Abstract
Objectives. We examined the impact of transitioning clients from a mental health clinic to a patient-centered medical home (PCMH) on mental health recovery.
Methods. We drew data from a large US County Behavioral Health Services administrative data set. We used propensity score analysis and multilevel modeling to assess the impact of the PCMH on mental health recovery by comparing PCMH participants (n = 215) to clients receiving service as usual (SAU; n = 22 394) from 2011 to 2013 in San Diego County, California. We repeatedly assessed mental health recovery over time (days since baseline assessment range = 0–1639; mean = 186) with the Illness Management and Recovery (IMR) scale and Recovery Markers Questionnaire.
Results. For total IMR (log-likelihood ratio χ2[1] = 4696.97; P < .001) and IMR Factor 2 Management scores (log-likelihood ratio χ2[1] = 7.9; P = .005), increases in mental health recovery over time were greater for PCMH than SAU participants. Increases on all other measures over time were similar for PCMH and SAU participants.
Conclusions. Greater increases in mental health recovery over time can be expected when patients with severe mental illness are provided treatment through the PCMH. Evaluative efforts should be taken to inform more widespread adoption of the PCMH.
In 2001, the Institute of Medicine (IOM) called for a commitment to improve the organization and delivery of health care in the United States.1 The IOM report notes that, because of advances in medical science and technology, Americans are living longer and an increase in the incidence and prevalence of chronic conditions has emerged. Despite these changes in the public’s health care needs, much of today’s health care system focuses primarily on acute needs. In addition, a growing consensus exists among providers, payers, and policymakers that the current primary care system rewards quantity of services delivered at the expense of higher-quality care.2 As a result, the United States has fallen behind other countries in areas such as amenable mortality, identified as being the worst of 16 industrial nations,3 and ranks poorly on access and safety.4
Following the IOM report, the patient-centered medical home (PCMH) has been discussed extensively as a delivery system innovation for facilitating health care delivery improvements.2,4–7 Although the American Academy of Pediatrics introduced the medical home concept in 1967, the concept was expanded in a 2002 policy statement to address some of the guidelines proposed in the 2001 IOM report, and in 2007 the principles of the PCMH were jointly approved.8 Among others, these PCMH principles include an emphasis on ongoing patient relationships with a personal physician, provision of comprehensive care by addressing all of the patient’s health care needs, and improving access to care and communication between patients and providers. There are now efforts to broadly expand the PCMH approach in the United States and Canada.9,10
With the increased interest in the PCMH model and its potential to improve the quality of health care in the United States, attention has turned to the characteristics of PCMH demonstration projects and the incorporation of mental health care. A nationwide survey of PCMH demonstration projects including more than 14 000 physicians caring for approximately 5 million patients identified key elements regarding their structure, payment models, and transformation processes.2 The results from these demonstration projects suggested 2 models for helping transform practices. The first was an implementation of a chronic care model by quality improvement coaching and collaborative learning. The second was a model featuring external transformation consultants.
Because the problems afflicting patients in the primary care setting are typically chronic, the implementation of a chronic care model has several advantages.11 However, the PCMH is not simply a tool for disease management, but it is
coordination and integration of the different care strategies for a person’s unique combination of chronic and acute diseases, health beliefs, resources, prevention needs, and complicating factors.7(p300)
The PCMH is intended to take a whole-person orientation that includes patients’ behavioral and mental health.12,13 Without the incorporation of the full psychosocial dimension of health and health care, the PCMH will be incomplete and less effective.7 Research has supported the hypothesis that the addition of mental health care to primary care systems can improve access to and quality of health care.14–18
In March 2011, a PCMH was created in San Diego County, California, with the intention of enhancing the overall mental and physical health for individuals with severe mental illness through a holistic and collaborative continuum of care across primary care and mental health.19 Evidence regarding the effectiveness of the PCMH on improving patient health outcomes, including mental health outcomes, is sparse in the peer-reviewed literature, and researchers are calling for more concerted efforts to address mental health outcomes in the PCMH.12,13,20 The purpose of this study was to use a methodologically rigorous approach employing advanced statistical techniques to assess the impact of the PCMH on participants’ mental health outcomes.
METHODS
The Community Research Foundation mental health and the Family Health Centers of San Diego primary care clinics were contracted to provide PCMH services.21 The Community Research Foundation is a private nonprofit community-based organization that provides mental health services to clients within San Diego County. The Family Health Centers of San Diego is a private nonprofit community clinic organization.22 The PCMH participants were selected from one Community Research Foundation mental health clinic and referred to the Family Health Centers of San Diego primary care clinic.20
To facilitate coordination between primary care and mental health, the PCMH contract had the following requirements: (1) the establishment of joint administrative and clinical functions and educational meetings, and an arrangement for information sharing between referring mental health and primary care clinics; (2) at least 1 behavioral health consultant and registered nurse care manager working in the PCMH; (3) a certified alcohol and drug counselor working in the PCMH to assist with the integrated treatment of individuals with co-occurring disorders; and (4) demonstration by providers of an increase in knowledge of behavioral and primary health care issues and health literacy with the intention of better facilitating comprehensive care.19 Mental health and primary care clinics were located within similar regions of San Diego County limiting great differences in travel time for participants transferred into the PCMH.
The remaining community mental health clinics within the San Diego County Mental Health (now Behavioral Health) Services are labeled services as usual (SAU). In the early 2000s, San Diego County Mental Health Services began their transformation to a recovery-oriented model of services delivery such that treatment is individualized and person-centered, strengths-based, and holistic, and emphasizes client empowerment, respect, and hope.23 Previous research has demonstrated an increase in the recovery orientation of San Diego County Mental Health Services, as well as improvements in clients’ mental health recovery while being treated in these mental health treatment programs.24–30
Study Participants
Patient-centered medical home participants.
The PCMH participants in this study included those who were transferred into the PCMH between the implementation in March 2011 and December 2013. Participants were eligible for transfer into the PCMH for meeting the following criteria: aged 18 years or older, indigent or eligible for Medi-Cal (California’s Medicaid program)–funded services, deemed as “stable” based upon eligibility criteria,21 and having a Milestones of Recovery Scale31 score of 6 or greater. Once participants were deemed eligible, staff members from this mental health clinic selected participants for transfer into the PCMH on the basis of their clinical judgment.
Service-as-usual participants.
We drew a comparison sample from other San Diego County mental health clinics wherein clients continue to receive mental health services. We identified participants in this SAU comparison group from the electronic medical record. As described in more detail in the “Statistical Analyses” section, we used propensity score analysis to assemble an SAU comparison group that is similar to the PCMH participants with the exception being they do not receive treatment under the PCMH model.
Measures
We gathered similar data for PCMH and SAU participants. As part of the PCMH and SAU programs’ administrative duties, all PCMH and SAU participants and their providers were asked to complete an assessment of mental health recovery during their initial treatment appointment (baseline), and every 6-month follow-up appointment. We acquired demographic information (age, gender, ethnicity, race, diagnoses, living status, education, employment status, insurance status) through the electronic medical record. We determined and reported participant diagnoses on the basis of the clinical judgment of their providers.
Illness Management and Recovery scale.
The Dartmouth Psychiatric Research Center developed the Illness Management and Recovery (IMR) client and clinician scales to assess progress over time in mental illness self-management treatment programs.32 The 15-item scales, generated by IMR practitioners and consumers with severe mental illness, demonstrate good convergent validity and internal consistency.33,34 Analyses assessing the psychometric properties of the IMR clinician scale within a sample of clients from San Diego County Adult Mental Health Services (n = 10 659) demonstrate high internal consistency (α = 0.82), and the scale comprised 3 interrelated factors: recovery, management, and substance.35 We used the IMR clinician scale in this study to assess the clinicians’ perspective of their clients’ mental health recovery. The total IMR score is simply a mean of all assessment items and reflects overall mental health recovery as perceived by the provider. The IMR Factor 1 Recovery scores represent progress toward personal goals, mental illness knowledge, involvement in self-help activities, and involvement of family or friends in treatment. The IMR Factor 2 Management scores represent symptom distress or relapse, impairment of functioning, and psychiatric hospitalization. The IMR Factor 3 Substance scores represent impairment of functioning through alcohol or drug use.
Recovery Markers Questionnaire.
The Recovery Markers Questionnaire (RMQ)36 is a measure of self-reported recovery and consists of 24 items, measured on 5-point Likert-type response options that range from 1 “strongly agree” to 5 “strongly disagree.” Analyses assessing the psychometric properties of the RMQ within this same sample of clients from San Diego County Adult Mental Health Services demonstrate very high internal consistency (α = 0.95) and good construct validity.35 The RMQ is a single-factor scale with total scores that represent overall mental health recovery from the perspective of the patient.
Statistical Analyses
Propensity score analysis.
In this study, we used propensity score analysis,37 a rigorous method for assessing causality in the absence of random assignment,38 conducted with Stata statistical software version 11 (StataCorp LP, College Station, TX). Rosenbaum and Rubin’s iterative approach to specifying a propensity score model specified that the probability of having been transferred into the PCMH condition was predicted by using baseline demographic and mental health recovery characteristics.39 Next, we assessed the comparability of PCMH and SAU patients, and we repeated model specification until the distribution of observed baseline covariates was similar between PCMH and SAU patients in each of several strata. For a more detailed description of the 4 methods of propensity score analysis, and its advantages and disadvantages, readers are referred to Rosenbaum and Rubin,39 Austin,40 Luellen et al.,41 and West et al.42
Multilevel modeling.
Multilevel modeling should be used in designs wherein observations are nested within a higher-level unit.43,44 In the present study, we used multilevel modeling to explore differences in growth trends in mental health recovery scores from baseline assessment over time between PCMH and SAU participants. More specifically, the target model includes 2 levels such that repeated mental health recovery assessments (level 1) are nested within individual patients (level 2). We entered propensity scores as a fixed, time-invariant covariate. We entered a variable indicating days since baseline assessment at the repeated assessment level, and entered the cross-level interaction between days since baseline assessment and treatment group condition at the patient level.
We assessed model fit of the target model by using a series of statistics. We assessed z tests and corresponding P values to determine statistical significance of the fixed effect of the explanatory variables when we included them in each of the models. We calculated log-likelihood ratio (LR) test statistics, χ2 difference (∆χ2) test statistics, and comparative fit indices to assess differences in overall model fit in comparison with variance components model. We compared obtained LR and ∆χ2 statistics with critical test values at α = 0.05 to assess statistically significant improvements in model fit. Obtained comparative fit indices values greater than 0.90 were indicative of descriptive improvements in model fit.45 We used the LR test statistics along with change in Akaike information criterion (AIC) to assess statistical and descriptive differences in overall model fit. Lower AIC values were indicative of better fit.46
RESULTS
Between the implementation of the PCMH in March 2011 and December 2013, the care of 215 individuals was transferred from the county mental health clinic to the PCMH. Of these participants, 200 were identified in the electronic medical record, which allowed the abstraction of demographic information. Baseline mental health recovery information was available for 214 PCMH participants. We assessed univariate χ2 and independent samples t tests to explore differences in baseline demographic and mental health recovery characteristics between PCMH and the full population of SAU patients with mental health recovery data (Table 1).
TABLE 1—
Demographic and Mental Health Recovery Differences Between Services as Usual and Patient-Centered Medical Home Participants at Baseline: San Diego County, CA, 2011–2013
| Characteristic | Services as Usual, No. (%) or Mean ±SD | Patient-Centered Medical Home, No. (%) or Mean ±SD |
| Gender | ||
| Female | 10 947 (51.0) | 94 (47.0) |
| Male | 10 516 (49.0) | 106 (53.0) |
| Race/ethnicity*** | ||
| White | 10 554 (51.1) | 96 (48) |
| African American | 2 562 (12.4) | 32 (16) |
| Asian/Pacific Islander | 1 516 (7.3) | 1 (0.5) |
| Hispanic | 4 649 (22.5) | 69 (34.5) |
| Native American | 187 (0.9) | 0 (0.0) |
| Other | 1 200 (5.8) | 2 (1.0) |
| Diagnosis | ||
| Schizophrenia and schizoaffective disorder | 7 139 (34.3) | 67 (33.5) |
| Bipolar disorders | 4 233 (20.3) | 53 (26.5) |
| Major depressive disorders | 6 614 (31.7) | 69 (34.5) |
| Other psychotic disorders | 623 (3.0) | 3 (1.5) |
| Other depression | 811 (3.9) | 3 (1.5) |
| Anxiety disorders | 1 097 (5.3) | 5 (2.5) |
| Dysthymia | 7 (0.0) | 0 (0.0) |
| Adjustment disorders | 92 (0.4) | 0 (0.0) |
| Alcohol use disorder | 28 (0.1) | 0 (0.0) |
| Substance use disorder | 37 (0.2) | 0 (0.0) |
| Cognitive disorders | 16 (0.1) | 0 (0.0) |
| Other | 137 (0.7) | 0 (0.0) |
| Living arrangement | ||
| Lives independently | 15 857 (75.5) | 165 (82.5) |
| Board and care | 1 920 (9.1) | 10 (5) |
| Homeless | 1 881 (9.0) | 17 (8.5) |
| Institutional | 284 (1.4) | 0 (0.0) |
| Justice-related | 125 (0.6) | 0 (0.0) |
| Other | 659 (3.1) | 8 (4.0) |
| Unknown | 268 (1.3) | 0 (0.0) |
| Employment*** | ||
| Unemployed | 17 332 (88.6) | 155 (79.1) |
| Employed for compensation | 1 762 (9.0) | 35 (17.9) |
| Employed not for compensation or volunteer | 462 (2.4) | 6 (3.1) |
| Insurance | ||
| Uninsured | 11 171 (49.9) | 94 (47.0) |
| Medi-Cal or Medicare only | 10 436 (46.6) | 96 (48.0) |
| Private | 787 (3.5) | 10 (5.0) |
| Education, y* | 12.08 ±2.85 | 12.48 ±2.64 |
| IMR total*** | 3.04 ±0.66 | 3.60 ±0.51 |
| Factor 1: Recovery*** | 2.74 ±0.85 | 3.34 ±0.73 |
| Factor 2: Management*** | 2.46 ±0.96 | 3.38 ±0.77 |
| Factor 3: Substance** | 4.63 ±0.93 | 4.77 ±0.77 |
| RMQ total** | 3.57 ±0.74 | 3.74 ±0.59 |
Note. IMR = Illness Management and Recovery scale; RMQ = Recovery Markers Questionnaire.
*P < .05; **P < .01; ***P < .001.
Propensity Scores
The final propensity score model regressed the probability of having been transferred into the PCMH treatment condition on race/ethnicity, living situation, insurance status, education, total IMR scores at baseline, IMR Factor 1 Recovery scores at baseline, IMR Factor 2 Management scores at baseline, and IMR Factor 3 Substance score at baseline.
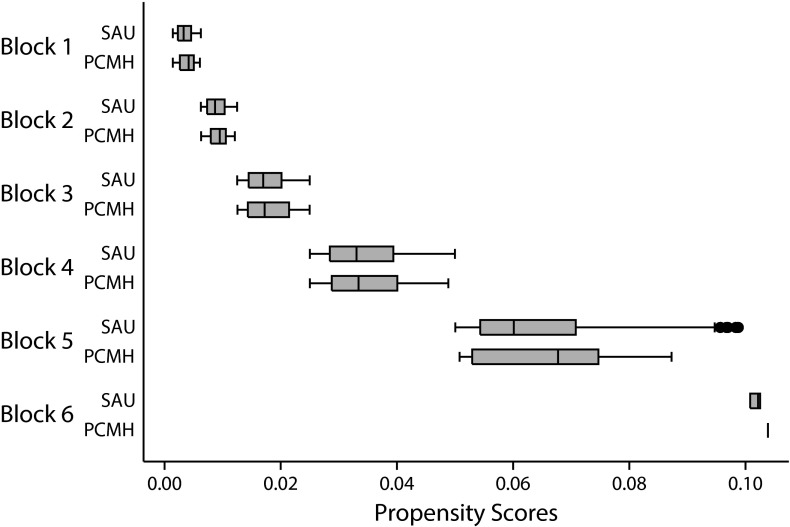
By using the common support option such that individuals with resulting propensity scores that are not shared between PCMH and SAU conditions are excluded, we created 6 strata such that the mean propensity score within each stratum was similar between PCMH and SAU participants. Figure 1 shows information regarding the resulting propensity scores for PCMH and SAU participants.
FIGURE 1—
Propensity scores for services as usual and patient-centered medical home participants by strata: San Diego County, CA, 2011–2013.
Note. PCMH = patient-centered medical home; SAU = services as usual. Whiskers indicate upper and lower 25% of participant propensity scores.
Multilevel Modeling
We progressively assessed 4 separate models to explore differences in growth trends in mental health recovery scores over time between PCMH and SAU participants with the previously mentioned propensity scores entered as a fixed, time-invariant covariate. Table 2 shows results from multilevel modeling. We present results from the fourth model, the full multivariate model. Assessment of model fit for this full multivariate model as it compares to the preceding models addresses whether growth trends in mental health recovery scores over time differed between PCMH and SAU participants.
TABLE 2—
Statistic and Descriptive Fit Indices From Multilevel Modeling to Explore Differences in Growth Trends in Mental Health Recovery Scores Over Time Between Patient-Centered Medical Home and Services as Usual Participants: San Diego County, CA, 2011–2013
| Mental Health Assessment Tool and Model Number | LR Test (χ2) vs Single-Level Model | LR Test (χ2) Comparison With Preceding Model | χ2 Difference (∆χ2) Test Comparison With Model 1 | CFI Comparison With Model 1 | AIC |
| Clinician-reported mental health recovery | |||||
| Total IMR | |||||
| Model 1 | 1 014.45*** | ||||
| Model 2 | 1 033.04*** | 514.002*** | 7327.14*** | 0.0694 | 10 668.77 |
| Model 3 | 2 589.69*** | 1 556.656*** | 11 491.73 | ||
| Model 4 | 7 286.66*** | 4 696.970*** | 13 019.77 | ||
| IMR factor 1: recovery | |||||
| Model 1 | 2 381.49*** | ||||
| Model 2 | 2 242.04*** | 760.912*** | 5247.56*** | 0.1336 | 7 425.19 |
| Model 3 | 2 262.65*** | 20.612*** | 7 440.01 | ||
| Model 4 | 2 265.87*** | 3.220 | 7 425.97 | ||
| IMR factor 2: management | |||||
| Model 1 | 1 615.46*** | ||||
| Model 2 | 1 562.06*** | 730.202*** | 13 254.00*** | 0.1027 | 18 956.51 |
| Model 3 | 1 676.75*** | 116.138*** | 19 039.31 | ||
| Model 4 | 1 686.10*** | 7.900** | 19 029.36 | ||
| IMR factor 3: substance | |||||
| Model 1 | 3 007.28*** | ||||
| Model 2 | 3 008.63*** | −31.728 | 208.33*** | 0.2110 | 353.79 |
| Model 3 | 3 008.63*** | 0.000 | 359.79 | ||
| Model 4 | 3 008.63*** | 2.000 | 359.79 | ||
| Client self-reported mental health recovery | |||||
| Total RMQ | |||||
| Model 1 | 1 838.62*** | ||||
| Model 2 | 1 829.48*** | 2.490 | 198.18** | 0.1534 | 322.98 |
| Model 3 | 1 829.48*** | 0.000 | 326.98 | ||
| Model 4 | 1 829.48*** | 0.000 | 326.98 | ||
Note. AIC = Akaike information criterion; CFI = comparative fit indices; IMR = Illness Management and Recovery scale; LR = log-likelihood ratio; RMQ = Recovery Markers Questionnaire. Model 1 is a 2-level variance components model including only an intercept, patient identifier, a repeated assessment-level residual error term, and the patient propensity score. Model 2 is a 2-level model wherein the days since baseline assessment, treatment group condition, and the treatment group condition by days interaction explanatory variables were introduced at the repeated assessment level. Model 3 is a 2-level model similar to model 2 with the exception that the effect of the treatment group condition was introduced as a patient-level coefficient. Model 4 is the full multivariate model. It is a 2-level model similar to model 3 with the exception that the effect of the cross-level interaction between treatment group condition and baseline assessment was introduced as a patient-level coefficient. The LR test (χ2) comparison with preceding model associated with model 4 addresses the question as to whether changes in mental health recovery over time differ between patient-centered medical home and services as usual participants.
*P < .05; **P < .01; ***P < .001.
Clinician-reported mental health recovery.
We assessed a full multivariate model by including the treatment group condition by days cross-level interaction effect at the patient level and fit to total IMR, IMR Factor 1 Recovery scores, IMR Factor 2 Management scores, and IMR Factor 3 Substance scores. We used z tests to confirm that the fixed effect of days since baseline assessment improves the fit of the model for total IMR scores (z = 23.75; P < .001), IMR Factor 1 Recovery scores (z = 27.61; P < .001), IMR Factor 2 Management scores (z = 26.95; P < .001), and IMR Factor 3 Substance scores (z = 2.66; P = .008). Results suggest that the fixed effect of treatment group condition does not improve the fit of the model for total IMR scores (z = −1.44; P = .148), IMR Factor 1 Recovery scores (z = −0.71; P = .475), IMR Factor 2 Management scores (z = −0.17; P = .868), or for IMR Factor 3 Substance scores (z = 0.73 P = .467). The z tests regarding the fixed effect of the treatment group condition by days since baseline assessment interaction varied between total IMR and factor scores. Specifically, results suggest that the fixed effect of this interaction does improve the fit of the model for total IMR scores (z = 1.99; P = .047), IMR Factor 1 Recovery scores (z = 2.57; P = .01), and IMR Factor 2 Management scores (z = 3.12; P = .002), but does not improve the fit of the model for IMR Factor 3 Substance scores (z = 0.43; P = .667).
Likelihood-ratio tests comparing this full model to a similar model that does not include the cross-level interaction between treatment group condition and days since baseline assessment at the patient level indicates significantly better fit when the cross-level interaction is included with regard to total IMR scores (LR χ2[1] = 4696.97; P < .001), and IMR Factor 2 Management scores (LR χ2[1] = 7.9; P = .005), but no difference in the fit of the model with regard to IMR Factor 1 Recovery scores (LR χ2[1] = 3.22; P = .073), or IMR Factor 3 Substance scores (LR χ2[1] = 2.00; P = .158).
The AIC values for this full model associated with total IMR scores, IMR Factor 1 Recovery scores, IMR Factor 2 Management, and IMR Factor 3 Substance scores demonstrated poorer overall descriptive model fit compared with models excluding this cross-level interaction.
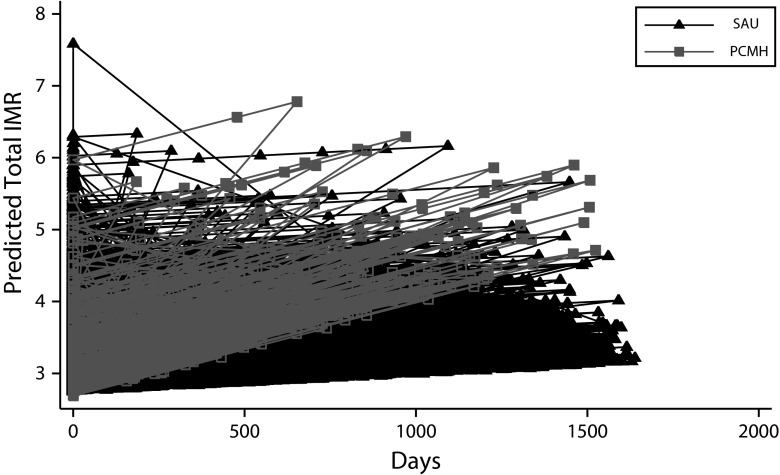
These analyses indicate that PCMH services result in greater improvements in clinician-rated measures of overall mental health recovery (Figure 2) and mental health management over time than SAU services. They also indicate that PCMH and SAU services result in similar improvements in the other clinician-rated measures of mental health recovery over time.
FIGURE 2—
Total Illness Management and Recovery scale score over time for services as usual and patient-centered medical home participants predicted from multilevel model: San Diego County, CA, 2011–2013.
Note. IMR = Illness Management and Recovery scale; PCMH = patient-centered medical home; SAU = services as usual.
Patient self-reported mental health recovery.
We assessed a full-multivariate model by including the treatment group condition by days cross-level interaction effect at the patient level and fit to total RMQ scores. The z tests confirm that the fixed effect of days since baseline assessment improves the fit of the model for total RMQ scores (z = 6.25; P < .001) whereas the fixed effect of treatment group condition (z = −1.06; P = .289) and the treatment group condition by days since baseline assessment interaction (z = −1.76; P = .078) do not improve the fit of the model for total RMQ scores.
The LR tests comparing this full model to a similar model that does not include the cross-level interaction between treatment group condition and days since baseline assessment at the patient level indicates no change in model fit when one includes the cross-level interaction with regard to total RMQ scores (LR χ2[1] = 0; P = 1).
The AIC value for this full model associated with total RMQ scores demonstrated no change in descriptive model fit in comparison with a similar model without the cross-level interaction.
These analyses indicate that PCMH and SAU services result in similar improvements in self-rated mental health recovery over time (Figure 3).
FIGURE 3—
Total Recovery Markers Questionnaire scores over time for services as usual and patient-centered medical home participants predicted from multilevel model: San Diego County, CA, 2011–2013.
Note. PCMH = patient-centered medical home; RMQ = Recovery Markers Questionnaire; SAU = services as usual.
DISCUSSION
For both clinician and patient ratings of mental health recovery, results suggest increases in mental health recovery over time irrespective of treatment group condition. Specifically, similar increases in clinician-reported IMR Factor 1 Recovery, and IMR Factor 3 Substance scores, and self-reported RMQ ratings of mental health recovery over time were found between PCMH and SAU participants. In addition, results suggested that for total IMR and IMR Factor 2 Management scores, the increases in mental health recovery scores over time were greater for PCMH participants than for SAU participants.
The finding that total IMR and IMR Factor 2 Management scores varied as a function of treatment group condition, whereas IMR Factor 1 Recovery, IMR Factor 3 Substance scores, and total RMQ scores were similar between groups, is quite interesting especially when one considers the role of the PCMH in enhancing progress toward mental health recovery. The IMR Factor 2 Management scores represent a patient’s symptom distress or relapse, impairment of functioning, and psychiatric hospitalization. The IMR Factor 1 Recovery scores represent a patient’s progress toward personal goals, mental illness knowledge, involvement in self-help activities, and involvement of family or friends in treatment. The IMR Factor 3 Substance scores represent impairment of functioning through alcohol or drug use. Total IMR scores comprise these 3 factors.
The findings of this study suggest the PCMH, a model for primary care services, performs at least equally well as mental health SAU in facilitating a patient’s progression toward mental health recovery. Furthermore, the PCMH may facilitate a patient’s illness management to a greater degree than SAU, and that greater illness management may be what is driving enhancements in overall clinician-reported mental health recovery.
There may be features of the PCMH model of health care delivery that contribute to greater management of symptoms and functioning, and prevention of relapse and psychiatric hospitalizations, than SAU. Previous research has elucidated several common structure and process-related clinical indicators of the PCMH in practice that theoretically align with a recovery-oriented model of mental health service delivery, particularly with regard to illness self-management. These include screening and preventive care processes, patient-guided health management, and improved access to medical records with subsequent use and continuity of services.47–49
It is important to consider the possibility that the differences in providers’ ratings of mental health recovery over time between PCMH and SAU patients may be a function of greater motivation for PCMH providers to demonstrate progress than for SAU providers. With the program status as an innovation pilot that was recently funded by the Mental Health Services Act,50 there are likely processes in place to monitor the PCMH structures, processes, and outcomes to a greater degree than the monitoring that is taking place in SAU. There may also be greater incentive to demonstrate program effectiveness in the PCMH than in SAU to secure continued or additional financial support to maintain the program following the pilot period. The fact that patient self-ratings of mental health recovery over time did not differ between PCMH and SAU patients is potential support for the hypothesis that differences in provider ratings of mental health recovery over time between PCMH and SAU patients was driven by greater motivation for providers to demonstrate program effectiveness in the PCMH than in SAU. Nonetheless, these results have important implications as interest regarding the PCMH model of health care delivery and its potential to improve the quality of health care in the United States grows.
These results provide support that the PCMH can serve as an alternative model of health care delivery for patients with severe mental illness without sacrificing the mental health recovery of these patients. Furthermore, these results provide support that even greater increases in clinician-reported mental health recovery over time can be expected when patients with severe mental illness are provided health care through the PCMH model of service delivery than through services as usual. Although other studies have demonstrated the promise the PCMH model of health care delivery holds for improving the physiological health of its patients, this is the first study to our knowledge that demonstrates the promise the PCMH model of health care delivery holds for improving the mental health recovery of its patients.
The results of this study are particularly relevant when one considers that the PCMH model is an important component of health care transformation in the United States.51 The Affordable Care Act has features that inherently support and promote the PCMH model of service delivery.52 Among others, these provisions include financially incentivizing state Medicaid programs to transfer select patients into medical home health care, funding the Centers for Medicare and Medicaid Services to test innovative models of health care such as the PCMH, and supporting the information technology infrastructure investments the PCMH model requires. The Affordable Care Act is also transforming the way in which health care providers are delivering care as its push for integrated care particularly in the primary care system is supporting more collaborative, multidisciplinary or interdisciplinary models of service delivery such as the PCMH. Although many are hesitant to embrace health care reform in the United States, the results of this study demonstrate the potential benefits of the Affordable Care Act in facilitating greater improvements in mental health recovery over time through the support of the PCMH.
As the PCMH model of health care delivery continues to spread across the United States, another area for future research is the economics of service provision under the PCMH versus specialty behavioral health services, particularly with regard to the long-term economic impacts of implementing the PCMH model. Previous reports have demonstrated mixed results with regard to the overall costs of the PCMH, and direct comparisons between studies are difficult because of the significant variations in the way costs are measured.53–58
Limitations
There are several limitations of this study, one being the limited generalizability of our findings. Our findings represent one PCMH within a nation of PCMH implementation efforts. Although San Diego County is large and comprises a diverse cultural mix of residents, it is possible that unique features of this PCMH within this setting are driving results that would not be found elsewhere. Continued evaluative efforts should be taken to address generalizability.
Another limitation is the lack of randomization. Ultimately, the transfer of patients from the county mental health clinic into the PCMH was determined by clinical judgment. Semistructured interviews with PCMH staff have illuminated shared concerns across staff “that the program was slow to populate.”50 Furthermore, results indicate that mental health program staff members were reluctant to transfer patients into the PCMH (J. Leich, e-mail communication, May 13, 2013). As a result, qualitative differences may exist between patients selected for transfer into the PCMH and patients selected to remain in SAU. Although propensity score analyses facilitate the equating of treatment group conditions on baseline characteristics, it is limited to the equating of groups on observed characteristics. As a result, significant biases may remain.59 Without reliable identification and assessment of the characteristics used for determining eligibility for transfer into the PCMH, equating groups on these unknown characteristics is an inherent challenge.
Conclusions
This study is among the first to assess the impact of transformation efforts on mental health recovery and is among the first to demonstrate the promise that the PCMH model of health care delivery holds for improving the mental health recovery of its patients. Through the use of rigorous statistical techniques equating treatment group conditions in the absence of randomization with propensity scores, and multilevel modeling to account for the nested data structure of repeated assessments within individual patients, results support the notion that similar or greater increases in mental health recovery over time can be expected when patients with severe mental illness are provided treatment through the PCMH than through SAU. These results hold tremendous implications as interest regarding the potential for the PCMH model of health care delivery to improve the quality of health care in the United States grows. With continued implementation of the PCMH to treat clients with severe mental illness, additional rigorous evaluative efforts should be taken to inform more widespread adoption.
Acknowledgments
This project was supported by a National Research Service Award Individual Predoctoral Training Grant (F31-MH100758-01A1) with the National Institute of Mental Health.
Human Participant Protection
This project was reviewed and approved by the University of California San Diego Human Research Protections Program’s institutional review board in accordance with the requirements of the Code of Federal Regulations on the Protection of Human Subjects (45 CFR 46 and 21 CFR 50 and 56), including its relevant subparts.
References
- 1. Committee on Quality of Health Care in America, Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century, Washington, DC: National Academy Press; 2001. Available at: http://www.nap.edu/html/quality_chasm/reportbrief.pdf. Accessed December 13, 2012.
- 2.Bitton A, Martin C, Landon B. A nationwide survey of patient centered medical home demonstration projects. J Gen Intern Med. 2010;25(6):584–592. doi: 10.1007/s11606-010-1262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nolte E, McKee M. Variations in amenable mortality—trends in 16 high-income nations. Health Policy. 2011;103(1):47–52. doi: 10.1016/j.healthpol.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 4.Barr MS. The need to test the patient-centered medical home. JAMA. 2008;300(7):834–835. doi: 10.1001/jama.300.7.834. [DOI] [PubMed] [Google Scholar]
- 5.Bolin JN, Gamm L, Vest JR, Edwardson N, Miller TR. Patient-centered medical homes: will health care reform provide new options for rural communities and providers? Fam Community Health. 2011;34(2):93–101. doi: 10.1097/FCH.0b013e31820e0d78. [DOI] [PubMed] [Google Scholar]
- 6.Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20(10):953–957. doi: 10.1111/j.1525-1497.2005.0178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DeGruy FV, Etz RS. Attending to the whole person in the patient-centered medical home: the case for incorporating mental healthcare, substance abuse care, and health behavior change. Fam Syst Health. 2010;28(4):298–307. doi: 10.1037/a0022049. [DOI] [PubMed] [Google Scholar]
- 8. Robert Graham Center. The patient centered medical home: history, seven core features, evidence and transformational change. 2007. Available at: http://www.aafp.org/online/etc/medialib/aafp_org/documents/about/pcmh.Par.0001.File.dat/PCMH.pdf. Accessed December 13, 2012.
- 9.Crabtree BF, Nutting PA, Miller WL, Stange KC, Stewart EE, Jaén CR. Summary of the National Demonstration Project and recommendations for the patient-centered medical home. Ann Fam Med. 2010;8(suppl 1):S80–S90. doi: 10.1370/afm.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosser WW, Colwill JM, Kasperski J, Wilson L. Progress of Ontario’s family health team model: a patient-centered medical home. Ann Fam Med. 2011;9(2):165–171. doi: 10.1370/afm.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511–544. [PubMed] [Google Scholar]
- 12.Stange KC, Nutting PA, Miller WL et al. Defining and measuring the patient-centered medical home. J Gen Intern Med. 2010;25(6):601–612. doi: 10.1007/s11606-010-1291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koh HK, Tavenner M. Connecting care through the clinic and community for a healthier America. Am J Public Health. 2012;102(suppl 3):S305–S307. doi: 10.2105/AJPH.2012.300760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dickinson WP, Miller BF. Comprehensiveness and continuity of care and the inseparability of mental and behavioral health from the patient-centered medical home. Fam Syst Health. 2010;28(4):348–355. doi: 10.1037/a0021866. [DOI] [PubMed] [Google Scholar]
- 15.Rost K, Pyne JM, Dickinson LM, LoSasso AT. Cost-effectiveness of enhancing primary care depression management on an ongoing basis. Ann Fam Med. 2005;3(1):7–14. doi: 10.1370/afm.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith JL, Williams JW, II, Owen RR, Rubenstein LV, Chaney E. Developing a national dissemination plan for collaborative care for depression: QUERI series. Implement Sci. 2008;3:59. doi: 10.1186/1748-5908-3-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang PS, Simon GE, Kessler RC. Making the business case for enhanced depression care: the National Institute of Mental Health–Harvard work outcomes research and cost-effectiveness study. J Occup Environ Med. 2008;50(4):468–475. doi: 10.1097/JOM.0b013e31816a8931. [DOI] [PubMed] [Google Scholar]
- 18.Watts BV, Shiner B, Pomerantz A, Stender P, Weeks WB. Outcomes of a quality improvement project integrating mental health into primary care. Qual Saf Health Care. 2007;16(5):378–381. doi: 10.1136/qshc.2007.022418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.County of San Diego Health and Human Services Agency, Behavioral Health Division. Innovation work plan. 2009. Available at: http://www.mhsoac.ca.gov/Counties/Innovation/docs/InnovationPlans/SanDiego_INN_Final_Plan_12_09.pdf. Accessed December 13, 2012.
- 20.Rittenhouse DR, Thom D, Schmittdiel J. Developing a policy-relevant research agenda for the patient-centered medical home: a focus on outcomes. J Gen Intern Med. 2010;25(6):593–600. doi: 10.1007/s11606-010-1289-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.State of California. Innovation. 2011. Available at: http://www.dmh.ca.gov/Prop_63/MHSA/Innovation. Accessed December 13, 2012.
- 22. San Diego County Health and Human Services Agency. Agreement with Family Health Centers of San Diego for Physical Health Integration Pilot. County Agreement Number 536234.
- 23.American Psychological Association. Recovery principles. Monit Psychol. 2012;43(1):55. [Google Scholar]
- 24. Sklar M, Sarkin A, Choi K. Transforming a large mental health system with recovery-based assessment. Paper presented at: the 91st Annual Meeting of the Western Psychological Association; April 28–May 1, 2011; Los Angeles, CA.
- 25.County of San Diego Health and Human Services Agency. San Diego, CA: Health Services Research Center; 2011. Performance Improvement Project. [Google Scholar]
- 26.County of San Diego Health and Human Services Agency. San Diego, CA: Health Services Research Center; 2011. Full service partnerships outcomes report: IMPACT. Available at: http://hsrc.ucsd.edu/index.php/reports [password required]. Accessed December 13, 2012. [Google Scholar]
- 27.County of San Diego Health and Human Services Agency. San Diego, CA: Health Services Research Center; 2012. Full service partnerships outcomes report: FSP programs. [Google Scholar]
- 28.County of San Diego Health and Human Services Agency. San Diego, CA: Health Services Research Center; 2012. Full service partnerships outcomes report: FSP-Lite programs. [Google Scholar]
- 29.County of San Diego Health and Human Services Agency. IMR outcomes report. San Diego, CA: Health Services Research Center; 2011. Available at: http://hsrc.ucsd.edu/index.php/reports [password required]. Accessed December 13, 2012. [Google Scholar]
- 30.County of San Diego Health and Human Services Agency. County Mental Health Services Program Databook, FY2010–2011. San Diego, CA: Health Services Research Center; 2012. Available at: http://hsrc.ucsd.edu/index.php/reports [password required]. Accessed December 13, 2012. [Google Scholar]
- 31.Pilon D, Ragins M. 2007. Milestones of Recovery Scale (MORS) Available at: http://www.mhsoac.ca.gov/Meetings/docs/Meetings/2014/June/CFLC_LowRecovWkgp_061714_MilestonesOfRecoveryScale.pdf. Accessed April 20, 2015.
- 32.Mueser KT, Gingerich S, Salyers MP, McGuire AB, Reyes RU, Cunningham H. The Illness Management and Recovery (IMR) Scales (Client and Clinician Versions) Concord, NH: New Hampshire–Dartmouth Psychiatric Research Center; 2004. [Google Scholar]
- 33.Hasson-Ohayon I, Roe D, Kravetz S. The psychometric properties of the Illness Management and Recovery scale: client and clinician versions. Psychiatry Res. 2008;160(2):228–235. doi: 10.1016/j.psychres.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 34.Salyers MP, Godfrey JL, Mueser KT, Labriola S. Measuring illness management outcomes: a psychometric study of clinician and consumer rating scales for illness self-management and recovery. Community Ment Health J. 2007;43(5):459–480. doi: 10.1007/s10597-007-9087-6. [DOI] [PubMed] [Google Scholar]
- 35.Sklar M, Sarkin AJ, Groessl EJ, Gilmer T. The psychometric properties of the Illness Management and Recovery scale in a large American public mental health system. Psychiatry Res. 2012;199(3):220–227. doi: 10.1016/j.psychres.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 36.Ridgway P, Press A. Assessing the Recovery-Orientation of Your Mental Health Program: A User’s Guide for the Recovery-Enhancing Environment Scale (REE). Version 1. Lawrence, KS: University of Kansas, School of Social Welfare; 2004. [Google Scholar]
- 37.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 38.Pruzek RM. Introduction to the special issue on propensity score methods in behavioral research. Multivariate Behav Res. 2011;46:389–398. doi: 10.1080/00273171.2011.576618. [DOI] [PubMed] [Google Scholar]
- 39.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39:33–38. [Google Scholar]
- 40.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Luellen JK, Shadish WR, Clark MH. Propensity scores: an introduction and experimental test. Eval Rev. 2005;29(6):530–558. doi: 10.1177/0193841X05275596. [DOI] [PubMed] [Google Scholar]
- 42.West SG, Biesanz JC, Pitts SC. Causal inference and generalization in field settings experimental and quasi-experimental designs. In: Reis HT, Judd CM, editors. Handbook of Research Methods in Social and Personality Psychology. New York, NY: Cambridge University Press; 2000. pp. 40–88. [Google Scholar]
- 43.Gibbons RD, Hedeker D, Elkin I et al. Some conceptual and statistical issues in analysis of longitudinal psychiatric data: application to the NIMH Treatment of Depression Collaborative Research Program dataset. Arch Gen Psychiatry. 1993;50(9):739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- 44.Raudenbush S, Bryk A. Hierarchical Linear Models. 2nd ed. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 45.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 46.Burnham KP, Anderson DR. Model Selection and Multimodel Inference: A Practical Information-Theoretic Approach. New York, NY: Springer; 2002. [Google Scholar]
- 47.Hornick J, Ralph R, Salmons T. Washington, DC: Center for Mental Health Services; 1999. Images of power and solidarity: assessing relationships between staff and clients of mental health programs. National Conference on Mental Health Statistics. [Google Scholar]
- 48.US Department of Health and Human Services. Mental Health: A Report of the Surgeon General. Rockville, MD: Substance Abuse and Mental Health Services Administration, National Institute of Mental Health; 1999. Available at: http://www.surgeongeneral.gov/library/mentalhealth/home.html. Accessed December 13, 2012. [Google Scholar]
- 49.Tryon GS, Winograd G. Goal consensus and collaboration. Psychotherapy. 2011;48(1):50–57. doi: 10.1037/a0022061. [DOI] [PubMed] [Google Scholar]
- 50.County of San Diego Health and Human Services Agency. San Diego, CA: Health Services Research Center; 2012. I-CARE Physical Health Integration Project baseline evaluation report. [Google Scholar]
- 51.Davis K, Abrams M, Stremikis K. How the Affordable Care Act will strengthen the nation’s primary care foundation. J Gen Intern Med. 2011;26(10):1201–1203. doi: 10.1007/s11606-011-1720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. The Patient Protection and Affordable Care Act, Pub. L. No. 111-148, 124 Stat. 855 (March 2010).
- 53.Hoff T, Weller W, DePuccio M. The patient-centered medical home: a review of recent research. Med Care Res Rev. 2012;69(6):619–644. doi: 10.1177/1077558712447688. [DOI] [PubMed] [Google Scholar]
- 54.Milstein A, Gilbertson E. American medical home runs. Health Aff (Millwood) 2009;28(5):1317–1326. doi: 10.1377/hlthaff.28.5.1317. [DOI] [PubMed] [Google Scholar]
- 55.Fortune-Greeley AK, Greene SB. Community Care of North Carolina program evaluation: strategies and challenges. N C Med J. 2009;70(3):277–279. [PubMed] [Google Scholar]
- 56.Dorr DA, Wilcox AB, Brunker CP, Burdon RE, Donnelly SM. The effect of technology-supported, multidisease care management on the mortality and hospitalization of seniors. J Am Geriatr Soc. 2008;56(12):2195–2202. doi: 10.1111/j.1532-5415.2008.02005.x. [DOI] [PubMed] [Google Scholar]
- 57.Gilfillan RJ, Tomcavage J, Rosenthal MB et al. Value and the medical home: effects of transformed primary care. Am J Manag Care. 2010;16(8):607–614. [PubMed] [Google Scholar]
- 58.Reid RJ, Fishman PA, Yu O et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care. 2009;27:362–367. [PubMed] [Google Scholar]
- 59.Reid RJ, Coleman K, Johnson EA et al. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29(5):835–843. doi: 10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]