Abstract
Background & Objectives:
Tubular adenomas are rare benign epithelial tumours of breast affecting predominantly females of child bearing age group. Till now, very small number of cases have been reported in the literature. Present study was carried out to evaluate the clinico-pathological features of tubular adenoma cases diagnosed during three years study period along with discussion of possible differential diagnoses.
Methods:
Overall, 346 female breast biopsies were diagnosed as benign lesions in three years (2010-2012), of which 10 cases of tubular adenomas were identified. Available clinical, radiological and cytological data of these cases were analysed retrospectively in detail.
Result:
Tubular adenomas were identified from 16 to 48 years of age with a predilection to younger age group (60% within 30 years). Most of the tubular adenomas were small and circumscribed mimicking fibroadenoma in almost all the cases. Diagnosis of tubular adenoma in each case was possible only after histological examination. Pre-operative diagnosis of tubular adenoma was not established by cytological and radiological evaluation in any case.
Conclusion:
Tubular adenomas are clinically indistinguishable from other benign breast neoplasms and it should be considered as potential differential diagnosis during histopathological evaluation of breast biopsies.
Key Words: Tubular adenoma, Breast, Pathology
Introduction
Tubular adenomas are rare benign neoplasms accounting for 0.13-1.7% benign breast lesions (1, 2). Distinctive clinico-pathological features of this rare tumour were initially described by Persaud et al. (1968) (3). Moross et al. (1983) published the first cytological and electron microscopical description of the lesions (4). Till now only few research articles have been published on this rare neoplasm and most of these were case reports (1, 5, 6).
Tubular adenomas are circumscribed, unencapsulated, slow growing, firm, mobile and small to medium sized lesions of female breast consisting of densely packed regular round tubules. Young women of reproductive age group (15-49 years) are commonly affected. Upper and outer quadrant of breast is the most preferred site. No association with pregnancy or oral contraceptive use has been reported which is sharply in contrast with lactating adenoma. Actually lactating and tubular adenoma are considered as similar lesions under different physiological conditions. Recurrence or increased risk of cancer is not reported from cases of tubular adenoma (7 -9).
Clinically this rare neoplasm closely resembles another much more frequent benign breast neoplasm namely fibroadenoma. Even preoperative cytological evaluation often fails to distinguish the lesions and histopathology remains gold standard for final confirmation (1, 5, 6). In the present study we discuss available clinico-pathological and radiological findings of 10 histopathologically confirmed tubular adenoma cases, encountered during study period of three years. During our research period, we had the opportunity to study relatively good numbers of this rare category tumour and our aim was to evaluate available clinico-cyto-radio-histopathological features of tubular adenoma cases expecting to find out some avenue or providing any clue to the future workers that may help in early diagnosis.
Material and Methods
The present study was conducted in the Department of Pathology, Bankura Sammilani Medical College, Bankura, West Bengal for a period of three years (1st January 2010 to 31th December 2012). It was a retrospective study and written consent was obtained routinely from each of the participating females, informing them about the nature and possible complications of the tests (FNAC, ultrasound, mammography and biopsy) done. During histopathological evaluation, 10 cases of tubular adenoma of breast were diagnosed and included in our study group. Detailed clinical data about age of the patient, duration, site, size, consistency and mobility of the breast lump, tenderness, skin and nipple changes, axillary lymph node status were recorded. All available radiological investigation (ultrasound and mammography) findings of these cases were collected and analysed.
Results
During our study period of three years, total 346 breast biopsies were interpreted as benign breast disease. Out of these 346 cases, ten cases (2.9%) were diagnosed as tubular adenoma. Table 1 shows that six out of ten cases in the study group (60%); belonged to second or third decade of life. The youngest and oldest cases were being 16 years and 48 years, respectively. Duration of the swellings was less than one year in majority of the cases (60%) with one case having less than six months (three months) history. Only one lesion was more than 5 cm (7.8 cm) in diameter while majority (50%) were less than 2.5 cm in diameter. Clinically only one case appeared to be suspicious of malignancy, the rest nine cases were interpreted as benign lesions.
Table 1.
Clinical presentation of tubular adenoma cases
| Total no of cases | Age (yr) | Duration (Months) | Size (cm) | Clinical presentation | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-10 | 11-20 | 21-30 | 31-40 | 41-50 | >51 | <2 | 2-6 | 7-12 | >12 | <2.5 | 2.5-5 | >5 | Benign | Suspicious | Malignant | |
| 10 | 0 | 4 | 2 | 3 | 1 | 0 | 0 | 1 | 5 | 4 | 5 | 4 | 1 | 9 | 1 | 0 |
Pre-operative radiological evaluation was possible in 8 cases (ultrasonography in all 8 cases and mammography in one case) and all the lesions were interpreted as benign. Fine needle aspiration cytology (FNAC) was done over 7 cases with uniform diagnosis of fibroadenoma in all cases (Table 2). Table 3 demonstrates the clinical, radiological and cytological features of individual cases. All ten cases underwent either radiological or cytological or combined pre-operative evaluation with uniform diagnosis of benign breast lesions suggesting fibroadenoma, before histopathological evaluation.
Table 2.
Radiological and cyto-histological presentation of tubular adenoma cases
| Total no of female breast biopsies | Total no of tubular adenoma cases | Percentage of tubular adenoma | Radiological evaluation |
Cytological evaluation |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Total no of cases | Report |
Total no of cases | Report |
||||||
| Benign | suspicious | Malignant | Fibroadenoma | Other diagnosis | |||||
| 346 | 10 | 2.89% | 8 | 8 | 0 | 0 | 7 | 7 | 0 |
Table 3.
Clinical, radiological and cytological features of individual cases of tubular adenoma of breast
| Serial no | Age (yr) | Site | Size (cm) | Duration (month) | Consistency | Tenderness | Mobility | Skin changes | Axillary lymph node | Clinical diagnosis | Radiological diagnosis | Cytological diagnosis | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| USG | Mammography | ||||||||||||
| 1 | 19 | UO (Lt) | 3.8 | 9 | Firm | Absent | Mobile | Absent | Absent | Benign | Benign | - | Fibroadenoma |
| 2 | 36 | UO (Rt) | 2.9 | 18 | Firm | Absent | Mobile | Absent | Absent | Benign | Benign | - | Fibroadenoma |
| 3 | 17 | LI (Rt) | 1.5 | 11 | Soft to firm | Absent | Mobile | Absent | Absent | Benign | - | - | Fibroadenoma |
| 4 | 48 | C (Lt) | 7 | 3 | Firm to hard | Mild | Slightly restricted | Absent | Absent | Suspicious of malignancy | Benign | Benign | Fibroadenoma |
| 5 | 33 | LO (Rt) | 2 | 9 | Firm | Absent | Mobile | Absent | Absent | Benign | Benign | - | - |
| 6 | 20 | UI (Lt) | 4.6 | 24 | Firm | Mild | Mobile | Absent | Absent | Benign | Benign | - | Fibroadenoma |
| 7 | 26 | LO (Rt) | 2.2 | 7 | Soft to firm | Absent | Mobile | Absent | Absent | Benign | Benign | - | - |
| 8 | 16 | UO (Lt) | 1.7 | 15 | Firm | Absent | Mobile | Absent | Absent | Benign | - | - | Fibroadenoma |
| 9 | 32 | LI (Lt) | 3.2 | 10 | Firm | Absent | Mobile | Absent | Absent | Benign | Benign | - | Fibroadenoma |
| 10 | 22 | LO (Lt) | 2.4 | 30 | Firm | Absent | Mobile | Absent | Absent | Benign | Benign | - | - |
Discussion
Different workers reported that 90% patients of tubular adenoma were younger than 40 years, similar to our experience (1, 10). Size of the tumours varies from 1 cm to 7.5 cm and duration before diagnosis 2 to over 12 months, consistent with our findings (1, 11, 12). Clinically, the majority are painless, freely mobile, circumscribed lesions resembling fibroadenoma or other benign breast lesions (1, 11, 13). We suspected malignancy in one out of the ten cases in our series due to older age of the patient (48 yr), large size of the lesion (7 cm in diameter) and comparatively shorter duration (3 months) though fixity to the surrounding structures and skin changes typical of malignant lesions were absent. Similar confusion was also reported previously (6).
In the present study, incidence of tubular adenoma among female benign breast lesions was much higher (2.89%), in comparison to maximum incidence of 1.7%, as reported by various workers (1, 7-9). We could not suggest any possible explanation for this higher incidence.
Pre-operative ultrasonographic evaluation was done in eight out of ten cases in the present study with finding of hypoechoic, circumscribed mass lesion in each case confirming possible benign nature of the lesions. Mammography was done in the only clinically suspicious case of our series and revealed well defined mass lesion without any calcification suggesting benignity. Similar experiences were also reported previously (1, 5, 6). Soo et al. reported calcifications found in the mammogram of three out of sixteen cases undergoing evaluation. All these three cases showed clustered microcalcifications without any linear, branching or cast like calcification typical of high grade ductal carcinoma in situ. Sonogram done over all the sixteen cases also revealed benign nature of sound transmission without any pattern (5). Few researchers proposed that pattern of dense punctuate or irregular micro-calcification without cast like or branching forms that are tightly grouped within a mass, if present, may suggest a diagnosis of tubular adenoma. But these features are usually encountered in post-menopausal cases and may cause confusion with malignancy (5, 10). However majority of the lesions in young patients simulate fibroadenomas without any diagnostic calcification, as seen in mammography (5, 10). Therefore still tubular adenomas cannot be differentiated from other benign breast lesions on radiological assessment alone (5, 14).
Fine needle aspiration cytology was approached in seven out of ten cases in our series. Smears were moderately cellular comprising of tight clumps of uniform bland appearing duct epithelial cells, myoepithelial cells, plenty of bare nuclei and variable stromal fragments. All the cases were interpreted as fibroadenoma of breast. Different workers also reported similar findings (1, 7-9,12). Shet et al. described the characteristic cytological feature of tubular adenoma as small three dimensional cell balls or clusters and tubular structures with or without acini (12). But excess tubular fragments should arouse the possibility of tubular adenosis or tubular carcinoma. Associated features like degeneration, necrosis or mucin secretion further create confusion with malignancy (12, 15, 16). Kumar et al. reported that only one out of six histologically documented tubular adenoma cases, cytology could be successfully employed for preoperative confirmation of diagnosis (17).
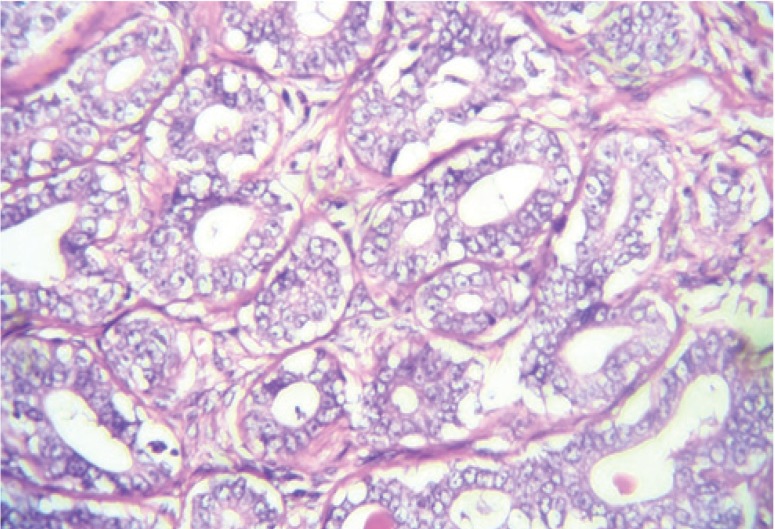
Histopathology of all the ten cases demonstrated sharply demarcated unencapsulated lesions, densely packed uniform round tubules, double layering of tubules, no cytological atypia of tubular lining cells, scanty stroma without any evidence of tubular compression (Fig.1, 2). Features were enough for diagnosis of tubular adenoma in each case. Different workers also reported that diagnosis of tubular adenoma on histopathology was easily accomplished (1, 7-9). Histopathological differential diagnoses of tubular adenoma include other benign breast lesions like lactating adenoma, fibroadenoma, microglandular adenosis, sclerosing adenosis, ductal adenoma, nipple adenoma and tubular adenosis (6-8). Lactating adenomas as already mentioned, are similar neoplasms under different physiologic conditions and can be differentiated by presence of prominent cytoplasmic vacuoles in the lining epithelium of tubules with abundant secretions in the lumens (lactational changes). Fibroadenoma with prominent adenomatous transformation may closely resemble tubular adenoma and can only be differentiated by presence of abundant stroma with typical inter and intralobular distinction at least at focal parts of the former lesion with variable rather than uniform size of the tubules (1, 10).
Fig.1.
Photomicrograph of histopathology of tubular adenoma of breast showing proliferation of closely packed tubules with scanty intervening stroma (H & E stain, ×100 view)
Fig. 2.
Photomicrograph of histopathology of tubular adenoma of breast showing double layered columnar epithelium without any atypia (H & E stain, ×400 view)
Microglandular adenosis is characterized by poor circumscription, absence of myoepithelial cell layer and irregular distribution of tubules with abundant stroma. Cellular stroma, compressed ducts and lack of sharp demarcation help to identify sclerosing adenosis. Duct adenomas exhibit encapsulation, lack of complete circumscription and presence of prominent stromal elements often with sclerosis. Nipple adenomas show overlapping features of duct adenomas without fibrous encapsulation and prominent papillomatosis with various sized small glands. Tubular adenoma and adenosis can be differentiated by diffuse, infiltrating growth pattern, irregular distribution of tubules and abundant stroma as seen in the later variant (1, 6-8). Only malignant lesion that closely mimics this benign neoplasm is tubular carcinoma which is differentiated by stellate infiltrative growth pattern rather than circumscription and lack of double layering of tubules (6-9). As a whole trademark histopathological features of tubular adenoma include complete circumscription, scanty stroma and uniform densely packed tubules.
Conclusion
Tubular adenoma is a rare benign breast neoplasm that can only be confirmed after histopathological examination. Attempts have been made for pre-operative identification of the neoplasm by radiology as well as cytology. But like other previous workers, we failed to achieve success regarding early identification of the tumour. We hope our study will encourage future research workers in this field that may help to reach the goal in near future.
Acknowledgment
Prof. (Dr) Swapan is highly appreciated. The authors declare that there is no conflict of interests.
References
- 1.Nikolaos SS, Georgios G, Gregorios K, Charalambos S, Konstantinos S, Vlasios T, Dimitrios S, Emmanuel L. Tubular Adenoma of the Breast: A Rare Presentation and Review of the Literature. J Clin Med Res. 2012;4(1):64–7. doi: 10.4021/jocmr746w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tavassoli FA, Devilee P, editors. Tumours of the breast Pathology and genetics of tumours of the breast and female genital organs, World Health Organization Classification of Tumours. Lyon, France: IARC; 2003. [Google Scholar]
- 3.Persaud V, Talerman A, Jordan R. Pure adenoma of the breast. Arch Pathol. 1968;86(5):481–3. [PubMed] [Google Scholar]
- 4.Moross T, Lang AP, Mahoney L. Tubular adenoma of breast. Arch Pathol Lab Med. 1983;107(2):84–6. [PubMed] [Google Scholar]
- 5.Soo MS, Dash N, Bentley R, Lee LH, Nathan G. Tubular adenoma of the breast: imaging findings with histologic correlation. Am J Radiology. 2000;174(3):757–61. doi: 10.2214/ajr.174.3.1740757. [DOI] [PubMed] [Google Scholar]
- 6.Fikret D, Manuk NM, Ahmet M, Deveci U, Yener N. Giant tubular adenoma of the breast: a rare entity. The Breast Journal. 2012;18(1):79–80. doi: 10.1111/j.1524-4741.2011.01186.x. [DOI] [PubMed] [Google Scholar]
- 7.Maiorano E, Albrizio M. Tubular adenoma of the breast: an immunohistochemical study of ten cases. Pathol Res Pract. 1995;191(12):1222–30. doi: 10.1016/S0344-0338(11)81130-1. [DOI] [PubMed] [Google Scholar]
- 8.O’Hara MF, Page DL. Adenomas of the breast and ectopic breast under lactational influences. Hum Pathol. 1985;16(7):707–12. doi: 10.1016/s0046-8177(85)80156-8. [DOI] [PubMed] [Google Scholar]
- 9.Hertel BF, Zaloudek C, Kempson RL. Breast adenomas. Cancer. 1976;37(6):2891–905. doi: 10.1002/1097-0142(197606)37:6<2891::aid-cncr2820370647>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 10.Irshad A, Ackerman SJ, Pope TL, Moses CK, Rumboldt T, Panzegrau B. Rare breast lesions: correlation of imaging and histologic features with WHO classification. Radiographics. 2008;28(5):1399–414. doi: 10.1148/rg.285075743. [DOI] [PubMed] [Google Scholar]
- 11.Tavassoli FA. Benign lesions Pathology of the Breast. 2nd ed. Stamford: Conn: Appleton& Lange; 1999. [Google Scholar]
- 12.Shet TM, Rege JD. Aspiration cytology of tubular adenomas of the breast. An analysis of eight cases. Acta Cytol. 1998;42(3):657–62. doi: 10.1159/000331822. [DOI] [PubMed] [Google Scholar]
- 13.Rosen PP. Fibroepithelial neoplasms. Rosen’s Breast Pathology. 3rd ed. New York: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 14.American College of Radiology. Breast imaging reporting and data system. 3rd ed. Reston, VA: American College of Radiology; 1998. [Google Scholar]
- 15.Mulvany N, Lowhagen T, Skoog L. Fine needle aspiration cytology of tubular adenoma of the breast A report of two cases. Acta Cytol. 1994;38(6):961–4. [PubMed] [Google Scholar]
- 16.Hanaki N, Ishikawa M, Nishioka M, Kikutsuji T, Kashiwagi Y, Miki H. A case of tubular adenoma of the breast simulating breast carcinoma. Nihon Rinsho Geka Gakkai Zasshi. 2000;61(4):894–897. [Article in Japanese, with English abstract] [Google Scholar]
- 17.Kumar N, Kapila K, Verma K. Characterization of tubular adenoma of breast--diagnostic problem in fine needle aspirates (FNAs) Cytopathology. 1998;9(5):301–7. doi: 10.1046/j.1365-2303.1998.00120.x. [DOI] [PubMed] [Google Scholar]