Abstract
Objective
We examined the relationship between chronotype and sleep disturbance, and assessed various factors that might be associated with sleep disturbance in Korean firefighters.
Methods
Self-administered questionnaires assessing chronotype, depression, alcohol use, posttraumatic stress disorder (PTSD), stress response and sleep quality were examined in 515 firefighters.
Results
Evening type firefighters more reported depression, alcohol use, PTSD, stress response and sleep disturbance. Also evening chronotype was the most significant risk factor for poor sleep quality (odds ratio [OR], 4.812; 95% confidence interval [CI], 2.448–9.459), even after controlling for all other variables (OR, 3.996; 95% CI, 1.806–8.841).
Conclusion
Chronotype was the factor most strongly associated with sleep disturbance, and therefore should be considered an important variable in sleep quality, particularly in occupations involving stressful activities, such as firefighting.
Keywords: Chronotype, Sleep disturbance, Insomnia, firefighter
INTRODUCTION
Chronotype (morning or evening) is determined according to diurnal preferences for activity and sleep.1) Several previous studies have suggested that chronotype represents an individual, stable characteristic, which may be underpinned by endogenous factors,2) and may affect biological and psychological functioning.3–5)
Sleep quality could be influenced by factors including age, circadian rhythm, work schedule and flexibility of sleep habits.6) Several studies have demonstrated that the evening chronotype is associated with sleep disturbance.7–12) The evening chronotype has also been associated with psychiatric illnesses including substance abuse,13) schizophrenia,14) and mood disorders,4,15–18) all of which can cause sleep disturbances.
Professional firefighting is a unique occupation, due to the high levels of stress and risk which it confers. Moreover, in many fire departments, firefighters typically work according to rotating shifts. Studies indicate that the prevalence of sleep disorders in firefighters is markedly higher compared with the general adult population. For example, in a recent study 59% of US firefighters were suffering from a sleep disorder.19) In a Brazilian study from 2012, 51% of firefighters were suffering from a sleep disorder.20) An Iranian study reported poor sleep quality (Pittsburgh Sleep Quality Index [PSQI] score of > 5) in 69.9% of a sample of firefighters in Tehran.21) Several studies have suggested that sleep disturbance in firefighters is related to psychological distress, excessive alcohol and smoking, depression and shiftwork.20–22)
Chronotype has been cited as a predictor of sleep disturbance in several studies assessing sleep quality among the general population and in nurses, but to date no study of firefighters has considered chronotype as a risk factor for sleep disturbance.
We investigated the relationship between chronotype and sleep quality in Korean firefighters, and assessed various factors that might be associated with sleep disturbance including age, shiftwork, stress response, post-traumatic stress disorder (PTSD), alcohol use, and depression.
METHODS
Data were collected from a sample of 584 emergency responders based in urban-area fire stations in the Republic of Korea. They were comprised of firefighters (n=271, 46.5%), 119 emergency medical services workers (n=104, 17.8%), 119 rescuer (n=35, 6.0%), administrative officials (n=111, 19.0%) and missing data (n=63, 10.8%). They were eligible to participate if they met the following inclusion criteria: between 18 and 65 years of age; willing and able to provide written informed consent; and able to read and write in Korean. All participants provided written informed consent following an explanation of the procedure. Evidence of cognitive impairment, or history of a psychotic disorder, represented the exclusion criteria. We excluded 69 subjects due to missing data, yielding a final sample size of 515. Demographic information pertaining to age, sex, marital status, religion and educational level, and occupational characteristics including work period, shiftwork and musculoskeletal symptoms, were obtained using a self-report questionnaire. Musculoskeletal symptoms were evaluated using the Korea Occupational Safety and Health Agency’s Guidelines on Occupational Harms Affecting the Musculoskeletal System (KOSHA code H-30-208).23)
Psychometric instruments, including a Korean translation of the Composite Scale (KtCS), the Beck Depression Inventory (BDI), a Korean version of the PSQI, the Stress Response Inventory (SRI), a Korean version of the Impact of the Event Scale-Revised (IES-R) and a Korean version of the Alcohol Use Disorders Identification Test (AUDIT), were used to assess chronotype, depression, sleep disturbance, stress response, PTSD symptoms and alcohol use, respectively. This study was approved by the Institutional Review Boards of Eulji University Hospital (EMC08-47) and Dongguk University Ilsan Hospital (DUMC2009-1-17).
Measures
KtCS
Chronotype is determined by a number of different self-assessment scales, validated in several countries.3) The Composite Scale of Morningness (CSM) is a 13-item questionnaire that assesses individual differences in the time of day a person prefers to carry out various activities, and classifies them as morning- or evening-type.24) Three items are scored on a 5-point scale (range, 1–5); the remaining 10 items are scored on a 4-point scale (range, 1–4). Higher scores indicate a greater morning preference. CSM consistently reported high level of reliability (>0.80) and it has good convergent validity with other questionnaires that measure circadian typology.25) The KtCS has acceptable psychometric properties (Cronbach’s α=0.82, test-retest reliability=0.82).26,27) In a previous study, the cut-off points for morning-type and evening-type were set at the 10th and 90th percentiles: scores of >41 are indicative of morning-type; scores of <26 indicate evening-type.27)
BDI
The BDI, a 21-item self-administered questionnaire, was developed to assess the severity of subjective depressive symptoms.28) Each response is assigned a score between 0 and 3, with higher scores representing greater symptom severity. The Korean version of the BDI has good psychometric properties (Cronbach’s α=0.86).29)
PSQI
The PSQI is a self-reported questionnaire that measures sleep quality during the previous month, and distinguishes “good” from “poor” sleepers. Higher mean scores correspond to reduced sleep quality, with scores of >5 indicative of poor sleep quality.30) However, in the Korean version of the PSQI, a cutoff score of 8.5 represents a sensitivity of 0.943 and a specificity of 0.844,31) which is higher than the score of 5 in the original paper.30) The Korean version of the PSQI has good psychometric properties (Cronbach’s α=0.84).31)
SRI
The SRI was developed by Koh et al.32) in 2000. It includes emotional, somatic, cognitive, and behavioral stress response items (n=39) across seven subscales (tension, aggression, somatization, anger, depression, fatigue, and frustration). Each subscale is scored using Likert-type scales: 0 (Not at all); 1 (Somewhat); 2 (Moderately); 3 (Very much); 4 (Completely). The SRI has a high degree of reliability and validity, and is therefore an effective measure of stress (Cronbach’s α= 0.97).32)
IES-R
The IES-R was developed by Weiss and Marmar.33) The original IES was a 15-item self-reported measure of two PTSD symptom domains, with seven items addressing intrusion and eight addressing avoidance. However, the original IES did not address hyperarousal symptoms; five items related to hyperarousal were thus added to the revised version. The IES-R uses 5-point scales (range, 0–4) to evaluate the severity of symptoms experienced during the previous week. The Korean version of the IES-R has good psychometric properties (Cronbach’s α=0.93).34)
AUDIT
The AUDIT is a 10-item questionnaire concerned with alcohol consumption, drinking behavior, and alcohol-related problems. The AUDIT provides a simple method of early detection of hazardous and harmful alcohol use in primary health care settings.35)
The Korean version of the AUDIT (AUDIT-K) has high internal consistency and test-retest reliability. The significant correlation coefficients of the AUDIT-K, with the Korean versions of the Michigan Alcoholism Screening Test (MAST-K) and Korean version of CAGE (CAGE-K), were 0.86 and 0.80, respectively. The optimal cut-off point was estimated as 12, at which value sensitivity and specificity were 0.84 and 0.86, respectively.36)
Data Analysis
Firefighters were categorized as being either morning, neither, or evening chronotypes, based upon their KtCS scores. For basic comparisons, sociodemographic characteristics were examined using one-way analysis of variance (ANOVA) for continuous variables, and chi-squared tests for categorical variables. Multivariate analysis of covariance (MANCOVA) was applied to evaluate differences between chronotypes with respect to IES-R, AUDIT, SRI, BDI and PSQI scores with age as a covariate to control for possible effects. Using a PSQI cutoff score of 8.5, we divided firefighters into good and poor sleepers. Logistic regression analyses were used to identify factors that might influence sleep quality. These factors were age, shift schedule, musculoskeletal symptoms, PTSD, alcohol use, stress response, depression and chronotype. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Statistical analyses were performed using the PASW Statistics for Windows software package (ver. 18.0; IBM Co., Armonk, NY, USA).
RESULTS
Sociodemographic Characteristics of the Study Sample (Table 1)
Table 1.
Sociodemographic characteristics of the study sample across chronotypes
| Characteristic | Morning-type | Neither-type | Evening-type | p value |
|---|---|---|---|---|
| Age (yr) | 42.01±8.54 | 37.57±7.61 | 35.22±5.87 | <0.001 |
| Sex (female) | 9 (9.28) | 15 (4.09) | 4 (7.84) | 0.097 |
| Marital status | 0.107 | |||
| Single, separated, deceased | 21 | 117 | 18 | |
| Married, remarried | 76 | 250 | 33 | |
| Religion | 0.151 | |||
| None | 54 (56.3) | 206 (56.3) | 38 (74.5) | |
| Buddhism | 21 (21.9) | 65 (17.8) | 2 (3.9) | |
| Christianity | 12 (12.5) | 66 (18) | 8 (15.7) | |
| Catholic | 9 (9.4) | 27 (7.4) | 3 (5.9) | |
| Education (yr) | 14.09±2.15 | 14.78±1.98 | 14.63±1.98 | 0.011 |
| Work period (mo), mean | 174.04 | 116.72 | 87.00 | <0.001 |
| Shift schedule | 0.006 | |||
| 8 or 24 hour rotating shifts | 66 (68.0) | 300 (81.7) | 43 (86.0) | |
| Daytime | 31 (31.9) | 67 (18.3) | 7 (14.0) | |
| Musculoskeletal symptoms (+) | 36 (37.1) | 147 (40.5) | 16 (31.4) | 0.420 |
Values are presented as number only, mean±standard deviation, and number (%).
We divided the firefighters into three groups according to their KtCS scores: morning-type (n=97, 18.8%), neither-type (n=367, 71.3%), and evening-type (n=51, 9.9%).
The proportion of female firefighters was 9.28% in morning-type, 4.09% in neither, and 7.84% in evening-type. No significant group differences in sex, marital status or religion were observed.
The morning-type group had the highest mean age, followed by the neither group, and then the evening-type group. One-way ANOVA revealed significant differences in mean age among the three groups (p<0.001).
Education, work period and shift schedule were also significantly different among the three groups. Morning-type firefighters were characterized by a lower education level (p<0.05) and longer work period (p<0.001) compared with the other two groups. However, after controlling for age, there were no significant differences between chronotypes in education and work period.
Comparison of the Psychiatric Rating Scale Scores of the Chronotypes
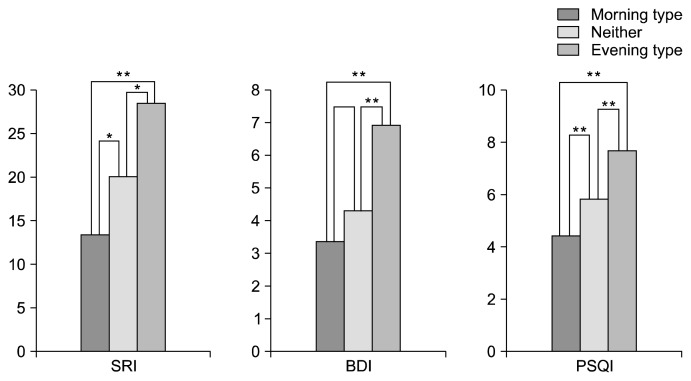
Descriptive data for circadian typology in the psychiatric rating scale scores are shown in Fig. 1 and Table 2. In all of the psychiatric rating scales, evening-types had higher scores than did morning-types. MANCOVA with controlling for age confirmed group differences in SRI, BDI and PSQI scores (p<0.05; Table 2). Post hoc comparisons revealed that all scores were significantly different between all groups (p<0.05), except difference of BDI between morning-type vs. neither-type (Figure 1).
Fig. 1.
Comparison of psychiatric scales between chronotypes. **p<0.01, *p<0.05.
SRI, Stress Response Inventory; BDI, Beck Depression Inventory; PSQI, Pittsburgh Sleep Quality Index.
Table 2.
The result of psychiatric rating scales of the study sample across chronotypes after controlling for age
| Morning-type | Neither-type | Evening-type | F | η2 | p value | |
|---|---|---|---|---|---|---|
| AUDIT | 8.34±5.57 | 9.24±5.95 | 10.86±7.74 | 1.392 | 0.011 | 0.245 |
| IES-R | 8.03±10.76 | 9.26±12.85 | 11.78±13.42 | 1.250 | 0.010 | 0.291 |
| SRI | 13.48±17.96 | 22.41±48.46 | 28.56±26.65 | 8.92 | 0.034 | <0.001 |
| BDI | 3.44±3.90 | 4.12±5.30 | 6.95±7.53 | 4.969 | 0.037 | 0.002 |
| PSQI | 4.41±2.49 | 5.84±3.05 | 7.54±3.48 | 9.267 | 0.067 | <0.001 |
Values are presented as mean±standard deviation.
AUDIT, Alcohol Use Disorders Identification Test; IES-R, Impact of the Event Scale-Revised; SRI, Stress Response Inventory; BDI, Beck Depression Inventory; PSQI, Pittsburgh Sleep Quality Index; η2, partial eta squared (effect size).
Factors Related to Sleep Disturbance (Table 3)
Table 3.
Logistic regression analysis of factors related to poor sleeper (PSQI>8.5)
| Variable | OR unadjusted† (95% CI) | p value | OR adjusted*† (95% CI) | p value |
|---|---|---|---|---|
| Age | 0.989 (0.959–1.020) | 0.479 | 1.000 (0.961–1.040) | 0.999 |
| Shift schedule‡ | 1.605 (0.824–3.124) | 0.164 | 1.720 (0.749–3.950) | 0.201 |
| Musculoskeletal symptoms§ | 1.629 (0.996–2.664) | 0.052 | 1.195 (0.655–2.183) | 0.562 |
| IES-R | 1.044 (1.025–1.065) | <0.001 | 1.019 (0.998–1.041) | 0.080 |
| AUDIT | 1.034 (0.995–1.076) | 0.088 | 1.015 (0.969–1.062) | 0.537 |
| SRI | 1.024 (1.013–1.036) | <0.001 | 1.004 (0.988–1.021) | 0.619 |
| BDI | 1.148 (1.098–1.201) | <0.001 | 1.132 (1.067–1.202) | <0.001 |
| KtCS¶ | 4.812 (2.448–9.459) | <0.001 | 3.996 (1.806–8.841) | 0.001 |
Odds ratio (OR) adjusted for all variables listed in the table.
Group: 0=good sleeper; 1=poor sleeper.
Shift schedule: 0=non-shift work, 1=shift work.
Musculoskeletal symptoms: 0=(−), 1=(+)
KtCS: 0=morning- and neither-type, 1=evening-type
PSQI, Pittsburgh Sleep Quality Index; CI, confidence interval; AUDIT, Alcohol Use Disorders Identification Test; IES-R, Impact of the Event Scale-Revised; SRI, Stress Response Inventory; BDI, Beck Depression Inventory; KtCS, Korean translation of Composite Scale.
Logistic regression analysis was performed to discern the effect of chronotype, and other variables, on sleep quality. All of the other previously listed variables were adjusted for.
Using a PSQI cutoff score of 8.5, we divided the firefighters into good (PSQI score of <8.5, n=328, 79.6%) and poor (PSQI score of >8.5, n=84, 20.4%) sleepers.
In a logistic regression analysis of the good and poor sleepers, IES-R (OR, 1.044; 95% CI, 1.025–1.065), BDI (OR, 1.148; 95% CI, 1.098–1.201), SRI (OR, 1.024; 95% CI, 1.013–1.036) and chronotype (OR, 4.812; 95% CI, 2.448–9.459) scores were all associated with sleep quality, but age (OR, 0.989; 95% CI, 0.959–1.020), shiftwork (OR, 1.605; 95% CI, 0.824–3.124), musculoskeletal symptoms (OR, 1.629; 95% CI, 0.996–2.664) and alcohol use (OR, 1.034; 95% CI, 0.995–1.076) were not. After controlling for all of the other variables listed in Table 3, BDI (OR, 1.132; 95% CI, 1.067–1.202) and chronotype (OR, 3.996; 95% CI, 1.806–8.841) were still significant predictors; chronotype was the most powerful predictor.
DISCUSSION
We assessed the relationship between chronotype and sleep disturbance in Korean firefighters, analyzing the effects of age, shiftwork, stress response, PTSD, alcohol use, and depression. We found that evening-type firefighters reported poorer sleep quality compared with morning-type firefighters. The major determinant of sleep quality was chronotype.
Some studies have reported that evening types are more common among men than women,37–39) although Merikanto et al.10) found that morning types were more frequent among men than women. In this study, we did not find any differences in chronotype according to sex. The discrepancy could be due to differences in the recruitment process and the representativeness of the study samples. Our study sample represented a special job population rather than a general population, and there were few women.
Chronotype has been shown to depend on age.40–43) In this study, the morning-type group had the oldest mean age, followed by the neither-type and evening-type groups. In other studies of chronotype, the morningness score tended to increase with age after adolescence.6,10,37,44–47) Furthermore, the period and amplitude of body temperature rhythms decrease with age.48) Earlier phases of the circadian temperature rhythm are associated with earlier habitual bed and wake times.49) With aging, the circadian rhythm phase moves forward so that individuals may shift toward the morning type. Our study subjects also showed significant variation in education level and work period, which were related to age. After controlling for age, these differences disappeared.
Most of our study subjects were shift workers, and fewer shift workers are morning types. We found that shift-work was not associated with sleep disturbance. Several studies have investigated the relationship between sleep quality and chronotype in shift nurses.11,12) Evening-type nurses working variable shifts were more likely to have poor sleep quality compared with morning types, after controlling for age. Consistent with our finding, the strongest predictor of sleep quality in nurses was chronotype rather than the shift schedule or pattern.12) However, other studies have found significantly reduced sleep duration and quality in evening-type versus morning-type shift workers.11,50,51) Sleep disturbance, fatigue, and work-related accidents are relatively common among shift workers.52) Furthermore, fatigue, decreased alertness, and poorer mood are more frequent among firefighters working night shifts.53) Consequently, shiftwork itself may be associated with sleep disturbances and other psychiatric symptoms. This study compared a relatively small number of non-shiftwork firefighters with shiftwork firefighters; therefore, future studies would benefit from larger sample sizes.
Consistent with previous studies,7,9,10) being an evening-type was associated with sleep disturbance in this study. Merikanto et al.10) have also reported that, among both males and females, evening types experience insufficient sleep and nightmares and are significantly more likely to have used hypnotics recently compared with the other chronotypes.10) Recent evidence linked the evening chronotype to more frequent and intense nightmares.54,55) In one study, compared with morning and intermediate chronotypes, evening types reported more pathological, insomnia-related symptoms, despite their having more total sleep time.7) One explanation for the poorer sleep quality in evening types may be that this chronotype is associated with a relatively longer circadian period,56) leading to higher levels of sleep inertia. Accordingly, evening-type individuals tend to experience morning sleepiness and insufficient sleep.10) The greater proneness of evening types to experience sleep problems compared with morning types may also be related to differences in their homeostatic sleep regulation, probably due to the faster homeostatic sleep pressure dissipation in morning types.57) Morning types show an increased homeostatic response to behavioral sleep fragmentation than do evening types. Chronotype and sex were shown to affect the sleep architecture and quantitative sleep electroencephalography parameters in healthy young adults.58,59)
In this study, evening types also had higher BDI scores compared with the other chronotypes. Several studies have suggested a relationship between depression and chronotype, patients with major depression included a higher proportion of evening chronotypes than did non-clinical populations4,5,55) and non-insomniacs.4,7,17) Another study suggested that evening chronotype is a risk factor for depression.4,17) Although evening preference has recently been identified as a risk factor for depression, it is not clear whether it is a direct risk factor or exerts a secondary effect through other factors, including delayed sleep timing and shortened sleep duration. Although our study does not demonstrate causal relationships among chronotype, sleep disturbance, and depression, it does suggest functional associations between variations in mood and the biological clock systems that regulate diurnal preference and sleep.
Few studies have focused on the influence of chronotype on hazardous alcohol consumption. Studies indicate that evening-type subjects consume more alcohol than do morning- and neither-type subjects.60,61) Prat and Adan62) evaluated the relation between the AUDIT scores and chronotype and found that evening-type subjects scored higher on the subscales for potential alcohol problems compared with morning- and neither-type subjects. They postulated that evening types may tend to consume more alcohol at the end of the day when they are highly activated, perhaps excessively so, and use alcohol as a depressant to counteract this level of activity. Other authors have pointed out that evening-type individuals are prone to higher novelty or sensation seeking and impulsivity,3,63,64) personality traits that have been associated with substance abuse, which might indirectly explain the association between eveningness and substance use.62) Our study also found that evening-type firefighters had higher AUDIT scores than did other chronotypes, although the difference was not significant. This could be due to differences in sociodemographic characteristics, including age, sex, marital status, and occupation. Our subjects included a wider range of ages, a much lower percentage of females, and more married people that that study. Especially, considering the distinct occupational characteristics, firefighters may represent a group at risk for drinking. The mean total AUDIT scores across the chronotypes in our study subjects were higher than general population. Several studies have revealed that the drinking levels of firefighters exceeded those of the general adult population.65,66)
It is well known that PTSD, depression, and alcohol use are associated with sleep disturbance. Previous studies of firefighters and other rescue workers have reported higher rates of all three phenomena.67) Several studies have assessed the factors associated with sleep disturbance in firefighters. Psychological distress, psychosomatic imbalance, suicidal ideation, and excessive alcohol use were significantly associated with sleep disturbance,20) and smoking, having a second job, and greater job experience were suggested as predictors of poor sleep.21) In a recent South Korean study of firefighters, shiftwork, musculoskeletal symptoms, and depression were associated with sleep disorders.22) Our study considered a relatively wide range of factors, including depression, PTSD, alcohol use, stress response, musculoskeletal symptoms, shiftwork, and chronotype. Depression and stress response were significantly related to chronotype. Additionally in multiple logistic regression analysis, the factor most strongly associated with sleep disturbance was chronotype. No previous study of firefighters has considered chronotype as a risk factor for sleep disturbance, so this result is noteworthy.
Professional firefighters are exposed to greater risks of physical and mental health problems and high-risk behaviors affecting psychosomatic well-being than most other groups of people are.19) These difficulties might result in adverse effects on performance and health, including psychiatric condition.19–21,67) Firefighters at particularly high risk for psychiatric problems are required to undergo individually tailored health promotion and prevention interventions.
According to our results, chronotype should be considered a risk factor for sleep disturbance in firefighters. Therefore, assessing chronotype may represent an important initial risk-analysis step. Identification of chronotype can be used not only to predict sleep disturbance but also to detect or prevent psychiatric disorders that may accompany sleep disturbance.
This study has several limitations. First, the cross-sectional design limits its ability to establish causal relationships. Therefore, the results should be interpreted cautiously, and future longitudinal and experimental research is required. Second, this study relied solely on self-reported questionnaires. Although all of the scales used have been validated, future studies using standardized interviews or observational methods could provide more accurate and detailed information on the complex mechanisms underlying the relationship between chronotype and sleep disturbance. Third, other factors that might influence sleep disturbance, such as nicotine and caffeine use, were not assessed comprehensively. Finally, the study included very few female participants. Future research involving more females is required to determine whether our results can be generalized to female firefighters.
In a Korean sample, evening-type firefighters were characterized by poorer sleep quality compared with both neither and morning-types. The variable most strongly associated with sleep quality was chronotype.
Chronotype should therefore be considered an important risk factor for sleep disturbance in occupations involving stressful activities and high-risk behaviors, such as firefighting.
Acknowledgments
This work was supported by Grant No KFI-2009-Next generation-001 from Korea National Emergency Management Agency.
REFERENCES
- 1.Freeman GL, Hovland CI. Diurnal variations in performance and related physiological processes. Psychol Bull. 1934;31:777–799. doi: 10.1037/h0071917. [DOI] [Google Scholar]
- 2.Kerkhof GA. Inter-individual differences in the human circadian system: a review. Biol Psychol. 1985;20:83–112. doi: 10.1016/0301-0511(85)90019-5. [DOI] [PubMed] [Google Scholar]
- 3.Adan A, Archer SN, Hidalgo MP, Di Milia L, Natale V, Randler C. Circadian typology: a comprehensive review. Chronobiol Int. 2012;29:1153–1175. doi: 10.3109/07420528.2012.719971. [DOI] [PubMed] [Google Scholar]
- 4.Chelminski I, Ferraro FR, Petros TV, Plaud JJ. An analysis of the “eveningness-morningness” dimension in “depressive” college students. J Affect Disord. 1999;52:19–29. doi: 10.1016/S0165-0327(98)00051-2. [DOI] [PubMed] [Google Scholar]
- 5.Hidalgo MP, Caumo W, Posser M, Coccaro SB, Camozzato AL, Chaves ML. Relationship between depressive mood and chronotype in healthy subjects. Psychiatry Clin Neurosci. 2009;63:283–290. doi: 10.1111/j.1440-1819.2009.01965.x. [DOI] [PubMed] [Google Scholar]
- 6.Paine SJ, Gander PH, Travier N. The epidemiology of morningness/eveningness: influence of age, gender, ethnicity, and socioeconomic factors in adults (30–49 years) J Biol Rhythms. 2006;21:68–76. doi: 10.1177/0748730405283154. [DOI] [PubMed] [Google Scholar]
- 7.Ong JC, Huang JS, Kuo TF, Manber R. Characteristics of insomniacs with self-reported morning and evening chronotypes. J Clin Sleep Med. 2007;3:289–294. [PMC free article] [PubMed] [Google Scholar]
- 8.Demir Zencirci A, Arslan S. Morning-evening type and burnout level as factors influencing sleep quality of shift nurses: a questionnaire study. Croat Med J. 2011;52:527–537. doi: 10.3325/cmj.2011.52.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vardar E, Vardar SA, Molla T, Kaynak C, Ersoz E. Psychological symptoms and sleep quality in young subjects with different circadian preferences. Biol Rhythm Res. 2008;39:493–500. doi: 10.1080/09291010701736884. [DOI] [Google Scholar]
- 10.Merikanto I, Kronholm E, Peltonen M, Laatikainen T, Lahti T, Partonen T. Relation of chronotype to sleep complaints in the general Finnish population. Chronobiol Int. 2012;29:311–317. doi: 10.3109/07420528.2012.655870. [DOI] [PubMed] [Google Scholar]
- 11.Yazdi Z, Sadeghniiat-Haghighi K, Javadi AR, Rikhtegar G. Sleep quality and insomnia in nurses with different circadian chronotypes: morningness and eveningness orientation. Work. 2014;47:561–567. doi: 10.3233/WOR-131664. [DOI] [PubMed] [Google Scholar]
- 12.Chung MH, Chang FM, Yang CC, Kuo TB, Hsu N. Sleep quality and morningness-eveningness of shift nurses. J Clin Nurs. 2009;18:279–284. doi: 10.1111/j.1365-2702.2007.02160.x. [DOI] [PubMed] [Google Scholar]
- 13.Adan A. Chronotype and personality factors in the daily consumption of alcohol and psychostimulants. Addiction. 1994;89:455–462. doi: 10.1111/j.1360-0443.1994.tb00926.x. [DOI] [PubMed] [Google Scholar]
- 14.Hofstetter JR, Mayeda AR, Happel CG, Lysaker PH. Sleep and daily activity preferences in schizophrenia: associations with neurocognition and symptoms. J Nerv Ment Dis. 2003;191:408–410. doi: 10.1097/01.NMD.0000071591.91247.67. [DOI] [PubMed] [Google Scholar]
- 15.Elmore SK, Dahl K, Avery DH, Savage MV, Brengelmann GL. Body temperature and diurnal type in women with seasonal affective disorder. Health Care Women Int. 1993;14:17–26. doi: 10.1080/07399339309516023. [DOI] [PubMed] [Google Scholar]
- 16.Mansour HA, Wood J, Chowdari KV, Dayal M, Thase ME, Kupfer DJ, et al. Circadian phase variation in bipolar I disorder. Chronobiol Int. 2005;22:571–584. doi: 10.1081/CBI-200062413. [DOI] [PubMed] [Google Scholar]
- 17.Drennan MD, Klauber MR, Kripke DF, Goyette LM. The effects of depression and age on the Horne-Ostberg morningness-eveningness score. J Affect Disord. 1991;23:93–98. doi: 10.1016/0165-0327(91)90096-B. [DOI] [PubMed] [Google Scholar]
- 18.Chung JK, Lee KY, Kim SH, Kim EJ, Jeong SH, Jung HY, et al. Circadian rhythm characteristics in mood disorders: Comparison among bipolar I disorder, bipolar II disorder and recurrent major depressive disorder. Clin Psychopharmacol Neurosci. 2012;10:110–116. doi: 10.9758/cpn.2012.10.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carey MG, Al-Zaiti SS, Dean GE, Sessanna L, Finnell DS. Sleep problems, depression, substance use, social bonding, and quality of life in professional firefighters. J Occup Environ Med. 2011;53:928–933. doi: 10.1097/JOM.0b013e318225898f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vargas de Barros V, Martins LF, Saitz R, Bastos RR, Ronzani TM. Mental health conditions, individual and job characteristics and sleep disturbances among firefighters. J Health Psychol. 2013;18:350–358. doi: 10.1177/1359105312443402. [DOI] [PubMed] [Google Scholar]
- 21.Mehrdad R, Haghighi KS, Esfahani AH. Sleep quality of professional firefighters. Int J Prev Med. 2013;4:1095–1100. [PMC free article] [PubMed] [Google Scholar]
- 22.Lim DK, Baek KO, Chung IS, Lee MY. Factors related to sleep disorders among male firefighters. Ann Occup Environ Med. 2014;26:11. doi: 10.1186/2052-4374-26-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cho JJ, Kim JY, Chang SJ, Fiedler N, Koh SB, Crabtree BF, et al. Occupational stress and depression in Korean employees. Int Arch Occup Environ Health. 2008;82:47–57. doi: 10.1007/s00420-008-0306-4. [DOI] [PubMed] [Google Scholar]
- 24.Smith CS, Reilly C, Midkiff K. Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. J Appl Psychol. 1989;74:728–738. doi: 10.1037/0021-9010.74.5.728. [DOI] [PubMed] [Google Scholar]
- 25.Di Milia L, Adan A, Natale V, Randler C. Reviewing the psychometric properties of contemporary circadian typology measures. Chronobiol Int. 2013;30:1261–1271. doi: 10.3109/07420528.2013.817415. [DOI] [PubMed] [Google Scholar]
- 26.Kook SH, Yoon JS, Lee HY. Cross validation of the Korean translation of composite scale(KtCS) to measure morningness-eveningness. J Korean Neuropsychiatr Assoc. 1999;38:297–305. [Google Scholar]
- 27.Yoon JS, Shin SM, Kook SH, Lee HY. A preliminary study on the Korean translation of composite scale(KtCS) to measure morningness: eveningness. J Korean Neuropsychiatr Assoc. 1997;36:122–134. [Google Scholar]
- 28.Beck AT, Steer RA. Internal consistencies of the original and revised Beck Depression Inventory. J Clin Psychol. 1984;40:1365–1367. doi: 10.1002/1097-4679(198411)40:6<1365::AID-JCLP2270400615>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 29.Rhee MK, Lee YH, Park SH, Sohn CH, Chung YC, Hong SK, et al. A standardization study of Beck depression inventory I - Korean version (K-BDI): reliability and factor anlysis. Korean J Psychopathol. 1995;4:77–95. [Google Scholar]
- 30.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 31.Sohn SI, Kim do H, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012;16:803–812. doi: 10.1007/s11325-011-0579-9. [DOI] [PubMed] [Google Scholar]
- 32.Koh KB, Park JK, Kim CH. Development of the stress response inventory. J Korean Neuropsychiatr Assoc. 2000;39:707–719. [Google Scholar]
- 33.Weiss DS, Marmar CR. The impact of event scale-revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford; 1997. pp. 399–411. [Google Scholar]
- 34.Lim HK, Woo JM, Kim TS, Kim TH, Choi KS, Chung SK, et al. Disaster Psychiatry Committee in Korean Academy of Anxiety Disorders. Reliability and validity of the Korean version of the Impact of Event Scale-Revised. Compr Psychiatry. 2009;50:385–390. doi: 10.1016/j.comppsych.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 36.Lee BO, Lee CH, Lee PG, Choi MJ, Namkoong K. Development of Korean version of Alcohol Use Disorders Identification Test(AUDIT-K): its reliability and validity. J Korean Acad Addict Psychiatry. 2000;4:83–92. [Google Scholar]
- 37.Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, et al. Epidemiology of the human circadian clock. Sleep Med Rev. 2007;11:429–438. doi: 10.1016/j.smrv.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 38.Lehnkering H, Siegmund R. Influence of chronotype, season, and sex of subject on sleep behavior of young adults. Chronobiol Int. 2007;24:875–888. doi: 10.1080/07420520701648259. [DOI] [PubMed] [Google Scholar]
- 39.Adan A, Natale V. Gender differences in morningness-eveningness preference. Chronobiol Int. 2002;19:709–720. doi: 10.1081/CBI-120005390. [DOI] [PubMed] [Google Scholar]
- 40.Roenneberg T, Wirz-Justice A, Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythms. 2003;18:80–90. doi: 10.1177/0748730402239679. [DOI] [PubMed] [Google Scholar]
- 41.Park YM, Matsumoto K, Seo YJ, Kang MJ, Nagashima H. Changes of sleep or waking habits by age and sex in Japanese. Percept Mot Skills. 2002;94:1199–1213. doi: 10.2466/pms.2002.94.3c.1199. [DOI] [PubMed] [Google Scholar]
- 42.Duffy JF, Czeisler CA. Age-related change in the relationship between circadian period, circadian phase, and diurnal preference in humans. Neurosci Lett. 2002;318:117–120. doi: 10.1016/S0304-3940(01)02427-2. [DOI] [PubMed] [Google Scholar]
- 43.Dijk DJ, Duffy JF, Czeisler CA. Contribution of circadian physiology and sleep homeostasis to age-related changes in human sleep. Chronobiol Int. 2000;17:285–311. doi: 10.1081/CBI-100101049. [DOI] [PubMed] [Google Scholar]
- 44.Koskenvuo M, Hublin C, Partinen M, Heikkilä K, Kaprio J. Heritability of diurnal type: a nationwide study of 8753 adult twin pairs. J Sleep Res. 2007;16:156–162. doi: 10.1111/j.1365-2869.2007.00580.x. [DOI] [PubMed] [Google Scholar]
- 45.Roepke SE, Duffy JF. Differential impact of chronotype on weekday and weekend sleep timing and duration. Nat Sci Sleep. 2010;2010:213–220. doi: 10.2147/NSS.S12572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim SJ, Lee YJ, Kim H, Cho IH, Lee JY, Cho SJ. Age as a moderator of the association between depressive symptoms and morningness-eveningness. J Psychosom Res. 2010;68:159–164. doi: 10.1016/j.jpsychores.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 47.Park YM, Matsumoto K, Seo YJ, Kang MJ, Nagashima H. Effects of age and gender on sleep habits and sleep trouble for aged people. Biol Rhythm Res. 2002;33:39–51. doi: 10.1076/brhm.33.1.39.1327. [DOI] [Google Scholar]
- 48.Weitzman ED, Moline ML, Czeisler CA, Zimmerman JC. Chronobiology of aging: temperature, sleep-wake rhythms and entrainment. Neurobiol Aging. 1982;3:299–309. doi: 10.1016/0197-4580(82)90018-5. [DOI] [PubMed] [Google Scholar]
- 49.Carrier J, Monk TH, Reynolds CF, 3rd, Buysse DJ, Kupfer DJ. Are age differences in sleep due to phase differences in the output of the circadian timing system? Chronobiol Int. 1999;16:79–91. doi: 10.3109/07420529908998714. [DOI] [PubMed] [Google Scholar]
- 50.Khaleque A. Sleep deficiency and quality of life of shift workers. Soc Indic Res. 1999;46:181–189. doi: 10.1023/A:1006971209513. [DOI] [Google Scholar]
- 51.Seo YJ, Matsumoto K, Park YM, Shinkoda H, Noh TJ. The relationship between sleep and shift system, age and chronotype in shift workers. Biol Rhythm Res. 2000;31:559–579. doi: 10.1076/brhm.31.5.559.5655. [DOI] [Google Scholar]
- 52.Lusa S, Häkkänen M, Luukkonen R, Viikari-Juntura E. Perceived physical work capacity, stress, sleep disturbance and occupational accidents among firefighters working during a strike. Work Stress. 2002;16:264–274. doi: 10.1080/02678370210163301. [DOI] [Google Scholar]
- 53.Paley MJ, Tepas DI. Fatigue and the shiftworker: firefighters working on a rotating shift schedule. Hum Factors. 1994;36:269–284. doi: 10.1177/001872089403600208. [DOI] [PubMed] [Google Scholar]
- 54.Nielsen T. Nightmares associated with the eveningness chronotype. J Biol Rhythms. 2010;25:53–62. doi: 10.1177/0748730409351677. [DOI] [PubMed] [Google Scholar]
- 55.Selvi Y, Aydin A, Boysan M, Atli A, Agargun MY, Besiroglu L. Associations between chronotype, sleep quality, suicidality, and depressive symptoms in patients with major depression and healthy controls. Chronobiol Int. 2010;27:1813–1828. doi: 10.3109/07420528.2010.516380. [DOI] [PubMed] [Google Scholar]
- 56.Emens JS, Yuhas K, Rough J, Kochar N, Peters D, Lewy AJ. Phase angle of entrainment in morning- and evening-types under naturalistic conditions. Chronobiol Int. 2009;26:474–493. doi: 10.1080/07420520902821077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mongrain V, Dumont M. Increased homeostatic response to behavioral sleep fragmentation in morning types compared to evening types. Sleep. 2007;30:773–780. doi: 10.1093/sleep/30.6.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mongrain V, Carrier J, Dumont M. Chronotype and sex effects on sleep architecture and quantitative sleep EEG in healthy young adults. Sleep. 2005;28:819–827. doi: 10.1093/sleep/28.7.819. [DOI] [PubMed] [Google Scholar]
- 59.Mongrain V, Carrier J, Dumont M. Circadian and homeostatic sleep regulation in morningness-eveningness. J Sleep Res. 2006;15:162–166. doi: 10.1111/j.1365-2869.2006.00532.x. [DOI] [PubMed] [Google Scholar]
- 60.Adan A. Chronotype and personality factors in the daily consumption of alcohol and psychostimulants. Addiction. 1994;89:455–462. doi: 10.1111/j.1360-0443.1994.tb00926.x. [DOI] [PubMed] [Google Scholar]
- 61.Nakade M, Takeuchi H, Kurotani M, Harada T. Effects of meal habits and alcohol/cigarette consumption on morningness-eveningness preference and sleep habits by Japanese female students aged 18–29. J Physiol Anthropol. 2009;28:83–90. doi: 10.2114/jpa2.28.83. [DOI] [PubMed] [Google Scholar]
- 62.Prat G, Adan A. Influence of circadian typology on drug consumption, hazardous alcohol use, and hangover symptoms. Chronobiol Int. 2011;28:248–257. doi: 10.3109/07420528.2011.553018. [DOI] [PubMed] [Google Scholar]
- 63.Adan A, Lachica J, Caci H, Natale V. Circadian typology and temperament and character personality dimensions. Chronobiol Int. 2010;27:181–193. doi: 10.3109/07420520903398559. [DOI] [PubMed] [Google Scholar]
- 64.Prat G, Adan A. Relationships among circadian typology, psychological symptoms, and sensation seeking. Chronobiol Int. 2013;30:942–949. doi: 10.3109/07420528.2013.790044. [DOI] [PubMed] [Google Scholar]
- 65.Haddock CK, Jahnke SA, Poston WS, Jitnarin N, Kaipust CM, Tuley B, et al. Alcohol use among firefighters in the Central United States. Occup Med (Lond) 2012;62:661–664. doi: 10.1093/occmed/kqs162. [DOI] [PubMed] [Google Scholar]
- 66.Piazza-Gardner AK, Barry AE, Chaney E, Dodd V, Weiler R, Delisle A. Covariates of alcohol consumption among career firefighters. Occup Med (Lond) 2014;64:580–582. doi: 10.1093/occmed/kqu124. [DOI] [PubMed] [Google Scholar]
- 67.Fullerton CS, Ursano RJ, Wang L. Acute stress disorder, posttraumatic stress disorder, and depression in disaster or rescue workers. Am J Psychiatry. 2004;161:1370–1376. doi: 10.1176/appi.ajp.161.8.1370. [DOI] [PubMed] [Google Scholar]