Abstract
While widespread lip service is given in the UK to the social determinants of health (SDoH), there are few published comparisons of how the UK's devolved jurisdictions ‘stack up’, in terms of implementing SDoH-based policies and programmes, to improve health equity over the life-course. Based on recent SDoH publications, seven key societal-level investments are suggested, across the life-course, for increasing health equity by socioeconomic position (SEP). We present hard-to-find comparable analyses of routinely collected data to gauge the relative extent to which these investments have been pursued and achieved expected goals in Scotland, as compared with England and Wales, in recent decades. Despite Scotland's longstanding explicit goal of reducing health inequalities, it has recently been doing slightly better than England and Wales on only one broad indicator of health-equity-related investments: childhood poverty. However, on the following indicators of other ‘best investments for health equity’, Scotland has not achieved demonstrably more equitable outcomes by SEP than the rest of the UK: infant mortality and teenage pregnancy rates; early childhood education implementation; standardised educational attainment after primary/secondary school; health care system access and performance; protection of the population from potentially hazardous patterns of food, drink and gambling use; unemployment. Although Scotland did not choose independence on September 18th, 2014, it could still (under the planned increased devolution of powers from Westminster) choose to increase investments in the underperforming categories of interventions for health equity listed above. However, such discussion is largely absent from the current post-referendum debate. Without further significant investments in such policies and programmes, Scotland is unlikely to achieve the ‘healthier, fairer society’ referred to in the current Scottish Government's official aspirations for the nation.
Keywords: Policies to reduce health inequalities, Scotland, England and Wales, United Kingdom, Lifecourse epidemiology, Public health
Highlights
-
•
We put forward seven societal-level investments for increasing health equity.
-
•
We compare evidence for their effectiveness in Scotland versus the rest of the UK.
-
•
There have been improvements in reducing childhood poverty in Scotland.
-
•
No evidence for improvements versus the rest of the UK for other investments.
-
•
We recommend policy debates should focus on pros/cons and costs of such investments.
Recent national and international reports have all recommended broad categories of policies, and types of public programmes, to help reduce socioeconomic inequalities in health (British Academy, 2014; Macintyre, 2007; Marmot, 2010; Marmot et al., 2008; European Commission, 2013). In many cases, these policies and programmes rightly attempt to directly influence the societal distribution of an underlying determinant of health, such as: income (especially after government taxes and transfers); educational and health services; social welfare benefits; and other goods and services important to health and well-being. What is found less often in the current published literature is any sort of ‘report card’ on a country's success in implementing these recommendations, and achieving specific objectives that one would expect from doing so. Part of the reason for this dearth of evidence within the UK relates to the increasingly disparate statistical indicators utilised across devolved jurisdictions to assess health, educational, and economic outcomes at the population level. This paper aims to fill that gap, focussing on comparable data on investments for health equity in Scotland, as compared with England (or, where data did not permit separation, England and Wales).
Prior to writing this paper, we distilled from key SDoH reports (Marmot, 2010; Marmot et al., 2008; Marmot and Wilkinson, 2003) what we regard as the seven key societal policies and programmes to help reduce health inequalities by socioeconomic position (Table 1). Our proposed ‘societal investments’ inevitably contain categories of public investment which others may not rank as highly in the hierarchy of interventions – at the whole-society level – that are critical to reducing socioeconomic and health inequality. However, we believe this is a strong first iteration, to which we hope others will make constructive revisions.
Table 1.
Seven key societal investments for improving health equity over the lifecourse.
| Stage of lifecourse | Societal investment |
|---|---|
| Very early life |
|
| |
| |
| Later childhood and adolescence |
|
| All of life |
|
| |
|
This article summarises the evidence, from both published studies and routinely collected data in the UK on socioeconomic and health outcomes, that illuminates how well Scotland in particular is doing, in comparison to the rest of the UK (given Scotland's well-known greater health and health inequality burden) (Hanlon et al., 2005). In most cases we have not attempted to assess Scottish and UK levels of financial investment, per se. This is because detailed analysis of expenditure on particular policies and programmes, especially in the public sector, is both difficult and inherently non-comparable across jurisdictions. Instead, we have tried to gauge the extent to which any results of those investments are currently evident, in terms of recent changes in specific population-level outcomes. Our focus is those outcomes related to socioeconomic inequalities, which one would expect to improve as a result of such interventions, if they were properly invested in and implemented, over time. In some cases we have not been able to access disaggregated UK data for these outcomes across the other devolved jurisdictions, for direct comparison to equivalent Scottish outcomes. In these cases we have resorted to all-UK-level data, which of course understates any differences between the rest of the UK and Scotland.
1. Investment #1: universally accessible (free at point-of-care), strongly promoted, high-quality sexual and reproductive education/counselling in youth; family planning; prenatal and perinatal care
The extent of provision, throughout the UK, of universally accessible (free at point-of-care), prenatal and perinatal services is more favourable than many developed countries (Roberts, 2012). Current UK-wide services through the National Health Service (NHS) ensure that virtually all mothers and children have very good chances of receiving, at no direct cost, high-quality prenatal/perinatal care by international standards, according to their needs and preferences, regardless of their gender, place of residence, ethnicity or socioeconomic position (SEP) (Krieger et al., 1997), thus enhancing equitable health outcomes (Marmot et al., 2008; Schoen et al., 2010). For example, there is little variation in the levels of expected mortality among very preterm babies of different socioeconomic backgrounds, receiving similar neonatal care (Smith et al., 2009). Nevertheless, infants born into social disadvantage in the UK continue to experience adverse birth and infant outcomes, including low birth weight, premature birth, stillbirth, and infant mortality (Weightman et al., 2012). Investments in early years, such as universal access to evidence-based prenatal/perinatal care, have the potential to reduce health inequalities in later life (Roberts, 2012). In the UK, one such investment that attempts to promote the well-being of infants and equalises their life chances is the universal Child Health Programme. The core of this programme is universally offered child health reviews, generally delivered through home visits by Health Visitors (HVs), but complemented by general practitioner (GP) and special nurse-led clinics, depending on local service models. The reviews comprise an integrated package of immunization, screening, surveillance, health promotion and parenting support delivered primarily by HVs to all infants and their families. However, despite the wide availability of such universal services, there still exist – as detailed below – marked socioeconomic differences in infant mortality in both England and Scotland.
1.1. Infant mortality
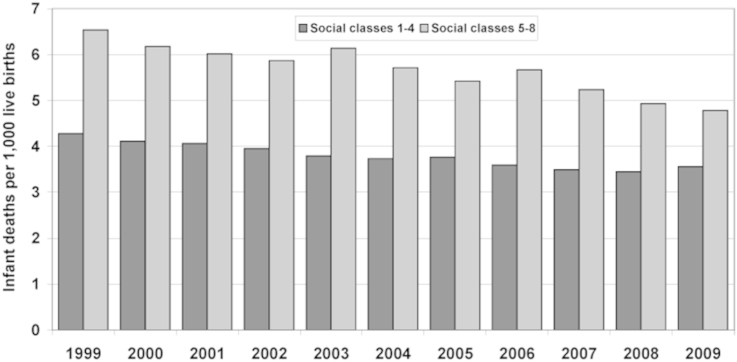
Current official publications of SEP gradients in early-life outcomes, using methods comparable across UK jurisdictions, are largely limited to time-trends in infant mortality rate (IMR). The longest comparable pair of time-series we could identify from Scotland, versus England and Wales, comes from the period 2001–2009 inclusive (Poverty, 2011; ONS, 2012). In England and Wales, IMR decreased in a linear fashion over this nine-year period, from approximately 6.5 to about 4.8/1000 live births (LBs) in the lower SEP groups, whereas the reduction in the higher SEP group was from a much lower 2001 rate of 4.2, to about 3.6/1000 live births by 2009 (Fig. 1). Thus, in England and Wales, the absolute IMR decline between these two calendar years' IMRs, in 2001 and 2009, was much greater in the lower-SEP grouping (1.7/1000 LBs) than in the higher-SEP grouping (0.6/1000 LBs). Despite a narrowing of the absolute gap between higher- and lower-SES IMR risks over this period, it must be noted that the gap was narrowing very slowly, with nine years of progress still leaving the lower-SEP infants with a substantially higher relative risk of death in 2009 compared to the higher-SEP infants that year, and – in the case of England and Wales – worse off than the higher-SEP infants were a decade earlier. Data from 2010 to 2011 are now available (after which ONS changed from using father's social class to highest household social class), showing similar patterns as seen in Fig. 3 (Supplementary Figs. 1 and 2).
Fig. 1.
England and Wales infant mortality rates by SEP (father's social class) (1999–2009). Source: Poverty UK, 2012 (Poverty, 2011).
Fig. 3.
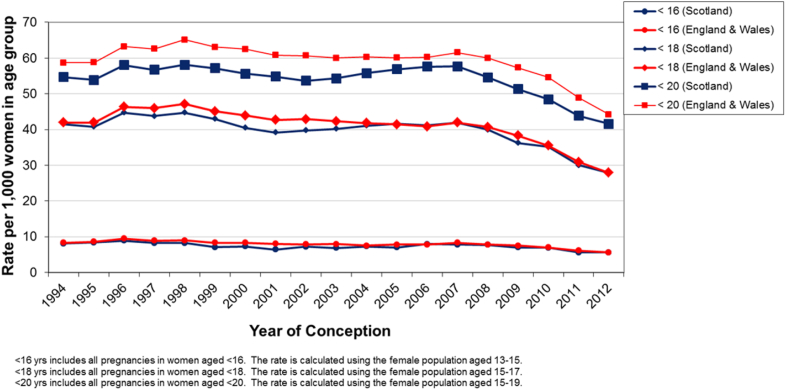
Comparison of teenage pregnancies in Scotland and England and Wales by age group at conception (1994–2012). Source: ISD Scotland, 2014 (Information Service Division Scotland, 2014).
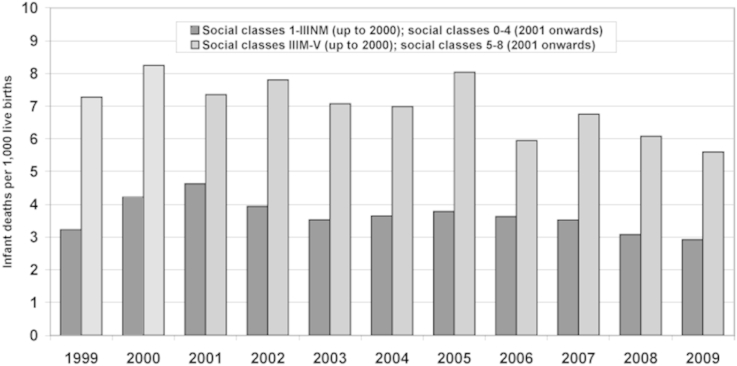
Comparable statistics from Scotland show more statistical instability over time (Fig. 2), due to the much smaller number of infant deaths in a population less than one tenth of the size of the UK as a whole (Poverty, 2011). Nonetheless, both jurisdictions show a remarkably similar overall pattern – a more rapid absolute decline in IMR, in the years leading up to 2009, for lower-SEP infants than for higher-SEP infants. However, that pattern of decline left the most recent IMRs much more discrepant – in terms of absolute health inequality gap – across the two social class groupings in Scotland than in England: 5.6 versus 2.9/1000 LBs (almost double) in 2009 within Scotland. Thus, while the overall IMR for all of England and Wales was either comparable to or slightly higher than the overall Scottish IMR for most years since 1995, the IMR gap between the two SEP groupings depicted in Figs. 1 and 2 was consistently larger in Scotland, throughout the nine years (3.5/1000 LBs in 2000–2001 to about 2.8/1000 LBs in 2008–9 – whereas the gap in England and Wales fell from 2.0 to 1.1/1000 LBs over the same period). Data for 2010–2012 now use the Scottish Index of Multiple Deprivation, SIMD, although similar time-trends continue (Supplementary Fig. 3). As with virtually every other routinely collected health outcome analysed annually in recent years by the Scottish Government (Frank and Haw, 2011, 2013), Scottish socioeconomic inequalities in health remain large, generally the largest in Western Europe (Popham and Boyle, 2010).
Fig. 2.
Scotland infant mortality rates by SEP (1999–2009). Source: Poverty UK, 2012 (Poverty, 2011).
Recent publications concerning the key determinants of differences in infant mortality (IMR) by SEP in the UK strongly suggest that two of these require novel and persistent programmes if SEP-related disparities in IMR are to decline: a) more aggressive smoking cessation support and incentives in pregnancy; (Tappin et al., 2015) b) more intensive support for breast feeding, especially right after birth (Hoddinott et al., 2012). As well, teenage pregnancy rates, although declining in the last half-decade in both Scotland (28.5% reduction between 2006 and 2011) (Information Service Division Scotland, 2014) and England, are still among the highest in Western Europe (Unicef, 2007). Although we were unable to find precisely comparable data on recent time-trends for teenage pregnancy rates by SEP, across Scotland and England/Wales, we would argue that teenage pregnancies are socially patterned. For example, in Scotland, teenage pregnancy rates among the most deprived declined from 102.0 to 80.6/1000 women aged 15–19 years in 2000–2011 (Supplementary Fig. 4). However, among the least deprived group, the decrease was from 21.0 to 18.4/1000 women aged 15–19 years (Information Service Division Scotland, 2014). There is ample evidence that higher, but recently declining teen pregnancy rates in Scotland contribute to its worse IMR and other child outcomes, and that these should be amenable to creative preventive programmes (Fig. 3) (Information Service Division Scotland, 2014; Unicef, 2007; Bonell, 2004; Harden et al., 2009; Scottish Parliament, 2013; Teenage Pregnancy Independent Advisory Group, 2010).
2. Investment #2: labour market, tax and transfer policies to lift all families with young children out of poverty
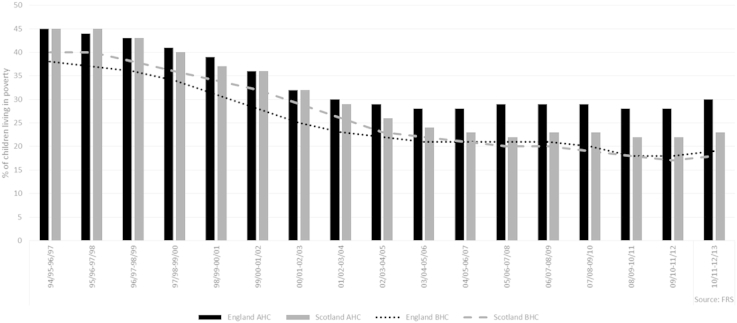
A UK household is in poverty if its income, after taxes, is below 60% of median household income (adjusted for household size/composition). This 60% threshold is routinely measured both before (‘BHC’) and after (‘AHC’) housing costs are deducted from income. The 60% median income threshold is also measured in relative terms (to measure any increase in the incomes of the poorest families against general rises in incomes in the population as a whole) and in absolute terms (to measure against a fixed point any increase in the incomes of the poorest families in real terms). From the late 1990s until 2010/11, child poverty in Scotland had decreased by approximately fifteen percentage points, to rates lower than those in England on both measures. The changing pattern in the AHC rate was largely due to “the high and rising cost of housing in England, and particularly the south of England” (Aldridge et al., 2013). Housing costs in England and Wales had risen from 10% higher a decade earlier to 25% higher. This had particularly affected those in the bottom half of the income distribution, indicating that “Scotland's lower housing costs help to keep poverty down” (Aldridge et al., 2013).
During the New Labour years (1997–2010) relative child poverty decreased from 26.7% to 19.7%. The reason this decrease was not more pronounced is attributed to the “strong growth in average real incomes over this period” (Dickens, 2011), i.e. the incomes of the poor must rise faster than those in the middle/top inorder for child poverty to reduce. However, income inequality is so deeply established in the UK that the proportion of children living in relative poverty remained high due to the rapidly increasing incomes of those at the higher end of the income spectrum. Meanwhile, absolute child poverty fell from 28.9% to 10.8% over the same period, reflecting “a substantial increase in the real incomes of the poor over this period” (Dickens, 2011). During this period, child poverty fell faster in Scotland than in the rest of the UK, for reasons already stated, in addition to specific early anti-poverty initiatives, such as the New Futures Fund for ex-offenders and substance users, which aimed to help “particularly disadvantaged youngsters overcome real barriers to finding work, and improve their employability through a wide range of initiatives”; (Dewar, 1998) and the Working for Families Fund which provided assistance for lone parents with complex needs who were far from employment-ready (Burchardt et al., 2009). These initiatives were complementary to, rather than divergent from, UK policies, and were a successful adjunct to the anti-poverty policy agenda (Burchardt et al., 2009).
While New Labour did not achieve its ambitious aim to reduce child poverty by 50% by 2010 the trend was heading in the right direction. Since 2010/11, however, due to the UK Coalition government's austerity measures, child poverty has been decreasing in relative terms due to a general fall in income but has been increasing in absolute terms across the entire UK (Fig. 4 – absolute; Supplementary Fig. 5 – relative). This increase in absolute terms is “unprecedented since records began in the 1960s” and marks a worrying reversal in the hitherto improving child poverty trend (Taylor-Robinson et al., 2014). Although Scotland is devolved, policies associated with income, such as minimum wage, tax credits and social security benefits, are reserved to the UK government at Westminster. Despite the Scottish Government's limited room for manoeuvre with regards policy divergence in relation to child poverty, there is a critique that it has had greater room for manoeuvre than it has utilised (Sinclair et al., 2011; Wincott, 2006).
Fig. 4.
Percentage of children living in households with less than 60 per cent of 2010/11 median household income held constant in real terms, by region and country, United Kingdom (1994/95–2012/13) Percentage of children living in Scottish and English households living in poverty before (BHC) and after (AHC) adjustment for housing costs (1994–2012). Source: Aldridge et al., 2013 (Teenage Pregnancy Independent Advisory Group, 2010).
Tackling poverty in Scotland specifically requires the efforts of both the Scottish Government and the 32 local authorities. The Scottish Government had existing powers over many of the areas that are central to tackling poverty (Aldridge et al., 2013). The scope of these powers are also expected to further increase in line with the Smith Commission following the 2014 independence referendum. The 32 Scottish local authorities also have responsibilities within areas such as housing, planning, urban design, transport, early years, leisure services, educational attainment, training and employment – all of which are vital to mitigate health inequalities and promote social and economic well-being (British Academy, 2014).
3. Investment #3: universally accessible (virtually free), high-quality early childhood education and care programmes, located in every neighbourhood within walking distance of parents' homes
The importance of early childhood is well documented, and intervention studies around the world have highlighted the positive impact of early childhood education and care (ECEC) on school readiness and performance (Nores and Barnett, 2010). Long-term follow-up studies from the US have provided robust evidence for the economic benefits of ECEC, particularly for children from disadvantaged backgrounds, with returns on investment ranging from US$4 to over US$10 for every dollar spent (Temple and Reynolds, 2007). The reduced cost to society comes through increased school readiness, higher educational attainment and employment, and decreased delinquent and criminal behaviour. Additional effects include improved social and emotional outcomes, higher self-esteem and social cohesion (Nores and Barnett, 2010; Temple and Reynolds, 2007), which have the potential to influence long-term mental and physical health.
While UK-wide law governs parental leave and tax funding for ECEC, Scotland has devolved control over most other aspects of early childhood programming. Publicly-funded part-time preschool is available to all children in Scotland and England from age three, and around 96% of eligible children are enrolled (Neumann et al., 2013). In 2014, Scotland increased preschool entitlement from 475 to 600 h annually, and part of the critical gap from age one, when parental leave entitlement ends, until age 3, when preschool entitlement begins, was addressed by extending entitlement to 2-year-olds from the most deprived backgrounds. Similar measures began in England in 2013 (Children in Scotland, 2011).
In 2007–2008 a two-year intervention to extend preschool duration was piloted in Scotland. While developmental outcomes for children involved in the intervention improved, they were not significantly different from the control group (Woolfson and King, 2008). Numerous factors may have influenced this result, including intervention variability and duration. There is also a challenge in ensuring that all early childhood educators have adequate training and terms of employment and attractive career trajectories (Neumann et al., 2013; Children in Scotland, 2011). In the UK, many staff at pre-school centres have only completed secondary school and are offered correspondingly low salaries (Scottish Government, 2006).
Given the international evidence in support of well-designed longer-term ECEC (including that from England), Scotland should not be deterred from pursuing programs and policies that aim to expand ECEC opportunities for all children. Analysis of the Program for International Student Assessment (PISA) 2009 data have shown that increasing ECEC duration to more than one year would have resulted in a 20-point increase in the UK's PISA literacy test scores and a world ranking 12 places higher (Mostafa and Green, 2012). Modelling the impact of universal ECEC on children's PISA literacy scores has also shown a major reduction in score variation across deciles of parental SEP, earning ECEC the label “win–win policy”, because it “boosts average performance and reduces inequalities” (Mostafa and Green, 2012). Economists call this a “Pareto improvement” (Culyer, 2005) – and there are not many of them in the modern policy-maker's kitbag.
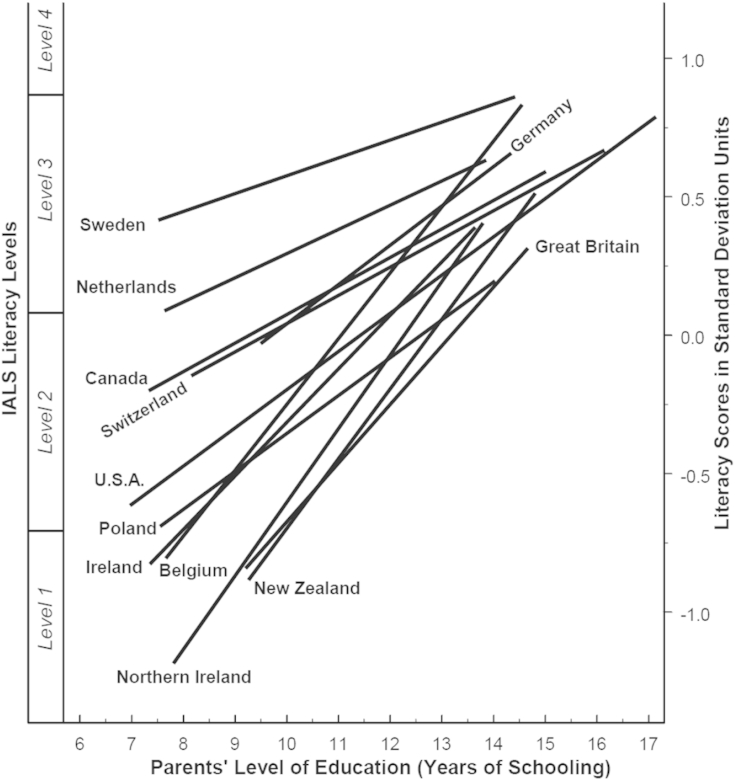
There is ample evidence that socioeconomic gradients in educational attainment remain significant across the UK. Analyses of the 2009 PISA data reveal gaps between the scores of children in the top and bottom SEP quartiles are very large (one standard deviation of the entire population distribution). Yet examination of data extending back two decades shows that such SEP differences in educational attainment are not inevitable, in that numerous countries in north-western Europe have achieved much smaller SEP gradients than any part of the UK (Fig. 5) (Willms, 2003). Work from Holland, Finland and Estonia highlights that “levelling the playing field of life” in those countries is largely attributable to the decades-long provision of universally accessible, high-quality preschool education, typically in local neighbourhood centres reachable by any parent, on foot, from their home, all year round (Sinclair, 2007). Data from 2007/08 to 2011/12 have shown that in Scotland “the attainment gap has remained unchanged. Even though overall leaver attainment increased slightly for all socioeconomic groups, the gap between children from the most and least deprived background remained the same”. (Sosu and Ellis, 2014). Similar patterns have been also been seen in England with earlier data (Goodman and Gregg, 2010).
Fig. 5.
Socioeconomic Gradients in Standardised Literacy Test Scores by Parental Education Level for 12 countries). Note, IALS = International Adult Literacy Survey. Source: Willms, 2003.
4. Investment #4: systematic support to enable universal secondary and – where appropriate – post-secondary – education and training, suited to full and productive employment
It is well established that education impacts positively upon health (Marmot, 2010). Findings from the UK National Child Development Study, tracking 15,000 people born in 1958, suggest that adults who attain secondary school qualifications have better health outcomes compared to adults with no qualifications (Feinstein et al., 2008). Despite this, inequalities in educational outcomes persist, with children from the most disadvantaged backgrounds most likely to perform poorly (Raffo et al., 2007).
Continued investment has been made in Scotland and England for providing financial support to 16–19 year olds attending school, through the Education Maintenance Allowance in Scotland and the 16–19 Bursary Fund (England) (Government, 2015). Machin et al. (2013) conclude that there are more similarities than differences between England and Scotland in terms of overall literacy and numeracy performance, with both countries performing well compared to the average scores for 32 OECD countries. However, closer inspection of data within countries reveals substantial educational inequalities according to SEP (Machin et al., 2013). For example, data from PISA 2009 indicate that 15 year olds from the lowest quartile SEP groups in both England and Scotland perform well below the average for literacy and numeracy for 32 OECD countries, compared to those in the highest quartile (Machin et al., 2013). There is good evidence that financial investment in schools and education impacts upon attainment, particularly for disadvantaged groups (Holmlund et al., 2011). Since 2002–03, spending per person on education was higher in Scotland than in the rest of the UK, peaking at 15.1% higher in 2006–07. However, the two countries' spending has since returned to comparable levels, with spending 0.4% higher in 2011–12 (Deaner and Phillips, 2013). It is unclear if this increased spend will have had any effect due to its relatively short duration from 2002 to 07. Returns on investment in education are unlikely to be visible immediately, and therefore current datasets based on tests of older children and youth, such as those utilised by Machin et al. (2013), may not yet have captured any longer term effects (Machin et al., 2013).
In Scotland, a recent key investment is the provision of free first-degree tuition for all residents enrolled in universities, with a view to reducing educational attainment inequalities by SEP. This was not pursued in England, which has recently adopted a policy of allowing universities to charge up to a ceiling of £9000 annually (Scottish Government, 2015). Current data from the UK Universities and Colleges Admission Service (UCAS) suggest that while higher education participation by students from intermediate and lower SEP backgrounds has risen across the four nations, it has done so at a similar rate to those from higher SEP backgrounds (1996–2010) (Croxford and Raffe, 2014). If anything, there may have been a relative decline in participation by lower SEP groups in Scotland (Croxford and Raffe, 2014).
As graduates of these variably-subsidised educational programmes throughout the UK work their way through the labour market in the future, one might expect to see in Scotland, compared to England, higher inter-generational upward mobility, in terms of final educational level attained, occupational status and income. However, current data suggest more similarities than differences.
5. Investment #5: accessible (free at point of care), high-quality primary, secondary and tertiary health care, combined with evidence-based public health services
The World Health Organisation (2012) defines the goal of universal health care as ensuring “that all people obtain the health services they need, of good quality, without suffering financial hardship when paying for them”. Universal health care is therefore a critical component of poverty reduction and any effort to reduce social inequalities (World Health Organisation, 2012).
The NHS provides universal health coverage in the UK, with minimum (subsidised) out-of-pocket expenses for medicines and services such as dentistry; specific provision varies slightly between the devolved jurisdictions. However, the primary evidence of the impact of universal health care comes from Canada which has a similar health care system to the UK with slightly less generous subsidies on medicines, dental and home care. James et al. (2007) evaluated the change in age-standardised expected years of life lost (SEYLL) in Canada from 1971 to 1996, with universal coverage having been introduced in 1968 (James et al., 2007). They found that the difference between the highest and lowest socioeconomic quintile in SEYLL from causes amenable to medical care (but not from other causes) had reduced by 60% (p < 0.001) in men and 78% (p < 0.001) in women (James et al., 2007). Like the UK, the different provinces in Canada have different policies towards funding medicines. Within Ontario medicines for those aged 65 years of age or older are publically funded. Booth et al. identified marked inequality gradients in mortality, myocardial infarction and stroke among the diabetic population across income quintiles, however these gradients were much reduced among those aged 65 years of age or older (Booth et al., 2012). In England, Barr et al. (2014) found that “between 2001 and 2011, the NHS health inequalities policy of increasing the proportion of resources allocated to deprived areas compared with more affluent areas was associated with a reduction in absolute health inequalities from causes amenable to health care” (Barr et al., 2014). These studies demonstrate that universal health coverage makes a significant contribution to reducing health inequalities.
Nolte and McKee (2011) studied 16 high-income countries and among those in Europe, the UK has the highest age-standardised rates of deaths from ”conditions that should be amenable to medical care”, but had also undergone one of the fastest reductions in such deaths between 1997/98 and 2006/07 (Nolte and McKee, 2011). Historically within the UK, Scotland is the country with the highest mortality (Young et al., 2010). However, residents of Scotland have similar or better self-reported health, receive a higher quality health service and subsequently have seen greater reductions in amenable deaths over time than residents of England, Wales or Northern Ireland (Young et al., 2010; Desai et al., 2011; McLean et al., 2007). The most recent Scottish report on the long term monitoring of health inequalities demonstrates relatively stable inequalities in almost a dozen routinely collected health outcomes (McCartney et al., 2013a), but there are some instances of absolute as well as relative inequalities increasing, which may at least partially be due to the post-2008 recession (Scottish Government, 2013). Although these annual reports are methodologically sophisticated, they rely entirely on routinely-collected health outcomes and hence have been subject to criticism for overreliance on outcomes that are inherently insensitive in the short-term to feasible policies and programmes (Frank and Haw, 2011, 2013). With the NHS in England, but not Scotland, undergoing significant changes and reorganisation, it is worth remembering that, as McKee et al. (2013) warn, universal health coverage should not be taken for granted. It is a key societal investment for achieving health equity (McKee et al., 2013).
6. Investment #6: strong, evidence-based economic and marketing controls on established health hazards, including: tobacco, alcohol, unhealthy foods, and gambling
Tobacco, alcohol, unhealthy foods and gambling are all products or activities which people pay to consume, and are marketed, for profit. Potential controls that could therefore be applied include consumption bans (universal or targeted at specific sub-populations, such as children, or specific locations, such as schools); pricing mechanisms to increase costs (assuming demand price elasticity); advertising and wider marketing bans; and sales restrictions (e.g. licensing hours, banning sales in certain outlets or locations). Other harm-reduction strategies exist for some products, such as curbs on food or tobacco product contents, or the types of gambling activities permitted in some jurisdictions. In this discussion, initiatives such as food or alcoholic drink labelling are not considered economic or marketing controls, as they fall more within the category of education or information provision.
Some economic measures and marketing restrictions have been employed across the UK jurisdictions to achieve the public health goals of reducing health-damaging behaviours and improving health and well-being. Given the varied policies and timescales of application we have chosen to focus on tobacco here. Policy summaries and prevalence rates of behaviours and health outcomes are available in Supplementary Document 1 for alcohol, diet/unhealthy foods and gambling taken from relevant cross-national comparative population-level data. The key objective of these kinds of investments is to reduce consumption, and, consequently, the harms associated with their consumption. Success could therefore be measured in terms of consumption (for example unit sales of tobacco), or in terms of negative outcomes (such as tobacco-related deaths). The robustness and availability of such measures is, of course, variable, and in many cases pragmatic choices need to be made where ideal indicators do not exist.
6.1. Tobacco
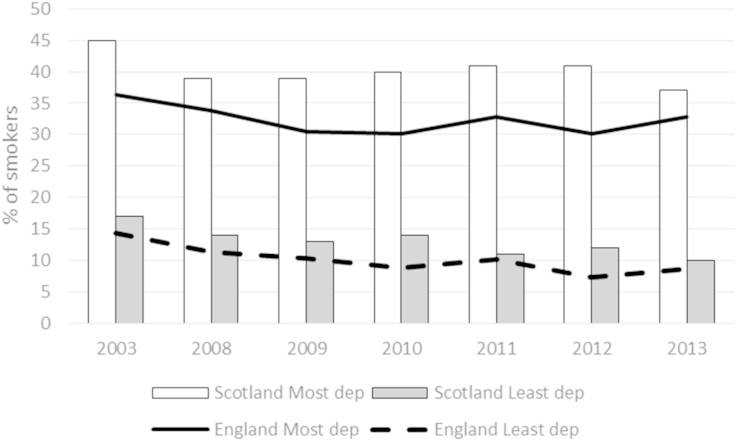
Tobacco restrictions include: a ban on smoking in enclosed public spaces (Scotland, March 2006; England, July 2007); raising the legal age to buy tobacco products to 18 years (October 2007, both countries); banning tobacco products from vending machines (Scotland, April 2013; England, October 2011); banning point-of-sale displays of tobacco products in large retail establishments (Scotland, April 2013; England, April 2012) and smaller stores (April 2015, both countries). Legal challenges from the tobacco industry (Scotland and England have separate legal systems) led to different implementation dates for some of these measures; sometimes, however, Scotland's politicians simply legislated sooner than their counterparts in England. Data from health surveys in Scotland and England over the last 20 years have shown that cigarette consumption has declined across both countries, particularly since the late 1990s. In Scotland, adult smoking prevalence is 23% and 20% for men and women respectively, while sitting at 24% and 17% in England (Craig and Mindell, 2014; Rutherford et al., 2014). Given the time differences in, for example the indoor smoking ban, natural experiments can be used to assess the effectiveness of policies that differ between similar jurisdictions. Pell et al. (2008) were able to use this technique to show that, overall, the number of admissions for acute coronary syndrome decreased by 17% in Scotland following the 2006 smoking ban. The comparable decline in England was 4% in the same time period (Pell et al., 2008). However, 67% of the decrease involved non-smokers (via reduced exposure to second-hand smoke). Therefore, while upstream interventions can have substantial health benefits across the population, changing behaviours in those who will experience the greatest health impact is a more difficult endeavour. Using data from the Scottish Health Survey and the Health Survey for England, both countries have seen smoking prevalence decline by approximately 6% between 2003 and 2013. However, the patterns by most and least deprived quintiles show that relative indices of inequality in both countries have increased similarly over this time-period (2.6–3.7 in Scotland and 2.5 to 3.8 in England) (Fig. 6). Absolute inequalities in Scotland did marginally decrease in Scotland (by 1%), but increased by 2.2% in England.
Fig. 6.
Cigarette smoking prevalence by most and least deprived quintile for England (Index of Multiple Deprivation) and Scotland (Scottish Index of Multiple Deprivation), 2003–2013. Source: Health Survey for England and Scottish Health Survey, UK Data Service.
The Nuffield Council on Bioethics' 2007 report ‘Public Health: Ethical Issues’ argues that strong, regulatory steps to reduce consumption of tobacco, alcohol, unhealthy foods and gambling require a higher level of evidence of effectiveness to justify their use, than would be the case for less interventionist approaches (Nuffield Council on Bioethics, 2007). The report states that “a more intrusive policy initiative is likely to be publicly acceptable only if it is clear that it will produce the desired effect and that this can be weighed against the loss of liberty that will result.” Similarly, the risks associated with such activities need to be demonstrably large enough to justify coercive policies. Additionally, to maximise health equity, and not just improve population health outcomes, any proposed steps must not contribute to the widening of inequalities. For example, mandatory food labelling (with calorie and nutritional contents) could increase inequalities if more educated people more readily apply this additional knowledge (Macintyre, 2007), whereas a ban on trans fats could have the opposite effect, as they are more commonly found in lower-priced food products, bought by economically disadvantaged people. However, with the results of the recent election in Westminster (2015), and the upcoming election in Holyrood (2016), it is unclear whether more equity-improving controls will be brought to bear on any of these chronic disease risk factors, all of which have either exposures or health consequences that are profoundly differential by SEP – in both Scotland and the rest of the UK.
7. Investment # 7: sustainable economic development policies that support full meaningful employment
Being out of work has been consistently associated with negative health outcomes, which include higher levels of mortality (Roelfs et al., 2011), mental ill-health (Paul and Moser, 2009), limiting longstanding illness (Bartley and Plewis, 2002), and poor self-rated health (Popham et al., 2012). This relates not only to being unemployed (not in work, but seeking employment), but also to those classed as being economically inactive (not in work and not seeking employment e.g. students, people looking after the family and home, long-term sick and disabled, temporarily sick and disabled, retired people and discouraged workers). The mechanisms linking negative health outcomes and a lack of employment fall under four main categories: relative poverty; social isolation and loss of self-esteem; health-related behaviours; and the effect of a period of unemployment on subsequent employment patterns (Bartley, 1994).
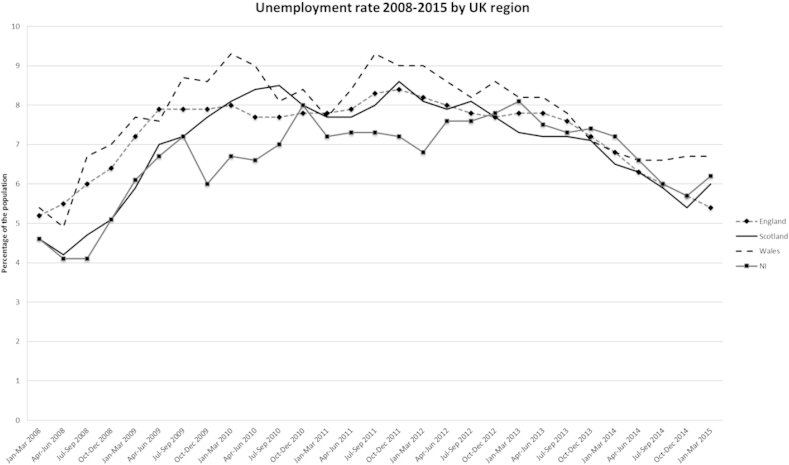
Focussing on unemployment, national data highlight a lack of any substantial difference in unemployment rates between January 2008–March 2015 (which includes the recent UK economic recession) when comparing Scotland with England, Wales and Northern Ireland for those aged 16+ (if anything, Wales has had the highest unemployment levels of the four UK regions) (Fig. 7). The pattern has also been similar for those economically inactive. However, these figures may disguise differences in working patterns across regions (e.g. low pay, part-time jobs, zero-hour contracts, in-work poverty, precariousness), smaller-scale regional differences and period/cohort effects (e.g. Scotland had higher rates of unemployment compared to the UK average in the 1980s during deindustrialisation) (McCartney et al., 2013b). Adult unemployment rates are currently around 6–8%, but youth unemployment (ages 16–24) are much higher, ranging from 11.6% (East Midlands) to 23.3% (North East) in England, with Scotland, Wales and Northern Ireland sitting at 13.8%, 21.2% and 21.0%, respectively (January–March 2015) (ONS) (ONS, 2015). This age group is also the only one to have seen continued rises in unemployment figures since 2010 (Aldridge et al., 2013). While a welcome downward trend in unemployment has been seen since late 2013, rates would appear closely linked to macro-level economic conditions (e.g. the global financial crisis) and still remain above those pre-2008.
Fig. 7.
Unemployment rate by UK region (2008–2015). Source: Labour Market Statistics, ONS (ONS, 2015).
Achieving and sustaining full, meaningful employment through sustainable and equitable economic development is a challenge for Scotland and all countries throughout the world. Improving employability for individuals is largely linked to “access to quality education, skills development, better health care, and equitable access to resources” (The Commonwealth, 2013). Most of the previous six investments aim to improve these very factors. A sustainable and equitable economy is built on the understanding and acceptance that all people in society deserve the opportunity to work and have an adequate standard of living. Some structures and polices that may help drive this goal include: a national, or even regional, living wage (compared to a minimum wage); more equitable pay structures/remuneration policies in both the public and private sector; financial incentives for the development and use of sustainable, green technologies and enterprises (e.g. renewable energy) with linked modern apprenticeships and training; grants for low-income students to help attend higher education; and changes in social attitudes towards benefits claimants (‘blame-culture). Where these policies fail and unemployment does occur, active labour market programmes are needed that: strengthen work incentives for people on benefits (tax credits; benefit conditions; conditional cash transfers); remove obstacles to employment and facilitate (re-)entry into the labour market (placements, subsidies, counselling, job search programmes); limit human capital depletion during unemployment (job creation schemes, unemployment-related training programmes); provide human capital investment (basic education, vocational training) (Bonoli, 2010). However, these policies may not be sufficient to deal with the harm that has already been caused years beforehand.
8. Conclusions
We conclude that, in recent years, Scotland shows evidence of more equitably distributed determinants of health, and the expected associated outcomes, across only one of the seven heterogeneous classes of outcomes reviewed above: child poverty rates. However, we are not convinced that the recently lower rates of child poverty in Scottish society are related to any deliberate policies and programmes deployed in Scotland, as argued above. Indeed, a January 2015 report on Health Inequalities, by the Scottish Parliamentary Committee on Health and Sport, points out that Scottish relative poverty increased between 2011/12 and 2012/13, from 15% to 19%, as the lengthy recession and further public sector cutbacks began to bite into local authority resources for anti-poverty measures, and welfare reforms began in earnest (Scottish Parliament, 2015).
In contrast, for the following important indicators of equity across major determinants of health that can be influenced by deliberate policies and programmes, we conclude that there is no clear evidence that Scotland has achieved more equitable outcomes than England, or the UK as a whole, in recent decades – indeed, in some cases, it may have done slightly worse:
-
•
Infant mortality and teenage pregnancy rates
-
•
Universal early childhood development and care programmes
-
•
Standardised educational attainment (e.g. PISA) scores (as well as the implementation of preschool, primary and secondary education policies which are capable of influencing these scores)
-
•
Any readily available indicators of health care system equity of performance across SEP
-
•
Any readily available indicators of the effectiveness of health protection programmes and policies aimed at equitably constraining population exposures to potentially hazardous consumption patterns for food, drink, tobacco, alcohol or gambling
-
•
Unemployment
On the other hand, there remains significant uncertainty about the longer-term effects of some differential policies recently pursued to a greater extent in Scotland, for any of the classes of outcome we have reviewed, across all seven “best investments.” That is simply because there has been an insufficient time period to provide definitive historical time-series data for these typically delayed outcomes, since policies and programmes began to diverge significantly in the devolved jurisdictions, just over a decade ago. Consequently, it is likely “too early to tell” whether Scotland may yet experience the often long-lagged effects of strongly redistributive policies, especially those affecting early life (Frank and Haw, 2011, 2013). However, the value and effectiveness of such upstream investments has been estimated by recent simulation modelling of Scottish data on health inequalities, suggesting that “living wage” legislation would have by far the largest impact on health inequalities, of a range of interventions modelled (Collins et al., 2014).
We note that the current post-referendum debate on Scottish independence, on both sides of the border, is remarkably silent on these issues. We call for that debate to be widened to address the pros and cons, and net costs, of further investments of these sorts, to equitably improve health over the lifecourse, in all parts of the UK. Without such investments, we doubt that Scotland can achieve its long-aspired-to vision of becoming a “healthier, wealthier and fairer society” (Scottish Government, 2007).
Acknowledgements
This work was funded by the SCPHRP core grant from the Medical Research Council (Grant Number MR/K023209/1) and the Chief Scientist Office of Scotland. The funders played no role in the conceptualisation or realisation of the research and no role in the decision to submit it for publication.
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.socscimed.2015.07.007.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Aldridge H., Kenway P., MacInnes T. New Policy Institute for Joseph Rowntree Foundation; York: 2013. Monitoring Poverty and Social Exclusion in Scotland 2013. [Google Scholar]
- Barr B., Bambra C., Whitehead M. The impact of NHS resource allocation policy on health inequalities in England 2001–11: longitudinal ecological study. BMJ. 2014;348:g3231. doi: 10.1136/bmj.g3231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartley M. Unemployment and ill health: understanding the relationship. J. Epidemiol. Community Health. 1994;48:333–337. doi: 10.1136/jech.48.4.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartley M., Plewis I. Accumulated labour market disadvantage and limiting long-term illness: data from the 1971–1991 Office for National Statistics' Longitudinal Study. Int. J. Epidemiol. 2002;31:336–341. [PubMed] [Google Scholar]
- Bonell C. Why is teenage pregnancy conceptualized as a social problem? A review of quantitative research from the USA and UK. Cult. Health Sex. 2004;6:255–272. doi: 10.1080/13691050310001643025. [DOI] [PubMed] [Google Scholar]
- Bonoli G. RECWOWE Publication, Dissemination and Dialogue Centre; Edinburgh, UK: 2010. The Political Economy of Active Labour Market Policy. REC-WP 01/2010, Working Papers on the Reconciliation of Work and Welfare in Europe. [Google Scholar]
- Booth G.L., Bishara P., Lipscombe L.L. Universal drug coverage and socioeconomic disparities in major diabetes outcomes. Diabetes Care. 2012;35:2257–2264. doi: 10.2337/dc12-0364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Academy, editor. “If You Could Do One thing…” Nine Local Actions to Reduce Health Inequalities. British Academy; London: 2014. [Google Scholar]
- Burchardt T., Holder H. Inequality and the devolved administrations: Scotland, Wales and Northern Ireland. In: Hills J., Sefton T., Stewart K., editors. Towards a More Equal Society? : Poverty, Inequality and Policy since 1997. Policy Press; Bristol: 2009. pp. 245–266. in association with the Joseph Rowntree Foundation. [Google Scholar]
- Children in Scotland . Children in Scotland; 2011. Early Childhood Education and Care: Developing a Fully Integrated System. [Google Scholar]
- Collins C., Denny C., Fischbacher C. NHS Health Scotland; Edinburgh, UK: 2014. Informing Investment to Reduce Health Inequalities (III) in Scotland: A Commentary. [Google Scholar]
- Craig R., Mindell J. The Health and Social Care Information Centre; Leeds, UK: 2014. Health Survey for England 2013: Health, Social Care and Lifestyles. [Google Scholar]
- Croxford L., Raffe D. Social class, ethnicity and access to higher education in the four countries of the UK. Int. J. Lifelong Educ. 2014;33:77–95. [Google Scholar]
- Culyer A.J. Edward Elgar Publishing; Cheltenham: 2005. The Dictionary of Health Economics. [Google Scholar]
- Deaner B., Phillips D. Institute for Fiscal Studies; London: 2013. Government Spending on Public Services in Scotland: Current Patterns and Future Issues. [Google Scholar]
- Desai M., Nolte E., Karanikolos M. Measuring NHS performance 1990–2009 using amenable mortality: interpret with care. J. R. Soc. Med. 2011;104:370–379. doi: 10.1258/jrsm.2011.110120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewar D. Scottsih Government; Edinburgh, UK: 1998. £500,000 to Help Unemployed in Highlands and Islands. [Google Scholar]
- Dickens R. Child poverty in Britain: past lessons and future prospects. Natl. Inst. Econ. Rev. 2011;218:7. [Google Scholar]
- European Commission . European Commission; Belgium: 2013. Health Inequalities in the EU: Final Report of a Consortium Consortium Lead: Sir Michael Marmot Brussels. [Google Scholar]
- Feinstein L., Budge D., Vorhaus J. Centre for Research on the Wider Benefits of Learning, Institute of Education; London: 2008. The Social and Personal Benefits of Learning: A Summary of Key Research Findings. [Google Scholar]
- Frank J., Haw S. Best practice guidelines for monitoring socioeconomic inequalities in health status: lessons from Scotland. Milbank Q. 2011;89:658–693. doi: 10.1111/j.1468-0009.2011.00646.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank J.W., Haw S. Commentary: persistent social inequalities in health—insensitive outcomes, inadequate policies, or both? Milbank Q. 2013;91:192–200. doi: 10.1111/milq.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman A., Gregg P. Joesph Rowntree Foundation; York, UK: 2010. Poorer Children's Educational Attainment: How Important Are Attitudes and Behaviour? [Google Scholar]
- Government U.K. UK Government; London: 2015. 16 to 19 Education: Financial Support for Students. [Google Scholar]
- Hanlon P., Lawder R.S., Buchanan D. Why is mortality higher in Scotland than in England and Wales? decreasing influence of socioeconomic deprivation between 1981 and 2001 supports the existence of a 'Scottish Effect'. J. Public Health. 2005;27:199–204. doi: 10.1093/pubmed/fdi002. [DOI] [PubMed] [Google Scholar]
- Harden A., Brunton G., Fletcher A. Teenage pregnancy and social disadvantage: systematic review integrating controlled trials and qualitative studies. BMJ. 2009;339:b4254. doi: 10.1136/bmj.b4254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoddinott P., Craig L., Maclennan G. The FEeding Support Team (FEST) randomised, controlled feasibility trial of proactive and reactive telephone support for breastfeeding women living in disadvantaged areas. BMJ Open. 2012;2:e000652. doi: 10.1136/bmjopen-2011-000652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmlund H., McNally S., Viarengo M. Does money matter for schools? Econ. Educ. Rev. 2011;29:1154–1164. [Google Scholar]
- Information Service Division Scotland . 2014. Teenage Pregnancy, Year of Conception Ending 31st December 2012. [Google Scholar]
- James P.D., Wilkins R., Detsky A.S. Avoidable mortality by neighbourhood income in Canada: 25 years after the establishment of universal health insurance. J. Epidemiol. Community Health. 2007;61:287–296. doi: 10.1136/jech.2006.047092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N., Williams D.R., Moss N.E. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu. Rev. Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- Machin S., McNally S., Wyness G. Educational attainment across the UK nations: performance, inequality and evidence. Educ. Res. 2013;55:139–164. [Google Scholar]
- Macintyre S. 2007. Inequalities in Health in Scotland: What Are They and what Can We Do about Them? Occasional Paper 17. Glasgow. [Google Scholar]
- Marmot M. Institute of Health Equity; London: 2010. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post 2010. [Google Scholar]
- Marmot M., Wilkinson R. second ed. World Health Organisation; Copenhagen, Denmark: 2003. Social Determinants of Health: The Solid Facts. [Google Scholar]
- Marmot M., Friel S., Bell R. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- McCartney G., Leyland A.H., Fischbacher C.M. Commentary: long-term monitoring of health inequalities in Scotland—a response to Frank and Haw. Milbank Q. 2013;91:186–191. doi: 10.1111/milq.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCartney G., Myers F., Taulbut M. NHS Health Scotland; Edinburgh, UK: 2013. Making a Bad Situation Worse? the Impact of Welfare Reform and the Economic Recession on Health and Health Inequalities in Scotland (Baseline Report) [Google Scholar]
- McKee M., Balabanova D., Basu S. Universal health coverage: a quest for all countries but under threat in some. Value Health. 2013;16:S39–S45. doi: 10.1016/j.jval.2012.10.001. [DOI] [PubMed] [Google Scholar]
- McLean G., Guthrie B., Sutton M. Differences in the quality of primary medical care for CVD and diabetes across the NHS: evidence from the quality and outcomes framework. BMC Health Serv. Res. 2007;7:74. doi: 10.1186/1472-6963-7-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mostafa T., Green A. LLAKES Institute of Education; London: 2012. Measuring the Impact of Universal Pre-school Education and Care on Literacy Performance Scores. [Google Scholar]
- Neumann I., McLean C., Koslowiski A. The Scottish Government; Edinburgh: 2013. International Review of Policy, Delivery and Funding. [Google Scholar]
- Nolte E., McKee M. Variations in amenable mortality-trends in 16 high-income nations. Health Policy. 2011;103:47–52. doi: 10.1016/j.healthpol.2011.08.002. [DOI] [PubMed] [Google Scholar]
- Nores M., Barnett W. Benefits of early childhood interventions across the world: (under) investing in the very young. Econ. Educ. Rev. 2010;29:271–282. [Google Scholar]
- Nuffield Council on Bioethics . 2007. Public Health: Ethical Issues. [Google Scholar]
- ONS . Office for National Statistics; London, UK: 2012. Using Indices of Deprivation in the United Kingdom: Guidance Paper. [Google Scholar]
- ONS (2015). http://www.ons.gov.uk/ons/rel/lms/labour-market-statistics/index.html.
- Paul K.I., Moser K. Unemployment impairs mental health: meta-analyses. J. Vocat. Behav. 2009;74:264–282. [Google Scholar]
- Pell J.P., Haw S., Cobbe S. Smoke-free legislation and hospitalizations for acute coronary syndrome. N. Engl. J. Med. 2008;359:482–491. doi: 10.1056/NEJMsa0706740. [DOI] [PubMed] [Google Scholar]
- Popham F., Boyle P. 2010. Assessing Socio-economic Inequalities in Mortality and Other Health Outcomes at the Scottish National Level. [Google Scholar]
- Popham F., Gray L., Bambra C. Employment status and the prevalence of poor self-rated health. Findings from UK individual-level repeated cross-sectional data from 1978 to 2004. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-001342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poverty UK (2011). http://www.poverty.org.uk/21/index.shtml.
- Raffo C., Dyson A., Gunter H. Joseph Rowntree Foundation; London: 2007. Education and Poverty: A Criticial Review of Theory, Policy and Practice. [Google Scholar]
- Roberts H. The Policy Press; Chicago: 2012. What Works in Reducing Inequalities in Child Health? [Google Scholar]
- Roelfs D.J., Shor E., Davidson K.W. Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Soc. Sci. Med. 2011;72:840–854. doi: 10.1016/j.socscimed.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutherford L., Hinchcliffe S., Sharp C. vol. 1. The Scottish Government; Edinburgh, UK: 2014. (The Scottish Health Survey 2013). Main Report. [Google Scholar]
- Schoen C., Osborn R., Squires D. How health insurance design affects access to care and costs, by income, in eleven countries. Health Aff. 2010;29:2323–2334. doi: 10.1377/hlthaff.2010.0862. [DOI] [PubMed] [Google Scholar]
- Scottish Government . Scottish Government; Edinburgh: 2006. Preschool and Childcare Workforce Statistics 2005. [Google Scholar]
- Scottish Government . Scottish Government; Edinburgh, UK: 2007. Strategic Objectives for Scotland. [Google Scholar]
- Scottish Government . The Scottish Government; Edinburgh: 2013. Statistical Bulletin: Health & Social Care Series – Long-term Monitoring of Health Inequalities October 2013 Report. [Google Scholar]
- Scottish Government . Scottish Government; Edinburgh: 2015. Financial Help for Students. [Google Scholar]
- Scottish Parliament . Scottish Parliament; Edinburgh, UK: 2013. Health and Sport Committee: Inquiry into Teenage Pregnancy. [Google Scholar]
- Scottish Parliament . Scottish Parliament; Edinburgh, UK: 2015. Report of the Health and Sport Committee: Health Inequalities. [Google Scholar]
- Sinclair A. The Work Foundation; London: 2007. 0–5: How Small Children Make a Big Difference. [Google Scholar]
- Sinclair S., McKendrick J.H. From social inclusion to solidarity. In: McKendrick J.H., Mooney G., Dickie J., editors. Poverty in Scotland 2011. Child Poverty Action Group; London: 2011. pp. 61–79. [Google Scholar]
- Smith L.K., Draper E.S., Manktelow B.N. Socioeconomic inequalities in survival and provision of neonatal care: population based study of very preterm infants. BMJ. 2009;339 doi: 10.1136/bmj.b4702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sosu E., Ellis S. Joesph Rowntree Foundation; York UK: 2014. Closing the Attainment Gap in Scottish Education. [Google Scholar]
- Tappin D., Bauld L., Purves D. Financial incentives for smoking cessation in pregnancy: randomised controlled trial. BMJ. 2015;350 doi: 10.1136/bmj.h134. [DOI] [PubMed] [Google Scholar]
- Taylor-Robinson D., Whitehead M., Barr B. Great leap backwards. BMJ. 2014;349:g7350. doi: 10.1136/bmj.g7350. [DOI] [PubMed] [Google Scholar]
- Teenage Pregnancy Independent Advisory Group . 2010. Final Report: Teenage Pregnancy: Past Successes – Future Challenges. (London) [Google Scholar]
- Temple J., Reynolds A. Benefits and costs of investments in preschool education: evidence from the child-parent centres and related programs. Econ. Educ. Rev. 2007;26:126–144. [Google Scholar]
- The Commonwealth . 2013. Commonwealth Heads of Government Meeting (CHOGM), 15-17 November, 2013, Colombo Declaration on Sustainable, Inclusive and Equitable Development. [Google Scholar]
- Unicef . 2007. Child Poverty and Perspective: An Overview of Child Wellbeing in Rich Countries. [Google Scholar]
- Weightman A.L., Morgan H.E., Shepherd M.A. Social inequality and infant health in the UK: systematic review and meta-analyses. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-000964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willms J. Literacy proficiency of youth: evidence of converging socioeconomic gradients. Int. J. Educ. Res. 2003;39:247–252. [Google Scholar]
- Wincott D. Paradoxes of new labour social policy: toward universal child care in Europe's “Most Liberal” welfare regime? social politics: International studies in gender. State Soc. 2006;13:286–312. [Google Scholar]
- Woolfson L., King J. The Scottish Government; Edinburgh: 2008. Evaluation of the Extended Preschool Provision for Vulnerable Two-year-olds Pilot Programme. [Google Scholar]
- World Health Organisation . World Health Organization; Geneva: 2012. Online Q&A: What Is Universal Health Coverage? [Google Scholar]
- Young H., Grundy E., O'Reilly D. Self-rated health and mortality in the UK: results from the first comparative analysis of the England and Wales, Scotland, and Northern Ireland Longitudinal Studies. Popul. Trends. 2010:11–36. doi: 10.1057/pt.2010.3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.