Abstract
Objectives. We evaluated a low-cost strategy for schools to improve the convenience and appeal of drinking water.
Methods. We conducted a group-randomized, controlled trial in 10 Boston, Massachusetts, schools in April through June 2013 to test a cafeteria-based intervention. Signage promoting water and disposable cups were installed near water sources. Mixed linear regression models adjusting for clustering evaluated the intervention impact on average student water consumption over 359 lunch periods.
Results. The percentage of students in intervention schools observed drinking water during lunch nearly doubled from baseline to follow-up compared with controls (+9.4%; P < .001). The intervention was associated with a 0.58-ounce increase in water intake across all students (P < .001). Without cups, children were observed drinking 2.4 (SE = 0.08) ounces of water from fountains; with cups, 5.2 (SE = 0.2) ounces. The percentage of intervention students observed with sugar-sweetened beverages declined (–3.3%; P < .005).
Conclusions. The current default of providing water through drinking fountains in cafeterias results in low water consumption. This study shows that an inexpensive intervention to improve drinking water’s convenience by providing cups can increase student water consumption.
Water is essential for life, and access to safe, clean drinking water is a hallmark of public health.1 Inadequate water intake has been linked with indicators of poor health, such as headaches,2 and associated with reduced cognitive functioning in children.3 Increasing water intake may improve attention, memory, and cognition.4,5 Replacing sugar-sweetened beverages (SSBs) with water facilitates weight loss in adults6 and could reduce energy intake and obesity risk in children,7–9 as well as the risk of dental caries.10 Despite these population benefits, water consumption among children and adolescents is low,11,12 and many children are not adequately hydrated.13 Increasing children’s water consumption could address several public health concerns simultaneously.14
Schools are a key partner in promoting water. Promoting student water consumption may be informed by a behavioral economics approach (i.e., “nudging” individuals toward making healthier choices15,16) and changing the default choice to a healthy choice. Wansink has proposed using a framework of making healthy foods “convenient, attractive, and normative.”17 Small modifications to school cafeterias can facilitate healthier choices.18–20
To improve drinking water access, the Healthy, Hunger-Free Kids Act of 2010 required schools participating in the National School Lunch Program to make free drinking water available in meal service areas during lunch.21 Although most students report that schools comply with this regulation,22 compliance can mean simply having a water fountain in the cafeteria, which does not necessarily translate to easy access or convenience. Drinking water access may be compromised in schools with older infrastructure23 or municipal water safety issues.24 Although schools may opt to provide bottled instead of tap water, this is a less sustainable solution because of the higher costs25 and the labor required for its distribution23; improving tap water access is therefore an important goal. However, even when students have access to free tap water, they may not drink it26; students often perceive tap water as unsafe or unpalatable27,28 despite tougher safety standards than bottled water.25 Improving drinking water access and increasing appeal are essential goals.
School-based interventions to increase water intake hold promise. Installing water fountains in German elementary schools increased water consumption and reduced prevalence of overweight in a randomized, controlled trial.29 Providing chilled, filtered water or reusable water bottles and educational materials in schools is associated with increased self-reported water intake.30–33 Placing water dispensers in school cafeterias is associated with an increased proportion of students drinking water.34 However, these interventions may be unfeasible for school districts with limited resources because they involve purchasing new materials and infrastructure and using instructional time for water promotion.
We aimed to evaluate a low-cost strategy for schools to improve the convenience and appeal of drinking water by using a randomized, controlled trial design. We hypothesized that an intervention involving promotional signage and the provision of cups would increase average student water consumption, increase the proportion of students who opt to drink water, and decrease the frequency of students bringing SSBs to drink at lunch.
METHODS
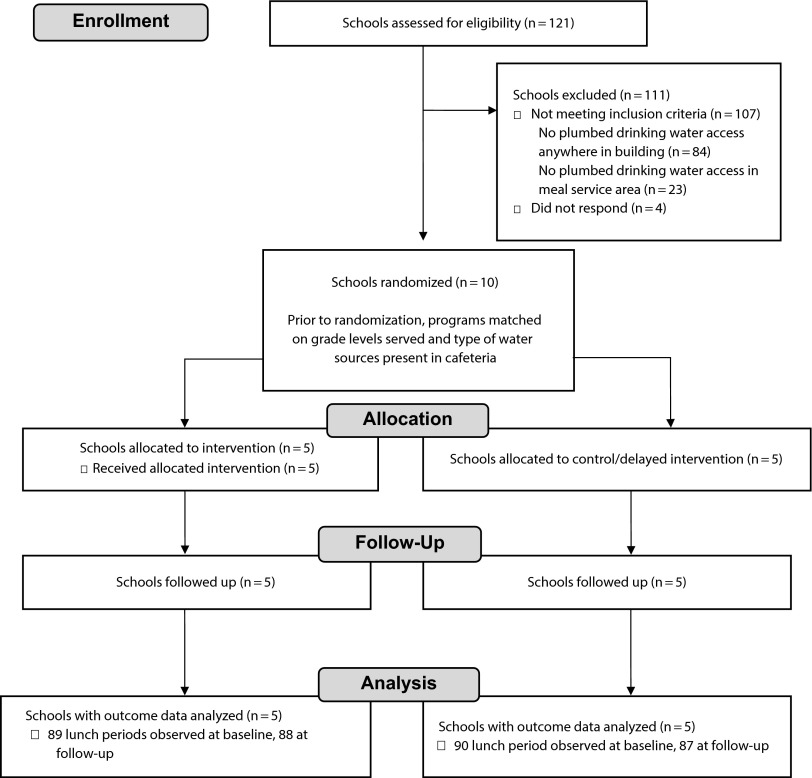
Ten Boston public schools (BPSs) participated in a group-randomized, controlled intervention trial from April to June 2013 (Figure 1). The unit of randomization was the school and the unit of analysis was the lunch period, with repeated observations of lunch periods over several days. Schools were eligible if they had plumbed cafeteria drinking water units that students could consistently access during lunch. To assess eligibility, a telephone survey was conducted in February 2013 of all BPSs identified as having any plumbed drinking water access (n = 37; other BPSs have bottled water only35). All 14 schools identified from this survey were invited to participate via a memorandum sent to school principals; 10 agreed to participate. We estimated that to detect an effect size of 0.14 ounces per student with 95% power, we would need 8 schools with 15 repeated observations of lunch per school.
FIGURE 1—
Grab a Cup, Fill It Up! intervention trial flow chart, Boston Public Schools, April–June 2013.
Schools were matched as closely as possible by the number and type of water sources (e.g., 1 or 2 fountains, fountain only, or fountain plus cooler) and by grade level. A colleague not involved in the study then randomized within these matched pairs to intervention or control status following baseline data collection by using a computer-based random number generator (5 intervention schools, 5 controls). Control schools received no intervention but were offered intervention materials the following year.
The primary outcome was change in the average amount of water consumed across the student population per lunch period. Secondary outcomes included changes in the percentage of students at each lunch who consumed water and changes in the percentage of students with SSBs at lunch. These outcomes were assessed during each lunch period for a week of consecutive school days at both baseline (April 2013) and 3 weeks later at follow-up (May–June 2013) via direct observation by trained research assistants.
Intervention
The “Grab a Cup, Fill It Up!” intervention was developed in partnership with BPS Food and Nutrition Services, BPS Health and Wellness, and BPS Facilities Management departments. Its goal was to increase water consumption by making drinking water more convenient and attractive to students while requiring minimal costs and staff time.
The intervention had 2 components. First, to promote water’s appeal, posters highlighting water source locations and encouraging consumption were displayed near cafeteria water access points. The posters were developed for a wide range of age groups and reading levels, with input from BPS students and staff. Second, to make consuming water easier, cup dispensers were installed next to cafeteria water fountains and stocked with 5-ounce recyclable cups chosen by BPS Food and Nutrition Services. Cafeteria managers and custodial staff at intervention schools agreed to stock the dispensers as part of their regular tasks.
Measures
Primary outcome.
The average amount of water consumed during lunch was measured with direct observation protocols. No identifying information was collected on students. During each lunch period observed, one research assistant counted the total number of students present while another research assistant measured student water intake.
For fountains, which were present in all participating schools, research assistants first estimated the flow rate by recording the amount of time (to 1/10 second) required to draw 8 ounces from the fountain. Each time a student used a fountain, research assistants recorded how long the student had the fountain turned on and in use, noting whether the student drank directly from the fountain or filled a cup or bottle. We estimated the ounces of water each student drew from the fountain by multiplying the time they used the fountain by the fountain’s flow rate. We assumed children consumed 96% of the water in their cup or bottle if they used one, and assumed that children consumed 32% of the water from the fountain stream if they drank directly from the fountain (based on related studies36,37; see Appendix, available as a supplement to the online version of this article at http://www.ajph.org, for additional details).
When water coolers were also available (3 schools), we estimated average student consumption by weighing the cooler at the beginning and end of each lunch period, estimating the total weight of water taken by students, converting to ounces, and dividing by the total number of students in the cafeteria during the lunch period.
In one school, teachers served students water with pitchers and cups in addition to the fountain; we noted the cup size (3 ounces) and estimated whether children drank none (0%), some (33%), most (67%), or all (100%) of the water served to them.37
Finally, we calculated the average amount consumed per student per lunch period by summing the total amount of water consumed across all students and consumption methods and dividing by the number of students present in the cafeteria.
Secondary outcomes.
To estimate the proportion of students consuming water, we divided the number of students consuming water by the total number of students in the cafeteria during the lunch period. To document other beverages students had during lunch, research assistants selected 1 table (not the same each day) in the cafeteria before students were seated. After students sat down, the research assistants recorded the beverage(s) each student had with his or her lunch. If time allowed, the research assistants moved to other tables to document beverages for more children. Research assistants were trained to categorize beverages on the basis of the beverage label and packaging as SSBs (this included calorically sweetened soda, energy drinks, fruit drinks, sports drinks, and coffee or tea), milk (including flavored milks), 100% juice, water from the cafeteria, water brought from outside the cafeteria, other beverages (e.g., smoothies, diet beverages), or no beverage. We estimated the proportion of students with each type of beverage by dividing the number observed with each beverage by the total number of students observed in the table scan. On average, research assistants documented beverages for 65% (SD = 35%) of the students in the lunchroom. Research assistants were not informed about the intervention purpose or school intervention status.
Research staff visited intervention schools weekly after implementation to document whether posters were in place and cups were available and to ask cafeteria managers about implementation progress.
Intervention staff recorded the costs of printing posters, installing cup dispensers, and supplying cups. We calculated start-up costs and ongoing costs separately. Start-up costs included posters (4 per school) and cup dispensers (2 per school) and installation costs. Ongoing costs included the average cost per day of providing cups. The cost of recycling the cups was not estimated because the schools had existing recycling programs.
We obtained grade levels served, student–teacher ratio, total enrollment, and enrollment by race/ethnicity, English-language-learner status, and free or reduced-price lunch status from BPS.
Statistical Analysis
Multilevel linear regression models estimated the difference in the change in average amount of water consumed and proportion of students consuming water per lunch period from baseline to follow-up between intervention and control schools. The unit of analysis was the lunch period. We used PROC MIXED in SAS version 9.3 (SAS Institute, Cary, NC) to account for the clustering of repeated observation days and lunch periods within schools.
At baseline, we observed 8 schools for 5 consecutive days and 2 schools for 3 or 4 days because of scheduling conflicts, for a total of 47 observation days and 179 lunch periods; we observed 1599 instances of a student drinking water. At follow-up, we observed 8 schools for 5 days and 2 for 4 days because of a holiday, for a total of 48 observation days and 180 lunch periods; we observed 2021 instances of a student drinking water. The number of observation days and lunch periods did not differ between intervention and control schools at baseline or follow-up. We used intention-to-treat protocols for all analyses of intervention impact.
RESULTS
Participating schools educated a diverse student body across a range of grade levels (Table 1). Three schools served kindergarten through 8th grade, and 4 were high schools. Six schools (3 intervention matched with 3 controls) had water fountains only in their cafeterias; 2 (1 intervention matched with 1 control) had coolers and fountains just outside the cafeteria that students were allowed to use during lunch. One control kindergarten-through-eighth-grade school had a fountain in addition to teacher-served water from pitchers and cups; this school was matched with an elementary intervention school with a fountain in addition to a cooler where teachers assisted children with getting water. Hispanic children made up about 40% of the student population, and most students were classified as low income.39
TABLE 1—
Characteristics of Schools (n = 10) Participating in the Grab a Cup, Fill It Up! Intervention Trial: Boston, MA, April–June 2013
| Variable | Intervention (n = 5), No. (%) or Mean ±SD | Control (n = 5), No. (%) or Mean ±SD | Pa |
| Grade levels | .46 | ||
| Elementary school | 2 (40) | 0 (0) | |
| Elementary and middle school combined | 1 (20) | 3 (60) | |
| High school | 2 (40) | 2 (40) | |
| Total enrollment | 725.2 ±554.0 | 874.0 ±988.87 | .8 |
| Male, average % | 49.3 ±5.5 | 45.4 ±9.2 | .48 |
| Race/ethnicity, average % | |||
| Non-Hispanic Black | 28.9 ±14.0 | 17.2 ±19.4 | .36 |
| Hispanic | 40.0 ±11.8 | 40.2 ±36.9 | .99 |
| Non-Hispanic White | 19.7 ±16.9 | 30.0 ±29.1 | .56 |
| Asian | 9.3 ±9.0 | 9.6 ±13.3 | .98 |
| Multiracial | 1.8 ±0.9 | 2.5 ±2.2 | .56 |
| English-language learner, average % | 25.6 ±15.9 | 21.0 ±27.3 | .78 |
| Low income,b average % | 66.8 ±13.1 | 51.2 ±22.3 | .28 |
| Receiving special education services, average % | 19.2 ±12.5 | 10.7 ±7.3 | .24 |
| Student–teacher ratio | 12.9 ±2.8 | 15.6 ±3.9 | .3 |
| No. of students present in cafeteria per lunch period | 152.5 ±143.1 | 163.3 ±246.0 | .72 |
| Water sources available in cafeteria | .16 | ||
| Fountains only | 3 | 3 | |
| Fountains and a cooler | 1 | 1 | |
| Fountains and teacher-assisted cooler | 1 | 0 | |
| Fountains and teacher-assisted pitcher and cups | 0 | 1 |
Note. School characteristics obtained from Boston Public Schools.38
P values are from the t test for continuous variables and the Fisher exact test for categorical variables.
The percentage of low-income enrollment indicates the percentage of students who are eligible for free or reduced-price lunch, receive Transitional Aid to Families benefits, or are eligible for food stamps. (Source: Massachusetts Department of Elementary and Secondary Education.39)
There were no differences in student demographics between intervention and control schools. However, baseline water consumption was significantly different between intervention and control schools (0.5 fewer ounces per student at intervention compared with control schools; P < .001), with a lower percentage of students taking water at intervention schools compared with controls (–12.9%; P < .001). Among students who consumed water at baseline, the majority consumed by drinking directly from the fountain in both intervention (60.7%) and control schools (59.8%), with fewer students using their own cups or bottles to get water from the fountain (7.7% in control schools, 3.0% in intervention schools); few students consumed water from coolers (2.9% in control schools, 4.6% in intervention schools).
After we adjusted for clustering and study design, participating in the intervention was associated with a 0.58-ounce (95% confidence interval [CI] = 0.27, 0.90; P < .001) increase in the average ounces of water consumed per student per lunch period at follow-up compared with control status (Table 2).
TABLE 2—
Estimated Intervention Impact on Water Consumption Behaviors During Lunch Periods From Baseline to Follow-Up Among 10 Boston Public Schools, April–June 2013
| Variable | Baseline Unadjusted Mean (SE) | Follow-Up Unadjusted Mean (SE) | Crude Change | Adjusted Changea (95% CI) | P |
| Cafeteria-provided water consumed/student/lunch period, oz | |||||
| Interventionb | 0.21 (0.03) | 0.74 (0.10) | +0.53 | +0.58 (0.27, 0.90) | < .001 |
| Controlc | 0.71 (0.10) | 0.65 (0.07) | −0.06 | ||
| Students in cafeteria who take free water during lunch period, % | |||||
| Interventionb | 5.8 (0.9) | 13.1 (1.2) | +7.3 | +9.4 (4.4, 14.4) | < .001 |
| Controlc | 18.7 (1.4) | 16.7 (1.4) | −2.0 |
Note. CI = confidence interval.
Unadjusted analyses account for clustering of lunch periods within observation days within schools. Adjusted analyses additionally account for matched pair status.
The intervention group had 90 lunch periods at baseline and 87 lunch periods at follow-up.
The control group had 89 lunch periods at baseline and 88 lunch periods at follow-up.
At baseline, the average percentage of students who took water during each lunch period was 5.8% in intervention schools and 18.7% at control schools. At follow-up, the percentage of students taking water had increased to 13.1% in intervention schools and decreased to 16.7% in control schools (Table 2). The intervention was associated with a significant increase in the percentage of children who took water during lunch (+9.4%; P < .001) compared with control schools.
Nearly 10% of students in intervention schools were observed with SSBs at baseline (all coming from outside the school food service program, which did not offer SSBs), compared with 7.9% of control students (Table 3). At baseline, about half of the students observed had milk at their lunch table in both intervention and control schools. We infrequently observed 100% juice and other beverages. The intervention was associated with a −3.3% (95% CI = −5.7, −1.0; P = .005) reduction in the percentage of students observed with SSBs at lunch in intervention schools compared with control schools, and a −3.0% (95% CI = −5.6, −0.3; P = .03) reduction in the percentage of students with 100% juice. There were no significant changes observed with milk or other beverages.
TABLE 3—
Estimated Intervention Impact on the Percentage of Students With Various Beverages at Their Lunch Tables From Baseline to Follow-Up in 10 Boston Public Schools, April–June 2013
| Variable | Baseline Unadjusted Mean % (SE) | Follow-Up Unadjusted Mean % (SE) | Unadjusted Change | Adjusted Changea (95% CI) | P |
| Students with sugar-sweetened beverages at table | |||||
| Intervention | 10.3 (0.5) | 9.3 (0.6) | −1.0 | −3.3 (−5.7, −1.0) | < .001 |
| Control | 7.9 (2.4) | 10.2 (0.5) | +2.3 | ||
| Students with milk at table | |||||
| Intervention | 50.3 (1.9) | 49.5 (1.5) | −0.8 | +0.52 (−4.8, 5.8) | .85 |
| Control | 43.6 (1.1) | 43.1 (1.0) | −0.4 | ||
| Students with 100% juice at table | |||||
| Intervention | 2.3 (0.3) | 1.8 (0.2) | −0.5 | −3.0 (−5.6, −0.28) | .03 |
| Control | 6.6 (2.3) | 9.0 (0.6) | +2.4 | ||
| Students with other beverages at table | |||||
| Intervention | 0.8 (0.1) | 0.6 (0.1) | −0.2 | −0.28 (−1.0, 0.48) | .47 |
| Control | 1.4 (0.2) | 1.3 (0.2) | −0.1 |
Note. CI = confidence interval.
Unadjusted analyses account for clustering of lunch periods within observation days within schools. Adjusted analyses additionally account for matched pair status.
To further explore the potential mechanisms of the intervention, we estimated the impact of providing cups, hypothesizing that these were essential for increasing water intake. We noted that students who drank water from fountains drank an average of 2.4 ounces per lunch (SE = 0.08) when drinking directly from the fountain (regardless of intervention status or time), but drank an average of 5.2 ounces per lunch (SE = 0.2) when using a cup. At follow-up, 54.9% of students who drank water in intervention schools used cups, compared with 1.6% at baseline (in control schools, 0.1% of students drinking water used cups at baseline or follow-up); meanwhile, the percentages of students using bottles did not change from baseline to follow-up in intervention or control schools. Therefore, the biggest shift in intervention schools appeared to be from drinking directly from the fountain to drinking with cups.
To quantify the impact of the cups, we examined the 860 observations of students drinking water from fountains just among intervention schools at follow-up. We estimated the association between having an intervention-provided cup or self-provided bottle and water consumption by calculating a regression model (adjusted for clustering of observations by days, lunch periods, and schools) with indicator variables for using a cup (yes or no) or bottle (yes or no); drinking directly from the fountain stream was the reference condition. Using a cup was associated with 3.3 more ounces of water consumed (P < .001).
The average total start-up cost of this intervention was $241.26 per school. Cup dispensers were $11.99 each. Installation of cup dispensers at 5 schools cost $806.40 total, or $161.28 per school. On average, 4 posters ($14 each) were installed per school. We estimated a total of $0.64 per school per day for cups (22 cups used per school per day in intervention schools*$0.03 per cup). Ongoing costs totaled $0.64 per day per school, or less than a tenth of a cent per day per student.
Cafeteria managers at intervention schools made positive comments about the intervention. At 2 schools, posters required replacement. Two schools (one of which had also had difficulty with signage) reported problems with stocking the cups consistently. The mean duration of the signage component of the intervention was 20.2 (3.0) days, with a range of 16 to 23 days. The mean duration of the cup component of the intervention was 15.4 (7.6) days, with a range of 5 to 22 days.
DISCUSSION
This group-randomized, controlled trial demonstrated that a low-cost intervention promoting the convenience and attractiveness of drinking water increased water consumption across the student population. The amount of water consumed per student more than tripled in intervention schools (from 0.21 to 0.74 ounces per student) while staying about the same in control schools (0.71 vs 0.65 ounces per student); similarly, the percentage of students choosing to drink water during lunch more than doubled, from 5.8% at baseline to 13.1% at follow-up. In addition, as more students consumed water during lunch, fewer students were observed with SSBs or 100% juice. The proportion of students taking milk did not change.
These results are consistent with studies of similar strategies to increase students’ water intake.29–34 Taken together, these findings suggest that schools can use a range of strategies to make it easier for students to drink more water, and that simple modifications to the school’s drinking water environment can have a significant impact. Although previous research has shown higher-cost strategies to be effective (i.e., purchasing reusable water bottles30 and updated water fixtures29,33,34), this study shows that simply providing cups—a strategy costing less than one tenth of a cent per student each day—can increase student water intake and the prevalence of water consumption.
These results also suggest that providing water to students through drinking fountains alone is a fairly inefficient and ineffective approach. We estimate that students intake about 2.4 (SE = 0.08) ounces from fountains, wasting two thirds of the water coming from the fountain. At follow-up, among intervention schools, students who drank water from a fountain by using a 5-ounce cup consumed 3.3 more ounces of water than students who drank directly from the fountain stream. Drinking directly from fountains is simply a less-efficient strategy for drinking water.36 Improving drinking water infrastructure, updating fixtures, and further increasing convenience, perhaps by offering tap water as a beverage on a lunch line,34 may also be necessary for increasing water intake further. However, for districts with limited resources, simply providing cups next to existing water fountains may be an effective strategy for increasing intake and reducing water waste. Promotion of reusable water bottles may be appropriate, particularly in schools without recycling programs or districts attempting to reduce overall waste production. Future studies should explore the impact of different strategies for water delivery on consumption.
Increasing student water intake may reduce the frequency with which students have an SSB at lunch. Although one previous similar intervention saw reductions in SSB consumption as water intake increased,31 most evaluations have not, despite including intervention activities targeted at reducing SSB consumption.29–31,33,40 It is possible that the SSB results in our study may not be generalizable to other schools (at the time of the study, BPSs’ policy on SSBs, which completely banned the sale or provision of SSBs on school property or at school-sponsored events, was stronger than most schools’). In addition, we were unable to measure SSB intake; it is possible that actual intake did not change despite the decreased prevalence of SSBs at lunch. Future research should further evaluate whether interventions to promote drinking water can also significantly reduce SSB consumption.
Although water intake, and the proportion of students taking water at lunch, did increase in this study, the average water consumed per lunch period across all students was still low. Post hoc analyses suggested that water consumption may have been even lower in high schools. Several of the school principals, cafeteria managers, and teachers at participating high schools informally reported to research assistants that students perceived the water from fountains as being poor quality, echoing findings from previous studies.27,28 In addition, many students avoided drinking any beverage with their lunches. In our study, at any given time, and across all grade levels, more than one quarter of students had nothing to drink with their lunch. Future intervention studies could assess whether more intensively targeting student perceptions of drinking water, especially tap water, might have a more favorable impact on water consumption, particularly among older students. Additional research should be conducted with students to understand why they do not consume a beverage with lunch.
We used a randomized, controlled design and observational methods to measure water intake, rather than relying on student self-report. Particularly with younger children, self-report of dietary intake is often not valid41 and may be subject to self-reporting biases in intervention studies. However, although research assistants were blinded to the intervention, it is possible that they ascertained what the intervention entailed. We could not assess intake over time at an individual student level, although we were still able to estimate the intervention’s population impact by using repeated observations of population-level data. In addition, because of the study’s short follow-up, we were unable to determine long-term impact on student behaviors.
Schools may increase student water intake during lunch and promote the habit of consuming water as a beverage via low-cost strategies such as providing cups and promoting water via signs. This inexpensive method to support student health cost less than a cent per student per day.
Acknowledgments
E. L. Kenney, S. L. Gortmaker, J. F. Reiner, and A. L. Cradock were supported by Cooperative Agreement 1U48DP001946 (including the Nutrition and Obesity Policy Research and Evaluation Network) from the Centers for Disease Control and Prevention, Prevention Research Centers Program. E. L. Kenney and S. L. Gortmaker were also supported by an anonymous donation in memory of Melvin R. Seiden.
The authors wish to thank Jeffrey Lane and William Grubbs of the Boston Public Schools and Michael Peck for their invaluable assistance in implementing the intervention, as well as the cafeteria managers and custodial staff in intervention schools. We also thank Rosalie Malsberger for her assistance with data management.
Note. The Centers for Disease Control and Prevention and the anonymous donor had no role in the design, analysis, or writing of this article.
Human Participant Protection
The study was approved by the Harvard T. H. Chan School of Public Health Office of Human Research Administration and the Boston Public Schools’ Data and Accountability Department and was registered with clinicaltrials.gov (NCT02280707).
References
- 1.Centers for Disease Control and Prevention. Ten great public health achievements—worldwide, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(24):814–818. [PubMed] [Google Scholar]
- 2.Shirreffs SM, Merson SJ, Fraser SM, Archer DT. The effects of fluid restriction on hydration status and subjective feelings in man. Br J Nutr. 2004;91(6):951–958. doi: 10.1079/BJN20041149. [DOI] [PubMed] [Google Scholar]
- 3.Bar-David Y, Urkin J, Kozminsky E. The effect of voluntary dehydration on cognitive functions of elementary school children. Acta Paediatr. 2005;94(11):1667–1673. doi: 10.1080/08035250500254670. [DOI] [PubMed] [Google Scholar]
- 4.Benton D, Burgess N. The effect of the consumption of water on the memory and attention of children. Appetite. 2009;53(1):143–146. doi: 10.1016/j.appet.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Edmonds CJ, Burford D. Should children drink more water?: the effects of drinking water on cognition in children. Appetite. 2009;52(3):776–779. doi: 10.1016/j.appet.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 6.Tate DF, Turner-McGrievy G, Lyons E et al. Replacing caloric beverages with water or diet beverages for weight loss in adults: main results of the Choose Healthy Options Consciously Everyday (CHOICE) randomized clinical trial. Am J Clin Nutr. 2012;95(3):555–563. doi: 10.3945/ajcn.111.026278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Popkin BM, D’Anci KE, Rosenberg IH. Water, hydration, and health. Nutr Rev. 2010;68(8):439–458. doi: 10.1111/j.1753-4887.2010.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang YC, Ludwig DS, Sonneville K, Gortmaker SL. Impact of change in sweetened caloric beverage consumption on energy intake among children and adolescents. Arch Pediatr Adolesc Med. 2009;163(4):336–343. doi: 10.1001/archpediatrics.2009.23. [DOI] [PubMed] [Google Scholar]
- 9.Briefel RR, Wilson A, Cabili C, Hedley Dodd A. Reducing calories and added sugars by improving children’s beverage choices. J Acad Nutr Diet. 2013;113(2):269–275. doi: 10.1016/j.jand.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 10.Armfield JM, Spencer J, Roberts-Thomson K, Plastow K. Water fluoridation and the association of sugar-sweetened beverage consumption and dental caries in Australian children. Am J Public Health. 2013;103(3):494–500. doi: 10.2105/AJPH.2012.300889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drewnowski A, Rehm CD, Constant F. Water and beverage consumption among adults in the United States: cross-sectional study using data from NHANES 2005–2010. BMC Public Health. 2013;13:1068. doi: 10.1186/1471-2458-13-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kant AK, Graubard BI. Contributors of water intake in US children and adolescents: associations with dietary and meal characteristics—National Health and Nutrition Examination Survey 2005–2006. Am J Clin Nutr. 2010;92(4):887–896. doi: 10.3945/ajcn.2010.29708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stookey JD, Brass B, Holliday A, Arieff A. What is the cell hydration status of healthy children in the USA? Preliminary data on urine osmolality and water intake. Public Health Nutr. 2012;15(11):2148–2156. doi: 10.1017/S1368980011003648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Drinking water: water and nutrition. 2014. Available at: http://www.cdc.gov/healthywater/drinking/nutrition. Accessed November 10, 2014.
- 15.Thaler RH, Sunstein CR. Nudge: Improving Decisions About Health, Wealth, and Happiness. Rev. and expanded ed. New York, NY: Penguin Books; 2009. [Google Scholar]
- 16.Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298(20):2415–2417. doi: 10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- 17.Wansink B. Convenient, attractive, and normative: the CAN approach to making children slim by design. Child Obes. 2013;9(4):277–278. doi: 10.1089/chi.2013.9405. [DOI] [PubMed] [Google Scholar]
- 18.Wansink B, Hanks AS. Slim by design: serving healthy foods first in buffet lines improves overall meal selection. PLoS ONE. 2013;8(10):e77055. doi: 10.1371/journal.pone.0077055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hanks AS, Just DR, Smith LE, Wansink B. Healthy convenience: nudging students toward healthier choices in the lunchroom. J Public Health (Oxf) 2012;34(3):370–376. doi: 10.1093/pubmed/fds003. [DOI] [PubMed] [Google Scholar]
- 20.Schwartz MB. The influence of a verbal prompt on school lunch fruit consumption: a pilot study. Int J Behav Nutr Phys Act. 2007;4:6. doi: 10.1186/1479-5868-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Child Nutrition and WIC Reauthorization Act of 2004. Pub. L. No. 108–265.
- 22.Hood NE, Turner L, Colabianchi N, Chaloupka FJ, Johnston LD. Availability of drinking water in US public school cafeterias. J Acad Nutr Diet. 2014;114(9):1389–1395. doi: 10.1016/j.jand.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 23.Cradock AL, Wilking CL, Olliges SA, Gortmaker SL. Getting back on tap: the policy context and cost of ensuring access to low-cost drinking water in Massachusetts schools. Am J Prev Med. 2012;43(3, suppl 2):S95–S101. doi: 10.1016/j.amepre.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 24.Ramirez SM, Stafford R. Equal and universal access?: water at mealtimes, inequalities, and the challenge for schools in poor and rural communities. J Health Care Poor Underserved. 2013;24(2):885–891. doi: 10.1353/hpu.2013.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel AI, Hampton KE. Encouraging consumption of water in school and child care settings: access, challenges, and strategies for improvement. Am J Public Health. 2011;101(8):1370–1379. doi: 10.2105/AJPH.2011.300142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patel AI, Chandran K, Hampton KE et al. Observations of drinking water access in school food service areas before implementation of federal and state school water policy, California, 2011. Prev Chronic Dis. 2012;9:E121. doi: 10.5888/pcd9.110315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Onufrak SJ, Park S, Sharkey JR, Merlo C, Dean WR, Sherry B. Perceptions of tap water and school water fountains and association with intake of plain water and sugar-sweetened beverages. J Sch Health. 2014;84(3):195–204. doi: 10.1111/josh.12138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patel AI, Bogart LM, Uyeda KE, Rabin A, Schuster MA. Perceptions about availability and adequacy of drinking water in a large California school district. Prev Chronic Dis. 2010;7(2):A39. [PMC free article] [PubMed] [Google Scholar]
- 29.Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics. 2009;123(4):e661–e667. doi: 10.1542/peds.2008-2186. [DOI] [PubMed] [Google Scholar]
- 30.Patel AI, Bogart LM, Elliott MN et al. Increasing the availability and consumption of drinking water in middle schools: a pilot study. Prev Chronic Dis. 2011;8(3):A60. [PMC free article] [PubMed] [Google Scholar]
- 31.Siega-Riz AM, El Ghormli L, Mobley C et al. The effects of the HEALTHY study intervention on middle school student dietary intakes. Int J Behav Nutr Phys Act. 2011;8:7. doi: 10.1186/1479-5868-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laurence S, Peterken R, Burns C. Fresh Kids: the efficacy of a Health Promoting Schools approach to increasing consumption of fruit and water in Australia. Health Promot Int. 2007;22(3):218–226. doi: 10.1093/heapro/dam016. [DOI] [PubMed] [Google Scholar]
- 33.Loughridge JL, Barratt J. Does the provision of cooled filtered water in secondary school cafeterias increase water drinking and decrease the purchase of soft drinks? J Hum Nutr Diet. 2005;18(4):281–286. doi: 10.1111/j.1365-277X.2005.00622.x. [DOI] [PubMed] [Google Scholar]
- 34.Elbel B, Mijanovich T, Abrams C et al. A water availability intervention in New York City public schools: influence on youths’ water and milk behaviors. Am J Public Health. 2014 doi: 10.2105/AJPH.2014.302221. Epub ahead of print December 18, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cradock AL, McHugh A, Mont-Ferguson H et al. Effect of school district policy change on consumption of sugar-sweetened beverages among high school students, Boston, Massachusetts, 2004–2006. Prev Chronic Dis. 2011;8(4):A74. [PMC free article] [PubMed] [Google Scholar]
- 36.Coetzee K, Bennett C. The efficiency of a drinking fountain. Appl Ergon. 1978;9(2):97–100. doi: 10.1016/0003-6870(78)90155-2. [DOI] [PubMed] [Google Scholar]
- 37.Kenney EL, Davison KK, Austin SB et al. Validity and reliability of a simple, low cost measure to quantify children’s dietary intake in afterschool settings. J Acad Nutr Diet. 2015;115(3):426–432. doi: 10.1016/j.jand.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boston, MA: Boston Public Schools; 2013. 2012–2013 reports on teaching and learning for participating schools. [Google Scholar]
- 39.Massachusetts Department of Elementary and Secondary Education. Profiles help: about the data: public schools and districts: students. Available at: http://profiles.doe.mass.edu/help/data.aspx?section=students. Accessed November 10, 2014.
- 40.Visscher TL, van Hal WC, Blokdijk L, Seidell JC, Renders CM, Bemelmans WJ. Feasibility and impact of placing water coolers on sales of sugar-sweetened beverages in Dutch secondary school canteens. Obes Facts. 2010;3(2):109–115. doi: 10.1159/000300848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Livingstone MB, Robson PJ, Wallace JM. Issues in dietary intake assessment of children and adolescents. Br J Nutr. 2004;92(suppl 2):S213–S222. doi: 10.1079/bjn20041169. [DOI] [PubMed] [Google Scholar]