Abstract
Background:
Laparoscopic spleen-preserving distal pancreatectomy (LSPDP) is an ideal procedure in selected patients with benign or low-grade malignant tumors in the body/tail of the pancreas. We describe our procedure and experience with splenic vessel-preserving LSPDP (SVP-LSPDP) in a retrospective case series.
Methods:
Six consecutive patients underwent SVP-LSPDP from January 2011 to September 2013. We evaluated the courses of the splenic artery by preoperative computed tomography and applied an individualized approach (the superior approach or inferior approach) to the splenic artery.
Results:
All of the operations were successful. The median surgical duration was 249 minutes. The median blood loss was 0 mL. Pathologic examination revealed 4 cases of insulinoma, 1 case of solid pseudopapillary tumor, and 1 case of pancreatic metastasis from renal carcinoma.
Conclusions:
In performing SVP-LSPDP, it is effective to make a strategic choice between 2 different approaches according to the course of splenic artery.
Key Words: pancreatic benign/low-grade malignant tumor, laparoscopic distal pancreatectomy, spleen preserving, splenic vessel preserving, splenic artery, computed tomography
Splenic preservation is associated with a reduction in perioperative infectious complications,1,2 postoperative pancreatic fistulas,3,4 and cancer occurrence.5,6 Therefore, in patients with benign or low-grade malignant tumors in the body and/or tail of the pancreas, spleen-preserving distal pancreatectomy is preferred over combined splenectomy. Furthermore, improvement in procedural feasibility and safety improvement have made laparoscopic spleen-preserving distal pancreatectomy (LSPDP) more common.3,7–12 To preserve the spleen, 2 surgical techniques can be used: (1) dissecting out the splenic artery and vein with division of the arterial and venous branches between the pancreas and the splenic artery and vein or (2) resection of the splenic artery and vein along with the pancreas but with careful preservation of the vascular collaterals in the splenic hilum, which allows the spleen to survive on the short gastric vessels (Warshaw technique).13 A recent study compared short-term outcomes between the preservation and the division of the splenic vessels during LSPDP, showing that the former was associated with an improved rate of spleen conservation.12 This procedure may become the strategy of choice in selected patients with benign or low-grade malignant tumors in the body/tail of the pancreas.
In contrast, LSPDP with preservation of the splenic vessels is technically demanding. Splenic vessel injuries or difficulties during the dissection occasionally require a conversion to the Warshaw technique.12 Hence, the approach to the splenic vessels is an important step. The present study describes the standard operating procedure for splenic vessel-preserving LSPDP (SVP-LSPDP) in our institute, and 2 types of approaches to the splenic artery are highlighted.
MATERIALS AND METHODS
Patients
A total of 6 patients, including 5 females and 1 male (median age, 70 y; age range, 37 to 80 y), were recruited consecutively from January 2011 to September 2013. Patients underwent SVP-LSPDP at the authors’ institution. They gave informed consent for operative management. The indication for surgery was the presence of tumors that were presumed to be benign or low grade, and 1 metastatic pancreatic tumor of renal cell carcinoma was included. The tumors were confined to the body and/or tail of the pancreas.
A preoperative endoscopic ultrasound-guided biopsy was performed in 3 patients, which confirmed neuroendocrine tumor in 2 patients and solid pseudopapillary neoplasm in 1 patient.
All patients routinely underwent imaging studies, including computed tomography (CT), during preoperative evaluations. In addition to the tumor localization, we focused on the courses of splenic arteries and classified them into 1 of 2 major types (Figs. 1A, B):
FIGURE 1.
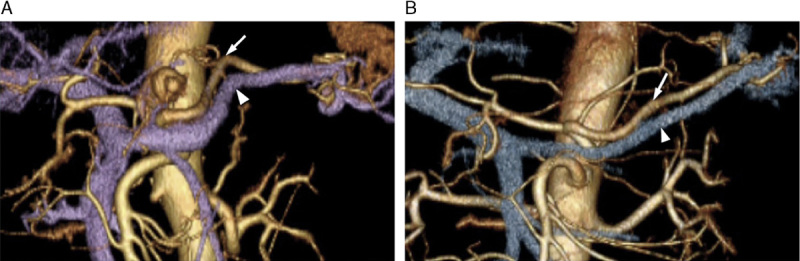
Three-dimensional computed tomography showing 2 types of splenic arteries. A, Type A. B, Type B. Arrow, splenic artery; arrowhead, splenic vein.
Type A: The splenic artery curved and ran superior to the pancreas.
Type B: The splenic artery passed relatively straight to the dorsal side of the pancreas.
There were 4 cases of the Type A splenic artery and 2 case of the Type B splenic artery.
Surgical Procedure
Patients were placed in the supine reverse Trendelenburg position with their legs apart under general anesthesia. The first trocar was placed in the umbilicus, and an electrolaparoscope (WA50013; Olympus Medical Systems, Tokyo, Japan) was inserted into the peritoneal cavity. The intra-abdominal pressure was set at 10 mm Hg. Under direct vision, a 12-mm trocar was inserted at the left paraxiphoid, followed by two 12-mm trocars in the bilateral subcostal areas, and a 5-mm trocar along the left anterior axillary line. The surgeon stood between the legs of the patient, with the first assistant standing on the right, and the camera operator standing on the left of the operating surgeon. We used laparoscopic coagulation shears (SONOSURG-X; Olympus Medical Systems, Tokyo, Japan) for dissection and vessel coagulation.
The left hepatic lobe was kept elevated, using a laparoscopic retractor through the left paraxiphoid trocar. The greater omentum was divided below the gastroepiploic arch to open a window to the bursa omentalis. Then, the window was enlarged to expose the pancreas, while the left gastroepiploic vessels and short gastric vessels were preserved. Laparoscopic ultrasonography was used supportively to identify the location of the tumor, and a surgical resection line was predetermined. When the course of the splenic artery was Type A, the peritoneum was cut along the superior pancreatic border to expose and tape the splenic artery at the dividing line (the superior approach) (Fig. 2A).
FIGURE 2.
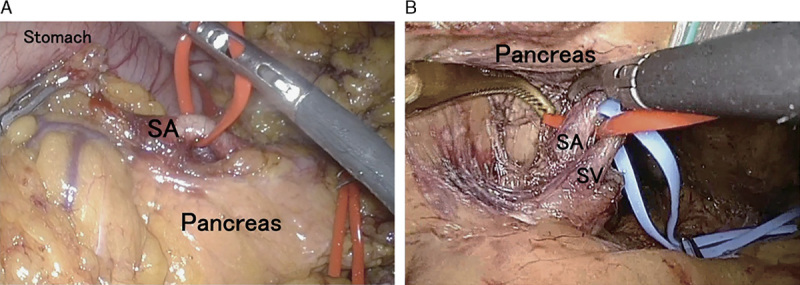
Approach to the splenic artery. A, Superior approach. B, Inferior approach. SA indicates splenic artery; SV, splenic vessel.
The inferior margin of the pancreatic body was liberated toward the splenic lower pole. Then, the pancreatic body was separated from the retroperitoneum until the splenic vein could be visualized. At the pancreas dividing line, the splenic vein was dissected and taped from the inferior pancreatic border. Paying close attention, the short branches of the splenic vein were sealed using laparoscopic coagulation shears or a vessel-sealing device (LigaSure; Covidien, Norwalk, CT).
When the course of the splenic artery was Type B, the artery was exposed and taped using the same procedure as that used for the vein (the inferior approach) (Fig. 2B).
After the separation of pancreas from the splenic vessels, a linear stapler was inserted between the parenchyma and vessels. The stapler (Endo-GIA Tri-Staple, black cartridge; Covidien, Norwalk, CT) was inserted through the right subcostal trocar. The pancreatic parenchyma was compressed and cut.
Pulling the distal pancreas ventrally allowed for dissection along the splenic vessels to the splenic hilum. The branches supplying the pancreas were sealed or clipped carefully. The specimen was retrieved in an endoscopic bag and extracted through the enlarged umbilicus incision.
Postoperative Complications
Postoperative complications were graded on the Clavien-Dindo classification.14 Pancreatic fistulas were defined according to the International Study Group on Pancreatic fistulas (ISGPF).15
Patency of the Splenic Vessels and the Perfusion of the Spleen
According to the classification system defined by Yoon et al,16 we classified patency of the splenic vessels and perfusion of the spleen. Briefly, patency of the splenic vessels was classified into 3 grades: intact (grade 0), partial occlusion or thrombosis (grade 1), and total occlusion or not identified (grade 2), whereas splenic perfusion was grouped into 4 grades: intact (grade 0), <50% infarction of total splenic volume (grade 1), 50% or more infarction (grade 2), and 100% infarction (grade 3). All patients routinely underwent CT before discharge (early CT assessment) and during outpatient clinic-based follow-up (late CT assessment). Two radiologists reviewed CT retrospectively and evaluated the blood flow of vessels and spleens in consensus.
Clinicopathologic Findings
A retrospective analysis was performed regarding the operative duration, blood loss, postoperative complications, postoperative length of stay, and pathologic findings. All values are expressed as median (range).
RESULTS
None of the patients required conversion to an open procedure. All patients’ spleens and splenic vessels were successfully preserved. The median operative time was 249 minutes (range, 218 to 392 min). The median blood loss was 0 mL (range, 0 to 210 mL). No blood transfusions were administered. There were no postoperative deaths. A pancreatic fistula (ISGPF Grade B) occurred in 1 patient. Two patients developed symptomatic intra-abdominal fluid collection (Clavien-Dindo Grade II). The postoperative length of hospital stay was 16.5 days (range, 12 to 25 d). Histopathologic examination of the surgical specimens revealed 4 cases of insulinoma, 1 case of solid pseudopapillary tumor, and 1 case of metastatic pancreatic cancer of renal cell carcinoma. The diameter of tumors was 10 mm (range, 6 to 22 mm).
Early CT assessment was performed at a median of 7 days (range, 6 to 11 d) postoperatively, whereas late CT assessment was performed at a median of 20 months (range, 7 to 27 mo). No case of complete obliteration was observed in the splenic artery or vein, whereas grade 1 stenosis in the preserved artery and vein was observed in 4 and 5 patients, respectively, during the early postoperative period and in 0 and 1 patients, respectively, during the follow-up period. One patient had grade 1 splenic infarction (<10%), which appeared within a month of operation and which persisted during follow-up. In addition, another patient was preoperatively noted to have a peripheral arterial aneurysm in the splenic artery and underwent transcatheter arterial embolization. As a result, this patient had grade 1 splenic infarction during the follow-up.
DISCUSSION
The prime difficulty in SVP-LSPDP is the fact that the splenic vessels are often embedded in the sulcus of the pancreatic parenchyma, and branches of the splenic vessels are fine and easily injured.7,8,17 Furthermore, splenic vessels vary among patients; while there are marked variations in the tortuosity of the splenic artery from its origin to the point of commencement of the hilar branches, the splenic vein is invariably straight.18 Therefore, in an effort to avoid damaging the vessels and to avoid unwanted bleeding, it is important to approach the splenic artery in an individualized fashion. Recent advancements in multiplanar and 3-dimensional reconstruction techniques in CT enable depiction of detailed information regarding the splenic arteries. Herein, we evaluated the courses of the splenic arteries preoperatively by CT and classified them into 2 major types for the surgical approach.
Both types of approaches to the splenic artery (the superior approach and the inferior approach) can be performed by laparoscopic surgery. In previous reports, the splenic artery was dissected out either by the superior approach or by inferior approach,8,7,16,17,19 but the comparative utility of these 2 approaches has not been clearly reported. An individualized approach for each patient makes it possible to expose and tape the artery in the shortest course, with minimal contact with pancreatic parenchyma and the splenic vein. This strategy may lead to shorter operative time and lower amounts of bleeding. In our series, both approaches (4 patients by the superior approach, 2 patients by the inferior approach) were able to be carried out safely and successfully with relatively stable operative time and minimal blood loss and without converting to Warshaw technique or combining splenectomy. A recent study reported an intention-to-treat analysis of intraoperative outcomes of SVP-LSPDP on 55 patients: the mean (SD) operative time was 214.7 (66.7) minutes, and mean (SD) blood loss 342.8 (223.5) mL, the conversion rate to laparotomy or Warshaw procedure was 9%, 21.8%, respectively.12 When compared with the report, our result was thought to be acceptable. Use of a 1-side approach only may result in increased operating time and increased risk of vessel injuries in the case of an opposite arterial course.
In contrast, another study has shown that the patency of the splenic vessels cannot always be preserved, even after SVP-LSPDP.16 After analyzing the patency of the splenic vessel in 22 patients who underwent SVP-LSPDP, no cases of total occlusion of the splenic artery were observed after surgery while total occlusion of the splenic vein was found in 7 (31.8%) patients within 1 month of surgery and in 10 (45.5%) patients within 6 months or more after surgery.16 They have also reported that, although partial vascular occlusion may change in follow-up, total vascular occlusion is less likely to improve.16 In our study of 6 patients, none of the patients had complete splenic vessel obliteration. As a consequence, neither severe splenic infarctions nor prominent perigastric varices, which require postoperative intervention, were observed during the follow-up period. In 1 patient, persistent partial splenic infarction (<10%) was observed after the operation despite the intact splenic vessels. The discrepancy may be due to the resection of the peripheral splenic artery during the operation. In the meantime, partial occlusion in the splenic vessels was found in some patients during this follow-up. Hwang et al20 suggested that obliteration in splenic vessels was related to frequent bleeding and vascular manipulation due to close and long activation of the laparoscopic coagulation shears. Therefore, development of strategies that minimize vascular manipulation and damage are needed.
In this article, we described our strategy for SVP-LSPDP based on the exact preoperative evaluation of the splenic artery. Although our experience is limited, we believe that it is worthwhile to apply either the superior approach or the inferior approach as appropriate according to the course of the splenic artery. Needless to say, more experience and skills are needed to make our procedure a standard technique.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Carrere N, Abid S, Julio CH, et al. Spleen-preserving distal pancreatectomy with excision of splenic artery and vein: a case-matched comparison with conventional distal pancreatectomy with splenectomy. World J Surg. 2007;31:375–382. [DOI] [PubMed] [Google Scholar]
- 2.Shoup M, Brennan MF, McWhite K, et al. The value of splenic preservation with distal pancreatectomy. Arch Surg. 2002;137:164–168. [DOI] [PubMed] [Google Scholar]
- 3.Choi SH, Seo MA, Hwang HK, et al. Is it worthwhile to preserve adult spleen in laparoscopic distal pancreatectomy? Perioperative and patient-reported outcome analysis. Surg Endosc. 2012;26:3149–3156. [DOI] [PubMed] [Google Scholar]
- 4.Kang CM, Chung YE, Jung MJ, et al. Splenic vein thrombosis and pancreatic fistula after minimally invasive distal pancreatectomy. Br J Surg. 2014;101:114–119. [DOI] [PubMed] [Google Scholar]
- 5.Mellemkjaer L, Olsen JH, Linet MS, et al. Cancer risk after splenectomy. Ugeskr Laeger. 1995;157:5097–5100. [PubMed] [Google Scholar]
- 6.Schwarz RE, Harrison LE, Conlon KC, et al. The impact of splenectomy on outcomes after resection of pancreatic adenocarcinoma. J Am Coll Surg. 1999;188:516–521. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez-Cruz L, Martinez I, Gilabert R, et al. Laparoscopic distal pancreatectomy combined with preservation of the spleen for cystic neoplasms of the pancreas. J Gastrointest Surg. 2004;8:493–501. [DOI] [PubMed] [Google Scholar]
- 8.Melotti G, Butturini G, Piccoli M, et al. Laparoscopic distal pancreatectomy: results on a consecutive series of 58 patients. Ann Surg. 2007;246:77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beane JD, Pitt HA, Nakeeb A, et al. Splenic preserving distal pancreatectomy: does vessel preservation matter? J Am Coll Surg. 2011;212:651–657. discussion 657–658. [DOI] [PubMed] [Google Scholar]
- 10.Song KB, Kim SC, Park JB, et al. Single-center experience of laparoscopic left pancreatic resection in 359 consecutive patients: changing the surgical paradigm of left pancreatic resection. Surg Endosc. 2011;25:3364–3372. [DOI] [PubMed] [Google Scholar]
- 11.Butturini G, Inama M, Malleo G, et al. Perioperative and long-term results of laparoscopic spleen-preserving distal pancreatectomy with or without splenic vessels conservation: a retrospective analysis. J Surg Oncol. 2012;105:387–392. [DOI] [PubMed] [Google Scholar]
- 12.Jean-Philippe A, Alexandre J, Christophe L, et al. Laparoscopic spleen-preserving distal pancreatectomy: splenic vessel preservation compared with the Warshaw technique. JAMA Surg. 2013;148:246–252. [DOI] [PubMed] [Google Scholar]
- 13.Warshaw AL. Distal pancreatectomy with preservation of the spleen. J Hepatobiliary Pancreat Sci. 2010;17:808–812. [DOI] [PubMed] [Google Scholar]
- 14.Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196. [DOI] [PubMed] [Google Scholar]
- 15.Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13. [DOI] [PubMed] [Google Scholar]
- 16.Yoon YS, Lee KH, Han HS, et al. Patency of splenic vessels after laparoscopic spleen and splenic vessel-preserving distal pancreatectomy. Br J Surg. 2009;96:633–640. [DOI] [PubMed] [Google Scholar]
- 17.Nakamura M, Nagayoshi Y, Kono H, et al. Lateral approach for laparoscopic splenic vessel-preserving distal pancreatectomy. Surgery. 2011;150:326–331. [DOI] [PubMed] [Google Scholar]
- 18.Sylvester PA, Stewart R, Ellis H. Tortuosity of the human splenic artery. Clin Anat. 1995;8:214–218. [DOI] [PubMed] [Google Scholar]
- 19.Ding X, Tan J, Qian J. Laparoscopic spleen-preserving distal pancreatectomy (LSPDP). Hepatogastroenterology. 2013;60:605–610. [DOI] [PubMed] [Google Scholar]
- 20.Hwang HK, Chung YE, Kim KA, et al. Revisiting vascular patency after spleen-preserving laparoscopic distal pancreatectomy with conservation of splenic vessels. Surg Endosc. 2012;26:1765–1771. [DOI] [PMC free article] [PubMed] [Google Scholar]


