Abstract
Ineffective parenting practices may maintain or exacerbate attention deficit/hyperactivity disorder (ADHD) symptoms and shape subsequent development of disruptive behavior disorders (DBD’s) in youth with ADHD. Recent theoretical models have suggested that parenting may exert effects on ADHD via its role in child temperament. The current study aimed to evaluate the indirect effects of parenting dimensions on child ADHD symptoms via child temperament. Youth ages 6–17 years (N=498; 50.4 % ADHD, 55 % male) completed a multi-stage, multi-informant assessment that included parent, child, and teacher report measures of parenting practices, child temperament, and ADHD symptoms. Statistical models examined the direct and indirect effects of maternal and paternal involvement, poor supervision, and inconsistent discipline on inattention and hyperactivity-impulsivity via child temperament and personality traits. Results indicated differential patterns of effect for negative and positive parenting dimensions. First, inconsistent discipline exerted indirect effects on both ADHD symptom dimensions via child conscientiousness, such that higher levels of inconsistency predicted lower levels of conscientiousness, which in turn, predicted greater ADHD symptomatology. Similarly, poor supervision also exerted indirect effects on inattention via child conscientiousness as well as significant indirect effects on hyperactivity-impulsivity via its impact on both child reactive control and conscientiousness. In contrast, primarily direct effects of positive parenting (i.e., involvement) on ADHD emerged. Secondary checks revealed that similar pathways may also emerge for comorbid disruptive behavior disorders. Current findings extend upon past work by examining how parenting practices influence child ADHD via within child mechanisms and provide support for multi-pathway models accounting for heterogeneity in the disorder.
Keywords: Parenting, Temperament, ADHD, Multiple mediation
Attention Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with adaptive functioning and development (e.g., difficulties in peer/social relationships, academic underachievement; American Psychiatric Association 2013). While prior research has demonstrated that this disorder is highly heritable (~70 %; Nikolas and Burt 2010), psychosocial context is crucial to its developmental course via multiple directional and bidirectional parent–child interchanges (Nigg et al. 2006). In particular, parenting behaviors such as quality of caregiving, and parent–child relationships are associated with ADHD (Barkley 1998; Ellis and Nigg 2009; Hawes et al. 2013; Martel et al. 2011), perhaps contributing to persistence and amplification of ADHD symptoms (Campbell et al. 2014). Effects are likely to be complex, including genotype-environment correlation (both parent and child may have difficult temperaments, for example), parent-driven effects, child-driven effects, and recursive processes. Children with ADHD have been described as demanding, moody, and uncooperative, which may make it particularly difficult for parents to effectively manage their children’s behavior (Johnston and Mash 2001; Mash and Johnston 1982; White 1999). Further, problematic parenting, including poor supervision and monitoring, has also been observed among parents, with ADHD, which may exacerbate child behavioral difficulties (Modesto-Lowe et al. 2008).
In addition to its relevance to ADHD, parenting has long been cited as an important contributor to child externalizing problems more generally (Marmorstein and Iacono 2004; Patterson et al. 1989). However, because most children with oppositional defiant (ODD) and conduct disorder (CD) also have ADHD, reviews have been forced to note ambiguity regarding whether parenting specifically influences ADHD (Deault 2010; Johnston and Mash 2001). Some past work has shown that ineffective parenting practices (i.e., inconsistent discipline, low involvement) are associated with child ADHD symptoms (Johnston and Jassy 2007; Lindahl 1998), even after controlling for comorbid ODD and CD (Ellis and Nigg 2009). However, other lines of research have indicated that negative parenting behaviors, including inconsistent discipline, may predict and exacerbate the development of subsequent child disruptive behavior disorders (DBDs) among youth with ADHD (Deault 2010; Johnston 1996; Johnston and Jassy 2007). Parenting effects on ADHD and DBDs may also be dependent upon child genotype (Martel et al. 2011). Taken together, suboptimal parenting practices appear to compound child ADHD symptoms, potentially leading to the development of comorbid problems.
So how might parenting influence or exacerbate ADHD symptoms? One potential mechanism is that parenting may shape children’s temperamental self-regulation capabilities, which in turn are salient predictors of children’s adjustment (Kiff et al. 2011; Rothbart and Bates 2006). We make five fundamental observations about child temperament to set the stage for this study. First, child temperament can be defined as individual variation in reactivity and self-regulation abilities, and temperament-related behavior involves tendencies to positive emotionality (sometimes labeled as surgency or extraversion), negative emotionality (sometimes labeled as neuroticism), agreeableness/hostility (sometimes seen as personality rather than temperament), and capacity to effortfully control cognition, attention, and emotion (Eisenberg et al. 1996, 2005; Finzi-Dottan et al. 2006; Nigg 2006b; Rothbart 2012). While temperament was traditionally seen as biological and heritable, contemporary understanding recognizes that surface behavioral traits seen as temperament are only moderately heritable and are also influenced by socialization (Deater-Deckard 2014; Nigg 2006b; Rothbart 2012).
Second, because they are attempting to describe child behavior, temperament and psychopathology are both influenced by genetic and psychosocial factors and inevitably compete to describe some of the same behavioral terrain. Indeed, effortful control and ADHD both appear to be underpinned by similar executive processes (Berlin et al. 2004; Bridgett et al. 2013). Nonetheless, temperament traits can be conceptually and empirically distinguished from ADHD (Lahey 2004; Martel and Nigg 2006; Nigg 2006b; Nigg et al. 2004). Temperament can be thought of as an individual liability (or protective) factor for subsequent emergence of ADHD. It is conceptually an early emerging set of behavioral tendencies that may set the stage or create vulnerability for ADHD.
Third, temperament necessarily includes psychosocial inputs as well. A recent theoretical model posited by Deater-Deckard (2014) amplifies the idea that the development and maintenance of self-regulation, a key aspect of temperament, is influenced by familial factors, including parenting. That is, through socialization during childhood and adolescence, parents manage the home environment and both scaffold and model appropriate behavior and self-regulation for their children. Ineffective or suboptimal parenting (e.g., insufficient parental responsiveness/warmth) may then disrupt the trajectory of self-regulation development (Bernier et al. 2012; Davidov and Grusec 2006), contributing to the onset and maintenance of child psychopathology including ADHD (Kim and Deater-Deckard 2011; Nigg 2000; Nigg et al. 2004). It is important to note, however, that parenting behaviors themselves are, in turn, shaped over time by the ongoing development of child self-regulatory capacities (Kaiser et al. 2010; Kiff et al. 2011), which strengthen as youth mature (Best and Miller 2010).
Fourth, several temperament traits are promising tools for describing and understanding heterogeneity in ADHD. Specifically, different levels of child temperament characteristics (e.g., low conscientiousness to inattention, low reactive control to hyperactivity) partially map onto the well-established ADHD sub-domains of inattention and hyperactivity-impulsivity (Martel and Nigg 2006; Nigg et al. 2004). Further, children with temperamentally-defined low effortful control and high impulsivity (an ADHD-like profile) have consistently been found to be more susceptible to the negative effects of ineffective parenting practices (Kiff et al. 2011).
Finally, with respect to developmental cascade models as well as etiological pathways to ADHD, child temperament traits can be seen not only as a liability factor of ADHD but also can be posited as a useful early developmental phenotype or precursor of ADHD (Martel et al. 2012; Nigg et al. 2004). The principal focus of the present study, while keeping these considerations and models in mind, is to address how child temperament traits and positive and negative parenting behaviors come together to statistically predict the severity of ADHD symptomatology.
Prior work has suggested that indirect effects, such as those proposed in the model by Deater-Deckard (2014) may be one way for understanding how these processes converge in the development of ADHD and other externalizing disorders. For instance, inadequate parenting practices have been found to influence child ODD and CD symptoms via their association with levels of effortful control in children (Chang et al. 2011). Empirical work has yet to test the hypothesis that parenting may be indirectly associated with ADHD symptoms via its relation with child temperament. For this hypothesis to be true, it should at minimum hold in cross sectional data; affirmation there could justify a more ambitious longitudinal investigation.
Yet, even if such effects are seen, it is unlikely that the association of parenting with child ADHD symptoms is statistically mediated through one single child temperament trait. Prior work suggests that multi-trait descriptors are needed to understand ADHD (Martel and Nigg 2006). Therefore, we aimed to test indirect effects in such a way as to allow for the concurrent examination of several statistical mediators. Methodologically this approach is also advantageous because multiple mediation is more parsimonious than single mediation as these models can simultaneously examine the combined and unique indirect effects of each individual temperament trait, while also taking into account their inter-correlations with one another.
By investigating the indirect association of parenting on ADHD via temperament, this study extends upon past work by examining how parenting behavior and within-child mechanisms simultaneously shape ADHD symptom dimensions, as well as illuminate more nuanced contributions to the multiple pathways of ADHD and comorbid DBDs. The aim of the current study was to examine if parenting dimensions exerted indirect effects on ADHD symptoms via their impact on child temperament traits. Using a cross-sectional design, we hypothesized that, in general, indirect effects of parenting on ADHD symptoms would indeed emerge, such that parenting dimensions would impact ADHD symptoms via child temperament traits. Additionally, based on prior work by Martel and Nigg (2006) and Ellis and Nigg (2009), two traits of particular interest included effortful control/conscientiousness and reactive control (Eisenberg et al. 2005), as these traits are important components of self-regulation and have been implicated in developmental pathways to ADHD.
Method
Participants
Participants were 498 youth ages 6–17 years- old (M= 10.8 years, SD=2.3 years; 55 % male). Participants were recruited from the community using several strategies in order to avoid the biases inherent in a purely clinic-referred sample. Recruitment tools included mass mailings to parents in the neighboring school districts, posting of public advertisements, and community outreach to local clinics. Racial and ethnic composition of the sample was similar to the surrounding area (73.3 % Caucasian, 8.8 % African-American, 5.0 % Hispanic/Latino, 11.2 % multi-ethnic) as were levels of parental education (51.0 % of mothers and 53.7 % of fathers reported completing high school or some college, whereas 26.1 % of mothers and 27.1 % of fathers reported completing a Bachelor’s degree). Youth and their parents completed a multi-stage, multi-informant assessment procedure to determine ADHD diagnostic status as well as the presence and absence of co-morbid disorders.
During stage 1, a parent completed a telephone screen to assess for exclusion criteria, which included a child history of intellectual disability, neurological impairments, seizure history, physical handicap, autistic disorder, or prescription of long-acting psychoactive medications (e.g., bupropion, anti-depressants). At stage 2, parents and their children completed a diagnostic testing visit. During the visit, parents completed a semi-structured interview, the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS-E; Puig-Antich and Ryan 1986) with trained masters level clinicians to evaluate onset, occurrence, persistence, and impairment for DSM-IV Axis I disorders, including ADHD. Interviewers all viewed and scored a common set of 20 KSADS-E interviews to ensure reliability with a standard. Agreement rates were moderate to high for ratings of ADHD symptoms of inattention (κ= 0.94) and hyperactivity–impulsivity (κ=0.81) as well as for comorbid DSM–IV diagnoses with a base rate of 5 % or greater (κs ranged from 0.74 to 0.92). Teachers and parents also completed several standardized rating scales, including the DSM-IV ADHD Rating Scale (DuPaul et al. 1998) and the Conners’ Revised Rating Scale (Conners 1997). Teachers and parents were instructed to rate and describe their child’s behavior off of their medication. While parents met with the interviewer during the diagnostic visit, children completed IQ and academic achievement assessments.
To determine final diagnostic status for participating youth, data from the parent and teacher rating scales combined with interview notes, observations, and history of treatment were evaluated by a diagnostic team comprised of a board-certified child psychiatrist and licensed child psychologist. Each professional arrived independently at a diagnosis for ADHD and all other Axis I disorders using a best-estimate procedure; any disagreements were resolved upon discussion. Their independent agreement rates were acceptable for all diagnoses with base rate >5 % in the sample (all ks>0.75) and agreement for ADHD, ODD, and CD were all acceptable (all ks>0.80). Based on these procedures, the final sample included 498 youth, which was comprised of 251 ADHD cases and 213 non-ADHD controls. Additionally, 34 youth had subthreshold/situational ADHD (e.g., 5 symptoms in one dimension or lack of cross-informant convergence on symptom presence between parents and teachers.) These youth were excluded for all tests of group differences, but included for all tests of dimensional associations. All study procedures were approved by the local Institutional Review Board. Parents provided written consent and children provided written assent.
Measures
Following the diagnostic visit, eligible families were invited to return to a second lab visit. Youth completed a neuropsychological testing battery as well as questionnaires regarding parenting. Parents completed measures of their child’s temperament. The key measures included in the current study are listed below.
ADHD Symptoms
Parents and teachers completed the DSM-IV ADHD Rating Scale (DuPaul et al. 1998), which asks informants to rate children on the core characteristics of ADHD (i.e., inattention, hyperactivity, and impulsivity) on a Likert-scale (0–3), indicating whether each symptom occurs “Never or Rarely,” “Sometimes,” “Often,” or “Very Often” for the child. The DSM-IV is in line with DSM-5 such that informants evaluate children on two dimensions of ADHD including 9 symptoms of inattention and 9 symptoms of hyperactivity-impulsivity. The final sum score for parent and teacher ratings of symptom dimensions were retained and a mean composite was computed for all subsequent analyses, based on recent work suggesting enhanced validity of average ratings (Martel et al. 2015). Internal consistencies for the inattention (α parent=0.93, α teacher=0.91) and hyperactivity (α parent=0.90, α teacher = 0.88) scales were adequate.
CD and ODD Symptoms
Parent report on the KSADS-E (Puig-Antich and Ryan 1986) was used to assess symptoms of ODD and CD. The KSADS-E asks parents to rate the presence or absence of the 8 DSM-IV ODD symptoms and 15 DSM-IV CD symptoms. Additionally, teachers provided Likert ratings (never, sometimes, often, and very often) for 8 CD items and 8 ODD items from the DBD rating scale (Pelham et al. 1992); a sum score was then computed and retained for subsequent analyses. Internal consistencies were adequate for teacher report of both CD (α=0.81) and ODD (α=0.94).
Child Temperament Characteristics
Parents also completed the common language version of the California Child Q-Sort (CCQ; Caspi et al. 1992) to assess youth temperament traits. Similar to a standard Q-Sort methodology, the CCQ has 100 cards that must be placed in a forced-choice, nine-category rectangular distribution. The informant rates child temperament traits by placing the descriptive cards in one of the nine categories. These categories range from one (least descriptive) to nine (most descriptive). The CCQ has been used to assess temperament across development during childhood and adolescence (Eisenberg et al. 2005; Martel et al. 2007). Five temperament traits were assessed using the Q-sort: reactive control, resiliency, negative emotionality, conscientiousness (proxy for effortful control), and agreeableness, based on prior theoretical conceptualizations (Eisenberg et al. 1996, 2005) and empirical work linking temperament traits to the development of ADHD and comorbid externalizing behaviors (Martel and Nigg 2006; Martel et al. 2007). Reactive control is conceptualized as the automatic modulation of emotion and behavior and is conceptualized as related to bottom up response systems in the brain, whereas effortful control (or conscientiousness) is defined as the relatively intentional cognitive control of emotional states and subsequent behavior and is likely associated with the top-down processes in the brain. Negative emotionality is the inclination for individuals to experience negative emotion such as anxiety or stress (Eisenberg et al. 1996) and is thought to be associated with general emotion dysregulation and DBDs (Sanson and Prior 1999). Finally, resiliency is defined as the ability to shift the modulation of reactive and effortful control depending on the context of a situation (Eisenberg et al. 1996). All traits demonstrated adequate internal consistency (αs range from 0.73 to 0.84).
To avoid the potential confound that could result from inclusion of identical or near-identical items (i.e., artificially inflated correlations between personality traits and symptoms) between traits and ADHD measures, items were rated for similarity by two raters. Items that were judged by both raters as identical or near identical were removed from the temperament or ADHD scale so long as adequate scale reliability could be retained, as detailed in (Martel and Nigg 2006). This resulted in the removal of 2 items from reactive control, 1 from effortful control, 3 inattention, and 2 items from the hyperactivity-impulsivity scale to avoid overlap with ADHD. No overlapping items with ODD or CD were identified.
Parenting Behaviors
The Alabama Parenting Questionnaire (APQ) was administered to participating youth to evaluate parenting styles (Shelton et al. 1996). This 42-item scale assesses different dimensions of parenting behaviors (e.g., parental involvement, poor monitoring/supervision, and inconsistent discipline). Past work indicates this measure demonstrates adequate reliability (Ellis and Nigg 2009; Essau et al. 2006) and convergent validity, displaying substantial and statistically significant correlations with interviews about parenting (Essau et al. 2006). Questions were read to children under the age of 12 in order to ensure comprehension of the items and completeness. Four subscales from the APQ were of interest in the current study; maternal and paternal involvement (e.g., “Your parent asks you about your day in school,” α= 0.79 for paternal involvement, α=0.81 for maternal involvement; poor monitoring/supervision, e.g., “You go out after dark without an adult with you,” α=0.77; inconsistent discipline, e.g., “You talk your parents out of punishing you after you have done something wrong,” α=0.71). Harsh discipline was omitted due to low reliability (α=0.49).
Data Analysis
Data analysis was performed using the Mplus software package (Muthen and Muthen 1998–2013). The use of robust maximum likelihood estimation with the Mplus software package allows for statistical control of normality and outliers. To address non-independence of sibling data (sample included 205 sibling pairs and 88 singleton children), Mplus uses a clustering feature that takes into account the non-independence of the data when testing models for significance and computing test statistics.
Descriptive statistics and group differences were examined through the use of chi-square statistics and t-tests. Bivariate correlations were performed in order to examine associations between variables. Finally, we tested for direct and indirect effects based on methodology by Preacher and Hayes (2008) using full information maximum likelihood techniques to address any missing data. In each model, parenting dimensions (child report) were entered as the predictor variable and ADHD symptom dimensions (mean composite of parent and teacher reports) were the outcome measure. Temperament traits (all parent report) of reactive control, resiliency, negative emotionality, conscientiousness (for effortful control), and agreeableness were examined simultaneously as multiple statistical mediators of the association between parenting and ADHD symptoms. Both the total indirect effects and the point estimates for each trait are estimated using this procedure. Sex, age, ethnicity, ODD and CD symptoms were included as covariates in all models.
Preacher and Hayes (2008) enumerate numerous advantages to specifying and testing one multiple mediation model versus separate simple mediation models. First, testing the total indirect effect of parenting on ADHD symptoms is comparable to performing a regression analysis with several predictors; thus, we can determine if an overall effect exists. Consequently if an effect is found, one can assume that the set of mediators (temperament traits) partially accounts for any effect of parenting on child ADHD symptoms. Second, using this method, it is possible to determine to what extent specific trait variables account for the association between parenting and child ADHD, conditional on the presence of the other traits in the model. That is, we can determine the magnitude of the contribution of each temperament trait to the relationship between parenting and child ADHD. Finally, including several mediators in a model allows us to examine the relative magnitude of the specific indirect effects associated with all the mediators.
Given the clustered nature of the sibling data, delta method standard errors were computed (as bootstrapped confidence intervals could not be computed with clustered data).
Importantly, however, the temporal ordering of variables in our primary model cannot be assured due to the cross-sectional nature of the data. Thus, we also conducted a series of alternative models that instead examine the impact of temperament traits on ADHD via their effects on parenting practices, consistent with prior work suggesting that child-driven effects on parenting behaviors may shape the development of ADHD and comorbid DBDs (Burke et al. 2008). Lastly, we also ran models examining DBD symptoms as outcomes (with ADHD covaried) to examine the specificity of effects.
Results
Demographic and Descriptive Statistics
Demographic and descriptive statistics are presented in Table 1. Results indicated that our diagnostic procedures were effective in discriminating the control group from the ADHD group. As expected, the ADHD group had significantly higher total symptom counts for all symptom domains measured by both parent- and teacher-report (p<0.001). Although the two groups did not differ in ethnicity composition, consistent with population distributions the ADHD group consisted of proportionally more males than the control group (p<0.001) so sex was covaried in all analyses. As expected, the ADHD group also had significantly more ODD and CD symptoms (p<0.001). Given these differences, models included child sex, age (as a precaution), medication history, and DBD symptoms as covariates. Although not different in race/ethnicity, we also included these variables as covariates in all mediation models.
Table 1.
Descriptive statistics for the control vs. ADHD group for demographics
| N | Control | ADHD | p-value |
|---|---|---|---|
| 213 | 251 | ||
| % Male | 42.3 % | 66.9 % | <0.001 |
| Age (SD) | 11.0 (2.4) | 10.5 (2.3) | 0.02 |
| % Stimulant medication | 1.4 % | 37.1 % | <0.001 |
| % Caucasian | 76.5 % | 72.1 % | 0.64 |
| Income (SD)+ | 79.0 (47.4) | 64.5 (38.7) | 0.002 |
| KSADS-E diagnostic interview | |||
| Parent inattention Sx (SD) | 0.74 (1.4) | 7.2 (1.9) | <0.001 |
| Parent hyperactivity-impulsivity Sx (SD) | 0.62 (1.2) | 4.3 (2.9) | <0.001 |
| % Oppositional defiant disorder (lifetime) | 14.1 % | 41.6 % | <0.001 |
| % Conduct disorder (lifetime) | 0.5 % | 8.4 % | <0.001 |
| Child temperament traits – parent report | |||
| Reactive control (SD) | 5.0 (1.0) | 4.2 (1.1) | <0.001 |
| Resiliency (SD) | 6.0 (0.86) | 5.2 (0.99) | <0.001 |
| Negative emotionality (SD) | 3.8 (1.2) | 4.6 (1.3) | <0.001 |
| Conscientiousness (SD) | 6.1 (1.3) | 3.9 (1.3) | <0.001 |
| Agreeableness (SD) | 6.6 (1.1) | 5.9 (1.3) | <0.001 |
| Parenting dimensions – youth report | |||
| Maternal involvement (SD) | 35.4 (5.8) | 33.4 (7.1) | 0.001 |
| Paternal involvement (SD) | 29.7 (10.3) | 26.4 (11.4) | 0.001 |
| Poor supervision/monitoring (SD) | 18.6 (5.3) | 20.6 (6.4) | <0.001 |
| Inconsistent discipline (SD) | 12.8 (3.7) | 14.1 (4.0) | <0.001 |
SD standard deviation, HI hyperactivity-impulsivity. Higher scores for temperament and parenting measures indicated that trait was more descriptive of the child and increased levels of the specific parenting behavior. + Income reported in thousands
Next, we examined differences between the control and ADHD children on parent report of child temperament characteristics and child report on parenting (see Table 1). As seen there, parents of ADHD- children were significantly more likely than the parents of the control group to classify their children as low (i.e., least descriptive) on traits of reactive control, resiliency, conscientiousness, and agreeableness (p<0.001, d’s=−0.76, −0.86, −1.69, and −0.58, respectively) and high (i.e., most descriptive) on negative emotionality (p<0.001, d=0.63). Finally, group differences were observed on child report of parenting on the APQ. Specifically, ADHD-youth reported lower levels of maternal involvement (p<0.01, d=−0.29) and paternal involvement (p<0.01, d=−0.30) and higher levels of poor supervision/monitoring (p<0.001, d= 0.34), and inconsistent discipline (p<0.001, d=0.33) compared to the control group.
Bivariate Correlations
Zero-order correlations for parent report of child temperament, child report of parenting, and the mean of parent and teacher report for ADHD symptoms can be seen in Table 2. Of note, similar to past work (Martel and Nigg 2006), bivariate correlations revealed several relations between inattention and temperament characteristics. Note that these reflect the correlations after removing overlapping items as described in Martel and Nigg (2006). In addition, Table 2 also displays the bivariate correlations for parent report of child temperament characteristics and child report of parenting behaviors. As seen there, child inattention and hyperactivity were modestly correlated with parenting variables (rs ranged −0.18 to 0.21) and moderately correlated with child temperament traits (rs ranged from −0.69 to 0.33).
Table 2.
Correlations ADHD symptoms, parenting behaviors, and child temperament traits
| Inattention | Hyperactivity | M-INV | P-INV | SUPV | INCD | |
|---|---|---|---|---|---|---|
| M-INV | −0.17*** | −0.14** | – | 0.35** | −0.18** | −0.05 |
| P–INV | −0.18*** | −0.17*** | 0.35** | – | −0.08 | −0.09* |
| SUPV | 0.21*** | 0.10* | −0.18** | −0.08 | – | 0.57** |
| INCD | 0.17*** | 0.09* | −0.05 | −0.09* | 0.57** | – |
| Reactive control | −0.33*** | −0.54*** | 0.07 | 0.07 | −0.08 | −0.05 |
| Resiliency | −0.42*** | −0.29*** | 0.03 | 0.09* | −0.08 | −0.07 |
| Neg. emotionality | 0.33*** | 0.30*** | −0.08 | −0.08 | 0.02 | 0.08 |
| Conscientiousness | −0.69*** | −0.53*** | 0.11* | 0.14** | −0.18*** | −0.17*** |
| Agreeableness | −0.33*** | −0.46*** | 0.10* | 0.13** | −0.12* | −0.16** |
M-INV maternal involvement, P-INV paternal involvement, SUPV poor supervision/monitoring, INCD inconsistent discipline.
p<0.05,
p<0.01,
p<0.001. ADHD symptoms scores reflect mean composites of parent and teacher report on the ADHD Rating Scale
Primary Tests of Direct and Indirect Effects
Inconsistent Discipline
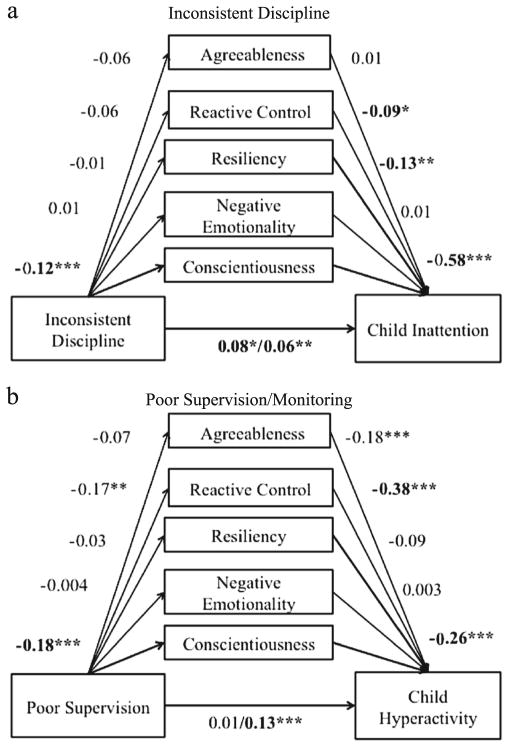
The model for parent inconsistent discipline and child inattention is depicted in Fig. 1a. The direct effect of inconsistent discipline on inattention was statistically significant (β=0.08, [0.02, 0.14], p=0.03), such that inconsistent discipline predicted more inattention. Additionally, the sum of the indirect effects was also statistically significant (β=0.06, [0.01, 0.12], p=0.009). Examination of specific indirect effects revealed that inconsistent discipline was associated with increased inattention via its association with lower conscientiousness (β=0.06, [0.03, 0.09], p=0.003). In contrast to inattention, the direct effect of inconsistent discipline on hyperactivity-impulsivity was not statistically significant (β=0.004, p=0.91) after accounting for the statistically significant indirect effects [β=0.06, [0.02, 0.09], p=0.02). Examination of the specific indirect effects again revealed an indirect pathway from inconsistent discipline to hyperactivity-impulsivity via child conscientiousness [β=0.03, [0.01, 0.04], p=0.01).
Fig. 1.
Mediational model depicting direct and indirect effects of inconsistent discipline and poor parental supervision on child ADHD symptoms. *p<0.05,** p<0.01, ***p<0.001
Poor Supervision and Monitoring
As seen in Fig. 1b, the effects of poor supervision and monitoring on hyperactivity were similar to the preceding: no direct effect remained after consideration of the statistically significant indirect effect (β= 0.13, [0.06, 0.18], p<0.001). Significant indirect pathways emerged via lower child reactive control (β=0.06, [0.03, 0.09], p=0.002) and lower conscientiousness (β=0.05, [0.03, 0.07], p<0.001) associated with more hyperactivity-impulsivity. Results when predicting inattention from supervision and monitoring also were similar to those seen for parent consistency, in that partial statistical mediation was observed. Thus, the direct effect of poor supervision on inattention was statistically reliable (β=0.11, [04, 0.18], p<0.001) but the sum of the indirect effects was also significant (β= 0.11, [0.06, 0.17], p<0.001). Indirect effects again emerged involving child lower conscientiousness (β=0.09, [0.06, 0.12], p<0.001).
Maternal Involvement
Next, we examined the direct and indirect effects of maternal involvement on ADHD symptom scores. The direct effect of maternal involvement on inattention was significant (β=−0.11, [−0.17, −0.04], p=0.007), indicating that lower levels of involvement predicted more inattention. However, the sum of the indirect effects was not significant (β=−0.03, [−0.07, 0.02], p=0.32). Similarly, as seen in Fig. 2a, the direct association of lower maternal involvement with hyperactivity was significant (β=−0.07, [−0.14, −0.01, p=0.050), whereas sum of the indirect effects was not (β=−0.04, [−0.09, 0.01], p=0.17). Thus, temperament effects were not contributory for maternal involvement.
Fig. 2.
Mediational model depicting direct effects of maternal and paternal involvement on child ADHD symptoms. * p<0.05, **p<0.01, ***p<0.001
Paternal Involvement
Paternal lower involvement was associated directly with both inattention (see Fig. 2b; β=−0.09, [−0.16, −0.02], p=0.02) and hyperactivity-impulsivity (β= −0.09, [−0.15, −0.02], p=0.03). Unlike maternal involvement, indirect effects were also observed for both inattention (β= −0.07, [−0.12, −0.02], p=0.02) and hyperactivity-impulsivity (β=−0.06, [−0.10, −0.02], p=0.02). In both cases, lower paternal involvement exerted an indirect effect on ADHD symptoms via lower child conscientiousness (inattention indirect effect=−0.06, [−0.10, −0.02], p =0.03; hyperactivity-impulsivity indirect effect =−0.03, [−0.05, −0.01], p=0.03).
Temporal Ordering of Variables and Equivalent Models
As mentioned earlier, the temporal ordering of the variables in our mediation models cannot be assured (due to the cross-sectional nature of the data), and the problem of model equivalency must be considered in interpreting the data. To this end, we conducted a secondary analysis of an alternative plausible model, which posits that child temperament traits statistically predict ADHD symptoms via their association with parenting dimensions (similar to theoretical and empirical work hypothesizing child-driven effects on parenting, see Burke et al. 2008). In these models, the four parenting dimensions were entered as simultaneous statistical mediators of the association between child temperament and ADHD symptom dimensions, and again, both direct and indirect effects were examined. Results indicated that all direct effects of child temperament traits on ADHD symptoms were significant (ranging from −0.64, to 0.31, all p<0.001), as expected based on prior work (Martel and Nigg 2006). However, the indirect effects of child temperament on ADHD symptoms via parenting dimensions were not reliable (all ps>0.06), with one exception. Indirect pathways between reactive control and ADHD symptoms via parenting were statistically significant for inattention (β=−0.04, p<0.001) and hyperactivity-impulsivity (β= −0.02, p=0.03). However, none of the specific indirect effects (via any one specific parenting dimension) were significant (all ps>0.09).
Specificity to ADHD
Given past work indicating that problematic parenting may lead to the development of disruptive behavior problems among youth with ADHD (Pfiffner et al. 2005), we also conducted secondary checks to evaluate the specificity of these effects to ADHD. Therefore, we re-ran all models with ODD and CD symptoms scores as the outcome rather than ADHD (with ADHD covaried, to ensure we did not “rediscover” the preceding findings due to the overlap of ADHD and ODD/CD). Because the method of assessment of ODD and CD varied between parents and teachers (i.e., parents completed the KSADS-E to assess ODD/CD, whereas ODD and CD ratings were provided via questionnaire by teachers), we examined ODD and CD as outcomes separately by informant. When utilizing parent-report of ODD and CD symptoms, no significant indirect pathways emerged, indicating that child temperament traits did not account for the association between parenting and disruptive behavior symptoms. However, direct effects did indeed emerge between inconsistent discipline and ODD (β=0.08, p=0.03), and between poor supervision/monitoring and CD (β=0.09, p=0.04).
However, when utilizing teacher reports of ODD and CD, results revealed some overlap with our primary analyses examining ADHD. Inconsistent discipline and poor supervision both exerted indirect effects on ODD (β=0.069, p=0.002) and CD symptoms (β=0.04, p=0.004) via child conscientiousness (and also via agreeableness for ODD). However, these indirect effects emerged in the absence of direct effects of inconsistent discipline and poor supervision/monitoring on ODD and CD. Further, while analyses revealed significant direct effects of paternal involvement on ODD (β=−0.16, p=0.001) and CD symptoms (β=−0.13, p=0.02), no significant indirect effects involving child temperament traits emerged. Further, no significant direct or indirect effects emerged when examining maternal involvement as a predictor of ODD and CD symptoms.
Discussion
The current study sought to explicitly test for the presence of indirect effects of parenting on child ADHD symptoms via child temperament characteristics. Consequently, we were able to simultaneously examine the direct effects of parenting on ADHD as well as indirect pathways involving child temperament traits as statistical mediators of these associations within the limitations of cross-sectional data. Consistent with our hypotheses, indirect effects of parenting on ADHD via child temperament did indeed emerge. Results indicated that inconsistent discipline exerted indirect effects on ADHD symptoms via its impact on child conscientiousness. Consistent with the current findings, past work has highlighted the association of inconsistent parenting with the severity and/or persistence of ADHD symptoms (Ellis and Nigg 2009; Lindahl 1998; Martel et al. 2011). The present study extends upon this past work by demonstrating that inconsistent discipline may partially influence child ADHD symptoms via child conscientiousness. Also in line with our hypotheses, poor parental supervision and monitoring predicted higher hyperactivity-impulsivity symptoms via child temperament traits of reactive control and conscientiousness, consistent with past work (Ellis and Nigg 2009; Martel and Nigg 2006). Thus, indirect pathways involving conscientiousness and reactive control in particular appear to be important for understanding the association between parenting and ADHD symptom dimensions.
Indirect effects also emerged for paternal involvement, such that these parenting behaviors impacted ADHD symptoms via effects on child conscientiousness. Interestingly, this pathway was not significant when examining maternal involvement as a predictor, potentially signaling some specificity of effects of maternal versus paternal parenting. While past work regarding specificity of paternal versus maternal parenting has been mixed (Gryczkowski 2010), prior research has demonstrated the importance of parental involvement for psychopathology more generally. For example, Hawes and colleagues (2013) found that low levels of parental involvement prospectively predicted increased levels of hyperactivity/inattention symptoms across a 12-month period. Similarly, in a 3-year longitudinal study of ADHD youth, less observed parental sensitivity predicted higher levels of inattention in middle childhood (Keown 2012). However, the current findings suggest that future exploration of parent-specific effects for ADHD may be warranted, particularly for positive parenting.
Implications
As noted earlier, questions remain regarding the role of parenting for shaping the development of ADHD versus comorbid DBDs. In line with past work by Chang and colleagues (2011), poor supervision and inconsistent discipline exerted indirect effects on ODD and CD symptoms via child conscientiousness, indicating some overlap in regard to indirect effects involving child conscientiousness in particular. That is, it may be the case that parenting practices that serve to exacerbate underlying problems in conscientiousness and effortful control may increase risk for development of comorbid DBDs among youth with ADHD. Additionally, however, indirect effects also emerged involving agreeableness in models of parenting as a predictor of ODD. This finding is in line with past work suggesting that negative affect and agreeableness help explain the overlap between ADHD and ODD (Martel and Nigg 2006; White 1999). Further, low levels of reactive control and agreeableness have been linked to increased hyperactivity-impulsivity specifically (Martel and Nigg 2006); hyperactivity-impulsivity in particular has been proposed to largely account for the overlap between ADHD and DBDs (Burns et al. 2014). Importantly, these traits have been hypothesized to reflect disruptions of bottom-up incentive processes (e.g., delaying rewards; Nigg 2006a), and difficulties regulating emotion and self-control, as well as low levels of agreeableness and high levels of negative affect, have been implicated as robust predictors of child DBDs (Martel et al. 2012). Thus, future work may benefit by examining the role of parenting in the emergence of such traits, as these may be crucial for understanding the development of externalizing comorbidity more generally.
In line with this, the results of the current study may be helpful for elucidating causal pathways of ADHD and comorbid DBDs, and more specifically, provide additional support for multiple pathway models of ADHD that have been developed in recent years (Sonuga-Barke 2006; Sonuga-Barke et al. 2010). Such models posit that top-down processes of cognitive control may be uniquely related to inattention and associated executive functioning deficits, whereas bottom-up processes are likely related with motivational or emotion-based deficits and are more closely associated with the hyperactive-impulsive symptom dimension (and potentially with externalizing psychopathology more generally, Sonuga-Barke 2006). In particular, child conscientiousness may be important for understanding the impact of parenting on inattention difficulties specifically, whereas reactive control may be particularly useful for understanding the impact of parenting on hyperactivity-impulsivity. These findings are in line with prior work demonstrating some specificity of trait associations with ADHD symptoms, including (1) associations between effortful control and inattention symptoms of ADHD and (2) associations between reactive control and hyperactivity-impulsivity (Martel and Nigg 2006). Consistent with these multiple-pathway theories, our findings support that inattention and hyperactivity-impulsivity symptoms of ADHD, while related, may have partially distinguishable etiologies (Sonuga-Barke 2006).
Finally, as proposed in the model by Deater-Deckard (2014), the present findings may have implications for elucidating the influential role that parenting plays on the development of children’s self-regulation skills and subsequent ADHD symptoms. Particularly with respect to conscientiousness (or effortful control) and reactive control, past work has indicated that maternal behavior (e.g., overcontrol/intrusiveness) at age 2 predicted decreased growth of children’s reactive control abilities at age 5 compared to children of nonintrusive mothers. Additionally, low levels of maternal warmth at age 2 predicted lower levels of children’s effortful control at age 5 (Graziano et al. 2010). Given that the present findings highlight the importance of conscientiousness and reactive control as mediators of the association between parenting and child ADHD, further work may benefit by investigating neural processes that underpin these traits in order to better connect how parenting practices may influence adaptive and maladaptive behaviors and how those associations may be modulated across development. Additionally, parenting interventions for families of children with ADHD may benefit from targeting specific parenting behaviors of parental monitoring and inconsistent discipline as these were shown to have the strongest indirect effects on ADHD symptoms (as well as ODD and CD) via child traits of conscientiousness and reactive control in the current study.
Limitations
There are some limitations to note of the current research. First, the current study used questionnaires to assess parenting behaviors (child-report) and child ADHD symptoms (parent-and teacher-report), whereas coded laboratory observations may have been informative as well (Wilson and Durbin 2012). However, we attempted to reduce potential informant bias and effects by utilizing reports from different individuals (parent reports of temperament, child reports of parenting, combination of parent- and teacher-ratings of ADHD symptoms), even though child reports on the APQ may be less reliable among younger children. Secondly, the temporal ordering of the variables in our mediational models reflects one proposed mechanism of several and cannot be assured due to the cross-sectional nature of the data. However, the present study is the minimum hurdle for the model; if associations are not present cross-sectionally, it would be difficult to discover them longitudinally. Additionally, checks of a competing model positing that child temperament traits may influence ADHD via parenting dimensions (reflecting a child-driven conceptualization of parenting) revealed only one set of significant indirect effects, providing some additional support for our hypothesized mechanism. Lastly, the current study investigated the complex relationships between parenting, temperament, and ADHD across a broad age range of children. Notably, these relationships are dynamic across development, and the impact of similar parenting dimensions may result in adaptive or maladaptive behaviors depending on the child’s stage of development. Future work would benefit from longitudinal examinations of these associations, both to clarify the temporal ordering of effects as well as to understand how development may further influence how these associations unfold over time.
Conclusion
The study was strengthened by the use of a multiple mediation framework to examine both direct and indirect effects of parenting on child ADHD via their impact on child temperament. Findings indicated that child temperament traits of reactive control and conscientiousness mediated the association between parenting and ADHD. Our findings extend recent work by elucidating potential differentiation in pathways from parenting to ADHD symptom dimensions of inattention versus hyperactivity-impulsivity, as well as provide support for the Deater-Deckard (2014) model which emphasizes the role of parental contributions in the development of children’s self-regulation abilities.
Acknowledgments
This work was supported by R01-MH070004-01A2 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health. The authors also thank all participating children and their families for making this work possible.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
Contributor Information
Josie M. Ullsperger, Email: josie-ullsperger@uiowa.edu, Department of Psychology, University of Iowa, Iowa City, IA 52242, USA
Joel T. Nigg, Department of Psychiatry, Oregon Health and Science University, Portland, OR, USA
Molly A. Nikolas, Department of Psychology, University of Iowa, Iowa City, IA 52242, USA
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington: Author; 2013. [Google Scholar]
- Barkley R. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. 2. New York: Guilford; 1998. [Google Scholar]
- Berlin L, Bohlin G, Rydell A. Child neuropsychology: a journal on normal and abnormal development in childhood and adolescence. Child Neuropsychology. 2004;9:255–266. doi: 10.1076/chin.9.4.255.23519. [DOI] [PubMed] [Google Scholar]
- Bernier A, Carlson S, Deschenes M, Matte-Gagne C. Social factors in the development of early executive functioning: a closer look in the caregiving environment. Developmental Science. 2012;15:12–24. doi: 10.1111/j.1467-7687.2011.01093.x. [DOI] [PubMed] [Google Scholar]
- Best J, Miller P. A developmental perspective on executive function. Child Development. 2010;81:1641–1660. doi: 10.1111/j.1467-8624.2010.01499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke J, Pardini D, Loeber R. Reciprocal relationships between parenting behavior and disruptive psychopathology from childhood through adolescence. Journal of Abnormal Child Psychology. 2008;36:679–692. doi: 10.1007/s10802-008-9219-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns GL, Moura MA, Beauchaine T, McBurnett K. Bifactor latent structure of ADHD/ODD symptoms: predictions of dual pathway/trait impulsivity etiological models of ADHD. Journal of Child Psychology and Psychiatry. 2014;55:393–401. doi: 10.1111/jcpp.12165. [DOI] [PubMed] [Google Scholar]
- Bridgett D, Oddi K, Laake L, Murdock K, Bachmann M. Integrating and differentiating aspects of self-regulation: effortful control, executive functioning, and links to negative affectivity. Emotion. 2013;13:47–63. doi: 10.1037/a0029536. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Halperin JM, Sonuga-Barke EJS. A developmental perspective on attention-deficit/hyperactivity disorder (ADHD) In: Lewis M, Rudolph KD, editors. Handbook of Developmental Psychopathology. New York: Springer Publishing; 2014. pp. 427–448. [Google Scholar]
- Caspi A, Block J, Block JH, Klopp B, Lynam D, Moffitt T, Stouthamer-Loeber M. A “common-language” version of the California child q-set for personality assessment. Psychological Assessment. 1992;4:512–523. [Google Scholar]
- Chang H, Olson S, Sameroff A, Sexton H. Child effortful control as a mediator of parenting practices on externalizing behavior: evidence for a sex-differentiated pathway across the transition from preschool to school. Journal of Abnormal Child Psychology. 2011;39:71–81. doi: 10.1007/s10802-010-9437-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conners CK. Conners rating scale-revised. Toronto: Multi-Health Systems; 1997. [Google Scholar]
- Davidov M, Grusec JE. Untangling the links of parental responsiveness to distress and warmth to child outcomes. Child Development. 2006;77:44–58. doi: 10.1111/j.1467-8624.2006.00855.x. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K. Family matters: Intergeneration and interpersonal processes of executive function and attentive behavior. Current Directions in Psychological Science. 2014;23:230. doi: 10.1177/0963721414531597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deault L. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder. Child Psychiatry and Human Development. 2010;41:168–192. doi: 10.1007/s10578-009-0159-4. [DOI] [PubMed] [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. The ADHD rating scale –IV: Checklists, norms, and clinical interpretation. New York: Guilford Press; 1998. [Google Scholar]
- Eisenberg N, Fabes R, Guthrie I, Murphy B, Maszk P, Holmgren R, Suh K. The relations of regulation and emotionality to problem behavior in elementary school children. Development and Psychopathology. 1996;8:141–162. [Google Scholar]
- Eisenberg N, Sadovsky A, Spinrad T, Fabes R, Losoya A, Valiente C, Reiser &, Shepard S. The relations of problem behavior status to children’s negative emotionality, effortful control, and impulsivity: concurrent relations and prediction of change. Developmental Psychopathology. 2005;41:193–211. doi: 10.1037/0012-1649.41.1.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis B, Nigg J. Parenting practices and attention-deficit/hyperactivity disorder: New findings suggest partial specificity of effects. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48:146–154. doi: 10.1097/CHI.0b013e31819176d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essau C, Sasagawa A, Frick P. Psychometric properties of the Alabama Parenting Questionnaire. Journal of Child and Family Studies. 2006;15:597–616. doi: 10.1007/s10826-006-9036-y. [DOI] [Google Scholar]
- Finzi-Dottan R, Manor I, Tyano S. ADHD, temperament, and parental style as predictors of the child’s attachment patterns. Child Psychiatry and Human Development. 2006;37:103–114. doi: 10.1007/s10578-006-0024-7. [DOI] [PubMed] [Google Scholar]
- Graziano P, Keane S, Calkins S. Maternal behavior and children’s early emotion regulation skills differentially predict development of children’s reactive and later effortful control. Infant and Child Development. 2010;19:333–353. doi: 10.1002/icd.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gryczkowski M. Differential relations between mothers’ and fathers’ parenting practices and child externalizing behavior. Journal of Child and Family Studies. 2010;19:539–546. [Google Scholar]
- Hawes D, Dadds M, Frost A, Russell A. Parenting practices and prospective levels of hyperactivity/inattention across early and middle childhood. Journal of Child Psychopathology and Behavioral Assessment. 2013;35:273–382. [Google Scholar]
- Johnston C. Parent characteristics and parent–child interactions in families of nonproblem children and ADHD children with higher and lower levels of oppositional-defiant behavior. Journal of Abnormal Child Psychology. 1996;24:85–104. doi: 10.1007/BF01448375. [DOI] [PubMed] [Google Scholar]
- Johnston C, Jassy J. Attention-deficit/hyperactivity disorder and oppositional/conduct problems: links to parent–child interactions. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2007;16:74–79. [PMC free article] [PubMed] [Google Scholar]
- Johnston C, Mash E. Families of children with attention-deficit/hyperactivity disorder: review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4:183–207. doi: 10.1023/a:1017592030434. [DOI] [PubMed] [Google Scholar]
- Kaiser N, McBurnett K, Pfiffner L. Child ADHD severity and positive and negative parenting as predictors of child social functioning: evaluation of three theoretical models. Journal of Attention Disorders. 2010;15:193–203. doi: 10.1177/1087054709356171. [DOI] [PubMed] [Google Scholar]
- Keown L. Predictors of boys’ ADHD symptoms from early to middle childhood: the role of father-child and mother-child interactions. Journal of Abnormal Child Psychology. 2012;40:569–581. doi: 10.1007/s10802-011-9586-3. [DOI] [PubMed] [Google Scholar]
- Kiff CJ, Lengua L, Zalewski M. Nature and nurturing: parenting in the context of child temperament. Clinical Child and Family Psychology Review. 2011;14:251–301. doi: 10.1007/s10567-011-0093-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Deater-Deckard K. Dynamic changes in anger, externalizing, and internalizing problems: attention and regulation. Journal of Child Psychology and Psychiatry. 2011;52:156–166. doi: 10.1111/j.1469-7610.2010.02301.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey B. Commentary: role of temperament in developmental models of psychopathology. Journal of Clinical Child and Adolescent Psychology. 2004;33:88–93. doi: 10.1207/S15374424JCCP3301_9. [DOI] [PubMed] [Google Scholar]
- Lindahl K. Family process variables and children’s disruptive behavior problems. Journal of Family Psychology. 1998;12:420–436. [Google Scholar]
- Marmorstein NR, Iacono WG. Major depression and conduct disorder in youth: associations with parental psychopathology and parent–child conflict. Journal of Child Psychology and Psychiatry. 2004;45:377–386. doi: 10.1111/j.1469-7610.2004.00228.x. [DOI] [PubMed] [Google Scholar]
- Martel M, Nigg J. Child ADHD and personality/temperament traits of reactive and effortful control, resiliency, and negative emotionality. Journal of Child Psychology and Psychiatry. 2006;47:1175–1183. doi: 10.1111/j.1469-7610.2006.01629.x. [DOI] [PubMed] [Google Scholar]
- Martel MM, Nigg JT, Wong MM, Fitzgerald HE, Jester JM, Puttler LI, Zucker RA. Childhood and adolescent resiliency, regulation, and executive functioning in relation to adolescent problems and competence in a high-risk sample. Development and Psychopathology. 2007;19:541–563. doi: 10.1017/S0954579407070265. [DOI] [PubMed] [Google Scholar]
- Martel M, Nikolas M, Jernigan K, Friderici K, Nigg J. Diversity in pathways to common childhood disruptive behavior disorders. Journal of Abnormal Child Psychology. 2012;40:1223–1236. doi: 10.1007/s10802-012-9646-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel M, Nikolas M, Jernigan K, Friderici K, Waldman I, Nigg J. The dopamine receptor D4 gene (DRD4) moderates family environmental effects on ADHD. Journal of Abnormal Child Psychology. 2011;39:1–10. doi: 10.1007/s10802-010-9439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Shimmack U, Nikolas MA, Nigg JT. Integration of symptom ratings from multiple informants in ADHD diagnosis: A psychometric model with clinical utility. Psychological Assessment. 2015 doi: 10.1037/pas0000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mash E, Johnston C. A comparison of the mother-child interactions of younger and older hyperactive and normal children. Child Development. 1982;53:1371–1381. [PubMed] [Google Scholar]
- Modesto-Lowe V, Danforth J, Brooks D. ADHD: Does parenting style matter? Clinical Pediatrics. 2008;47:865–872. doi: 10.1177/0009922808319963. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user’s guide. 7. Los Angeles: Muthen & Muthen; 1998–2013. [Google Scholar]
- Nigg JT. On inhibition/disinhibition in developmental psychopathology: views from cognitive and personality psychopathology and a working inhibition taxonomy. Psychological Bulletin. 2000;126:220–246. doi: 10.1037/0033-2909.126.2.220. [DOI] [PubMed] [Google Scholar]
- Nigg J. What causes ADHD? Understanding what goes wrong and why. New York: Guilford Press; 2006a. [Google Scholar]
- Nigg JT. Temperament and developmental psychopathology. Journal of Child Psychology and Psychiatry. 2006b;47:395–422. doi: 10.1111/j.1469-7610.2006.01612.x. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Goldsmith H, Sachek J. Temperament and attention deficit hyperactivity disorder: the development of a multiple pathway model. Journal of Clinical Child and Adolescent Psychopathology. 2004;33:42–53. doi: 10.1207/S15374424JCCP3301_5. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Hinshaw SP, Huang-Pollack C. Disorders of attention and impulse regulation. In: Cicchetti D, Cohen D, editors. Developmental psychopathology. 2. New York: Wiley; 2006. pp. 358–403. [Google Scholar]
- Nikolas M, Burt SA. Genetic and environmental influences on ADHD symptom dimensions of inattention and hyperactivity: a meta-analysis. Journal of Abnormal Psychology. 2010;119:1–17. doi: 10.1037/a0018010. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Debaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. American Psychologist. 1989;44:329–335. doi: 10.1037/0003-066X.44.2.329. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pfiffner L, McBurnett K, Rathouz P, Judice S. Family correlates of oppositional and conduct disorders in children with attention deficit/hyperactivity disorder. Journal of Abnormal Child Psychology. 2005;33:551–563. doi: 10.1007/s10802-005-6737-4. [DOI] [PubMed] [Google Scholar]
- Preacher K, Hayes A. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Puig-Antich J, Ryan N. Kiddie schedule for affective disorders and schizophrenia. Pittsburgh: Western Psychiatric Institute; 1986. [Google Scholar]
- Rothbart MK. Becoming who we are: Temperament and personality in development. New York: The Guilford Press; 2012. [Google Scholar]
- Rothbart MK, Bates JE. Temperament. In: Eisenberg N, Damon W, Lerner RM, editors. Handbook of child psychology: Vol. 3, Social, Emotional, and Personality Development. 6. Hoboken: Wiley; 2006. pp. 99–166. [Google Scholar]
- Sanson A, Prior M. Temperament and behavioral precursors to oppositional defiant disorder and conduct disorder. In: Quay H, Hogan A, editors. Handbook of disruptive behavior disorders. New York: Kluwer Academic/Plenum Publishers; 1999. pp. 397–417. [Google Scholar]
- Shelton KK, Frick PJ, Wooton JM. The assessment of parenting practices in families of elementary school-aged children. Journal of Clinical Child Psychology. 1996;25:317–329. [Google Scholar]
- Sonuga-Barke E. Causal models of attention-deficit hyperactivity disorder: from common simple deficits to developmental pathways. Biological Psychiatry. 2006;57:1231–1238. doi: 10.1016/j.biopsych.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke E, Bitsakou P, Thompson M. Beyond the dual pathway model: Evidence for the dissociation of timing, inhibitory, and delay-related impairments in attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:345–355. doi: 10.1016/j.jaac.2009.12.018. [DOI] [PubMed] [Google Scholar]
- White J. Personality, temperament, and ADHD: a review of the literature. Personality and Individual Differences. 1999;27:589–598. [Google Scholar]
- Wilson S, Durbin E. The laboratory parenting assessment battery: development and preliminary validation of an observational parenting measure. Psychological Assessment. 2012;24:823–832. doi: 10.1037/a0028352. [DOI] [PubMed] [Google Scholar]