Abstract
Objectives. We assessed whether living in counties with Title X clinics and increased use of long-acting reversible contraception (LARC) in Colorado are associated with decreased risk of adverse birth outcomes.
Methods. We linked Title X clinic counties to the Colorado birth data set by using the mother’s county of residence. We compared low birth weight (LBW) and preterm birth (PTB) in 2008 and 2012, in counties with and without Title X clinics. We compared the relationship between LARC use and the incidence of LBW or PTB in 2012 for women living in counties with Title X clinics.
Results. For women living in counties with Title X clinics, the odds of PTB were significantly lower in 2012 compared with 2008 (odds ratio = 0.85; 95% confidence interval = 0.81, 0.89; interaction P = .02). For women living in Title X clinic counties in 2012, a higher proportion of LARC use (> 12.4%) was significantly associated with decreased risk of PTB (P = .02) compared with a low proportion of LARC use (≤ 4.96%).
Conclusions. Improved access to family planning services and increased use of LARC are associated with lower risk of PTB.
Unintended pregnancy is a significant public health issue in the United States. According to the most recent published estimates, 51% of pregnancies in the United States were unintended, and 60% of unintended pregnancies resulted in a live birth.1 Unintended pregnancies are associated with increased risk of adverse pregnancy outcomes, such as preterm birth (PTB) and delivery of low–birth weight (LBW) infants.2–8 In a large systematic review, Shah et al. reported increased odds of PTB (odds ratio [OR] = 1.31; 95% confidence interval [CI] = 1.09, 1.58) and LBW (OR = 1.36; 95% CI = 1.25, 1.48) among unintended pregnancies ending in live birth compared with intended pregnancies.2 The link between unintended pregnancy and poor birth outcomes is likely multifaceted, and may be associated with maternal socioeconomic risk factors, inadequate prenatal care, and preconceptual and prenatal maternal behavioral risk factors such as smoking and alcohol use.9–11 As part of the national effort to improve overall public health, increasing the proportion of pregnancies that are intended and decreasing the rates of PTB and LBW deliveries are all objectives of the Healthy People 2020 initiative.12
In 2008, 37% of live births in Colorado resulted from unintended pregnancies according to the Pregnancy Risk Assessment Monitoring System.13 To address this issue, the Colorado Initiative to Reduce Unintended Pregnancy (Colorado Initiative) was developed and enacted in 2009 with the generous support of an anonymous donor.14 As part of the effort, the Colorado Family Planning Initiative was implemented through the Colorado Department of Public Health and Environment. Two of the primary goals of the initiative were (1) increasing the number of women accessing family planning services and (2) increasing the adoption of long-acting reversible contraceptive (LARC) methods such as intrauterine devices and contraceptive implants.14 Long-acting reversible contraceptive methods are safe and highly effective forms of contraception that have been shown to reduce rates of unintended pregnancy.15–18
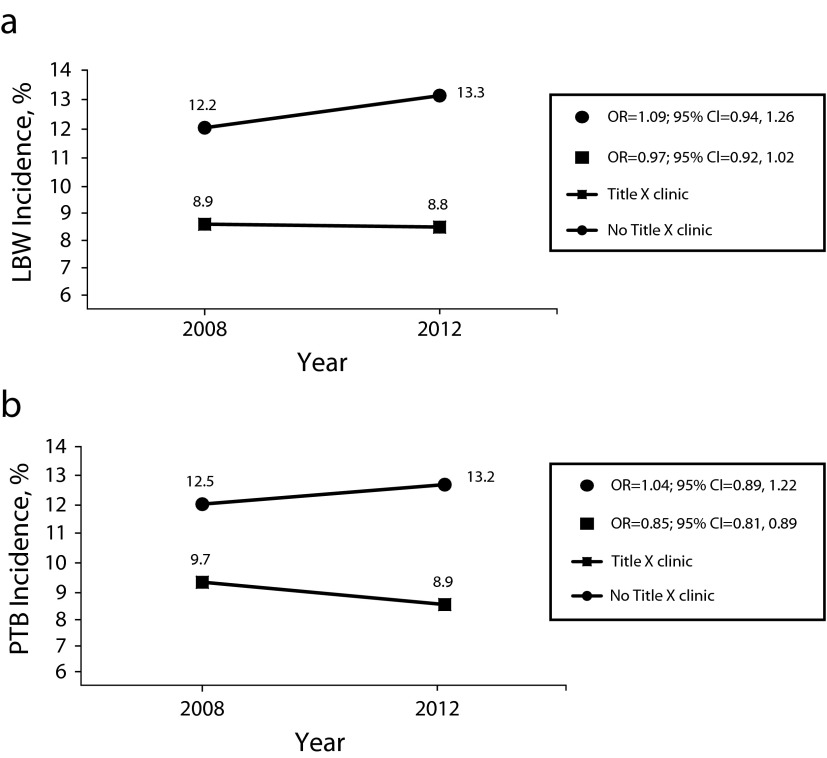
To help achieve these objectives, the Colorado Initiative provided funding to 28 Title X–funded agencies across the state of Colorado from 2009 to 2013, serving 37 of 64 Colorado counties. Those 37 counties were home to 95% of the state’s low-income population (defined as individuals with incomes at or below 150% of the federal poverty level).14 The locations of Colorado Title X clinics are shown in Figure 1. This distribution of resources in Colorado is important, in light of the known disparities of unintended pregnancy rates for women on the basis of socioeconomic status, age, race/ethnicity, and level of education.1
FIGURE 1—
Counties and locations of Title X clinics: Colorado, 2008 and 2012.
Source. Colorado Department of Public Health and Environment Family Planning Unit.
The funding for the Colorado Initiative specifically supported the provision of intrauterine devices and contraceptive implants to women seeking care at Title X clinics, training for providers and staff on the counseling and provision of LARC methods, and technical assistance to Title X agencies related to increasing the use of these methods.14 Many of the Title X clinics across the state successfully executed the primary objectives of the Colorado Initiative, resulting in a rise in the total number of clients accessing family planning services per year from 46 201 to 64 148 and the proportion of women choosing LARC methods out of all women using contraception at Title X clinics from 0.8% to 8.6% from 2008 to 2012 (G. Klinger, Colorado Department of Public Health and Environment, e-mail communication, April 1, 2014).
Although LARC use is on the rise in the United States, there is little in the published literature demonstrating an association between the use of LARC methods and rates of adverse birth outcomes.19 Given the scale of the Colorado Initiative, there is a unique opportunity to evaluate this possible association. As a result of improved use of family planning services in general and LARC use in particular, we hypothesized the following: (1) there will be a significant decrease in LBW and PTB in Colorado from 2008 to 2012; (2) for women living in Colorado counties in 2012 compared with 2008, LBW and PTB will differ by whether there is a Title X clinic in that woman’s county of residence; and (3) for women living in Colorado counties with Title X clinics in 2012, there will be a significant inverse association between LARC use at Title X clinics and LBW and PTB.
METHODS
We designed this study as a cross-sectional analysis of a cohort data set with an ecological exposure. We conducted the study with the Colorado Health Information birth data set and Title X clinic contraception data for 2008 and 2012, both obtained from Colorado Department of Public Health and Environment. The study population consisted of women who gave birth in Colorado in 2008 (n = 70 842) and 2012 (n = 65 959). We excluded nonsingleton births and records missing the woman’s county of residence, resulting in a total study population of 68 932 women in 2008 and 64 108 women in 2012. To look at the association between LARC use and LBW or PTB, we restricted the analysis to women living in counties with Title X clinics in 2012 (n = 59 979), as this was thought to be the peak of the Colorado Initiative’s impact on LARC use for which there were available data.
The outcome measures included (1) LBW defined as less than 2500 grams and (2) PTB defined as less than 37 weeks gestation, obtained from the Colorado birth data set. Small for gestational age, defined as an infant below the 10th percentile for weight for the infant’s gestational age, also could have been assessed as an adverse outcome. However, LBW and PTB have more direct implications on costly health care than small for gestational age, which applies to both term and preterm infants, does not take into account infants that are constitutionally small, and does not capture infants born preterm and LBW who are at an appropriate weight for their gestational age.20,21 For example, in one large study of very low–birth weight infants, only 22% were classified as small for gestational age.22 In addition, LBW and PTB are more frequently reported in the literature, allowing for better comparisons with previous research.2
We used the unpaired student t test to make bivariate comparisons of continuous baseline characteristics between women living in counties with Title X clinics and those without. We used the χ2 test to compare dichotomous and categorical data.
We used bivariate analysis and a literature review to determine which variables were important to include in the multivariable models. We included covariates if they met the definition of a confounding variable. In addition, we included covariates in the model regardless of their influence on the unstandardized regression parameter estimates if they were thought to be associated with the outcomes (LBW or PTB) based on previous literature.23 We assessed prenatal care with the GINDEX, which is a measure of the adequacy of prenatal care that takes into account the month prenatal care began, the number of prenatal care visits, and the gestational age at delivery.24 We conducted statistical analyses with SAS version 9.3 (SAS Institute Inc, Cary, NC). We considered P values less than .05 to be statistically significant.
We used a logistic regression model to examine the association between year of delivery (2008 compared with 2012) and LBW or PTB, with adjustment for maternal age, race/ethnicity, body mass index (BMI; defined as weight in kilograms divided by the square of height in meters), education, income, marital status, prenatal care, smoking status, history of gonorrhea, history of chlamydia, history of congenital anomaly, and interpregnancy interval. We included every birth record in the state during the 2 years of interest in this analysis, including the nonsingleton births and records missing the woman’s county of residence that we excluded for the remaining analyses.
We used a logistic regression model to conduct a stratified analysis to determine if year of delivery (2008 vs 2012) modified the association between having a Title X clinic in the county and LBW or PTB, with adjustment for maternal age, race/ethnicity, BMI, education, income, marital status, prenatal care, smoking status, history of gonorrhea, history of chlamydia, history of congenital anomaly, and interpregnancy interval.
To examine the effect of LARC use on LBW or PTB, we calculated use for each county containing a Title X clinic as the proportion of women using LARC methods out of all women using contraception at Title X clinics in that county. We then divided LARC use into quartiles, which we assigned to each woman in the 2012 birth data set according to her county of residence, and used as the ecological exposure.
We used generalized estimating equations to examine the association between quartiles of LARC use in counties with Title X clinics and LBW or PTB in 2012, with adjustment for maternal age, race/ethnicity, BMI, education, income, marital status, prenatal care, smoking status, history of gonorrhea, history of chlamydia, history of congenital anomaly, and interpregnancy interval.
RESULTS
Baseline characteristics of the study population by Title X clinic presence are shown for 2008 and 2012 in Table 1. In 2008, counties without Title X clinics had a significantly higher percentage of LBW and PTB, women who smoked more heavily during pregnancy, and women who were of a more high-risk age group (< 18 or > 40 years) compared with counties with a Title X clinic. In 2008, counties with a Title X clinic had a higher percentage of African American women. Education level and prepregnancy BMI did not differ significantly between the 2 groups in 2008. The results for 2012 were similar to those for 2008 with the exception that in 2012 counties without Title X clinics had a significantly higher percentage of women who had not completed a high-school education.
TABLE 1—
Baseline Characteristics of Births According to County Presence or Absence of a Title X Clinic: Colorado, 2008 and 2012
| 2008 |
2012 |
|||||
| Variables | Title X Clinic (n = 64 166), % or Mean ±SD | No Title X Clinic (n = 4766), % or Mean ±SD | P | Title X Clinic (n = 59 979), % or Mean ±SD | No Title X Clinic (n = 4129), % or Mean ±SD | P |
| Baseline characteristics | ||||||
| Maternal age, y | < .001 | < .001 | ||||
| <18 and >40 | 8.7 | 10.3 | 6.7 | 8.4 | ||
| 18–40 (Ref) | 91.3 | 89.7 | 93.3 | 91.6 | ||
| Maternal race/ethnicity | ||||||
| Non-Hispanic White (Ref) | 59.3 | 67.5 | 61.5 | 69.7 | ||
| Hispanic White | 28.0 | 18.4 | < .001 | 24.1 | 16.2 | < .001 |
| African American | 5.2 | 1.1 | < .001 | 5.7 | 0.8 | < .001 |
| Other | 7.5 | 13.0 | < .001 | 8.7 | 13.3 | < .001 |
| Maternal education | .62 | < .001 | ||||
| < high school completed | 21.3 | 21.1 | 14.5 | 16.9 | ||
| High-school graduate or higher degree obtained (Ref) | 78.7 | 78.9 | 85.5 | 83.1 | ||
| Maternal income, $ | ||||||
| < 15 000 (Ref) | 24.4 | 28.3 | 25.1 | 29.9 | ||
| 15 000-24 999 | 13.2 | 17.3 | .02 | 12.2 | 15.4 | .27 |
| 25 000-34 999 | 9.9 | 11.3 | .83 | 9.6 | 10.1 | .34 |
| 35 000-49 999 | 9.8 | 11.6 | .76 | 9.8 | 11.1 | .42 |
| 50 000-74 999 | 15.3 | 15.6 | .63 | 14.5 | 16.3 | .22 |
| > 75 000 | 27.5 | 15.9 | < .001 | 28.8 | 17.2 | < .001 |
| Maternal smoking status | ||||||
| ≥10 cigarettes/d | 3.9 | 7.2 | < .001 | 3.1 | 5.5 | < .001 |
| 1–9 cigarettes/d | 4.5 | 6.3 | < .001 | 4.2 | 5.7 | < .001 |
| Nonsmoker (Ref) | 91.6 | 86.5 | 92.7 | 88.8 | ||
| Maternal marital status | ||||||
| Married (Ref) | 73.3 | 68.8 | 75.2 | 69.0 | ||
| Divorced | 1.3 | 2.0 | < .001 | 1.9 | 3.0 | < .001 |
| Never married | 23.5 | 26.6 | < .001 | 21.1 | 26.3 | < .001 |
| Widowed | 0.1 | 0.2 | .01 | 0.1 | 0.1 | .95 |
| Maternal prepregnancy BMI | 25.3 ±5.7 | 25.4 ±5.9 | .21 | 25.7 ±5.9 | 25.9 ±6.1 | .02 |
| GINDEX | ||||||
| No prenatal care | 3.2 | 1.2 | .01 | 2.4 | 1.6 | .01 |
| Inadequate prenatal care | 14.3 | 11.0 | < .001 | 13.6 | 9.4 | < .001 |
| Intermediate prenatal care | 27.0 | 31.8 | < .001 | 28.4 | 30.5 | .01 |
| Adequate prenatal care (Ref) | 48.1 | 50.8 | 49.1 | 52.8 | ||
| Excessive prenatal care | 7.4 | 5.2 | < .001 | 6.8 | 5.7 | < .001 |
| Months since most recent delivery | .08 | .88 | ||||
| < 18 | 13.5 | 14.4 | 12.5 | 12.5 | ||
| ≥ 18 (Ref) | 86.5 | 85.6 | 87.5 | 87.5 | ||
| STI history | ||||||
| Gonorrhea | 0.1 | 0.2 | .63 | 0.2 | 0.02 | .02 |
| Chlamydia | 1.9 | 2.1 | .53 | 2.1 | 2.1 | .93 |
| Congenital anomaly history | 1.7 | 4.5 | < .001 | 3.0 | 3.8 | .004 |
| Outcome variables | ||||||
| Birth weight, g | < .001 | < .001 | ||||
| < 2500 | 8.9 | 12.2 | 8.8 | 13.3 | ||
| ≥ 2500 (Ref) | 91.1 | 87.8 | 91.2 | 86.7 | ||
| Gestation, wk | < .001 | < .001 | ||||
| < 37 | 9.7 | 12.5 | 8.9 | 13.2 | ||
| ≥ 37 (Ref) | 90.3 | 87.5 | 91.1 | 86.8 | ||
Notes. BMI = body mass index (weight in kilograms divided by the square of height in meters); GINDEX = graduated index reflecting adequacy of prenatal care24; STI = sexually transmitted infection. We used the χ2 test to compare dichotomous and categorical data; we used the unpaired student t test to compare the continuous variable of BMI.
Overall Impact of the Colorado Initiative
Overall in the state of Colorado, there was a decrease in the percentage of PTB from 2008 to 2012 (8.92% vs 8.29%). After we adjusted for confounders, there was a 12% decrease in the odds of PTB when we compared 2012 (during the initiative) to 2008 (preinitiative; OR = 0.88; 95% CI = 0.84, 0.91; P < .001; data not shown).
The percentage of LBW deliveries in Colorado was 8.14% in 2012 compared with 8.17% in 2008, and in multivariable analysis, adjusted percentages were not significantly different (OR = 0.97; 95% CI = 0.91, 1.02; P = .14; data not shown).
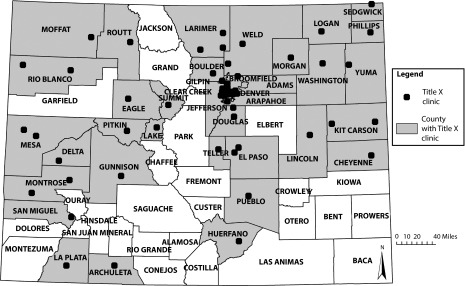
In multivariable analysis, the odds of PTB were significantly lower for women living in counties with a Title X clinic in 2012 compared with 2008 (OR = 0.85; 95% CI = 0.81, 0.89) but not for women living in counties without a Title X clinic (OR = 1.04; 95% CI = 0.89, 1.22; interaction of Title X county by year P = 0.02; Figure 2). There was no significant association between LBW and living in a county with or without a Title X clinic during the Colorado Initiative (2012) compared with before the initiative (2008; Figure 2).
FIGURE 2—
Risk, according to year and residence in a county with a Title X clinic, of (a) low birth weight and (b) preterm birth: Colorado, 2008 and 2012.
Note. CI = confidence interval; LBW = low birth weight; OR = odds ratio; PTB = preterm birth. Estimates obtained from crude incidence of low birth weight and preterm birth according to year (2008 or 2012) and residence in a county with and without a Title X clinic. Odds ratios obtained from logistic regression models, adjusted for maternal age, race/ethnicity, body mass index (weight in kilograms divided by the square of height in meters), education, income, marital status, prenatal care, smoking status, history of gonorrhea, history of chlamydia, history of congenital anomaly, and interpregnancy interval. Estimates with the 95% confidence intervals are shown. For low birth weight, the interaction P = .15; for preterm birth, P = .017.
Quartiles of Long-Acting Reversible Contraceptive Use
After we assessed the distribution of the proportion of LARC use at Title X clinics within each county, LARC uptake clearly differed at 4 meaningful and clinically interpretable levels (Table 2). In the unadjusted model, LARC use was not associated with PTB (OR = 0.89; 95% CI = 0.76, 1.04; P = .14 for LARC quartile 2 compared with 1; OR = 0.95; 95% CI = 0.82, 1.10; P = .47 for LARC quartile 3 compared with 1; and OR = 0.93; 95% CI = 0.82, 1.07; P = .32 for LARC quartile 4 compared with 1). In the adjusted model, exposure by county to the Title X clinics with the highest LARC use quartile (> 12.4%) was significantly associated with a decrease in PTB compared with exposure to clinics with the lowest LARC use quartile (≤ 4.96%), as shown in Table 2 (P = .02). The second LARC use quartile (4.97%–8.75%) was also significantly associated with a decrease in PTB compared with the lowest quartile (P = .04). The estimate for the third LARC use quartile (8.76%–12.4%) was in a similar direction but did not reach statistical significance (P = .15).
TABLE 2—
Risk of Low Birth Weight and Preterm Birth Associated With Long-Acting Reversible Contraception Use at Title X Clinics in the Woman’s County of Residence: Colorado, 2012
| Low Birth Weight |
Preterm Birth |
||||||
| LARC Use | Sample Size, No. | Incidence, % | OR (95% CI) | P | Incidence, % | OR (95% CI) | P |
| Quartile 1 (≤ 4.96%) | 16 035 | 8.77 | 1.00 (Ref) | 9.36 | 1.00 (Ref) | ||
| Quartile 2 (4.97%–8.75%) | 14 373 | 8.56 | 0.94 (0.82, 1.08) | .35 | 8.42 | 0.82 (0.71, 0.97) | .04 |
| Quartile 3 (8.76%–12.4%) | 15 133 | 8.63 | 0.96 (0.83, 1.10) | .47 | 8.91 | 0.89 (0.78, 1.03) | .15 |
| Quartile 4 (> 12.4%) | 15 494 | 8.29 | 0.92 (0.80, 1.07) | .24 | 8.81 | 0.81 (0.70, 0.96) | .02 |
Note. CI = confidence interval; LARC = long-acting reversible contraception. We obtained all estimates from a generalized estimating equation, with adjustment for maternal age, race/ethnicity, body mass index (weight in kilograms divided by the square of height in meters), education, income, marital status, prenatal care, smoking status, history of gonorrhea, history of chlamydia, history of congenital anomaly, and interpregnancy interval.
In the unadjusted model, LARC use was not associated with LBW for LARC quartile 2 compared with 1 (OR = 0.97; 95% CI = 0.83, 1.13; P = .70), for LARC quartile 3 compared with 1 (OR = 0.98; 95% CI = 0.85, 1.13; P = .74), or for LARC quartile 4 compared with 1 (OR = 1.05; 95% CI = 0.92, 1.20; P = .47). There were no significant relationships between LARC use quartile and LBW in the adjusted model (Table 2).
DISCUSSION
Although there is clear evidence of an association between unintended pregnancy and adverse birth outcomes, little has been published regarding the impact of access to family planning services and use of highly effective birth control methods on birth outcomes.2 The Colorado Initiative presents a unique opportunity to evaluate this association. We found that living in a county with a Title X clinic during the Colorado Initiative was protective for PTB. We also found that living in a county with a Title X clinic with the highest degree of LARC use at the peak of the Colorado Initiative was associated with decreased odds of PTB. The effect is strong enough to be seen at the state level—there has been a 12% decrease in the adjusted odds of PTB when we compared 2012 to 2008. We saw none of these statistically significant associations for LBW.
Counties with Title X clinics in Colorado are generally more urban and thus contain a greater proportion of the Colorado population. When one is comparing the demographics of women in counties with and without Title X clinics (Table 1), it is important to note that, despite statistically significant variations between the 2 groups because of the large sample size in the data set, there were very few clinically relevant differences in maternal and infant baseline characteristics between the 2 groups in either 2008 or 2012. In both years, the important population differences between the 2 groups were related to racial/ethnic composition and smoking status. In particular, there was a higher percentage of African American women living in the counties with Title X clinics, and a higher percentage of smokers living in counties without Title X clinics in both 2008 and 2012. Because African American women and women who are smokers are at greater risk for PTB, this dichotomy in baseline population differences is notable; however, we adjusted for both factors in the analysis.
The size and scope of the Colorado Health Information birth data set is a major strength of the study, allowing us to explore the statewide impact of the family planning initiative on adverse birth outcomes. Many of the other effects and outcomes of the Colorado Initiative are also being explored. In particular, when analyzing trends in Colorado before and during the Colorado Initiative, Ricketts et al. reported significant declines in fertility rates and abortion rates among female adolescents and young women aged 15 to 24 years, and in the numbers of infants receiving services through the Special Supplemental Nutrition Program for Women, Infants, and Children.14 However, to our knowledge, this is the first investigation of the impact of the Colorado Initiative on adverse birth outcomes. Unlike much of the data in the birth certificate data set that is self-reported, gestational age and birth weight are objectively measured and have no missing data for the years examined. This allows for validity in calculations of the percentages of PTB and LBW, and in the estimates of the associations between these outcomes and our exposures of interest.
Limitations
There are several limitations of this study. First, our analysis was limited to the existing variables in the data set. Though many common risk factors for adverse birth outcomes and demographic variables were available, there may be additional factors that affect adverse birth outcomes that we were unable to control for in this analysis. A further limitation is that the Colorado birth data set does not collect pregnancy intention information, so it is unknown if the number of unintended pregnancies changed from 2008 to 2012. Our overall hypothesis, and basis for the study, is that in counties with Title X clinics where LARC use increased the most dramatically, we would expect a decrease in the number of unintended pregnancies, resulting in a decrease in adverse birth outcomes such as LBW and PTB. Despite this limitation, many of the characteristics controlled for in this analysis are the very factors thought to be in part responsible for adverse birth outcomes in unintended pregnancies, such as lack of prenatal care and unhealthy maternal behaviors. Even after we controlled for these proxies of unintended pregnancy, significant relationships persisted.
An additional limitation of this study is that, by aggregating LARC use data at the county level, the large variations in LARC use at the individual Title X clinics were washed out. This would bias our estimates toward the null for both PTB and LWB, and could explain why there were no significant associations seen for LBW deliveries. Although this is a limitation in our methodology, if one considers that we identified a significant protective effect on PTB for women living in counties with Title X clinics in 2012, the true effect of the exposure to a county with a Title X clinic in 2012 compared with 2008 may be even more protective.
This study is specifically limited by the ecological nature of the exposures, and it is important to note that other temporal trends could be responsible for the results. Alternative hypotheses as to why the rates of PTB have decreased from 2008 to 2012 include hypothetical temporal changes in the overall health care system, improvements in prenatal care, improvements to the treatment of preterm labor, or increased access to health care in general. One important temporal trend that coincides with the present study period is the adoption of the national quality standard to reduce elective delivery before 39 weeks gestation, supported and promoted by the American College of Obstetricians and Gynecologists, the March of Dimes, and the Joint Commission.25,26 Although each of these alternative hypotheses could be explored further, it has been reported that, despite important medical advances in the past several decades, PTB rates have been on the rise in the United States.27,28 With this in mind, the associations found in this study are notable, and may indicate an impact of the Colorado Initiative on PTB.
Conclusions
Future studies should examine the association between preventing unintended pregnancy and adverse birth outcomes. A similar family planning initiative occurred concurrently in Iowa; therefore, it would be valuable to perform a parallel analysis of the impact of the Iowa Initiative to Reduce Unintended Pregnancy on birth outcomes in that state.
Because of the association found in the present study between LARC use and PTB, increasing LARC uptake at the population level may be an important future direction for public health policy, programming, and research. In particular, our results suggest that providing access to free or affordable highly effective methods of contraception will lead to an overall reduction in rates of PTB. Although the funding provided through the Colorado Initiative ended in 2013, we encourage public health leaders in Colorado and across the United States to provide ongoing advocacy for the support of accessible and affordable family planning services.
Acknowledgments
This study was initiated through the Colorado School of Public Health Research Methods in Epidemiology course. The authors would like to thank the course professors, Dennis Lezotte, PhD, MS, Jill Norris, PhD, MPH, Jan Lowery, PhD, MPH, and Ned Calonge, MD. The authors would also like to thank Kirk Bol, MSPH, and Greta Klingler, MPH, at the Colorado Department of Public Health and Environment for providing access to the data, and Stephanie Teal, MD, MPH, of the University of Colorado School of Medicine Department of Obstetrics and Gynecology for her additional conceptual guidance.
Human Participant Protection
The Colorado Multiple Institutional Review Board approved the study protocol, and determined that it was not human participant research (no. 14-0876).
References
- 1.Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health. 2014;104(suppl 1):S43–S48. doi: 10.2105/AJPH.2013.301416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shah PS, Balkhair T, Ohlsson A, Beyene J, Scott F, Frick C. Intention to become pregnant and low birth weight and preterm birth: a systematic review. Matern Child Health J. 2011;15(2):205–216. doi: 10.1007/s10995-009-0546-2. [DOI] [PubMed] [Google Scholar]
- 3.Mohllajee AP, Curtis KM, Morrow B, Marchbanks PA. Pregnancy intention and its relationship to birth and maternal outcomes. Obstet Gynecol. 2007;109(3):678–686. doi: 10.1097/01.AOG.0000255666.78427.c5. [DOI] [PubMed] [Google Scholar]
- 4.Sable MR, Spencer JC, Stockbauer JW, Schramm WF, Howell V, Herman AA. Pregnancy wantedness and adverse pregnancy outcomes: differences by race and Medicaid status. Fam Plann Perspect. 1997;29(2):76–81. [PubMed] [Google Scholar]
- 5.Kost K, Lindberg L. Pregnancy intentions, maternal behaviors, and infant health: investigating relationships with new measures and propensity score analysis. Demography. 2015;52(1):83–111. doi: 10.1007/s13524-014-0359-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Afable-Munsuz A, Braveman P. Pregnancy intention and preterm birth: differential associations among a diverse population of women. Perspect Sex Reprod Health. 2008;40(2):66–73. doi: 10.1363/4006608. [DOI] [PubMed] [Google Scholar]
- 7.Kost K, Landry DJ, Darroch JE. The effects of pregnancy planning status on birth outcomes and infant care. Fam Plann Perspect. 1998;30(5):223–230. [PubMed] [Google Scholar]
- 8.Pulley L, Klerman LV, Tang H, Baker BA. The extent of pregnancy mistiming and its association with maternal characteristics and behaviors and pregnancy outcomes. Perspect Sex Reprod Health. 2002;34(4):206–211. [PubMed] [Google Scholar]
- 9.D’Angelo D, Williams L, Morrow B et al. Preconception and interconception health status of women who recently gave birth to a live-born infant—Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 26 reporting areas, 2004. MMWR Surveill Summ. 2007;56(10):1–35. [PubMed] [Google Scholar]
- 10.Hellerstedt WL, Pirie PL, Lando HA et al. Differences in preconceptional and prenatal behaviors in women with intended and unintended pregnancies. Am J Public Health. 1998;88(4):663–666. doi: 10.2105/ajph.88.4.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robbins CL, Zapata LB, Farr SL et al. Core state preconception health indicators—pregnancy risk assessment monitoring system and behavioral risk factor surveillance system, 2009. MMWR Surveill Summ. 2014;63(3):1–62. [PubMed] [Google Scholar]
- 12.Healthy People 2020. Washington, DC: US Department of Health and Human Services, Office of Disease Prevention and Health Promotion; Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx. Accessed March 23, 2014. [Google Scholar]
- 13.Centers for Disease Control and Prevention, Division of Reproductive Health. Pregnancy Risk Assessment Monitoring System (PRAMS): CPONDER. 2014. Available at: http://www.cdc.gov/prams/cponder.htm. Accessed November 11, 2014.
- 14.Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014;46(3):125–132. doi: 10.1363/46e1714. [DOI] [PubMed] [Google Scholar]
- 15.ACOG Practice Bulletin No. 121: Long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol. 2011;118(1):184–196. doi: 10.1097/AOG.0b013e318227f05e. [DOI] [PubMed] [Google Scholar]
- 16.Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120(6):1291–1297. doi: 10.1097/aog.0b013e318273eb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stoddard A, McNicholas C, Peipert JF. Efficacy and safety of long-acting reversible contraception. Drugs. 2011;71(8):969–980. doi: 10.2165/11591290-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winner B, Peipert JF, Zhao Q et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366(21):1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]
- 19.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fertil Steril. 2012;98(4):893–897. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trudnak Fowler T, Fairbrother G, Owens P, Garro N, Pellegrini C, Simpson L. Trends in complicated newborn hospital stays and costs, 2002–2009: implications for the future. Medicare Medicaid Res Rev. 2014;4(4):pii. doi: 10.5600/mmrr.004.04.a03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Russell RB, Green NS, Steiner CA et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics. 2007;120(1):e1–e9. doi: 10.1542/peds.2006-2386. [DOI] [PubMed] [Google Scholar]
- 22.Lemons JA, Bauer CR, Oh W et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1995 through December 1996. NICHD Neonatal Research Network. Pediatrics. 2001;107(1):E1. doi: 10.1542/peds.107.1.e1. [DOI] [PubMed] [Google Scholar]
- 23.Blencowe H, Cousens S, Chou D et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013;10(suppl 1):S2. doi: 10.1186/1742-4755-10-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alexander GR, Kotelchuck M. Quantifying the adequacy of prenatal care: a comparison of indices. Public Health Rep. 1996;111(5):408–418. discussion 419. [PMC free article] [PubMed] [Google Scholar]
- 25.ACOG Practice Bulletin No. 107: Induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386–397. doi: 10.1097/AOG.0b013e3181b48ef5. [DOI] [PubMed] [Google Scholar]
- 26.Main EK. New perinatal quality measures from the National Quality Forum, the Joint Commission and the Leapfrog Group. Curr Opin Obstet Gynecol. 2009;21(6):532–540. doi: 10.1097/GCO.0b013e328332d1b0. [DOI] [PubMed] [Google Scholar]
- 27.Muglia LJ, Katz M. The enigma of spontaneous preterm birth. N Engl J Med. 2010;362(6):529–535. doi: 10.1056/NEJMra0904308. [DOI] [PubMed] [Google Scholar]
- 28.Blencowe H, Cousens S, Oestergaard MZ et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379(9832):2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]