Abstract
Objectives. We piloted a monitoring mechanism to document police encounters around programs targeting people who inject drugs (PWID), and assessed their demographic predictors at 2 Baltimore, Maryland, needle exchange program (NEP) sites.
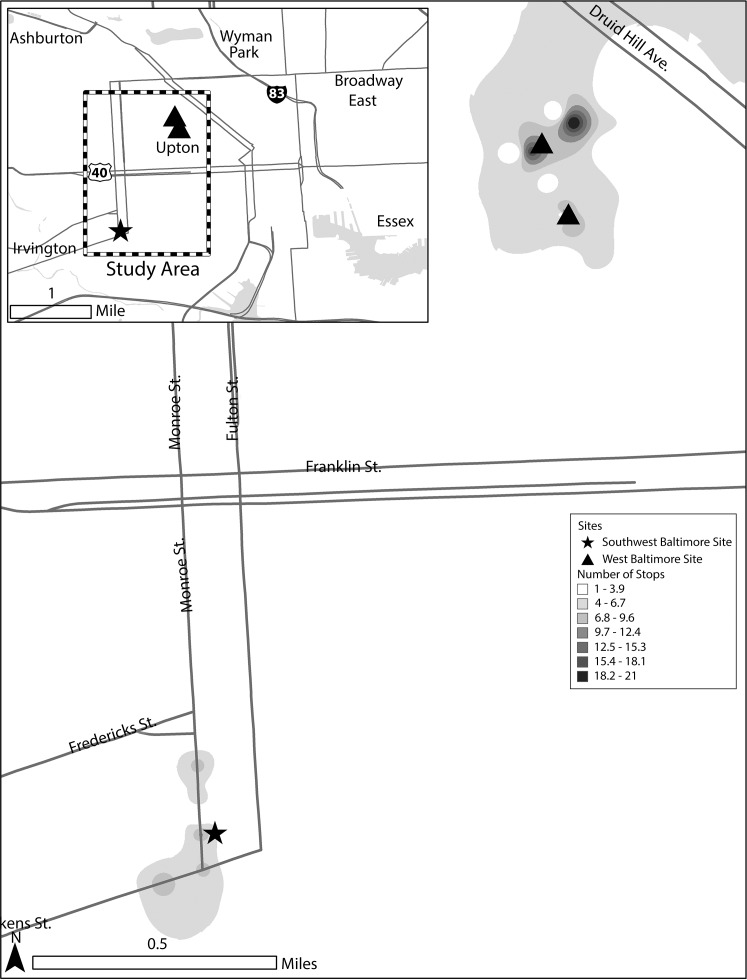
Methods. In a brief survey, 308 clients quantified, characterized, and sited recent police encounters. Multivariate linear regression determined encounter predictors, and we used geocoordinate maps to illustrate clusters.
Results. Within the past 6 months, clients reported a median of 3 stops near NEP sites (interquartile range [IQR] = 0–7.5) and a median of 1 arrest in any location (IQR = 0–2). Three respondents reported police referral to the NEP. Being younger (P = .009), being male (P = .033), and making frequent NEP visits (P = .02) were associated with reported police stops. Among clients reporting arrest or citation for syringe possession, Whites were significantly less likely than non-Whites to report being en route to or from an NEP (P < .001). Reported encounters were clustered around NEPs.
Conclusions. Systematic surveillance of structural determinants of health for PWID proved feasible when integrated into service activities. Improved monitoring is critical to informing interventions to align policing with public health, especially among groups subject to disproportionate levels of drug law enforcement.
Laws and policing practices are broadly understood to act as structural determinants of health for people who inject drugs (PWID). In many US jurisdictions, laws have historically prevented over-the-counter sale and possession of syringes, reflecting a theory that legal restrictions on access to clean injection equipment can deter drug abuse.1 Other policies have banned federal, state, and municipal appropriations for needle exchange programs (NEPs), vastly underresourcing these public health initiatives and facilitating infectious disease spread among PWID and across communities.1,2 Possession of injecting equipment is generally a crime under state laws prohibiting drug paraphernalia, authorizing syringe confiscation and arrest of PWID by street-level law enforcement officers.3
In the past 2 decades, an extensive evidence base demonstrating NEPs to be both efficacious in reducing the transmission of infectious disease (such as HIV and HCV) and cost-effective without increasing drug abuse3a has helped shift the US policy environment relating to syringe access. To date, 28 states have established regulation of retail sale and possession of syringes; NEPs have received official authorization in at least 18 states, sometimes only in the context of a public health emergency.3 Elsewhere, NEP clients gained formal or informal exemption from drug paraphernalia laws to encourage program use.4 These shifts have occurred in the context of other drug policy reforms that have begun the process of aligning the criminal justice regime with sound public health science.5,6
There is considerable evidence, however, that policy reform is in and of itself insufficient to align police practices with public health prevention efforts in the realm of substance abuse.7–10 Wide enforcement discretion, management failures, and other gaps in the policy implementation process10 leave room for police officers to continue to confiscate legal injection equipment and interfere with the functioning of NEPs even after legal sanction.9,11,12
Even under a favorable policy regime, policing practices can adversely affect the behavior and health of PWID. A number of studies from the United States and elsewhere suggest that police encounters are associated with higher odds of HIV infection, drug overdose, and other deleterious outcomes among PWID.10,13–25 Extrajudicial police practices such as unauthorized confiscation of injection equipment and physical abuse are widespread and have shown especially robust associations with risk behavior and adverse health outcomes among PWID, including HIV seroconversion.14,23,26–37 In a national survey of NEPs in the United States, 43% reported that their clients experience police harassment on at least a monthly basis.8 Aside from direct police interference with NEP program operations,10,18–21,25 experience and perceptions of police practices can deter uptake of disease prevention services by PWID.13–17,38–40 Disproportionate police presence in communities of color and racially biased policing practices likely exacerbate racial disparities in HIV acquisition and other health outcomes.13–17,38
Although police interference has been sporadically documented and linked to risky injection behaviors among PWID populations, little research has attempted to evaluate mechanisms for systematically measuring the extent or prevalence of these adverse interactions. According to our previous research, only a small minority of NEPs in the United States report consistently monitoring adverse events involving police and program clients or staff.8 To our knowledge, those programs that do have a system for documenting police encounters have not formally described their methods or analyzed their findings. We piloted and evaluated a surveillance system to document levels of reported police interaction with NEP clients in an urban setting of Baltimore, Maryland. In light of the racially charged nature of drug law enforcement,41–44 our hypothesis was that non-White NEP clients would report higher levels of police encounters than White clients.
METHODS
With an estimated population of more than 40 000 PWID, Baltimore has some of the highest rates of heroin use, injection drug use, and injection-attributable HIV and HCV in the United States.45–49 During the relevant period, Baltimore City reported approximately 20 000 drug-related arrests per year—what translates to the highest rate in the state.50 African Americans, who make up an overall majority (64%) of Baltimore’s population, are nonetheless overrepresented among the city’s residents involved in the criminal justice system, as well as those affected by HIV and HCV.50,51,52 Over the years, the state of Maryland has introduced policy interventions designed to curb drug addiction, scale up substance use treatment, and reduce drug-related harms. In the realm of syringe access, Maryland’s legislature created the Baltimore City Needle Exchange Program in 1994, including special immunity from drug paraphernalia laws for NEP clients and employees.3a,53
For almost 2 decades, the Baltimore City Health Department has implemented the NEP by operating retrofitted camper vans on a 1-for-1 exchange model. These mobile exchange points make scheduled stops at sites throughout city neighborhoods most affected by the injection drug use and infectious disease syndemic.51 In 2010, the program serviced 2346 unique clients through its 17 sites.51 An interagency agreement with the Baltimore City Health Department requires the Baltimore Police Department to instruct its officers to maintain a discretionary zone or reduced police activity around NEP vans during program hours, and under state law, clients carrying NEP participant identification cards are protected from criminal liability for possession or distribution of paraphernalia when traveling to and from the exchange sites.3a
Building on research from other jurisdictions demonstrating that police officers may not be fully informed about public health–oriented criminal justice reforms targeting drug users7,9 and anecdotal reports of persistent police presence around the Baltimore NEP sites, we piloted a surveillance mechanism to understand the prevalence, location, and characteristics of reported police encounters among Baltimore NEP clients.
We developed an 11-item interviewer-administered client experience survey. The instrument assessed basic respondent characteristics plausibly associated with reported police encounters, including demographics (e.g., age, gender, race), drug use risk behaviors (e.g., age at initiation of injection drug use), and history of NEP use. The instrument also prompted respondents for an estimated number of times they experienced specific police encounters over the previous 6-month period, including number of times stopped in the neighborhood (the 2- to 3-block radius) of the NEP during program hours, number of times arrested or detained by police, number of times cited specifically for possession of injection equipment, and number of times police referred or accompanied them to the NEP. For each category of encounter, clients with nonzero responses were asked to approximate the cross streets of their most recent reported encounter in that category. Survey participation was voluntary and anonymous.
To maximize age and ethnic diversity, we chose 2 NEP sites for this pilot: 1 in Southwest Baltimore, serving a diverse population that includes a large proportion of White users, and 1 in West Baltimore, serving primarily African Americans. The pilot ran between March 2010 and May 2012. All clients who visited either site during the study period were eligible, but participation was limited to 1 set of responses per client. Using a prepared script, study staff and volunteers recruited clients meeting eligibility criteria (no previous participation) and offered them a $10 incentive in the form of a gift card to a local pharmacy and grocery store.
We conducted analyses with Stata version 10 (StataCorp LP, College Station, TX) to understand the prevalence and correlates of reported client interactions with police. For the police stop variable, we built a linear regression model to determine predictors of reported police encounters in the vicinity of the NEP. We used the Pearson χ2 test to compare differences between the responses of White and non-White clients with regard to the demographic characteristics of gender, age, parole or probation status, and NEP visit history. We used a t test to determine whether the mean age at first injection differed by race. By using a backward elimination procedure, we retained covariates that changed the main exposure coefficient by greater than 10% in the final multiple linear regression model.54
We used the Pearson’s χ2 test to compare White and non-White respondent groups with regard to reported police encounters (past 6 months) dichotomized around the median: proportion reportedly stopped by police 4 or more times near the NEP site, proportion reportedly arrested or detained 4 or more times regardless of location, proportion reportedly arrested or cited for possession of syringes going to or from the NEP site, and proportion who reportedly had injection equipment confiscated or destroyed by police.
Finally, we used the geocoordinates gathered for the most recent reported police encounter in each category to create maps of “hotspots,” illustrating the geographical concentration of clients’ reported police encounters around the 2 NEP sites.
RESULTS
Demographics are displayed in Table 1. By design, the sample (n = 308) participants were approximately split between the 2 sites (55% at the West Baltimore and 45% at the Southwest Baltimore site) and White and non-White NEP clients (40% and 60%, respectively). The sample was 75% male, with a median age of 35 years. The median age at first injection was 20 years, and 21% reported being on parole or probation. Participants reported visiting the NEP a median of 12 times (interquartile range [IQR] = 3–26) in the preceding 6 months. We found significant differences between the White and non-White sample with regard to both gender and age (Table 1).
TABLE 1—
Respondent Demographic Characteristics Among Needle Exchange Clients by Race: Baltimore, MD, 2010–2012
| Characteristic | White, No. (%) or Mean ±SD | Non-White, No. (%) or Mean ±SD | Total No. (%) or Mean ±SD | Pa |
| Total | 123 (39.94) | 185 (60.06) | 308 (100) | |
| Gender | < .001 | |||
| Female | 50 (40.65) | 25 (13.51) | 75 (24.35) | |
| Male | 72 (58.53) | 157 (84.86) | 229 (74.35) | |
| Age, y | < .001 | |||
| ≤ 34 | 62 (50.41) | 6 (3.24) | 68 (22.08) | |
| > 34 | 61 (49.59) | 179 (96.76) | 240 (77.92) | |
| On parole or probation | .193 | |||
| Yes | 30 (24.39) | 34 (18.37) | 64 (20.78) | |
| No | 91 (73.98) | 149 (80.54) | 240 (77.92) | |
| Age 1st injected drugs, y | 22.72 ±7.24 | 22.78 ±8.56 | 22.76 ±8.05 | .477 |
| Visits to this NEP site during past 6 mob | .021 | |||
| > 13 | 73 (59.35) | 85 (45.95) | 158 (51.30) | |
| ≤ 13 | 50 (40.65) | 100 (54.05) | 150 (48.70) |
Note. NEP = needle exchange program. The sample size was n = 308 clients.
P values between White and non-White participants were determined according by Pearson χ2 test or (in the case of mean age of first injection drug use) t test.
Response values for items measuring visits to the needle exchange program site were capped at 78 (West Baltimore) and 104 (Southwest Baltimore), the maximum number of times the needle exchange program operates at those sites during a 6-month period.
Table 2 displays the frequency of White and non-White NEP clients’ reported police interactions during the preceding 6 months, including frequency of reported police stops near the NEP site, arrests or citations specifically for possession of injecting equipment, police confiscation or destruction of injecting equipment, arrest or detention at any location, and police referrals to the NEP. Within the past 6 months, clients reported a median of 3 stops near the pilot NEP sites during program hours (IQR = 0–7.5) and a median of 1 arrest in any location (IQR = 0–2). Three respondents (< 1%) reported being referred to the NEP by police officers over that time period.
TABLE 2—
Needle Exchange Program Clients’ Encounters With Police During the Past 6 Months by Race: Baltimore, MD, 2010–2012
| Variable | White, No. (%) | Non-White, No. (%) | Total No. (%) | Pa |
| Total | 123 (39.94) | 185 (60.06) | 308 (100) | |
| Times stopped by police near this NEP site during operating hours | .793 | |||
| 0 | 30 (24.39) | 48 (25.95) | 78 (25.32) | |
| 1–3 | 39 (31.71) | 52 (28.11) | 91 (29.55) | |
| ≥ 4 | 54 (43.90) | 85 (45.95) | 139 (45.13) | |
| Times arrested or detained (any charge or location) | .466 | |||
| 0 | 60 (48.78) | 82 (44.32) | 142 (46.10) | |
| 1–3 | 53 (43.09) | 92 (44.73) | 145 (47.08) | |
| ≥ 4 | 10 (8.13) | 11 (5.95) | 21 (6.82) | |
| If ever arrested or cited, times specifically for injection equipment while going to or from NEP site | < .001 | |||
| 0 | 17 (58.62) | 8 (18.18) | 25 (34.25) | |
| 1–3 | 9 (31.03) | 35 (79.55) | 44 (60.27) | |
| ≥ 4 | 3 (10.34) | 1 (2.27) | 4 (5.48) | |
| Times police took, confiscated, or destroyed injection equipment without arrest or citation | .796 | |||
| 0 | 67 (54.47) | 93 (50.27) | 160 (51.94) | |
| 1–3 | 37 (30.08) | 60 (32.61) | 97 (31.60) | |
| ≥ 4 | 19 (15.45) | 31 (16.85) | 50 (16.29) | |
| Times referred to NEP by police | .811 | |||
| 0 | 122 (99.19) | 182 (98.91) | 304 (98.70) | |
| 1 | 1 (0.81) | 2 (1.09) | 3 (0.97) |
Note. NEP = needle exchange program. The sample size was n = 308 clients.
P values between White and non-White participants were determined by Pearson χ2 test.
Of the clients (n = 73) who reported having been arrested or cited specifically for possession of injection equipment, 68% reported that the encounters took place while the client was going to or from the exchange site. Non-Whites were more likely than Whites to report being on their way to or from an NEP site at the time they received such an arrest or citation (82% vs 41%, respectively; Table 2).
In a multivariate model, being younger and attending the NEP site more frequently was associated with increased report of police stops in the vicinity of the NEP sites, controlling for NEP site. Male clients reported experiencing almost 5 more stops on average than female clients. (Table 3).
TABLE 3—
Summary of Linear Regression Predicting Number of Police Stops Near Needle Exchange Program Site: Baltimore, MD, 2010–2012
| Model 1 (n = 303)a |
Model 2 (n = 303)b |
|||||
| Variable | B (95% CI) | SE | P | B (95% CI) | SE | P |
| Age | −0.238 (–0.418, 0.059) | 0.091 | .009 | −0.259 (–0.465, 0.052) | 0.105 | .014 |
| Gender: male | 5.020 (0.397, 9.642) | 2.349 | .033 | 4.946 (0.302, 9.591) | 2.360 | .037 |
| NEP visits | 0.098 (0.0158, 0.180) | 0.042 | .02 | 0.096 (0.013, 0.178) | 0.042 | .024 |
| NEP site | −0.902 (–5.464, 3.660) | 2.318 | .698 | |||
| Constant | 13.601 (5.864, 21.339) | 3.932 | .001 | 15.922 (1.857, 29.987) | 7.147 | .698 |
Note. CI = confidence interval; NEP = needle exchange program.
R2 = 0.0400; adjusted R2 = 0.0304; F = 4.15.
R2 = 0.0405; adjusted R2 = 0.0276; F = 3.14.
Heat maps representing reported police stops and syringe confiscation (Figure 1) provide visual representations of the high levels of police–NEP client interactions, vividly illustrating the structural environment created by policing practices around NEP operations at our pilot sites. They may also document apparent confusion about the interagency agreements designating areas of NEP activity for reduced engagement (i.e., visibility and enforcement intensity) by Baltimore City Police Department officers. A comparison between the 2 areas reveals reported police activity to be particularly concentrated around the West Baltimore NEP site, although the vicinity of the Southwest Baltimore site saw a slightly higher mean number of reported stops (9.17, compared with 8.48 at West Baltimore).
FIGURE 1—
Police encounter locations reported by needle exchange clients: Baltimore, MD, 2010–2012.
DISCUSSION
This study’s pilot surveillance system revealed that NEP clients in Baltimore continue to experience adverse police encounters related to use of NEP services and possession of clean injecting equipment. Clients in the sample reported a median of 3 police stops in and around 2 NEP sites, and non-White clients were more likely to report arrest or confiscation of injecting equipment while traveling to or from the NEP site. Clients who were younger, male, and more frequent users of the NEP were more likely to report police encounters in the programs' vicinity.
By quantifying the prevalence and nature of NEP clients’ interactions with Baltimore police, the results refine our understanding of who, among the city’s NEP client population, is more likely to experience stops, arrest, detention, and confiscation of injection equipment by police. We also identified geographic “hotspots,” indicating where adverse PWID interactions with police are occurring. Collection of this information will help to develop targeted strategies to ensure full implementation and access to NEP services, and will inform collaborative programs with law enforcement to reduce policing barriers to syringe access.
Our data suggest that active clients are also more likely to report experiencing adverse police interactions than those who visit the NEP less regularly. To the extent that this may reflect law enforcement practices that target NEP clients, geospatial surveillance is an important additional tool to help identify and address those police practices through better management, training, and service coordination. Eliminating policing as a barrier to accessing critical public health services facing the neediest segment of the PWID population is critical to the full uptake and impact of NEPs.
Nationally, individuals aged 25 to 34 years account for the largest proportion of new HIV infections, with African Americans being disproportionally affected.55 There have also been recent reports of quickly rising incidence of heroin injection and HCV infection among young people transitioning from prescription drug abuse.56,57 Nonetheless, PWID in this age category are underrepresented in both our sample and the population served by Baltimore City Health Department’s risk reduction services.
This context makes our finding that younger male NEP clients are more likely to report being stopped by police that much more salient. It is perhaps unsurprising, given that youth is generally associated with higher rates of criminal justice involvement and has been theorized to be subject to increased police surveillance.58–60 This level of reported interaction with police may also reflect the fact that a substantial proportion of our sample was under parole or probation supervision. If police encounters are understood to be collateral to NEP access, young male injection drug users may instead choose to visit the NEP less frequently, or not at all, increasing their risk of unsafe injection. Strategic collaboration with law enforcement offers the chance to enhance access to NEP services among young male PWID at high risk for infectious disease transmission.61
To ensure that syringe access laws are properly implemented, better and more systematic surveillance of police interactions with PWID is needed.9,62,63 Drug users in Baltimore City and around the world report that their experiences of and perceptions regarding police activity have a direct impact on decisions related to the manner, location, and timing of drug consumption, which in turn determine the relative risk or safety of drug use.16,31,37,39,64–66 Existing data make clear that without ongoing efforts to ensure that policing practices align with legal reforms permitting syringe possession, PWID may continue to experience extrajudicial syringe confiscation, detention, and other adverse encounters.8,64 Our findings add important new evidence to a body of research on this critical and underexamined element of the PWID risk environment, highlighting the racial gradients in such encounters.
Documentation of adverse police interaction is required for NEPs to continue offering effective syringe access and prevention services. Our findings expose a misalignment between formal law and stated police policy on the one hand and practice on the other. This is consistent with previous studies identifying gaps in the implementation of syringe access laws and policies.9,10 In view of experience from other jurisdictions, these findings illustrate the need for more robust policing policies7; improved education, management, and incentive structures for front-line officers67; improved communication between police and public health professionals working with vulnerable groups61,68; and better client knowledge of legal rights to access risk reduction services.68 Surveillance data of the kind collected in this study is vital for informing all of these programmatic elements, while also echoing broader calls for increased transparency, accountability, and bias-free policing. Such calls have gained additional urgency in the context of the recent unrest linked to fraught community–police relations in Baltimore and elsewhere.
Limitations
Our findings are limited in that they document correlations and cannot prove causation. The respondent client population is a convenience sample and may not be representative of the overall NEP clientele or the overall PWID population in Baltimore. In some cases, respondents reported numbers of encounters beyond possible figures, resulting in this variable’s value being capped at the maximum number of days the NEP site was in operation during a 6-month period. All data, including police encounter data, were based on self-report, and could not be externally validated.
Interruptions in data collection because of staffing and funding shortages extended the study period over 20 months and challenged a “snapshot” cross-sectional design. Although a number of additional domains of inquiry (e.g., drug use dynamics) could ideally also inform our understanding of factors associated with adverse police encounters, the limited scope of the project required us to make tough choices to accommodate the time, space, and resource constraints. Despite these limitations, our findings reveal significant and sustained levels of reported police activity in the vicinity of the Baltimore NEPs, with disproportionate impact on non-White and younger injectors.
Conclusions
This pilot surveillance effort yielded important programmatic lessons. Both domestically and internationally, staff at agencies serving drug users and other criminalized groups should anticipate a “learning curve” for local police after a change in law takes effect.64 Trainings should be used to inform new recruits and veteran officers to changes in the law and standard operating procedures, along with broader information about the function, rationale, and occupational and public health benefits of public health services targeting people with addiction problems. Analogous police trainings have been used elsewhere, with positive results.63,68–71 Protocols to assist clients after they report an adverse interaction should be put in place.
Used periodically to assess the frequency and character of adverse police interaction among NEP clients, some version of the instrument used in this project can serve as a tool for improved coordination and communication with law enforcement. Incorporating this tool into an NEP program can equip program administrators with real-time data on the extent of adverse—or positive—police interactions among their client base. These data can also help assess efforts to improve operational coordination between police social service, drug treatment, and other agencies working with PWID, including service referrals.61 Geospatial surveillance can help bridge public health efforts to police management tools such as Compstat, which uses crime data to inform deployment decisions. These data can be used to inform policy, training, and other interventions to better align police practices with public health goals.7,62,63
Acknowledgments
Funding was provided by the Open Society Foundations Criminal Justice Fund and the Campaign for the New Drug Policy. L. Beletsky is also supported in part by National Institute of Drug Abuse awards number R01DA039073 (L. Beletsky and S. Strathdee: PIs) and R37 DA019829 (S. Strathdee: PI).
We gratefully acknowledge the contribution of the following: Baltimore City Health Department Needle Exchange Program (NEP) clients; Baltimore City Department of Health Risk Reduction Services; NEP staff and volunteers (Lamont Clark, Derrick Hunt, Emily Clossner, Peter Fotang); and Project GIS Consultant (Emily Perkins).
Note. Opinions expressed are the authors’ own and do not necessarily reflect the view of the Open Society Foundations, the National Institutes of Health, or the National Institute of Drug Abuse.
Human Participant Protection
The study protocol was reviewed by the institutional review board of Johns Hopkins University.
References
- 1.Taussig JA, Weinstein B, Burris S, Jones TS. Syringe laws and pharmacy regulations are structural constraints on HIV prevention in the US. AIDS. 2000;14(suppl 1):S47–S51. doi: 10.1097/00002030-200006001-00007. [DOI] [PubMed] [Google Scholar]
- 2.Green TC, Martin EG, Bowman SE, Mann MR, Beletsky L. Life after the ban: an assessment of US syringe exchange programs’ attitudes about and early experiences with federal funding. Am J Public Health. 2012;102(5):e9–e16. doi: 10.2105/AJPH.2011.300595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burris, S. Syringe possession laws map. Law Atlas: The Policy Surveillance Portal. 2015. Available at: http://lawatlas.org/query?dataset=paraphernalia-laws. Accessed June 30, 2015.
- 3a.Wodak A, Cooney A. Do needle syringe programs reduce HIV infection among injecting drug users: a comprehensive review of the international evidence Subst Use Misuse. 2006. 41(6):777–813. [DOI] [PubMed]
- 4.Burris S. Syringe distribution laws map. Law Atlas: The Policy Surveillance Portal. 2014. Available at: http://lawatlas.org/query?dataset=syringe-policies-laws-regulating-non-retail-distribution-of-drug-paraphernalia. Accessed April 25, 2015.
- 5.Executive Office of the President of the United States. National Drug Control Strategy. 2014. Available at: https://www.whitehouse.gov/sites/default/files/ndcs_2014.pdf. Accessed April 25, 2015.
- 6. Peters J. Albany reaches deal to repeal ’70s drug laws. New York Times. March 26, 2009:A1.
- 7.Beletsky L, Thomas R, Smelyanskaya M et al. Policy reform to shift the health and human rights environment for vulnerable groups: the case of Kyrgyzstan’s instruction 417. Health Hum Rights. 2012;14(2):34–48. [PubMed] [Google Scholar]
- 8.Beletsky L, Grau LE, White E, Bowman S, Heimer R. The roles of law, client race, and program visibility in shaping police interference with the operation of US syringe exchange programs. Addiction. 2011;106(2):357–365. doi: 10.1111/j.1360-0443.2010.03149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beletsky L, Macalino G, Burris S. Attitudes of police officers towards syringe access, occupational needle-sticks, and drug use: a qualitative study of one city police department in the United States. Int J Drug Policy. 2005;16:267–274. [Google Scholar]
- 10.Burris S, Blankenship KM, Donoghoe M et al. Addressing the “risk environment” for injection drug users: the mysterious case of the missing cop. Milbank Q. 2004;82(1):125–156. doi: 10.1111/j.0887-378X.2004.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maher L, Dixon D. Policing and public health: law enforcement and harm minimization in a street-level drug market. Br J Criminol. 1999;39(4):488–512. [Google Scholar]
- 12.Martinez AN, Bluthenthal RN, Lorvick J, Anderson R, Flynn N, Kral AH. The impact of legalizing syringe exchange programs on arrests among injection drug users in California. J Urban Health. 2007;84(3):423–435. doi: 10.1007/s11524-006-9139-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Binswanger IA, Redmond N, Steiner JF, Hicks LS. Health disparities and the criminal justice system: an agenda for further research and action. J Urban Health. 2012;89(1):98–107. doi: 10.1007/s11524-011-9614-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper H, Moore L, Gruskin S, Krieger N. Characterizing perceived police violence: implications for public health. Am J Public Health. 2004;94(7):1109–1118. doi: 10.2105/ajph.94.7.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shannon K, Kerr T, Allinott S, Chettiar J, Shoveller J, Tyndall MW. Social and structural violence and power relations in mitigating HIV risk of drug-using women in survival sex work. Soc Sci Med. 2008;66(4):911–921. doi: 10.1016/j.socscimed.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Hammett T, Bartlett N, Chen Y et al. Law enforcement influences on HIV prevention for injection drug users: observations from a cross-border project in China and Vietnam. Int J Drug Policy. 2005;16:235–245. [Google Scholar]
- 17.Small W, Kerr T, Charette J, Schechter M, Spittal P. Impacts of intensified police activity on injection drug users: evidence from an ethnographic investigation. Int J Drug Policy. 2006;17:85–95. [Google Scholar]
- 18.Cohen J, Csete J. As strong as the weakest pillar: harm reduction, law enforcement and human rights. Int J Drug Policy. 2006;17(1):101–103. [Google Scholar]
- 19.Wolfe D, Malinowska-Sempruch K. Seeing double: mapping contradictions in HIV prevention and illicit drug policy worldwide. In: Beyer C, editor. Public Health and Human Rights: Evidence Based Approaches. Baltimore, MD: The Johns Hopkins University Press; 2007. [Google Scholar]
- 20.Lazzarini Z, Bray S, Burris S. Evaluating the impact of criminal laws on HIV risk behavior. J Law Med Ethics. 2002;30(2):239–253. doi: 10.1111/j.1748-720x.2002.tb00390.x. [DOI] [PubMed] [Google Scholar]
- 21.Bluthenthal RN, Kral AH, Erringer EA, Edlin BR. Drug paraphernalia laws and injection-related infectious disease risk among drug injectors. J Drug Issues. 1999;29(1):1–16. [Google Scholar]
- 22.Rhodes T, Mikhailova L, Sarang A et al. Situational factors influencing drug injecting, risk reduction and syringe exchange in Togliatti City, Russian Federation: a qualitative study of micro risk environment. Soc Sci Med. 2003;57(1):39–54. doi: 10.1016/s0277-9536(02)00521-x. [DOI] [PubMed] [Google Scholar]
- 23.Kerr T, Small W, Wood E. The public health and social impacts of drug market enforcement: a review of the evidence. Int J Drug Policy. 2005;16:210–220. [Google Scholar]
- 24.Grund J-PC, Heckathorn DD, Broadhead RS, Anthony D. In Eastern Connecticut, IDUs purchase syringes from pharmacies but don’t carry syringes. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;10(1):104–105. doi: 10.1097/00042560-199509000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Csete J. Do Not Cross: Policing and HIV Risk Faced by People Who Use Drugs. Toronto, ON: Canadian HIV/AIDS Legal Network; 2007. [Google Scholar]
- 26.Open Society Foundations. To protect and serve: how police, sex workers, and people who use drugs are joining forces to improve health and human rights. 2014. Available at: http://www.opensocietyfoundations.org/sites/default/files/protect-serve-20140716.pdf. Accessed April 25, 2015.
- 27.Koester S. The prevalence of additional injection-related HIV risk behaviors among injection drug users. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;12(2):202–207. doi: 10.1097/00042560-199606010-00015. [DOI] [PubMed] [Google Scholar]
- 28. Doe v Bridgeport Police Department, 198 FRD 325 (D CT 2001).
- 29. Roe v City of New York, 232 F Supp 2d 240 (SD NY 2002).
- 30.Friedman SR, Cooper HL, Tempalski B et al. Relationships of deterrence and law enforcement to drug-related harms among drug injectors in US metropolitan areas. AIDS. 2006;20(1):93–99. doi: 10.1097/01.aids.0000196176.65551.a3. [DOI] [PubMed] [Google Scholar]
- 31.Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors’ ability to practice harm reduction: a qualitative study. Soc Sci Med. 2005;61(3):673–684. doi: 10.1016/j.socscimed.2004.12.030. [DOI] [PubMed] [Google Scholar]
- 32.Davis CS, Burris S, Metzger D, Becher J, Lynch K. Effects of an intensive street-level police intervention on syringe exchange program utilization: Philadelphia, Pennsylvania. Am J Public Health. 2005;95(2):233–236. doi: 10.2105/AJPH.2003.033563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aitken C, Moore D, Higgs P, Kelsall J, Kerger M. The impact of a police crackdown on a street drug scene: evidence from the street. Int J Drug Policy. 2002;13:189–198. [Google Scholar]
- 34.Blankenship KM, Koester S. Criminal law, policing policy, and HIV risk in female street sex workers and injection drug users. J Law Med Ethics. 2002;30(4):548–559. doi: 10.1111/j.1748-720x.2002.tb00425.x. [DOI] [PubMed] [Google Scholar]
- 35.Beletsky L, Heimer R, editors. Aligning Criminal Justice and HIV Prevention: From Conflict to Synergy. New Haven, CT: Yale University Centre for Interdisciplinary Research on AIDS; 2009. Available at: http://papers.ssrn.com/sol3/papers.cfm?abstract_id=1478245. Accessed April 2, 2015. [Google Scholar]
- 36.Pollini RA, Brouwer KC, Lozada RM et al. Syringe possession arrests are associated with receptive syringe sharing in two Mexico–US border cities. Addiction. 2008;103(1):101–108. doi: 10.1111/j.1360-0443.2007.02051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rhodes T, Platt L, Sarang A, Vlasov A, Mikhailova L, Monaghan G. Street policing, injecting drug use and harm reduction in a Russian city: a qualitative study of police perspectives. J Urban Health. 2006;83(5):911–925. doi: 10.1007/s11524-006-9085-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iguchi MY, Bell J, Ramchand RN, Fain T. How criminal system racial disparities may translate into health disparities. J Health Care Poor Underserved. 2005;16(4 suppl B):48–56. doi: 10.1353/hpu.2005.0114. [DOI] [PubMed] [Google Scholar]
- 39.Bluthenthal RN. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Med Anthropol. 1997;18(1):61–83. doi: 10.1080/01459740.1997.9966150. [DOI] [PubMed] [Google Scholar]
- 40.Heimer R, Bluthenthal RN, Singer M, Khoshnood K. Structural impediments to operational syringe-exchange programs. AIDS Public Policy J. 1996;11(4):169–184. [PubMed] [Google Scholar]
- 41.New York, NY: American Civil Liberties Union; 2013. The war on marijuana in black and white: billions of dollars wasted on racially biased arrests. [Google Scholar]
- 42.Fellner J. Race, drugs, and law enforcement in the United States. Stanford Law Policy Rev. 2009;20:42. [Google Scholar]
- 43.Stolberg SG, Nixon R. Freddie Gray in Baltimore: another city, another death in the public eye. New York Times. April 22, 2015:A1. Available at: http://www.nytimes.com/2015/04/22/us/another-mans-death-another-round-of-questions-for-the-police-in-baltimore.html. Accessed April 25, 2015. [Google Scholar]
- 44.Targeting Blacks: Drug Law Enforcement and Race in the United States. New York, NY: Human Rights Watch; 2008. [Google Scholar]
- 45.Center for HIV Surveillance, State of Maryland. Baltimore City HIV/AIDS epidemiological profile. Maryland Department of Health and Human Hygiene; 2013. Available at: http://phpa.dhmh.maryland.gov/OIDEOR/CHSE/Shared%20Documents/Baltimore-City.pdf. Accessed April 25, 2015.
- 46.Mehta S, Galai N, Astemborski J et al. HIV incidence among injection drug users in Baltimore, Maryland (1988–2004) J Acquir Immune Defic Syndr. 2006;43(3):368–372. doi: 10.1097/01.qai.0000243050.27580.1a. [DOI] [PubMed] [Google Scholar]
- 47.Friedman SR, Tempalski B, Cooper H et al. Estimating numbers of injecting drug users in metropolitan areas for structural analyses of community vulnerability and for assessing relative degrees of service provision for injecting drug users. J Urban Health. 2004;81(3):377–400. doi: 10.1093/jurban/jth125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Genberg B, Astemborski J, Vlahov D, Kirk GD, Mehta SH.Incarceration and injection drug use in Baltimore, Maryland. Addiction In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Amon JJ, Garfein RS, Ahdieh-Grant L et al. Prevalence of hepatitis C virus infection among injection drug users in the United States, 1994–2004. Clin Infect Dis. 2008;46(12):1852–1858. doi: 10.1086/588297. [DOI] [PubMed] [Google Scholar]
- 50.Annapolis, MD: State of Maryland; 2013. Crime in Maryland: 2012 uniform crime report. Available at: http://www.goccp.maryland.gov/msac/documents/2012-Crime-In-Maryland.pdf. Accessed March 27, 2015. [Google Scholar]
- 51.Baltimore City Health Department. Community risk reduction: Baltimore City Needle Exchange Program. Available at: http://health.baltimorecity.gov/hiv-std-services/community-risk-reduction. Accessed March 10, 2015.
- 52.Maryland Department of Health and Mental Hygiene. Blacks or African Americans in Maryland: health data and resources. 2013. Available at: http://dhmh.maryland.gov/mhhd/Documents/Maryland-Black-or-African-American-Data-Report-December-2013.pdf. Accessed April 25, 2015.
- 53.Brodwater L. Baltimore wants to give out thousands more needles to drug users. Baltimore Sun. January 17, 2014. Available at: http://articles.baltimoresun.com/2014-01-17/news/bs-md-srb-legislative-agenda-20140117_1_clean-syringes-baltimore-county-addicts. Accessed April 20, 2015. [Google Scholar]
- 54.Hosmer D, Lemeshow S. Applied Logistic Regression. New York, NY: Wiley and Sons; 2002. [Google Scholar]
- 55.Centers for Disease Control and Prevention. Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report. 2012(4):17. Available at: http://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf. Accessed April 25, 2015. [Google Scholar]
- 56.Lankenau SE, Teti M, Silva K, Jackson Bloom J, Harocopos A, Treese M. Patterns of prescription drug misuse among young injection drug users. J Urban Health. 2012;89(6):1004–1016. doi: 10.1007/s11524-012-9691-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Peavy KM, Banta-Green CJ, Kingston S, Hanrahan M, Merrill JO, Coffin PO. “Hooked on” prescription-type opiates prior to using heroin: results from a survey of syringe exchange clients. J Psychoactive Drugs. 2012;44(3):259–265. doi: 10.1080/02791072.2012.704591. [DOI] [PubMed] [Google Scholar]
- 58.Beletsky L, Heller D, Jenness S, Neaigus A, Gelpi-Acostae C, Hagan H. Syringe access, syringe sharing, and police encounters among people who inject drugs in New York City: a community-level perspective. Int J Drug Policy. 2014;25(1):105–111. doi: 10.1016/j.drugpo.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mcara L, Mcvie S. The usual suspects? Street-life, young people and the police. Criminology and Criminal Justice. 2005;5(1):5–36. [Google Scholar]
- 60.Brown S. Understanding Youth and Crime: Listening to Youth? 2nd ed. Berkshire, England: Open University Press; 2005. [Google Scholar]
- 61.DeBeck K, Wood E, Zhang R, Tyndall M, Montaner J, Kerr T. Police and public health partnerships: evidence from the evaluation of Vancouver’s supervised injection facility. Subst Abuse Treat Prev Policy. 2008;3(1):11. doi: 10.1186/1747-597X-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Beletsky L, Grau LE, White E, Bowman S, Heimer R. Content, correlates and predictors of police training initiatives by syringe exchange programs. Drug Alcohol Depend. 2011;119(1-2):145–149. doi: 10.1016/j.drugalcdep.2011.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Beletsky L, Agrawal A, Moreau B, Kumar P, Weiss-Laxer N, Heimer R. Police training to align law enforcement and HIV prevention: preliminary evidence from the field. Am J Public Health. 2011;101(11):2012–2015. doi: 10.2105/AJPH.2011.300254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Beletsky L, Wagner KD, Arredondo J et al. Implementing Mexico’s “Narcomenudeo” drug law reform: a mixed-methods assessment of early experiences among people who inject drugs. J Mixed Methods Research. 2015 Epub ahead of print. [Google Scholar]
- 65.Wood E, Kerr T, Small W, Jones J, Schechter MT, Tyndall MW. The impact of a police presence on access to needle exchange programs. J Acquir Immune Defic Syndr. 2003;34(1):116–118. doi: 10.1097/00126334-200309010-00019. [DOI] [PubMed] [Google Scholar]
- 66.Beletsky L, Lozada R, Gaines T et al. Syringe confiscation as an HIV risk factor: the public health implications of arbitrary policing in Tijuana and Ciudad Juarez, Mexico. J Urban Health. 2013;90(2):284–298. doi: 10.1007/s11524-012-9741-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Beletsky L, Thomas R, Shumskaya N, Artamonova I, Smelyanskaya M. Police education as a component of a national HIV response: lessons from Kyrgyzstan. Drug Alcohol Depend. 2013;132(suppl 1):S48–S52. doi: 10.1016/j.drugalcdep.2013.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Silverman B, Davis C, Graff J, Bhatti U, Beletsky L. Harmonizing disease prevention and police practice in the implementation of HIV prevention programs: up-stream strategies from Wilmington, Delaware. Harm Reduct J. 2012;9:17. doi: 10.1186/1477-7517-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hedegaard H, Chen L, Warner M. QuickStats: rates of drug poisoning deaths involving heroin, by selected age and racial/ethnic groups—United States, 2002 and 2011. MMWR Morbid Mortal Wkly Rep. 2014;63:595. [Google Scholar]
- 70.Green TC, Zaller N, Palacios WR et al. Law enforcement attitudes toward overdose prevention and response. Drug Alcohol Depend. 2013;133(2):677–684. doi: 10.1016/j.drugalcdep.2013.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Davis CS, Beletsky L. Bundling occupational safety with harm reduction information as a feasible method for improving police receptiveness to syringe access programs: evidence from three US cities. Harm Reduct J. 2009;6:16. doi: 10.1186/1477-7517-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]