wall, and the gray lines correspond to the projections of the subjective vertical meridians of the left eye onto the wall. (A) Patient with vertical-rectus-muscle–mediated fusion, demonstrating an incomitant hyperdeviation that increases in down gaze (patient 1 shown). (B) Another patient with vertical-rectus-muscle–mediated vertical fusion, showing a left hyperdeviation that increases in adduction of the higher, left eye (also interpretable as a relatively comitant cyclovertical deviation, combining extorsion and elevation, of the left eye's approximately square eye movement pattern; patient 6 shown). (C) Patient with oblique-muscle–mediated fusion, showing general spread of comitance (patient 8 shown). (D) Patient with mixed (oblique/rectus muscle) mechanism of vertical fusional vergence, showing a right hyperdeviation that increases in upgaze and adduction of the higher, right eye (also interpretable as extorsion and elevation of the right eye's entire eye movement pattern; patient 10 shown).
Two of the seven patients who primarily used their vertical rectus muscles for vertical fusional vergence (patients 1 and 2) showed an incomitant hyperdeviation that increased in down gaze (Fig. 2A). Three other patients in this seven-patient cohort (patients 4, 6, and 7) showed an incomitant hyperdeviation that uniformly increased in adduction of the higher eye (Fig. 2B). Note that although the hyperdeviation in Fig. 2B appears incomitant, the eye movement pattern of the higher eye is relatively undistorted/square but is extorted and displaced upward (mentally connect the left eye's streaks to appreciate this), also interpretable as truly a relatively comitant cyclovertical deviation. Of the two remaining patients with vertical-rectus-muscle–mediated vertical fusion, patient 3 showed a hyperdeviation that increased particularly in down gaze and adduction of the higher eye, and patient 5 showed a general spread of comitance, with a slightly greater deviation in down gaze and abduction than in down and adduction of the higher eye.
The patient with oblique-muscle–mediated fusion (patient 8) showed general spread of comitance (Fig. 2C), typical for a longstanding pattern of “SOP” that has been compensated by vertical prism.
Two of the patients with the mixed (oblique/rectus) mechanism of vertical fusional vergence (patients 9 and 10) showed a hyperdeviation that increased in upgaze and adduction of the higher eye, with a greater deviation in elevation and adduction than in depression and adduction of the higher eye (Fig. 2D; also note extorsion and elevation of the higher eye's entire eye movement pattern). The remaining patient with the mixed fusion mechanism (patient 11) showed a somewhat more comitant cyclovertical deviation, increasing in adduction of the higher eye (similar to Fig. 2B).
Surgery
No specific differences were observed among the three groups of patients in terms of findings from intraoperative forced traction testing. Of particular note is that in those vertical-rectus-muscle–mediated fusion patients with increasing hyperdeviation primarily in down gaze, the ipsilateral inferior oblique muscle was felt to be relatively tighter than its direct antagonist, the ipsilateral superior oblique muscle.
Of the seven patients using the vertical rectus muscle mechanism of vertical fusional vergence, three had an ipsilateral inferior oblique muscle denervation and extirpation procedure, and the other four had a large ipsilateral inferior oblique muscle myectomy, with two of those (where the hyperdeviation was greater in abduction and depression than in adduction and depression; see the Table) having additional ipsilateral superior rectus muscle recession. These latter two patients were the only ones requiring further surgery for overcorrection.
The patient who primarily used the oblique muscles for vertical fusional vergence had an ipsilateral inferior oblique muscle recession.
Of the three patients with the mixed fusion mechanism, partly using the presumed paretic superior oblique muscle to fuse vertically, one had an ipsilateral inferior oblique muscle recession and contralateral inferior rectus muscle recession, one had an ipsilateral inferior oblique muscle denervation and extirpation procedure, and one had an ipsilateral inferior oblique muscle moderate myectomy.
Discussion
In conclusion, we found three different patterns of vertical fusional vergence in our patients with “congenital unilateral SOP,” in agreement with earlier findings using scleral search coil recordings.9 These may be summarized by avoidance of the superior oblique muscle, by primarily using the vertical rectus muscles to fuse; primary use of the oblique muscles; and primary activation of the superior oblique muscle in the higher eye, and of the superior rectus muscle in the lower eye.
Do these different fusion mechanisms only represent different compensatory strategies, or do they also perhaps differentiate various forms of ocular motility patterns grouped together as “congenital SOP”?
Differences were present among the three groups of patients on Lancaster red-green testing. For example, the patients with vertical-rectus-muscle–mediated fusion, while all showing some amount of subjective extorsion between the two eyes, represent a heterogeneous group, with the hyperdeviation either increasing primarily in down gaze (Fig. 2A), increasing in adduction of the higher eye in both upgaze and down gaze (Fig. 2B), or increasing primarily in both adduction and down gaze of the higher eye.
In those vertical-rectus-muscle–mediated fusion patients with increasing hyperdeviation primarily in down gaze (Fig. 2A), the eye alignment pattern appears to reflect an inverted Brown pattern, that is, unilateral deficiency of depression in adduction, suggesting superior oblique muscle underaction, without significant ipsilateral inferior oblique muscle overaction (similar to the lack of significant superior oblique muscle “overaction” in a Brown syndrome).16 Note in Figure 2A that the greatest hyperdeviation is in depression and adduction, suggesting a left superior oblique muscle underaction. There is minimal left hyperdeviation in elevation and adduction, indicating only minimal right inferior oblique muscle overaction, therefore the designation as an “inverted Brown pattern.” This pattern has historically been felt to be caused by contracture of the superior rectus muscle on the side of the paretic superior oblique muscle, but, because the limitation of depression of the higher eye in down gaze disappears across the board with a large inferior oblique muscle weakening procedure alone,16 it now appears to be caused by an inferior oblique muscle that is tighter than its direct antagonist, the ipsilateral superior oblique muscle, consistent with forced traction testing of the oblique muscles at surgery in such patients (see the Table).
In the vertical-rectus-muscle–mediated fusion patients with increasing hyperdeviation of the eye moving into adduction (described by the term strabismus “sursoadductorius” in the European literature), as shown in Figure 2B, the eye alignment pattern, which is also interpretable as a relatively comitant cyclovertical deviation of the higher eye's movement pattern (combining extorsion and elevation), is caused by a shortened inferior oblique muscle in combination with a lengthened superior oblique muscle in the higher eye. This pattern is often referred to simply as “overaction” of the inferior oblique muscle in the higher eye in the non-European literature.
The patient with oblique-muscle–mediated vertical fusion exhibited essentially no subjective extorsion between the two eyes on Lancaster red-green testing and showed a comitant vertical deviation, as illustrated in Figure 2C.
As illustrated in Figure 2D, the patients with the mixed (oblique/rectus muscle) mechanism of vertical fusional vergence predominately showed an increasing hyperdeviation in adduction and in upgaze (also interpretable as extorsion and elevation of the higher eye's entire eye movement pattern), suggesting ipsilateral inferior oblique muscle overaction. These patients in the dissociated state showed the largest amount of subjective extorsion between the two eyes in straight-ahead gaze of all the groups (see the Table).
Contrary to vertical-rectus-muscle–mediated and oblique-muscle–mediated fusion, the oblique/rectus muscle fusion mechanism (involving activation of the ipsilateral superior oblique muscle and contralateral superior rectus muscle) results in a cyclovergence with intorsion of both eyes. The ratio of cyclovergence to vertical vergence for this mixed fusional mechanism was significantly greater than that for either of the other two fusional mechanisms (P < 0.05, see the Table). Thus, the mixed mechanism results in the greatest torsional change per degree of vertical deviation fused, whereas vertical-rectus-muscle–mediated fusion results in some, and oblique-muscle–mediated fusion results in essentially no torsional disparity per degree of vertical deviation fused.
It is tempting to speculate that a larger amount of resting state extorsion may influence the choice of the vertical fusional vergence mechanism, for the mixed mechanism provides intorsion of both eyes that could help compensate for the larger amount of extorsion in this group.
It is thus possible that the amount of extorsion a patient experiences influences the choice of fusion mechanism used: (1) if there is no or minimal subjective extorsion and a comitant deviation in the resting state, the “normal” mechanism for vertical fusional vergence, using both eye's oblique muscles,4 is used; (2) if there is some subjective extorsion between the two eyes present, the inferior rectus muscle of the higher eye and the superior rectus muscle of the lower eye (the latter providing some intorsion) tend to be used for vertical fusional vergence; and (3) if a significant amount of subjective extorsion between the two eyes is sensed, then both intorters are used, that is, the ipsilateral superior oblique muscle and the contralateral superior rectus muscle. This idea is in conflict with the prevailing notion that it is primarily the vertical disparity that is the stimulus for motor fusion in patients with SOP.17,18 However, if various strategies are available for reducing the vertical disparity, it is attractive to think that the strategy will be chosen that also best reduces the torsional disparity.
The mechanism used for vertical fusional vergence also may help guide the optimal surgical approach. For example, in our patients using the vertical rectus muscles to fuse, the superior rectus muscle in the higher eye is the direct antagonist of the inferior rectus muscle, which is one of those being used to fuse. Weakening of this superior rectus muscle, in addition to weakening the inferior oblique muscle, both in the higher eye, led to overcorrections, and might best be avoided. This is in accordance with previous studies in patients with strabismus sursoadductorius19,20 and with the inverted Brown pattern,16 which have shown that surgery performed on the ipsilateral inferior oblique muscle alone yields the best results.
The patients using the mixed (oblique/rectus muscle) fusion mechanism, on the other hand, might benefit from a “mixed” surgery, that is, weakening of the antagonists of the respective oblique/rectus muscles being used for fusion. In particular, as demonstrated in patient 9, if the problem in these patients is more a larger amount of extorsion, rather than hyperdeviation, then perhaps for this type of “congenital SOP,” the ideal surgical treatment may be surgery to weaken both extorters, that is, the ipsilateral inferior oblique muscle and the contralateral inferior rectus muscle.
Some limitations of our study should be discussed. First, a true acquired SOP comparison group would have been helpful. Second, additional measurements of cyclovertical fusional amplitude, as well as superior oblique muscle cross-sectional areas by magnetic resonance imaging, when fusing and when not fusing, might have helped better characterize the SOP patient groups.
Further investigations in more patients will be necessary to determine the true significance of the different fusion mechanisms, and may help to elucidate different causes for this motility pattern in different individuals (i.e., primary neurologic abnormality, versus primary or secondary8 muscle abnormality, versus primary orbital/trochlear7 abnormality), and may help further optimize approaches for surgical correction.
Acknowledgments
Supported in part by National Institutes of Health Grant R01 EY019347 (HSY).
Disclosure: K. Irsch, None; D.L. Guyton, None; H.-J. S. Park, None; H.S. Ying, None
References
- 1. Enright JT. Unexpected role of the oblique muscles in the human vertical fusion reflex. J Physiol. 1992; 451: 279–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Van Rijn LJ,, Collewijn H. Eye torsion associated with disparity-induced vertical vergence in humans. Vision Res. 1994; 34: 2307–2316. [DOI] [PubMed] [Google Scholar]
- 3. Cheeseman EW,, Guyton DL. Vertical fusional vergence: the key to dissociated vertical vergence in humans. Arch Ophthalmol. 1999; 117: 1188–1191. [DOI] [PubMed] [Google Scholar]
- 4. Irsch K,, Guyton DL,, Ramey NA,, Adyanthaya RS,, Ying HS. Vertical vergence adaptation produces an objective vertical deviation that changes with head tilt. Invest Ophthalmol Vis Sci. 2013; 54: 3108–3114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Özkan SB,, Aribal ME,, Sener EC,, Sanac AS,, Gürcan F. Magnetic resonance imaging in evaluation of congenital and acquired superior oblique palsy. J Pediatr Ophthalmol Strabismus. 1997; 34: 29–34. [DOI] [PubMed] [Google Scholar]
- 6. Chan TK,, Demer JL. Clinical features of congenital absence of the superior oblique muscle as demonstrated by orbital imaging. J Am Assoc Pediatr Ophthalmol Strabismus. 1999; 3: 143–150. [DOI] [PubMed] [Google Scholar]
- 7. DeSa LCF,, Good WV. Craniofacial anomalies and strabismus. : Good WV,, Hoyt CS, Strabismus Management. Oxford, UK: Butterworth-Heinemann; 1995: 128–129. [Google Scholar]
- 8. Guyton DL. Ocular torsion reveals the mechanisms of cyclovertical strabismus: The Weisenfeld Lecture. Invest Ophthalmol Vis Sci. 2008; 49: 847–857. [DOI] [PubMed] [Google Scholar]
- 9. Mudgil AV,, Walker M,, Steffen H,, Guyton DL,, Zee DS. Motor mechanisms of vertical fusion in individuals with superior oblique paresis. J AAPOS. 2002; 6: 145–153. [DOI] [PubMed] [Google Scholar]
- 10. Ramey NA,, Ying HS,, Irsch K,, Müllenbroich MC,, Vaswani R,, Guyton DL. A novel haploscopic viewing apparatus with a three-axis eye tracker. J AAPOS. 2008; 12: 498–503. [DOI] [PubMed] [Google Scholar]
- 11. Irsch K,, Ramey NA,, Kurz A,, Guyton DL,, Ying HS. Video-based head movement compensation for novel haploscopic eye tracking apparatus. Invest Ophthalmol Vis Sci. 2009; 50: 1152–1157. [DOI] [PubMed] [Google Scholar]
- 12. Christoff A,, Guyton DL. The Lancaster red-green test. Am Orthopt J. 2006; 56: 157–165. [DOI] [PubMed] [Google Scholar]
- 13. Hwang JM,, Guyton DL. The Lancaster red-green test before and after occlusion in the evaluation of incomitant strabismus. J AAPOS. 1999; 3: 151–156. [DOI] [PubMed] [Google Scholar]
- 14. Muthusamy B,, Chang HP,, Irsch K,, et al. Differentiating bilateral superior oblique paresis from sensory extorsion. J AAPOS. 2013; 17: 471–476. [DOI] [PubMed] [Google Scholar]
- 15. Guyton DL. Exaggerated traction test for the oblique muscles. Ophthalmology. 1981; 88: 1035–1040. [DOI] [PubMed] [Google Scholar]
- 16. Awadein A,, Pesheva M,, Guyton DL. “Inverted Brown pattern”: A tight inferior oblique muscle masquerading as superior oblique underaction—clinical characteristics and surgical management. J AAPOS. 2006; 10: 565–572. [DOI] [PubMed] [Google Scholar]
- 17. Guyton DL,, von Noorden GK. Sensory adaptations to cyclodeviations. : Reinecke RD, Strabismus: Proceedings of the Third Meeting of the International Strabismological Association. New York: Grune & Stratton; 1978; 399–403. [Google Scholar]
- 18. von Noorden GK. Clinical observations in cyclodeviations. Ophthalmology. 1979; 86: 1451–1461. [DOI] [PubMed] [Google Scholar]
- 19. Klainguti G. Strabisme surso-adducteur décompensé. Klin Monatsbl Augenheilkd. 2004; 221: 298–303. [DOI] [PubMed] [Google Scholar]
- 20. Schmidt S,, Gräf M,, Kaufmann H,, Lorenz B. Behandlung des Stabismus sursoadductorius (congenital superior oblique palsy) im Kindesalter. Klin Monatsbl Augenheilkd. 2011; 228: 874–879. [DOI] [PubMed] [Google Scholar]