Abstract
Background:
Isolates of Staphylococcus aureus express a myriad of adhesive surface proteins that play important role in colonization of the bacteria on nasal and skin surfaces, beginning the process of pathogenesis. The aim of this study was to screen several of the Microbial Surface Components Recognizing Adhesive Matrix Molecules (MSCRAMMs) genes among the isolate of S. aureus from hospitalized children.
Methods:
A total of 22 S. aureus isolates were collected from hospitalized children in Tehran from 2012 to 2013. Detection of the mecA and several adhesive surface proteins genes including clfA, B (encoding clumping factors A, B); fnbA, B (encoding finronectin binding proteins A, B); fib (encoding fibrinogen binding protein); eno (encoding laminin binding protein); cna (encoding collagen binding protein); ebps (encoding elastin binding protein) and bbp (encoding bone sialo-protein binding protein), was performed by PCR.
Results:
The clfAB genes were detected among all the isolates. The prevalence of fnbA, fnbB, fib, eno, cna, ebps and bbp was 63%, 6%, 50%, 59%, 82%, 63%, 9% and 0%, respectively.
Conclusion:
The high prevalence of these genes is important for future plans in vaccine designation. MRSA and MSSA isolates similarly can produce adhesive surface proteins for colonization.
Key Words: Staphylococcus aureus, Surface Proteins, Virulence, Pediatrics, MRSA
Introduction
Staphylococcus aureus is a ubiquitous bacterial human pathogen in both community- and nosocomial sources, although referred as a human normal flora as well (1). These isolates asymptomatically colonize on surfaces of healthy individuals, and thus the carriers can spread these infectious pathogens. S. aureus co-infections with viral influenza cause deaths among children (2). Especially for Community-associated methicillin-resistant S. aureus (CA-MRSA) strains play important role in children infections via producing the Panton Valentine Leukocidin (PVL) and some other toxins. This pathogen has also been associated with high morbidity and mortality in pediatric oncology patients detected in pulmonary nodules (3). Furthermore, several “new” clinical syndromes, such as severe sepsis and Waterhouse–Friderichsen syndrome, can cause high mortality among children (4).
Infants born to mothers with staphylococcal colonization have been more likely to be colonized (5). S. aureus primarily inhabits in the moist squamous epithelium in the anterior nares of colonized individuals (6), although the bacterium is capable of colonizing in a number of different anatomical sites including the nasopharynx via a numerous surface-attached (adhesive) and secreted proteins. Thus, colonized individuals may be at risk of endogenous infections with S. aureus that has entered in the sterile sites of the body through several routes, such as wounds and indwelling medical devices (7).
Microbial surface components recognizing adhesive matrix molecules (MSCRAMMs) on S. aureus surface, mediate staphylococcal adherence to components of the extracellular matrix of the host (8). These components are attached covalently to peptidoglycan by sortase enzymes (9). Furthermore, these components participate in biofilm formation, in addition to the ica operon that produces the polysaccharide intercellular adhesion [PIA] (10). Clumping factor A (ClfA) is the major staphylococcal fibrinogen (Fg) binding protein and is responsible for the observed clumping of S. aureus in blood plasma, culminating in arthritis and endocarditis (11). MSCRAMMs play a key role in initiation of endovascular, bone and joint and prosthetic-device infections (12). These structures can bind to molecules such as collagen (mostly via Cna), fibronectin (via FnbAB), and fibrinogen (with ClfAB and Fib) and thus evade immune system, and then can develop infections (13, 14). The aim of this study was to screen the MSCRAMMs genes among the isolates of S. aureus from hospitalized children.
Material and Methods
Bacterial isolates
A total of 22 S. aureus clinical isolates were collected from center of Tehran, Iran and also from different systemic infectious sites of hospitalized children, from July 2012 to January 2013. The isolates were identified with biochemical tests, such as mannitol fermentation on Mannitol Salt Agar (MSA) medium, slide and tube coagulase tests, DNase production, and colony morphology on blood agar medium.
The study was approved by Ethics Committee of the university.
Clindamycin inducible resistance
The Double disk diffusion (D-test) was performed in Muller Hinton Agar medium using clindamycin (2ug) and erythromycin (15ug) according to Clinical and Laboratory Standards Institute (CLSI) guidelines.
Detection of MRSA strains
Phenotypic detection of MRSA strains was conducted with oxacillin (1µg) (15) in the antibiotic susceptibility test. Moreover, PCR assay was performed to detect mecA gene with specific primers (Table 1).
Table 1.
Sequences and sizes of primers used in this study
| Primer | Sequence 5 3 | Product size |
|---|---|---|
| mecA | F:GTG AAG ATA TAC CAA GTG ATT R:ATG CGC TATAGATTGAAA GGA |
147 |
| clfA | F: 5-ATTGGCGTGGCTTCAGTGCT-3 R: 5-CGTTTCTTCCGTAGTTGCATTTG-3 |
288 |
| clfB | F: 5-ACATCAGTAATAGTAGGGGCAAC-3 R: 5-TTCGCACTGTTTGTGTTTGCAC-3 |
204 |
| fnbA | F: 5-CATAAATTGGGAGCAGCATCA-3 R: 5- ATCAGCAGCTGAATTCCCATT-3 |
128 |
| fnbB | F: 5-GTAACAGCTAATGGTCGAATTGATACT-3 R: 5-CAAGTTCGATAGGAGTACTATGTTC-3 |
524 |
| fib | F: 5-CTACAACTACAATTGCGTCAACAG-3 R: 5-GCTCTTGTAAGACCATTTTCTTCAC-3 |
405 |
| cna | F: 5-AAAGCGTTGCCTAGTGGAGA-3 R: 5-AGTGCCTTCCCAAACCTTTT-3 |
192 |
| eno | F: 5-ACGTGCAGCAGCTGACT-3 R: 5-CAACAGCATCTTCAGTACCTTC-3 |
301 |
| ebps | F: 5-CATCCAGAACCAATCGAAGAC-3 R: 5- AGTTACATCATCATGTTTATCTTTTG-3 |
188 |
| bbp | F: 5-AACTACATCTAGTACTCAACAACAG-3 R: 5-ATGTGCTTGAATAACACCATCATCT-3 |
574 |
Extraction of genomic DNA
One colony of each bacterial isolate was suspended in 200 µl of TE buffer, and then the enzyme lysostaphin was added (totally 200µl of TE buffer and 20µl of lysostaphin [2µg/ml, Sigma]). Genomic DNA of each S. aureus isolate was isolated according to Straubinger method (16).
PCR reaction
The purpose of using simplex and multiplex PCR was to determine mecA gene in MRSA and the genes encoding adhesive surface proteins including clfAB, fnbAB, fib, eno, cna, ebps and bb. The specific primers for these genes have been depicted in Table 1.
Reaction mixture for mecA gene: 9.5µl Distilled water (D.W), 1µl primer, 1.5µl MgCl2 (50mM), 3µl 10x buffer, 2µl dNTPs (10mM), 2µl Taq polymerase (500U) and 5µl DNA template.
Reaction mixture for clfAB, fnbAB and fib multiplex: 9.5µl D.W, 1µl primer, 1.5µl MgCl2, 3µl 10x buffer, 2.5µl dNTPs, 2µl Taq polymerase and 5µl DNA template.
Reaction mixtµre for eno, cna, ebps and bbp multiplex: 9.5µl D.W, 1µl each primer, 1.5µl MgCl2, 3µl 10x buffer, 2.5µl dNTPs, 2µl Taq polymerase and 5µl DNA template.
Data Analysis
Pearson Chi- Square was used for data analysis. A P‐value less than 0.05 was considered as significant.
Results
Antibiotic susceptibility test
In the antibiotic susceptibility test, all the isolates were susceptible to vancomycin and linezolid. Five (22.7%) isolates were resistant to oxacillin and mecA gene was detected among them. Two methicillin susceptible S. aureus (MSSA) isolates showed inducible resistance to clindamycin. However, this phenomenon was not observed among MRSA strains.
Detection of genes encoding adhesive surface proteins:
All the isolates (MRSA and MSSA) harbored clfA,B genes. The prevalence of fnbA, fnbB, fib, eno, cna, ebps and bbp was as 63,6%, 50%, 59%, 82%, 63%, 9% and 0, respectively (Fig 1, 2). However, the frequency of these genes among MRSA isolates was 80%, 40%, 80%, 100%, 60%, 0% and 0%, respectively. There was no significant difference between MRSA and MSSA regarding prevalence of MSCRAMMs genes. Among blood isolates, the clfAB, fnbA, fnbB, fib, eno, cna, ebps and bbp were detected in 100% (n= 4), 50% (n= 2), 75% (n= 3), 100% (n= 4), 75% (n= 3), 50% (n= 2), 25% (n= 1) and 0% (n= 0) of the isolates, respectively.
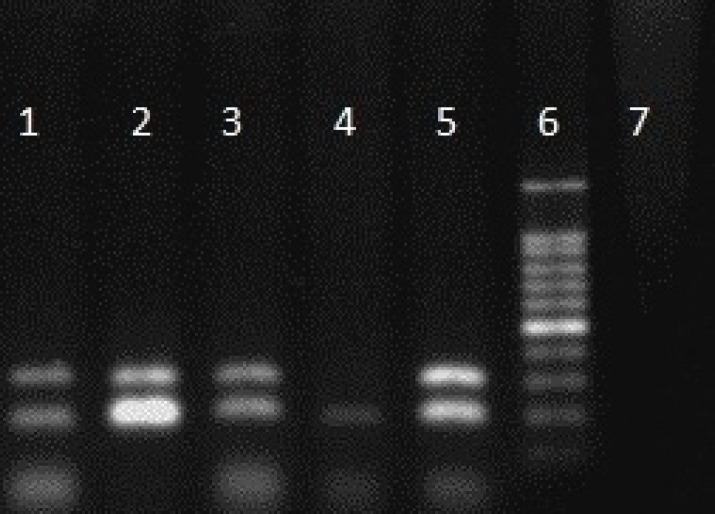
Fig. 1.
Products of multiplex PCR for eno, cna, ebps and bbp genes. Columns 1- 3: eno and cna genes. Column 6: marker
Fig. 2.
Products of multiplex for clfAB, fnbAB and fib genes. Columns 1 and 2: clfAB, fnbAB and fib genes. Column 4: marker
Discussion
In the present study, all the isolates were susceptible to vancomycin and linezolid. The glycopeptide antibiotics have remained the last resorts for treatment of MRSA infections (17). Morbidity and mortality due to MRSA have been frequently reported from many geographical areas (18). A previous study in Iran showed one vancomycin resistant (VRSA) isolate harboring the vanA gene (19). Two of our isolates had inducible clindamycin resistance. In our previous study, similarly this phenomenon was low (4%) (20).
In this study, five isolates were resistant to methicillin. We previously observed that all MRSA isolates exhibited SCCmec type III. MRSA strains, particularly those with SCCmec type III, represent serious human pathogens in Iran (21-23).
On the other hand, we previously determined that the majority of our isolates belonged to the accessory gene regulator (agr) group I (25), and there was no relationship between virulence genes and agr specific groups. The agr of S.aureus is a global regulator of the staphylococcal virulence genes, which include secreted virulence factors and surface proteins.
All the isolates examined in our study harbored clfA,B genes. Clumping factors play a critical role in attachment and colonization of S. aureus. Similar to our study, Klein et al. detected clfB in 91.8% of the isolates (26). There are no previous studies for clfA, B genes prevalence from Iran. Atshan et al. depicted that all strains harbored clfA, B genes (27). Moreover, Momtaz reported that nearly 20% of S. aureus isolates causing mastitis contain clfA gene (28). These studies suggest that S.aureus strains from different clinical sites may contain different frequencies of clumping factors, being essential for colonization. Furthermore, we observed that all the MRSA and MSSA strains, regardless of infection sites, harbored these two genes. In this study, the frequency of fnbA and fnbB was 63.6% and 50%, respectively. We detected fnbA and fnbB genes in four (80%) and two (40%) MRSA isolates. The frequency was not significantly different from MSSA strains. The fnbA and fnbB genes were detected from two (50%) and three (75%) blood isolates. All isolates causing bloodstream infection harbored clfAB and fnbAB genes and produced strong biofilms (29). The fibrinogen binding protein gene (fib) was detected in all the isolates. Similar to our study, Bodén reported that the fib gene was present in all S. aureus strains (30). The prevalence of eno and cna genes was 82% and 63%, respectively, exhibiting the critical role of these genes during colonization of S. aureus. Duran et al. depicted that 78.4% of isolates harbored cna gene (31). In contrast to these, Arciola detected cna gene in 46% of isolates (32). The frequency of the ebps gene was 9%, however none of the isolates harbored bbp gene. These genes have been mostly detected among strains isolated from catheters and in addition from blood infections. In Paniagua and coworkers study, the most prevalent virulence genes were clfA, clfB, cna, bbp, ebps and ica (65.6 %, n = 21) among catheter related S.aureus isolates (33). By the phenotypic test, 26 (36.1%) strains were strong, 30 (41.6%) strains were moderate, and in 16 (22.3%) strains were weak biofilm producers (34). Tang though surveyed different sources, detected the bbp gene amplification only in one strain (35).
In the present study, there was no significant difference between MRSA and MSSA strains regarding biofilm production and frequency of MSCRAMMs genes. The source of infections can play a significant role in determination of pattern and expression of the predominant types of genes necessary for the attachment of S. aureus. To our knowledge, previous studies on the MSCRAMMs genes prevalence are scarce in Iran. Detection of these genes can help know the most prevalent exposing proteins and can culminate in developing new vaccine designs according to Iranian isolates to prevent severe infections.
Conclusion
All the isolates (MRSA and MSSA) harbored clfA,B genes. Moreover, prevalence of fnbA and eno genes was high. The high prevalence of these genes is important for future plans in vaccine designation. MRSA and MSSA isolates similarly can produce adhesive surface proteins for colonization.
Acknowledgments
The authors acknowledge the efforts of Stuff in Loghman Hospital of Tehran and their helps for collection of bacterial isolates . This study was supported by a grant from Tarbiat Modares University, Faculty of Medical Sciences, Tehran, Iran.
Conflict of interest
The authors declare that there is no conflict of interests.
References
- 1.Bien J, Sokolova O, Bozko P. Characterization of Virulence Factors of Staphylococcus aurous: Novel function of known virulence factors that are implicated in activation of airway epithelial proinflammatory response. J Pathogen. 2011:601905. doi: 10.4061/2011/601905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finelli L, Fiore A, Dhara R, Brammer L, Shay DK, Kamimoto L, et al. Influenza-associated pediatric mortality in the United States: increase of Staphylococcus aureus coinfection. Pediatrics. 2008;122(4):805–11. doi: 10.1542/peds.2008-1336. [DOI] [PubMed] [Google Scholar]
- 3.McNeil JC, Hulten KG, Kaplan SL, Mahoney DH, Mason EO. Staphylococcus aureus infections in pediatric oncology patients: high rates of antimicrobial resistance, antiseptic tolerance and complications. Pediatr Infect Dis J. 2013;32(2):124–8. doi: 10.1097/INF.0b013e318271c4e0. [DOI] [PubMed] [Google Scholar]
- 4.Adem PV, Montgomery CP, Husain AN, Koogler TK, Arangelovich V, Humilier M, et al. Staphylococcus aureus sepsis and the waterhouse friderichsen syndrome in children. N Engl J Med. 2005;353:1245–51. doi: 10.1056/NEJMoa044194. [DOI] [PubMed] [Google Scholar]
- 5.Jimenez-Truque N, Tedeschi S, Saye EJ, McKenna BD, Langdon W, Wright JP, et al. Relationship between maternal and neonatal Staphylococcus aureus colonization. Pediatrics. 2012;129(5):e1252–9. doi: 10.1542/peds.2011-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mulcahy ME, Geoghegan JA, Monk IR, O'Keeffe KM, Walsh EJ, Foster TJ, et al. Nasal colonisation by Staphylococcus aureus depends upon clumping factor B binding to the squamous epithelial cell envelope protein loricrin. PLoS Pathog. 2012;8(12):e1003092. doi: 10.1371/journal.ppat.1003092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edwards AM, Massey RC, Clarke SR. Molecular mechanisms of Staphylococcus aureus nasopharyngeal colonization. Mol Oral Microbiol. 2012;27(1):1–10. doi: 10.1111/j.2041-1014.2011.00628.x. [DOI] [PubMed] [Google Scholar]
- 8.Vazquez V, Liang X, Horndahl JK, Ganesh VK, Smeds E, Foster TJ, et al. Fibrinogen is a ligand for the Staphylococcus aureus microbial surface components recognizing adhesive matrix molecules (MSCRAMM) bone sialoprotein-binding protein (Bbp) J Biol Chem. 2011;286(34):29797–805. doi: 10.1074/jbc.M110.214981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heilmann C. Adhesion mechanisms of staphylococci. Adv Exp Med Biol. 2011;715:105–23. doi: 10.1007/978-94-007-0940-9_7. [DOI] [PubMed] [Google Scholar]
- 10.Mirzaee M, Najar Peerayeh Sh, Ghasemian AM. Detection of icaABCD genes and biofilm formation in clinical isolates of methicillin resistant Staphylococcus aureus. Iran J Pathol. 2014;9(4):257–262. [Google Scholar]
- 11.Ganesh VK, Rivera JJ, Smeds E, Ko YP, Bowden MG, Wann ER, et al. A structural model of the Staphylococcus aureus ClfA-fibrinogen interaction opens new avenues for the design of anti-staphylococcal therapeutics. PLoS Pathog. 2008;4(11):e1000226. doi: 10.1371/journal.ppat.1000226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Archer NK, Mazaitis MJ, Costerton JW, Leid JG, Powers ME, Shirtliff ME. Staphylococcus aureus biofilms: properties, regulation, and roles in human disease. Virulence. 2011;2(5):445–59. doi: 10.4161/viru.2.5.17724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foster TJ, Geoghegan JA, Ganesh VK, Höök M. Adhesion, invasion and evasion: the many functions of the surface proteins of Staphylococcus aureus. Nat Rev Microbiol. 2014;12(1):49–62. doi: 10.1038/nrmicro3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang M, Ko YP, Liang X, Ross CL, Liu Q, Murray BE, et al. Collagen-binding microbial surface components recognizing adhesive matrix molecule (MSCRAMM) of Gram-positive bacteria inhibit complement activation via the classical pathway. J Biol Chem. 2013;288(28):20520–31. doi: 10.1074/jbc.M113.454462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karami S, Rahbar M, Vand Yousefi J. Evaluation of five phenotypic methods for detection of methicillin resistant Staphylococcus aureus (MRSA) Iran J Pathol. 2011;6(1):27–31. [PMC free article] [PubMed] [Google Scholar]
- 16.Annerose G, Christiane W, Sven P, Reinhard KS. Identification of pathogens in mastitis milk samples with fluorescence in situ hybridization. J Vet Diagnost Invest. 2013;25(3):386–94. doi: 10.1177/1040638713486113. [DOI] [PubMed] [Google Scholar]
- 17.Saderi H, Owlia P, Maleki Z, Habibi M, Rahmati N. Susceptibility to vancomycin in Staphylococcusaureus isolated from patients of four university-affiliated hospitals in Tehran. Iran J Pathol. 2008;3(3):161–66. [Google Scholar]
- 18.Faghri J, Shahbazzadeh D, Pooshang Bagheri K, Moghim Sh, Ghasemian Safaei H. Two dimensional structural analysis and expression of a new Staphylococcus aureus adhesin based fusion protein. Iran J Basic Med Sci. 2012;15(2):725–38. [PMC free article] [PubMed] [Google Scholar]
- 19.Azimian A, Peerayeh SN, Mirab-SS , Naderi M, Ghazvini K, Samiee SM, et al. Occurrence of methicillin resistant Staphylococcus aureus (MRSA) among clinical samples in Tehran-Iran and its correlation with polymorphism of specific accessory gene regulator (agr) groups. Braz J Microbiol. 2012;43(2):779–85. doi: 10.1590/S1517-83822012000200043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghasemian A, Najar Peerayeh Sh, Bakhshi B, Mirzaee M. Inducible clindamycin resistance in clinical isolates of Staphylococcus aureus. Arch Clin Infect Dis. 2014;9(2):e16218. [Google Scholar]
- 21.Ghasemian A, Najar Peerayeh Sh, Bakhshi B, Mirzaee M. Accessory gene regulator specificity groups among Staphylococcus aureus isolated from hospitalized children. Arch Pediatr Infect Dis. 2014;2(2):e16096. [Google Scholar]
- 22.Ghaznavi-Rad E, Nor Shamsudin M, Sekawi Z, Khoon LY, Aziz MN, Hamat RA, et al. A simplified multiplex PCR assay for fast and easy discrimination of globally distributed staphylococcal cassette chromosome mec types in methicillin resistant Staphylococcus aureus. J Med Microbiol. 2010;59:1135–139. doi: 10.1099/jmm.0.021956-0. [DOI] [PubMed] [Google Scholar]
- 23.Japoni A, Jamalidoust M, Farshad S, Ziyaeyan M, Alborzi A, Japoni S, et al. Characterization of SCCmec types and antibacterial susceptibility patterns of methicillin-resistant Staphylococcus aureus in Southern Iran. Jpn J Infect Dis. 2011;64(1):28–33. [PubMed] [Google Scholar]
- 24.Fatholahzadeh B, Emaneini M, Gilbert G, Udo E, Aligholi M, Modarressi MH, et al. staphylococcal cassette chromosome mec (SCCmec) analysis and antimicrobial susceptibility patterns of methicillin-resistant Staphylococcus aureus (MRSA) isolates in Tehran, Iran. Microb Drug Resist. 2008;14(3):217–20. doi: 10.1089/mdr.2008.0822. [DOI] [PubMed] [Google Scholar]
- 25.Ghasemian A, Najar Peerayeh Sh, Bakhshi B, Mirzaee M. Detection of accessory gene regulator groups genes and cassette chromosome mec types among Staphylococcus aureus isolated from intensive care unit patients. Asian Pac J Trop Dis. 2015;5(2):153–57. [Google Scholar]
- 26.Klein RC, Fabres-Klein MH, Brito MA, Fietto LG, Ribon Ade O. Staphylococcus aureus of bovine origin: genetic diversity, prevalence and the expression of adhesin-encoding genes. Vet Microbiol. 2012;160(1-2):183–88. doi: 10.1016/j.vetmic.2012.05.025. [DOI] [PubMed] [Google Scholar]
- 27.Atshan SS, Nor Shamsudin M, Sekawi Z, Lung LT, Hamat RA, Karunanidhi A, et al. Prevalence of adhesion and regulation of biofilm-related genes in different clones of Staphylococcus aureus. J Biomed Biotechnol. 2012;2012:976972. doi: 10.1155/2012/976972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Momtaz H, Rahimi E, Tajbakhsh E. Detection of some virulence factors in Staphylococcus aureus isolated from clinical and subclinical bovine mastitis in Iran. Afr J Biotechnol. 2010;9(25):3753–58. [Google Scholar]
- 29.Kawamura H, Nishi J, Imuta N, Tokuda K, Miyanohara H, Hashiguchi T, et al. Quantitative analysis of biofilm formation of methicillin-resistant Staphylococcus aureus (MRSA) strains from patients with orthopaedic device-related infections. FEMS Immunol Med Microbiol. 2011;63(1):10–5. doi: 10.1111/j.1574-695X.2011.00821.x. [DOI] [PubMed] [Google Scholar]
- 30.Bodén Wästfelt MK, Flock JI. Incidence of the highly conserved fib gene and expression of the fibrinogen-binding (Fib) protein among clinical isolates of Staphylococcus aureus. J Clin Microbiol. 1995;33(9):2347–52. doi: 10.1128/jcm.33.9.2347-2352.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duran N, Yunus D, Burcin O, Cemil D, Aydiner K. Detection of adhesin genes and slime production among Staphylococci in orthopaedic surgical wounds. Afr J Microbiol Res. 2010;9:708–15. [Google Scholar]
- 32.Arciola CR, Campoccia D, Gamberini S, Baldassarri L, Montanaro L. Prevalence of cna, fnbA and fnbB adhesin genes among Staphylococcus aureus isolates from orthopedic infections associated to different types of implant. FEMS Microbiol Lett. 2005;246:6. doi: 10.1016/j.femsle.2005.03.035. [DOI] [PubMed] [Google Scholar]
- 33.Paniagua-Contreras G, Monroy-Pérez E, Gutiérrez-Lucas R, Sainz-Espuñes T, Bustos-Martínez J, Vaca S. Genotypic characterization of methicillin-resistant Staphylococcus aureus strains isolated from the anterior nares and catheter of ambulatory hemodialysis patients in Mexico. Folia Microbiol (Praha) 2014;59(4):295–302. doi: 10.1007/s12223-013-0300-4. [DOI] [PubMed] [Google Scholar]
- 34.Mirzaee M, Najar-Peerayeh Sh, Behmanesh M, Forouzandeh Moghadam M, Ghasemian A. Biofilm formation and presence of ica genes in Staphylococcus aureus isolated from intensive care unit. J Mazandaran Univ Med Sci. 2014;24(115):43–51. (Persian) [Google Scholar]
- 35.Tang J, Chen J, Li H, Zeng P, Li J. Characterization of adhesin genes, staphylococcal nuclease, hemolysis, and biofilm formation among Staphylococcus aureus strains isolated from different sources. Foodborne Pathog Dis. 2013;10(9):757–63. doi: 10.1089/fpd.2012.1474. [DOI] [PubMed] [Google Scholar]