Abstract
Background and Objectives:
Bariatric surgery has been shown to be an effective weight loss treatment for the morbidly obese, but some primary care physicians remain hesitant about postoperative treatment and management of patients who have undergone the surgery and recommend it to their obese patients infrequently. The purpose of this study was to evaluate perceptions of primary care physicians of the role of bariatric surgery in the management of obese patients and to identify possible barriers to treatment.
Methods:
A survey of PCPs within our institution was conducted to determine attitudes, knowledge, and practices regarding the treatment of morbidly obese patients, with a specific focus on identifying factors that influence referral patterns for bariatric surgery.
Results:
Among 161 eligible PCPs, 57 (35.4%) responded. Most respondents (59%) reported that at least 1 in 4 of their patients had a BMI ≥35 kg/m2. Although 39% thought that diet and exercise were an effective means of sustained weight loss, only 12% were satisfied with prescribing nonsurgical interventions. Sixty-three percent agreed that bariatric surgery is generally effective in the long term. All respondents were aware of the commonly established benefits, including improvement of diabetes, hypertension, and hyperlipidemia. In addition, 65% were familiar with the indications for bariatric surgery, and 70% felt comfortable discussing it with patients as a treatment option. Fewer than half of the respondents felt confident in providing postoperative management. Cost was a perceived limitation, with 53% reporting that most of their patients could not afford bariatric surgery.
Conclusions:
The general attitude of PCPs toward bariatric surgery is supportive. Physicians are largely aware of the indications and benefits; however, far fewer are comfortable in management of patients after surgery. A lack of supplemental information and concerns regarding the cost of surgery can impede treatment and referrals.
Keywords: Attitudes, Bariatric surgery, Consultation and referral physicians, Primary care
INTRODUCTION
Obesity has become epidemic in the United States. Studies have demonstrated that diet and lifestyle modifications are relatively ineffective in treating morbid obesity in the long term; that there are currently no effective pharmaceutical agents to treat obesity; that bariatric surgery is the only effective and currently available therapy for sustained weight loss in the morbidly obese; and that most patients with diabetes, hyperlipidemia, hypertension, and obstructive sleep apnea experience complete resolution or improvement of obesity-related comorbidities after undergoing bariatric surgery.1
Although primary care physicians (PCPs) acknowledge the benefits of bariatric surgery for patients who qualify, it is infrequently recommended, and referral rates for surgical evaluation and treatment are not consistent with the number of those affected.2–6 A national survey demonstrated that PCPs identify a need for additional education to improve obesity care.7 Although most PCPs believe obesity can be successfully managed, an equal number express lack of confidence in their ability to treat bariatric patients.3,4 The purpose of this study was to evaluate PCPs' perceptions of the role of bariatric surgery in the treatment of obese patients and to identify possible barriers to recommending it.
METHODS
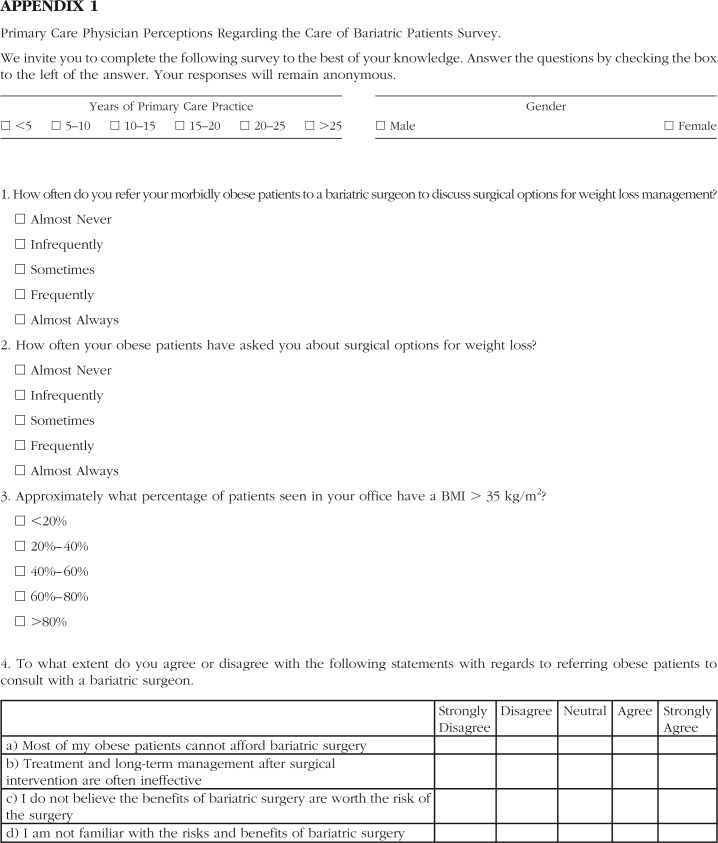
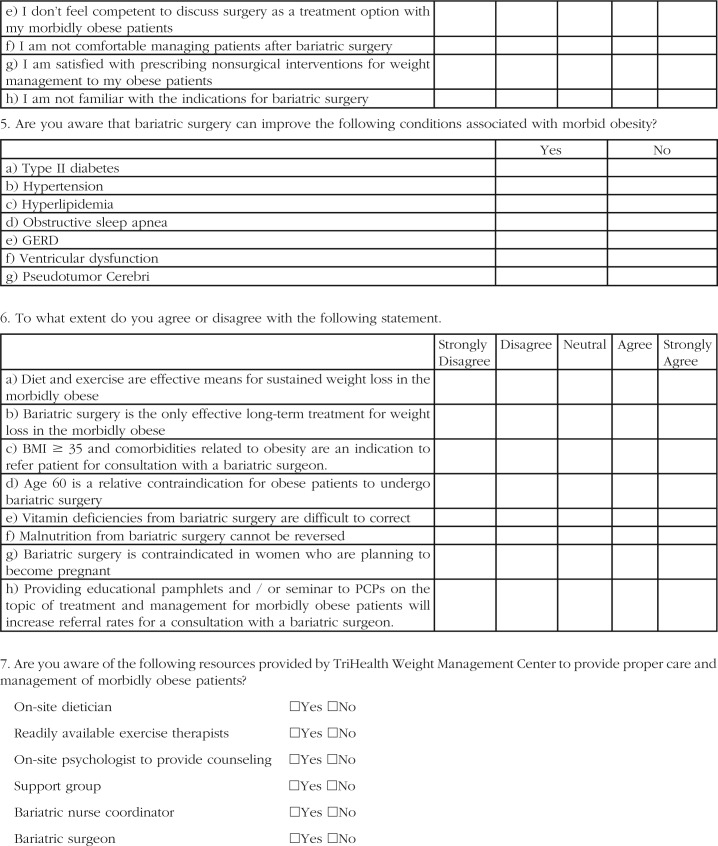
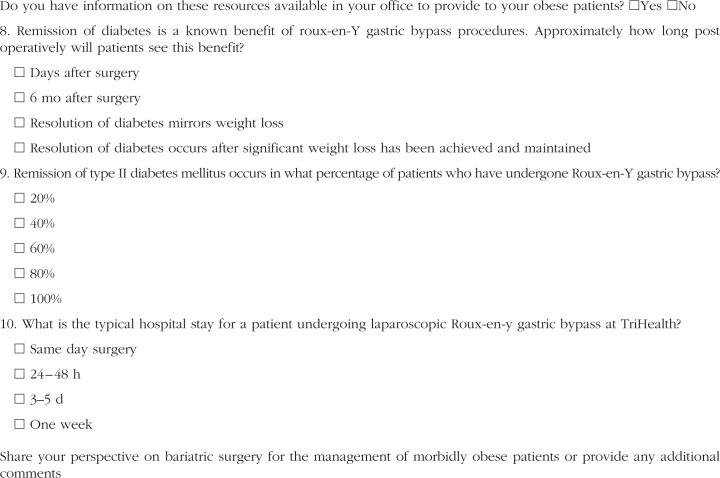
The study was approved by the Institutional Review Board of The Good Samaritan TriHealth Hospital. A 10-item survey was created to elicit PCPs' attitudes, knowledge, and practices regarding treatment and management of morbidly obese patients (Appendix 1). Survey questions addressed attitudes and perception toward treatment and management of bariatric patients, overall knowledge regarding benefits of bariatric surgery, and awareness of institutional resources available for these patients. The survey was pilot tested for content validity and clarity of questions. A comments section was also provided for feedback. Responses were graded on a 5-point Likert scale (1, strongly disagree; 2, disagree; 3, neutral; 4, agree; and 5, strongly agree). The responses were also dichotomized as follows: strongly disagree/disagree versus strongly agree/agree. All PCPs (internists and family practitioners) affiliated with our independent academic medical center were invited to complete the survey anonymously. PCPs were asked to report the frequency of bariatric referrals and consultations. Descriptive statistics were reported and analyses were performed by using R statistical analysis software (version 3.0.3) with the extension package “Likert” for creating graphs.8,9
RESULTS
Among 161 eligible PCPs, 57 (35.4%) completed the survey. Sixty-one percent of the respondents were men and 39% were women. Fifty percent had been in practice for more than 20 years. Most respondents (n = 79; 59%), reported that at least 1 in 4 of their patients had a BMI ≥35 kg/m2; however, only 6 (9%) indicated that they frequently or almost always referred their morbidly obese patients to bariatric surgeons. Fifty-one percent (n = 29) of the respondents reported that their obese patients asked about surgical options for weight loss. Seventy percent (n = 39) felt comfortable discussing it as a treatment option with their morbidly obese patients; however, fewer than half (25; 44%) felt confident in providing postoperative management. Twenty-two (39%) believed that diet and exercise are an effective means of obtaining sustained weight loss, but only 12% (n = 7) were satisfied with prescribing nonsurgical interventions. Sixty-three percent (n = 36) agreed that long-term management with bariatric surgery is generally effective. Cost was a commonly cited limitation, with 53% (n = 30) reporting that most of their patients could not afford bariatric surgery (Figure 1).
Figure 1.
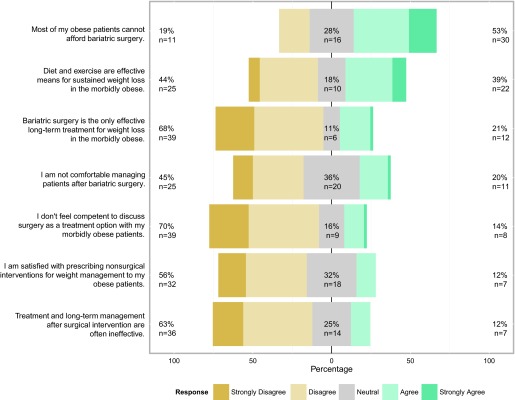
Factors influencing referral for bariatric surgery.
All respondents were aware of the commonly established benefits of bariatric surgery, including improvement of diabetes, hypertension, and hyperlipidemia. In addition, 65% (n = 37) believed that they were familiar with indications for bariatric surgery, whereas 85% (n = 48) indicated awareness based on our questions. Thirteen percent (n = 7) believed that vitamin deficiencies caused by bariatric surgery are difficult to correct, and 2% (n = 1) thought that malnutrition after bypass could not be reversed. Nine percent (n = 5) of the respondents thought that the risks of surgery outweigh the benefits. Sixty-three percent (n = 36) believed that providing educational pamphlets and seminars to PCPs on the topic of treatment and management of morbidly obese patients would increase referrals for bariatric surgery (Table 1).
Table 1.
Primary Care Physicians' Attitudes Toward Bariatric Surgery
| Statement | Total responses N | Strongly Disagree n (%) | Disagree n (%) | Neutral n (%) | Agree n (%) | Strongly Agree n (%) |
|---|---|---|---|---|---|---|
| Vitamin deficiencies from bariatric surgery are difficult to correct. | 57 | 10 (18) | 35 (61) | 5 (9) | 6 (11) | 1 (2) |
| Providing educational pamphlets and/or seminars to PCPs on the topic of treatment and management for morbidly obese patients will increase referral rates for a consultation with a bariatric surgeon. | 57 | 1 (2) | 4 (7) | 16 (28) | 28 (49) | 8 (14) |
| Malnutrition after bariatric surgery cannot be reversed. | 52 | 15 (29) | 29 (56) | 7 (13) | 1 (2) | 0 |
| I do not believe the benefits of bariatric surgery are worth the risk of the surgery. | 56 | 7 (12) | 28 (50) | 16 (29) | 5 (9) | 0 |
| I am not familiar with the risks and benefits of bariatric surgery. | 55 | 20 (36) | 26 (47) | 6 (11) | 2 (4) | 1 (2) |
| I am not familiar with the indications for bariatric surgery. | 57 | 11 (19) | 26 (46) | 16 (28) | 4 (7) | 0 |
| BMI ≥35 and comorbidities related to obesity are an indication to refer patient for consultation with a bariatric surgeon. | 57 | 0 | 5 (9) | 4 (7) | 38 (67) | 10 (18) |
Nearly half of the respondents (n = 26; 46%) were unaware of the resources provided by our institution's weight management center, and only 26% (n = 15) had information about the availability of bariatric surgery for their morbidly obese patients. There was no significant difference in referral patterns based on the sex of the PCP or the number of years in practice. There was also no significant difference in attitudes and general knowledge base regarding bariatric surgery between referring and nonreferring PCPs (Table 2).
Table 2.
Relationship of Primary Care Physician Responses to Referral Status
| Statement | Referring PCP |
Nonreferring PCP |
||
|---|---|---|---|---|
| Disagree n (%) | Agree n (%) | Disagree n (%) | Agree n (%) | |
| Most of my obese patients cannot afford bariatric surgery. | 10 (24) | 22 (54) | 1 (6) | 8 (50) |
| I am not comfortable managing bariatric patients after surgery. | 18 (45) | 8 (20) | 7 (44) | 3 (19) |
| I am satisfied with prescribing nonsurgical interventions for weight management to my obese patients. | 21 (51) | 4 (10) | 11 (69) | 3 (19) |
| Diet and exercise are effective means for sustained weight loss in the morbidly obese. | 18 (44) | 16 (39) | 7 (44) | 6 (38) |
| Bariatric surgery is the only effective long-term treatment for weight loss in the morbidly obese. | 27 (66) | 10 (24) | 12 (75) | 2 (12) |
| I do not believe the benefits of bariatric surgery are worth the risk of the surgery. | 27 (66) | 3 (7) | 8 (53) | 2 (13) |
DISCUSSION
Obesity has become epidemic in America, requiring health care providers to stay abreast of counseling and treatment options. A review from Mayo Clinic10 describes the role of PCPs as essential in identifying potential candidates for bariatric surgery. With the increased use of surgery to treat obesity comes a need for PCPs, not only to screen patients who would benefit from an operation, but also to become familiar with principles that guide follow-up care and lifelong monitoring. A similar review by the Cleveland Clinic echoed the importance of having PCPs as part of a multidisciplinary team to provide comprehensive care to bariatric patients.11
Our study revealed that PCPs within our institution had at least a general understanding of the short- and long-term benefits of bariatric surgery. All physicians responding to the survey were aware of the major medical benefits, and many commented on personal experience with postoperative success in their patients. However, our study also confirmed the report by Sarwer et al12 that although PCPs acknowledge the benefit of bariatric surgery, they seem reluctant to refer patients. We did not observe any significant differences based on the sex of our respondents, as opposed to a survey study by Sansone et al,5 in which female PCPs were less supportive of bariatric surgery. Studies have also suggested that PCPs have a negative attitude toward obese patients and feel ineffective in managing this disease.13,14
Our study showed that 2 of the primary barriers to referrals to a bariatric surgeon were high costs and insufficient insurance coverage. Our survey did not query regarding the knowledge of actual cost or insurance coverage for bariatric surgeries and therefore does not show whether the barrier is caused by a knowledge or perception gap.
Nearly half of the respondents in our study were unaware of the comprehensive long-term weight loss services (dietician, exercise therapists, psychologist, and support groups) offered by our institutional weight management center, and just as many were unaware of how to provide such services to patients. Our failure to provide sufficient awareness of our weight management center to our PCP colleagues is a likely contributor to the low degree of confidence expressed in treating and managing this patient population. According to a study by Forman-Hoffman et al,15 lack of information for both clinicians and patients is a perceived barrier in the management of obesity.
In a survey of PCPs, Perlman et al16 found that, in addition to general misconceptions and lack of knowledge about bariatric surgery, fears of complication and death are the most common reasons for avoiding referrals to a bariatric surgeon. Although our survey did not identify a lack of knowledge as a barrier in referral patterns and we did not study fear of adverse outcomes, it did reveal that the existence of institutional resources does not guarantee their optimal use and that communication between disciplines is essential.
Additional studies are needed to establish which educational programs will best serve and foster advancements in the medical and surgical care of the morbidly obese. A multidisciplinary approach to bariatric patients will promote better outcomes and quality of life. We believe that efforts should be made to develop educational programs that can assist PCPs in treating and referring obese patients for surgery. Referral patterns are based on a certain level of comfort, and a lack of knowledge about surgery can impede the referral process.10,16
The findings of our study may have limited generalizability because of the low response rate and small sample size. The results, however, suggest a recurring theme that, although PCPs may acknowledge the benefits of bariatric surgery, they seem reluctant to refer patients. In addition, the questions on the survey were not from a validated questionnaire, but instead were constructed from an extensive review of the literature. Questions may be subject to biases and interests of the investigators, thus again limiting the generalizability of the results. It is possible that the wording or the structure of the questions in some way encouraged a positive or a negative response by some PCPs; therefore, our conclusions should be interpreted with caution.
We considered qualitative methods, such as focus groups and in-depth interviews, as the means of data collection, but we opted to conduct an anonymous survey, to reduce the influence of social-desirability response bias and to maintain the confidentially of the results. Our decision does not underestimate the extent to which a focus group or an in-depth interview provides reliable and valid information. To explore general practitioners' beliefs about obesity management, one group used a qualitative method, with in-depth, semistructured interviews, yet recognized that the responses to the questions in the interview may have been influenced by their own views and perspectives.17
CONCLUSION
The general attitude among PCPs toward bariatric surgery is supportive. Physicians are largely aware of the indications and benefits; however, far fewer are comfortable in the management of patients after surgery. Use of weight management centers by PCPs and patients is dependent on the visibility of these resources. A lack of supplemental information and concerns regarding the cost of surgery can impede treatment and referrals.
APPENDIX 1
Contributor Information
Shahryar Tork, Department of Surgery.
Katherine M. Meister, Department of Surgery.
Anna L. Uebele, Department of Surgery.
Lala R. Hussain, TriHealth Hatton Research Institute.
Scott R. Kelley, Division of Colon and Rectal Surgery.
George M. Kerlakian, TriHealth Weight Management Center, Good Samaritan TriHealth Hospital, Cincinnati, Ohio..
Kevin M. Tymitz, TriHealth Weight Management Center, Good Samaritan TriHealth Hospital, Cincinnati, Ohio..
References:
- 1. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–1737. [DOI] [PubMed] [Google Scholar]
- 2. Avidor Y, Still CD, Brunner M, Buchwald JN, Buchwald H. Primary care and subspecialty management of morbid obesity: referral patterns for bariatric surgery. Surg Obes Relat Dis. 2007;3:392–407. [DOI] [PubMed] [Google Scholar]
- 3. Ferrante JM, Piasecki AK, Ohman-Strickland PA, Crabtree BF. Family physicians' practices and attitudes regarding care of extremely obese patients. Obesity (Silver Spring). 2009;17:1710–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Salinas GD, Glauser TA, Williamson JC, Rao G, Abdolrasulnia M. Primary care physician attitudes and practice patterns in the management of obese adults: results from a national survey. Postgrad Med. 2011;123:214–219. [DOI] [PubMed] [Google Scholar]
- 5. Sansone RA, McDonald S, Wiederman MW, Ferreira K. Gastric bypass surgery: a survey of primary care physicians. Eat Disord. 2007;15:145–152. [DOI] [PubMed] [Google Scholar]
- 6. Woolford SJ, Clark SJ, Gebremariam A, Davis MM, Freed GL. To cut or not to cut: physicians' perspectives on referring adolescents for bariatric surgery. Obes Surg. 2010;20:937–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bleich SN, Bennett WL, Gudzune KA, Cooper LA. National survey of US primary care physicians' perspectives about causes of obesity and solutions to improve care. BMJ Open. 2012;2:e001871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bryer J, Speerschneider K. Likert: functions to analyze and visualize Likert type items. R package version 1.1. Vienna, Austria: R Foundation for Statistical Computing, October 17, 2014. Available at: http://jason.bryer.org/likert. [Google Scholar]
- 9. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2014. Available at: http://www.r-project.org/. [Google Scholar]
- 10. Presutti RJ, Gorman RS, Swain JM. Primary care perspective on bariatric surgery. Mayo Clinic Proceed. 2004;79:1158–1166, 2004; quiz 1166. [DOI] [PubMed] [Google Scholar]
- 11. Choban PS, Jackson B, Poplawski S, Bistolarides P. Bariatric surgery for morbid obesity: why, who, when, how, where, and then what? Cleve Clin J Med. 2002;69:897–903. [DOI] [PubMed] [Google Scholar]
- 12. Sarwer DB, Ritter S, Wadden TA, Spitzer JC, Vetter ML, Moore RH. Physicians' attitudes about referring their type 2 diabetes patients for bariatric surgery. Surg Obes Relat Dis. 2012;8:381–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bocquier A, Paraponaris A, Gourheux JC, Lussault PY, Basdevant A, Verger P. Obesity management knowledge, attitudes and practices of general practitioners in southeastern France: results of a telephone survey [in French]. Presse Med. 2005;34:769–775. [DOI] [PubMed] [Google Scholar]
- 14. Foster GD, Wadden TA, Makris AP, et al. Primary care physicians' attitudes about obesity and its treatment. Obes Res. 2003;11:1168–1177. [DOI] [PubMed] [Google Scholar]
- 15. Forman-Hoffman V, Little A, Wahls T. Barriers to obesity management: a pilot study of primary care clinicians. BMC Fam Pract. 2006;7:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Perlman SE, Reinhold RB, Nadzam GS. How do family practitioners perceive surgery for the morbidly obese? Surg Obes Relat Dis. 2007;3:428–433. [DOI] [PubMed] [Google Scholar]
- 17. Epstein L, Ogden J. A qualitative study of GPs' views of treating obesity. Br J Gen Pract. 2005;55:750–754. [PMC free article] [PubMed] [Google Scholar]