Abstract
Objectives. We explored whether collective concerns about the safety, effectiveness, and necessity of influenza vaccines mediate racial/ethnic disparities in vaccine uptake among health care workers (HCWs).
Methods. We used a self-administered Web-based survey to assess race/ethnicity (exposure), concerns about influenza vaccination (mediator; categorized through latent class analysis), and influenza vaccine uptake (outcome) for the 2012 to 2013 influenza season among HCWs at St. Jude Children’s Research Hospital in Memphis, Tennessee. We used mediation analysis to estimate prevalence ratios (PRs) and 95% confidence intervals (CIs) for the total, direct, and indirect effects of race/ethnicity on influenza vaccine uptake.
Results. Non-Hispanic Blacks had lower influenza vaccine uptake than non-Hispanic Whites (total effect: PR = 0.87; 95% CI = 0.75, 0.99), largely mediated by high concern about influenza vaccines (natural indirect effect: PR = 0.89; 95% CI = 0.84, 0.94; controlled direct effect: PR = 0.98; 95% CI = 0.85, 1.1). Hispanic and Asian HCWs had modestly lower uptake than non-Hispanic Whites, also mediated by high concern about influenza vaccines.
Conclusions. Racial/ethnic disparities among HCWs could be attenuated if concerns about the safety, effectiveness, and necessity of influenza vaccines were reduced.
Despite an increase in influenza vaccine uptake among health care workers (HCWs) aged 18 years and older from 64% for the 2010 to 2011 influenza season to 72% for the 2012 to 2013 influenza season,1 vaccine uptake among HCWs in the United States fails to meet the Healthy People 2020 goal of 90%.2 In particular, vaccine uptake historically has been lower among non-Hispanic Blacks and Hispanics than among non-Hispanic Whites not only in the general population but also among HCWs.3–11 For example, an analysis of National Health Interview Survey data for the 2010 to 2011 influenza season suggested that vaccine uptake was 59% among non-Hispanic White HCWs, whereas vaccine uptake was 44% and 45% among non-Hispanic Black and Hispanic HCWs, respectively.5 Nevertheless, little is known about the reasons (i.e., mediators) for racial/ethnic disparities in influenza vaccine uptake among HCWs. A greater understanding of mediators of racial/ethnic disparities in influenza vaccine uptake would provide mechanistic insight on a population level and identify targets for intervention to reduce these disparities, which could ultimately increase overall vaccine coverage among HCWs.
Vaccine-related concerns (e.g., about safety, efficacy, and necessity) have been consistently reported as barriers to influenza vaccine uptake for HCWs as a whole.12–16 For example, HCWs who reported concerns about vaccine safety had between 50% and 78% lower odds of influenza vaccine uptake than HCWs who did not report safety concerns.14 Nevertheless, vaccine-related concerns have not been systematically explored as potential mediators of racial/ethnic disparities among HCWs. Although vaccine-related concerns have been explored as potential mediators of racial/ethnic disparities in influenza vaccine uptake among the general population17,18 and among the elderly,19,20 these studies addressed mediation through approaches that are now known to be misleading.21–26 In addition, concerns about vaccine safety, efficacy, and necessity have conventionally been reported as independent barriers to vaccination. An unobserved attitude or behavior likely underlies these vaccine concerns, and efforts to operationalize this underlying latent construct may yield novel insight about vaccine hesitancy that can facilitate intervention.27 Therefore, we aimed to operationalize the latent construct underlying vaccine concerns, and we used contemporary mediation analysis to address whether these concerns mediate the association between race/ethnicity and influenza vaccine uptake among HCWs in a pediatric comprehensive cancer center where influenza vaccination is offered free of charge to employees and is highly recommended but not mandatory.
METHODS
All employees at St. Jude Children’s Research Hospital in Memphis, Tennessee, effectively qualify as HCWs according to the Centers for Disease Control and Prevention definition.28 Our eligible population thus included all individuals employed at St. Jude for at least 30 days between October 1, 2012, and March 31, 2013 (i.e., the 2012–2013 influenza season). The exclusion of HCWs employed less than 30 days is consistent with the National Healthcare Safety Network guidelines for defining the denominator for estimating influenza vaccine uptake for HCWs during the 2012 to 2013 influenza season.29
Variables
We invited employees by e-mail to participate in a self-administered online survey. We sent the invitations on August 1, 2013, and made the survey available until September 15, 2013. We sent HCWs periodic reminders requesting participation. We ascertained information about influenza vaccine uptake and knowledge and attitudes about the vaccine with standardized questions from national surveys (e.g., the National Health Information Survey), some of which we modified for our setting (Table A, available as a supplement to this article at http://www.ajph.org).
Our outcome of interest was influenza vaccine uptake during the 2012 to 2013 influenza season. Our exposure of interest for this study was self-reported race/ethnicity, categorized as non-Hispanic White, non-Hispanic Black, Hispanic, Asian, or other. Our mediator of interest was concern about the influenza vaccine. The available literature consistently documents 4 concerns about the influenza vaccine among HCWs: (1) the vaccine causes influenza, (2) the vaccine has serious side effects, (3) the vaccine is ineffective, and (4) the vaccine is unnecessary.12–16
Data Analysis
Because the 4 concerns about the influenza vaccine likely manifest from an underlying but unobserved attitude or behavior, we first used exploratory latent class analysis30 to operationalize the unobserved attitude or behavior. Latent class analysis is a model-based statistical method that uses data from observed variables (in our study, the 4 concerns about the influenza vaccine) to distinguish classes of an unobserved (i.e., latent) variable. We specified models with 2 to 4 classes and selected the best-fitting final model according to the Bayesian information criterion, which is a well-established goodness-of-fit criterion that facilitates selection of parsimonious models, where the lowest value is preferred.31 The class with the highest posterior probability from the final model defined class membership for each individual.
We estimated the total, direct, and indirect effects of race/ethnicity on influenza vaccine uptake through established methods for causal mediation analysis in a potential outcome framework.21,25,26,32 The purpose of causal mediation analysis is to explore whether the association between an exposure and an outcome is the result of a direct effect or of an indirect effect through a specified mediator. Figure A (available as a supplement to this article at http://www.ajph.org) illustrates dependency assumptions in a directed acyclic graph for the relation between race/ethnicity and influenza vaccine uptake, where the exposure of interest is race/ethnicity, the mediator of interest is vaccine-related concerns, and the outcome of interest is influenza vaccine uptake.33 We used this directed acyclic graph to specify the causal mediation model, which facilitated decomposition of the total effect (i.e., the combined direct and indirect effects) into separate direct and indirect effects.21,25,26,32
Odds ratios overestimate risk ratios when the outcome is common (i.e., > 10%),34 which can distort interpretations about the magnitude of racial/ethnic disparities.35 Therefore, we used Poisson regression to directly estimate prevalence ratios (PRs) and corresponding 95% confidence intervals (CIs) for total, direct, and indirect effects of race/ethnicity on influenza vaccine uptake, with automated methods for causal mediation analysis by Valeri and Vanderweele.26 We adjusted PRs for age, gender, occupational category (as a proxy for socioeconomic status), and direct patient contact to reduce confounding bias and strengthen identifiability assumptions for valid interpretation of direct and indirect effects.26 We estimated both natural and controlled effects. We derived natural indirect effects from the observed values of the mediator; these provided insight about naturally occurring mediation. We calculated the controlled direct effect from an assigned value for the mediator, providing insight about the exposure–outcome relation if the value of the mediator could be changed through intervention (e.g., reduction of vaccine concerns).21,25
Sensitivity Analysis
We explored the sensitivity of potential misclassification of vaccination status on our estimate for the total effect of race/ethnicity on vaccine uptake. Direct estimates for the sensitivity and specificity of self-reported vaccination status to adjust for misclassification were not available for our population. Therefore, we derived our initial values from a published report about the validity of self-reported vaccination status, which compared self-report with information in an immunization registry.36 From these initial values, we assumed nondifferential misclassification but varied the specificity of self-reported vaccination status more than the sensitivity because for HCWs in our setting, social desirability may motivate greater false-positive than false-negative reporting.37
We computed misclassification-adjusted estimates by the following formula38:
where A is the adjusted count for the racial/ethnic subgroup, A* is the observed count, Fp is the false-positive probability, N is the sample size for the racial/ethnic subgroup, Se is sensitivity, and Sp is specificity. A/N thus estimated the misclassification-adjusted influenza vaccine uptake for each subgroup. We then compared these adjusted vaccine uptakes among racial/ethnic subgroups (i.e., non-Hispanic Black and White HCWs) to estimate misclassification-adjusted PRs.38
RESULTS
The eligible population comprised 3366 HCWs, of whom 2340 (70%) participated in the survey. The exclusion of participants with missing exposure, mediator, or outcome information resulted in a sample of 2003 HCWs (60% of eligible population). Table 1 summarizes the characteristics of the final study population. Briefly, the median age of respondents was 44 years (interquartile range = 35–54 years). The majority of HCWs were female (71%) and non-Hispanic White (72%). The proportion of non-Hispanic Blacks (16%) was comparable to the proportion of Black HCWs in the United States (15%).39 The majority of participants were research (32%) and clinical (physicians, nurses, etc.; 26%) personnel, and 32% of HCWs reported having direct patient contact. Finally, 82% of respondents supported mandatory influenza vaccination.
TABLE 1—
Characteristics of Health Care Workers Who Participated in 2012–2013 Influenza Vaccine Survey: St. Jude Children’s Research Hospital, Memphis, TN
| Characteristic | No. (%)a | Vaccine Uptake, No. (%)b |
| Overall | 2003 | 1742 (87) |
| Age, y | ||
| 18–29 | 187 (9) | 156 (83) |
| 30–39 | 551 (28) | 465 (84) |
| 40–49 | 518 (26) | 449 (87) |
| 50–59 | 513 (26) | 452 (88) |
| ≥ 60 | 234 (12) | 220 (94) |
| Gender | ||
| Female | 1423 (71) | 1243 (87) |
| Male | 580 (29) | 499 (86) |
| Race/ethnicity | ||
| Non-Hispanic White | 1438 (72) | 1293 (90) |
| Non-Hispanic Black | 313 (16) | 241 (77) |
| Hispanic | 40 (2) | 33 (83) |
| Asian | 150 (8) | 122 (81) |
| Other | 62 (3) | 53 (85) |
| Occupational category | ||
| Administrative | 377 (19) | 326 (86) |
| Clinical laboratory | 95 (5) | 84 (88) |
| Clinical (e.g., physician, nurse) | 514 (26) | 495 (96) |
| Support services (e.g., food services, facilities management) | 200 (10) | 174 (87) |
| Research | 645 (32) | 523 (81) |
| Other | 172 (9) | 140 (81) |
| Direct patient contact | ||
| Yes | 645 (32) | 606 (94) |
| No | 1358 (68) | 1136 (84) |
| Support mandatory vaccination | ||
| Yes | 1636 (82) | 1464 (89) |
| No | 227 (11) | 171 (75) |
| Uncertain | 140 (7) | 107 (76) |
Percentage refers to column distribution. For example, 71% women and 29% men for distribution by gender.
Percentage refers to each stratum (row). For example, influenza vaccine uptake among women was 87%.
Table 1 also summarizes overall and subgroup-specific influenza vaccine uptake. Overall, uptake was 87%, with no meaningful variation by gender (87% of women and 86% of men). We observed variation in vaccine uptake by age group, race/ethnicity, occupational category, direct patient contact, and support for mandatory vaccination. Uptake was highest among non-Hispanic White HCWs (90%) and lowest among non-Hispanic Black HCWs (77%). Clinical personnel reported the highest (96%), and research personnel the lowest (81%) uptake. HCWs with direct patient contact reported higher vaccine uptake (94%) than HCWs without direct patient contact (84%). HCWs who supported mandatory vaccination reported higher vaccine uptake (89%) than HCWs who were opposed (75%).
Table B (available as a supplement to this article at http://www.ajph.org) summarizes the goodness-of-fit characteristics of the latent class models used to operationalize the unobserved attitude or behavior that underlay concerns about the influenza vaccine. A 2-class model (high concern and low concern) best fit the underlying attitude or behavior. Table 2 summarizes the conditional probabilities of responses to individual questions about vaccine concerns conditional on membership in each class. We defined the 2 classes as high and low concern because of the relative abundance of concerns about the influenza vaccine in the former class and relatively minimal concerns in the latter. In particular, the high-concern group had a high conditional probability (97%) of reporting concern about vaccine side effects, whereas the low-concern group had a low conditional probability of reporting this concern (11%).
TABLE 2—
Latent Class Analysis Results for Conditional Probabilities for High or Low Concern About Influenza Vaccines Among Health Care Workers Who Participated in 2012–2013 Influenza Vaccine Survey: St. Jude Children’s Research Hospital, Memphis, TN
| Response | High Concern, % | Low Concern, % |
| Vaccine causes influenza | ||
| Yes | 63 | 0.5 |
| No | 37 | 99.5 |
| Concern about side effects | ||
| Yes | 97 | 11 |
| No | 3.5 | 89 |
| Vaccine is ineffective | ||
| Yes | 52 | 3 |
| No | 48 | 97 |
| Vaccine is unnecessary | ||
| Yes | 28 | 2 |
| No | 72 | 98 |
Note. High-concern group, n = 263 (13% of participants); low-concern group, n = 1740 (87% of participants).
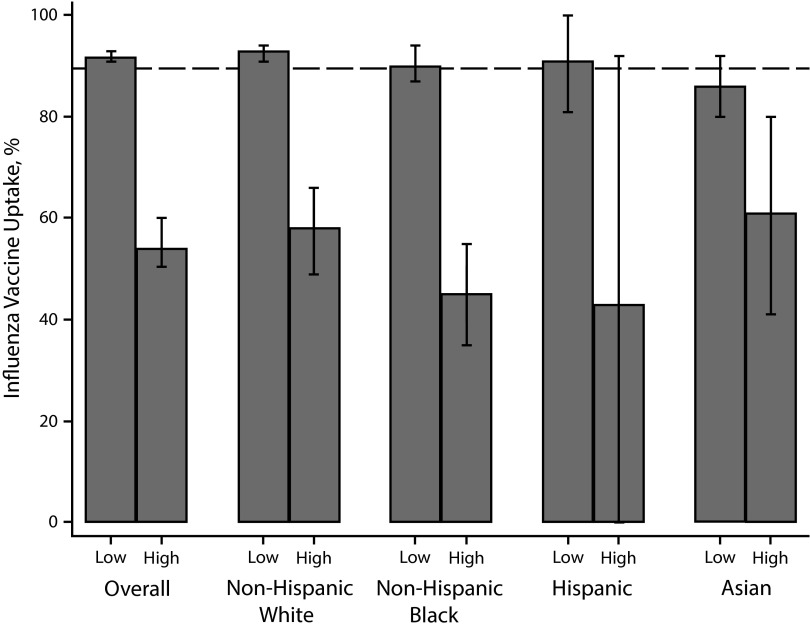
Figure 1 illustrates the overall and race/ethnicity-specific influenza vaccine uptake by level of concerns about the influenza vaccine. The Healthy People 2020 goal of 90% influenza vaccination coverage was satisfied overall and for all racial/ethnic subgroups with low concern about the vaccine except among Asians (87%). The high-concern group of HCWs, overall and broken down into racial/ethnic subgroups, failed to meet the Healthy People 2020 goal; vaccine uptake was below 50% for the high-concern non-Hispanic Black and Hispanic subgroups.
FIGURE 1—
Overall and race/ethnicity-specific influenza vaccine uptake by level of concern about influenza vaccines among health care workers: St. Jude Children’s Research Hospital, Memphis, TN, 2012–2013 influenza season.
Note. Dashed reference line represents the Healthy People 2020 goal of 90% influenza vaccine coverage for health care workers. Error bars represent 95% confidence intervals. Overall: low-concern group, n = 1740; high-concern group, n = 263. Non-Hispanic Whites: low-concern group, n = 1438; high-concern group, n = 120. Non-Hispanic Blacks: low-concern group, n = 220; high-concern group, n = 93. Hispanics: low-concern group, n = 33; high-concern group, n = 7. Asians: low-concern group, n = 122; high-concern group, n = 28.
Table 3 summarizes the total, direct, and indirect effects (mediated by high concern about the influenza vaccine) of race/ethnicity on vaccine uptake among HCWs. Non-Hispanic Blacks had lower influenza vaccine uptake than non-Hispanic Whites (total effect: PR = 0.87; 95% CI = 0.75, 0.99), which was largely mediated by high concern about influenza vaccines (natural indirect effect: PR = 0.89; 95% CI = 0.84, 0.94; controlled direct effect: PR = 0.98; 95% CI = 0.85, 1.1). By contrast, the total effects of Hispanic and Asian race/ethnicity on influenza vaccine uptake among HCWs were more modest, but these modest effects were also mediated by high concern about influenza vaccines (Hispanics, natural indirect effect: PR = 0.95, 95% CI = 0.87, 1.0; controlled direct effect: PR = 1.0, 95% CI = 0.70, 1.4; Asians, natural indirect effect: PR = 0.97; 95% CI = 0.93, 1.0; controlled direct effect: PR = 0.99; 95% CI = 0.81, 1.2).
TABLE 3—
Total, Direct, and Indirect Effects of Race/Ethnicity on Vaccine Uptake Among Health Care Workers Who Participated in 2012–2013 Influenza Vaccine Survey: St. Jude Children’s Research Hospital, Memphis, TN
| Effect Type | Non-Hispanic Blacks,a PR (95% CI) | Hispanics, PR (95% CI) | Asians, PR (95% CI) |
| Total effect | 0.87 (0.75, 0.99) | 0.95 (0.67, 1.35) | 0.97 (0.80, 1.18) |
| Natural direct effect | 0.97 (0.84, 1.13) | 1.00 (0.70, 1.41) | 1.00 (0.82, 1.22) |
| Natural indirect effectb | 0.89 (0.84, 0.94) | 0.95 (0.87, 1.04) | 0.97 (0.93, 1.02) |
| Controlled direct effect | 0.98 (0.85, 1.14) | 1.00 (0.70, 1.45) | 0.99 (0.81, 1.22) |
Note. CI = confidence interval; PR = prevalence ratio.
Prevalence ratio and 95% CIs adjusted for age, gender, and occupation; each racial/ethnic group was compared with non-Hispanic Whites.
Mediated by high concern about influenza vaccines.
Table C (available as a supplement to this article at http://www.ajph.org) summarizes the results of our sensitivity analysis exploring the impact of potential outcome misclassification on estimates for the effect of race/ethnicity on influenza vaccine uptake. The PRs modestly but consistently moved further away from the null with progressively lower sensitivity and specificity. For example, when we used the sensitivity and specificity estimates reported by Irving et al.,36 adjustment for misclassification yielded a 16% relative difference in uptake between non-Hispanic Black and non-Hispanic White HCWs, by contrast to the 13% relative difference in our original estimate.
DISCUSSION
Influenza vaccine uptake in our study population was 87% for the 2012 to 2013 influenza season, but uptake differed by race/ethnicity. In particular, uptake was 13% (95% CI = 1.0%, 25%) lower among non-Hispanic Black than White HCWs. We identified distinct classes of HCWs with high and low concern about influenza vaccines. Our results suggest that high concern about influenza vaccines substantially mediates the association between race/ethnicity and vaccine uptake (i.e., the apparent disparities in uptake may be attributable to high concern about influenza vaccines among racial/ethnic minorities), particularly for non-Hispanic Blacks. Nevertheless, our results suggest that racial/ethnic disparities could be attenuated if high concern about the influenza vaccine were reduced. The resulting increase in vaccine uptake could facilitate meeting the Healthy People 2020 goal of 90% coverage.
Racial/ethnic disparities in influenza vaccine uptake among HCWs have consistently been reported in the literature.3–11 In particular, the relative difference in uptake between non-Hispanic Black and White HCWs reported in studies published between 2002 and 2013 ranges from 25% to 47%.3–10 The 13% relative difference in uptake between non-Hispanic Black and White HCWs that we observed is thus lower than in previous studies, but our attenuated estimate may be attributable to a comprehensive influenza vaccination program at our institution that targets HCWs with direct patient contact and provides vaccination free of charge.40 Our population thus had high vaccine uptake overall and less potential for variation between subgroups. Nevertheless, previous studies did not explore potential mediating factors in the association between race/ethnicity and influenza vaccine uptake. Therefore, our study provides unique information about the mechanism by which race/ethnicity may influence vaccine uptake.
Limitations
The cross-sectional nature of our data introduced ambiguity about the temporal sequence of vaccine concerns (our mediator) and vaccination acceptance. Nevertheless, even longitudinal studies among HCWs may not necessarily be able to distinguish this sequence because concerns about the vaccine and vaccine uptake in previous seasons may precede ever becoming an HCW. Our analysis thus assumed that vaccine concerns occurred prior to vaccination and that the mediator–outcome relation was materially insensitive to unmeasured confounding, but these assumptions were untestable.
As with all studies that use self-reported vaccination status for outcome measurement, our results may have been sensitive to outcome misclassification. We explored the impact of potential misclassification on our comparisons of influenza vaccine uptake among non-Hispanic Black and White HCWs. The results of our sensitivity analysis suggested modest underestimation of the relative difference in uptake between these racial/ethnic subgroups. Nevertheless, we encourage conservative interpretation of these results because the misclassification rate in our HCW population may have differed from the misclassification rate in the general population sample we used to derive sensitivity and specificity estimates. In addition, we assumed a nondifferential misclassification mechanism, but differential misclassification could result in bias toward or away from the null depending on the misclassification rates for each racial/ethnic subgroup. Unfortunately, the overall or race-specific validity of self-reported vaccination status is unknown for HCWs. Future studies should consider either incorporating validation studies or using more accurate measures of vaccination status.
Despite the high participation proportion in our survey even after exclusion of HCWs with missing values for relevant covariates, the estimate of influenza vaccine uptake in our final sample may have been sensitive to bias from nonparticipation. If nonparticipants had lower vaccine uptake, then we may have overestimated overall uptake in the source population (i.e., all eligible HCWs). In addition, we cannot exclude the possibility that our estimates for direct and indirect effects were sensitive to selection bias from nonparticipation. For example, if non-Hispanic Whites (our reference population) with high concern about the influenza vaccine and low vaccine uptake composed a high proportion of nonparticipants, then we might have overestimated the mediating effect of vaccine concerns. We also might have overestimated the mediating effect of vaccine concerns if racial/ethnic minorities with high concern about the influenza vaccine and low uptake composed a high proportion of nonparticipants. Unfortunately, the inherent lack of data about nonparticipants limits our understanding about which scenario prevailed in our population.
Conclusions
Our results suggest that despite high vaccination coverage overall, uptake was still lower for non-Hispanic Black than White HCWs. More importantly, our findings suggest that greater concerns about the safety, effectiveness, and necessity of the influenza vaccine among non-Hispanic Black HCWs mediated this racial/ethnic disparity. Assuming that bias did not appreciably affect the interpretation of our results, the practical value of our study is the identification of a modifiable factor (i.e., vaccine concerns) to target for reducing racial/ethnic disparities in influenza vaccine coverage among HCWs. Interventions to address vaccine concerns may need to be tailored to racial/ethnic groups not only for culturally sensitive content but also for delivery.41 A key component of tailored approaches is the promotion of trust.42 For example, engaging opinion leaders—both within the institution and in the community—who can promote vaccination and provide culturally targeted messaging may aid in reducing racial/ethnic disparities.43 Approaches to promoting trust in different institutions and populations may vary, and thus tailored interventions will require understanding local circumstances.
A mandatory vaccination policy, which is being more widely adopted across health care institutions in the United States,44 may seem to be an appealing solution to racial/ethnic disparities because it applies to all racial/ethnic groups of HCWs. Nevertheless, mandatory vaccination is controversial and does not address the fundamental issues underlying vaccine hesitancy. Furthermore, no studies have addressed whether mandatory vaccination improves actual clinical outcomes.45 Consequently, addressing vaccine concerns should be a continued focus even at institutions that adopt a mandatory vaccination policy.46
Finally, HCWs are often viewed as an isolated group, which is an inadequate sociocultural perspective for understanding barriers to vaccination. Multilevel perspectives such as the socioecological model of health promotion recognize that individuals cluster in social networks and that social networks cluster in communities.47 This model has been used to better understand the context of barriers to vaccination and propose multilevel interventions.48 Future studies should explore multilevel perspectives to better understand how sociocultural phenomena affect racial/ethnic disparities in influenza vaccine uptake among HCWs.
Acknowledgments
This work was supported by the American Lebanese Syrian Associated Charities.
We are grateful to Nina Tinner and Chris Vukodinovich for assistance with data collection.
Note. The funding source was not involved in the study design, data collection, analysis, interpretation, writing, or decision to submit this article.
Human Participant Protection
This study was assessed by the St. Jude Children’s Research Hospital institutional review board and considered exempt from oversight because of an anonymous survey procedure that precluded identification of participants in any way.
References
- 1.Centers for Disease Control and Prevention. Influenza vaccination coverage among health-care personnel—United States, 2012–13 influenza season. MMWR Morb Mortal Wkly Rep. 2013;62(38):781–786. [PMC free article] [PubMed] [Google Scholar]
- 2.Healthy People 2020: Immunization and Infectious Diseases. Washington, DC: US Dept of Health and Human Services; 2010. [Google Scholar]
- 3.Ludwig-Beymer P, Gerc SC. An influenza prevention campaign: the employee perspective. J Nurs Care Qual. 2002;16:1–12. doi: 10.1097/00001786-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Lu PJ, Ding H, Black CL. H1N1 and seasonal influenza vaccination of US healthcare personnel, 2010. Am J Prev Med. 2012;43(3):282–292. doi: 10.1016/j.amepre.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu PJ, Singleton JA, Euler GL, Williams WW, Bridges CB. Seasonal influenza vaccination coverage among adult populations in the United States, 2005–2011. Am J Epidemiol. 2013;178(9):1478–1487. doi: 10.1093/aje/kwt158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nowalk MP, Lin CJ, Zimmerman RK et al. Self-reported influenza vaccination rates among health care workers in a large health system. Am J Infect Control. 2008;36(8):574–581. doi: 10.1016/j.ajic.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Lu P, Bridges CB, Euler GL, Singleton JA. Influenza vaccination of recommended adult populations, U.S., 1989–2005. Vaccine. 2008;26(14):1786–1793. doi: 10.1016/j.vaccine.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 8.King WD, Woolhandler SJ, Brown AF et al. Brief report: influenza vaccination and health care workers in the United States. J Gen Intern Med. 2006;21(2):181–184. doi: 10.1111/j.1525-1497.2006.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walker FJ, Singleton JA, Lu P, Wooten KG, Strikas RA. Influenza vaccination of healthcare workers in the United States, 1989–2002. Infect Control Hosp Epidemiol. 2006;27(3):257–265. doi: 10.1086/501538. [DOI] [PubMed] [Google Scholar]
- 10.Caban-Martinez AJ, Arlinghaus A, Reme SE. Correlates of seasonal flu vaccination among U.S. home health aides. Vaccine. 2013;31(2):287–290. doi: 10.1016/j.vaccine.2012.10.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu PJ, O’Halloran A, Bryan L et al. Trends in racial/ethnic disparities in influenza vaccination coverage among adults during the 2007–08 through 2011–12 seasons. Am J Infect Control. 2014;42(7):763–769. doi: 10.1016/j.ajic.2014.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Talbot TR, Talbot HK. Influenza prevention update: examining common arguments against influenza vaccination. JAMA. 2013;309:881–882. doi: 10.1001/jama.2013.453. [DOI] [PubMed] [Google Scholar]
- 13.Vasilevska M, Ku J, Fisman DN. Factors associated with healthcare worker acceptance of vaccination: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2014;35(6):699–708. doi: 10.1086/676427. [DOI] [PubMed] [Google Scholar]
- 14.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals—a review of studies on attitudes and predictors. Vaccine. 2009;27(30):3935–3944. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 15.Bellia C, Setbon M, Zylberman P, Flahault A. Healthcare worker compliance with seasonal and pandemic influenza vaccination. Influenza Other Respir Viruses. 2013;7(suppl 2):97–104. doi: 10.1111/irv.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hofmann F, Ferracin C, Marsh G, Dumas R. Influenza vaccination of healthcare workers: a literature review of attitudes and beliefs. Infection. 2006;34(3):142–147. doi: 10.1007/s15010-006-5109-5. [DOI] [PubMed] [Google Scholar]
- 17.Lindley MC, Wortley PM, Winston CA, Bardenheier BH. The role of attitudes in understanding disparities in adult influenza vaccination. Am J Prev Med. 2006;31(4):281–285. doi: 10.1016/j.amepre.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 18.Marin MG, Johanson WG, Jr, Salas-Lopez D. Influenza vaccination among minority populations in the United States. Prev Med. 2002;34(2):235–241. doi: 10.1006/pmed.2001.0983. [DOI] [PubMed] [Google Scholar]
- 19.Hebert PL, Frick KD, Kane RL, McBean AM. The causes of racial and ethnic differences in influenza vaccination rates among elderly Medicare beneficiaries. Health Serv Res. 2005;40(2):517–537. doi: 10.1111/j.1475-6773.2005.00370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rangel MC, Shoenbach VJ, Weigle KA, Hogan VK, Strauss RP, Bangdiwala SI. Racial and ethnic disparities in influenza vaccination among elderly adults. J Gen Intern Med. 2005;20(5):426–431. doi: 10.1111/j.1525-1497.2005.0097.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pearl J. The causal mediation formula—a guide to the assessment of pathways and mechanisms. Prev Sci. 2012;13(4):426–436. doi: 10.1007/s11121-011-0270-1. [DOI] [PubMed] [Google Scholar]
- 22.Robins JM, Greenland S. Identifiability and exchangeability for direct and indirect effects. Epidemiology. 1992;3(2):143–155. doi: 10.1097/00001648-199203000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Cole SR, Hernan MA. Fallibility in estimating direct effects. Int J Epidemiol. 2002;31(1):163–165. doi: 10.1093/ije/31.1.163. [DOI] [PubMed] [Google Scholar]
- 24.Kaufman JS, Maclehose RF, Kaufman S. A further critique of the analytic strategy of adjusting for covariates to identify biologic mediation. Epidemiol Perspect Innov. 2004;1(1):4. doi: 10.1186/1742-5573-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hafeman DM, Schwartz S. Opening the Black Box: a motivation for the assessment of mediation. Int J Epidemiol. 2009;38(3):838–845. doi: 10.1093/ije/dyn372. [DOI] [PubMed] [Google Scholar]
- 26.Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137–150. doi: 10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Influenza vaccination information for healthcare workers. Available at: http://www.cdc.gov/flu/healthcareworkers.htm. Accessed July 11, 2013.
- 29.Centers for Disease Control and Prevention, National Healthcare Safety Network. Healthcare personnel (HCP) influenza vaccination summary reporting in NHSN. Available at: http://www.cdc.gov/nhsn/faqs/FAQ-Influenza-Vaccination-Summary-Reporting.html. Accessed May 12, 2014.
- 30.McCutcheon AL. Latent Class Analysis. Newbury Park, CA: Sage Publications; 1987. [Google Scholar]
- 31.Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–464. [Google Scholar]
- 32.VanderWeele TJ. A three-way decomposition of a total effect into direct, indirect, and interactive effects. Epidemiology. 2013;24(2):224–232. doi: 10.1097/EDE.0b013e318281a64e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48. [PubMed] [Google Scholar]
- 34.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160(4):301–305. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- 35.Schwartz LM, Woloshin S, Welch HG. Misunderstandings about the effects of race and sex on physicians’ referrals for cardiac catheterization. N Engl J Med. 1999;341(4):279–283. doi: 10.1056/NEJM199907223410411. discussion 286–287. [DOI] [PubMed] [Google Scholar]
- 36.Irving SA, Donahue JG, Shay DK, Ellis-Coyle TL, Belongia EA. Evaluation of self-reported and registry-based influenza vaccination status in a Wisconsin cohort. Vaccine. 2009;27(47):6546–6549. doi: 10.1016/j.vaccine.2009.08.050. [DOI] [PubMed] [Google Scholar]
- 37.Godin G, Vézina-Im LA, Naccache H. Determinants of influenza vaccination among healthcare workers. Infect Control Hosp Epidemiol. 2010;31(7):689–693. doi: 10.1086/653614. [DOI] [PubMed] [Google Scholar]
- 38.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 39.Bureau of Labor Statistics. Labor force statistics from the Current Population Survey. Available at: http://www.bls.gov/cps/cpsaat18.htm. Accessed March 6, 2015.
- 40.McCullers JA, Speck KM, Williams BF, Liang H, Mirro J., Jr Increased influenza vaccination of healthcare workers at a pediatric cancer hospital: results of a comprehensive influenza vaccination campaign. Infect Control Hosp Epidemiol. 2006;27(1):77–79. doi: 10.1086/500003. [DOI] [PubMed] [Google Scholar]
- 41.Cooper LA, Hill MN, Powe NR. Designing and evaluating interventions to eliminate racial and ethnic disparities in health care. J Gen Intern Med. 2002;17(6):477–486. doi: 10.1046/j.1525-1497.2002.10633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fiscella K. Commentary—anatomy of racial disparity in influenza vaccination. Health Serv Res. 2005;40(2):539–549. doi: 10.1111/j.1475-6773.2005.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Valente TW, Pumpuang P. Identifying opinion leaders to promote behavior change. Health Educ Behav. 2007;34(6):881–896. doi: 10.1177/1090198106297855. [DOI] [PubMed] [Google Scholar]
- 44.Miller BL, Ahmed F, Lindley MC, Wortley PM. Increases in vaccination coverage of healthcare personnel following institutional requirements for influenza vaccination: a national survey of U.S. hospitals. Vaccine. 2011;29(50):9398–9403. doi: 10.1016/j.vaccine.2011.09.047. [DOI] [PubMed] [Google Scholar]
- 45.Pitts SI, Maruthur NM, Millar KR, Perl TM, Segal J. A systematic review of mandatory influenza vaccination in healthcare personnel. Am J Prev Med. 2014;47(3):330–340. doi: 10.1016/j.amepre.2014.05.035. [DOI] [PubMed] [Google Scholar]
- 46.Awali RA, Samuel PS, Marwaha B et al. Understanding health care personnel’s attitudes toward mandatory influenza vaccination. Am J Infect Control. 2014;42(6):649–652. doi: 10.1016/j.ajic.2014.02.025. [DOI] [PubMed] [Google Scholar]
- 47.Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: John Wiley & Sons; 2008. [Google Scholar]
- 48.Kumar S, Quinn SC, Kim KH, Musa D, Hilyard KM, Freimuth VS. The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Educ Behav. 2012;39(2):229–243. doi: 10.1177/1090198111415105. [DOI] [PMC free article] [PubMed] [Google Scholar]