Abstract
Objective:
Stroke frequently complicates infective endocarditis (IE). However, the temporal relationship between these diseases is uncertain.
Methods:
We performed a retrospective study of adult patients hospitalized for IE between July 1, 2007, and June 30, 2011, at nonfederal acute care hospitals in California. Previously validated diagnosis codes were used to identify the primary composite outcome of ischemic or hemorrhagic stroke during discrete 1-month periods from 6 months before to 6 months after the diagnosis of IE. The odds of stroke in these periods were compared with the odds of stroke in the corresponding 1-month period 2 years earlier, which was considered the baseline risk of stroke.
Results:
Among 17,926 patients with IE, 2,275 strokes occurred within the 12-month period surrounding the diagnosis of IE. The risk of stroke was highest in the month after diagnosis of IE (1,640 vs 17 strokes in the corresponding month 2 years prior). This equaled an absolute risk increase of 9.1% (95% confidence interval 8.6%–9.5%) and an odds ratio of 96.5 (95% confidence interval 60.1–166.0). Stroke risk was significantly increased beginning 4 months before the diagnosis of IE and lasting 5 months afterward. Similar temporal patterns were seen when ischemic and hemorrhagic strokes were considered separately.
Conclusions:
The association between IE and stroke persists for longer than previously reported. Most diagnoses of stroke and IE are made close together in time, but a period of heightened stroke risk becomes apparent several months before the diagnosis of IE and lasts for several months afterward.
Infective endocarditis (IE) occurs in 1.7 to 6.2 per 100,000 people per year in the United States and Europe.1 Stroke often complicates IE, affecting approximately 16% to 25% of patients with IE.2,3 Cerebral embolism heralding or following a diagnosis of IE substantially increases morbidity and mortality.3–5 However, knowledge is limited regarding the time period during which patients with IE face a heightened stroke risk, with reports ranging from as early as 40 days before IE is recognized to as late as 5 weeks after the start of antibiotic treatment.3,4,6–8 Recent data suggest that IE may increase stroke risk for even longer periods of time, as one European cohort study reported that patients had a moderately increased risk of embolic events up to 180 days after community-acquired bacteremia.9 We hypothesized that the risk of stroke in the setting of IE persists for longer than current data suggest. Therefore, we sought to better delineate the time period during which patients diagnosed with IE face an increased stroke risk.
METHODS
Study design.
We performed a retrospective study of the temporal relationship between IE and stroke diagnoses using administrative claims data from California. The California Office of Statewide Health Planning and Development collects data about all emergency department (ED) visits and hospital stays at nonfederal acute care hospitals in California. After quality checking, these data are provided in a deidentified format to the Agency for Healthcare Research and Quality for its Healthcare Cost and Utilization Project.10 A unique record linkage number for each patient allows longitudinal tracking of ED encounters and hospitalizations.11 Because this publicly available database includes only deidentified data, our institutional review board certified our study as exempt from review.
Patients.
We identified all patients hospitalized with IE between July 1, 2007, and June 30, 2011, using the following previously validated ICD-9-CM codes for infective endocarditis: 421.0 (acute and subacute infective endocarditis), 421.1 (endocarditis, valve unspecified, in diseases classified elsewhere), 421.9 (acute endocarditis, unspecified), and 424.9 (endocarditis, valve unspecified). These codes have been frequently used in prior studies of endocarditis and have a positive predictive value of 81% and a sensitivity of 93%12–16 for IE based on the modified Duke criteria.17 Patients younger than 18 years of age were excluded because IE in children has been recognized as a different clinical entity from IE in adults, associated with different predisposing factors (e.g., congenital heart disease) and presenting far less often with extracardiac manifestations.18 To maximize our ability to assess follow-up ED visits and admissions, we excluded patients who were not California residents.
Outcomes.
In accordance with a validated algorithm, ischemic stroke was defined as ICD-9-CM codes 433.x1, 434.x1, or 436 in any diagnosis code position in the absence of a primary discharge code for rehabilitation (V57) or any codes for subarachnoid hemorrhage (430), intracerebral hemorrhage (431), or trauma (800–804 and 850–854).19 Hemorrhagic stroke was defined by the presence of discharge codes for intracerebral hemorrhage (431) or subarachnoid hemorrhage (430) in the absence of a primary discharge code for rehabilitation (V57) or trauma (800–804 and 850–854). This algorithm has been validated to have a sensitivity of ≥82% and a specificity of ≥93% for both ischemic and hemorrhagic stroke subtypes.19 To focus on incident diagnoses, we included only the first recorded diagnosis of IE or stroke. In our primary analysis, we included all ischemic and hemorrhagic strokes; in secondary analyses, we considered ischemic strokes separately from hemorrhagic strokes.
Statistical analysis.
We determined the odds of first-recorded stroke hospitalizations during 1-month periods from 6 months before to 6 months after IE as compared with the corresponding 1-month period 2 years earlier. In a sensitivity analysis, we used the corresponding 1-month periods starting 1 year earlier. This design allowed us to compare the risk of stroke during the period surrounding the diagnosis of IE in relation to each patient's baseline risk of stroke well before developing IE. Since we had data from January 1, 2005, through December 31, 2011, we excluded patients with a first-recorded IE diagnosis before July 1, 2007, or after June 30, 2011, so as to have full data on the 6 months before and after the IE diagnosis and the accompanying time period 2 years prior. Absolute risks and odds ratios (ORs) were calculated using a Mantel-Haenszel estimator for matched data. The p values were not adjusted for multiple comparisons. All statistical analyses were performed with Stata/MP, version 13 (StataCorp, College Station, TX).
RESULTS
Among 17,926 patients with IE, 2,275 developed a stroke during the 12-month period surrounding the diagnosis of IE. Of these patients, 1,877 (82.5%) had an ischemic stroke diagnosis, 312 (13.7%) had a hemorrhagic stroke diagnosis, and 86 (3.8%) had a concurrent ischemic and hemorrhagic stroke diagnosis. Patients with stroke more often had vascular risk factors and markers of more severe IE (table 1). Stroke risk was highest in the month following the diagnosis of IE as compared with the same 1-month period 2 years earlier (1,640 events vs 17). This corresponded to an absolute increase in risk of 9.1% (95% confidence interval [CI] 8.6%–9.5%) and an OR of 96.5 (95% CI 60.1–166.0) (table 2). The risk of stroke was significantly elevated from the fourth month before the IE diagnosis (OR 3.1; 95% CI 1.6–6.5) through the fifth month afterward (OR 2.6; 95% CI 1.4–5.2) (figure) (table 2).
Table 1.
Baseline characteristics of patients with infective endocarditis, stratified by the occurrence of strokea
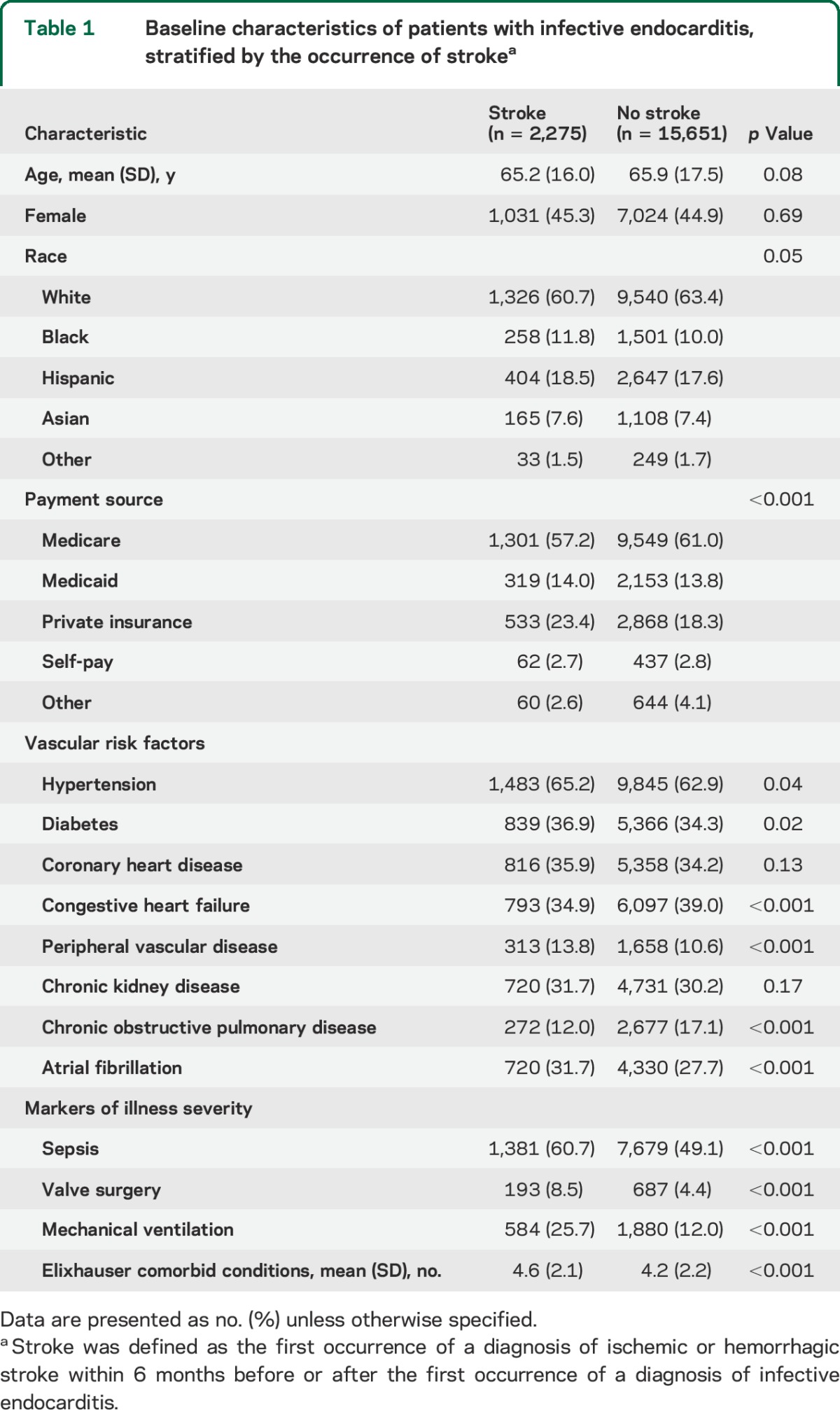
Table 2.
OR and absolute risk of stroke for 1-month intervals before and after the diagnosis of IE

Figure. Temporal relationship between infective endocarditis and stroke.
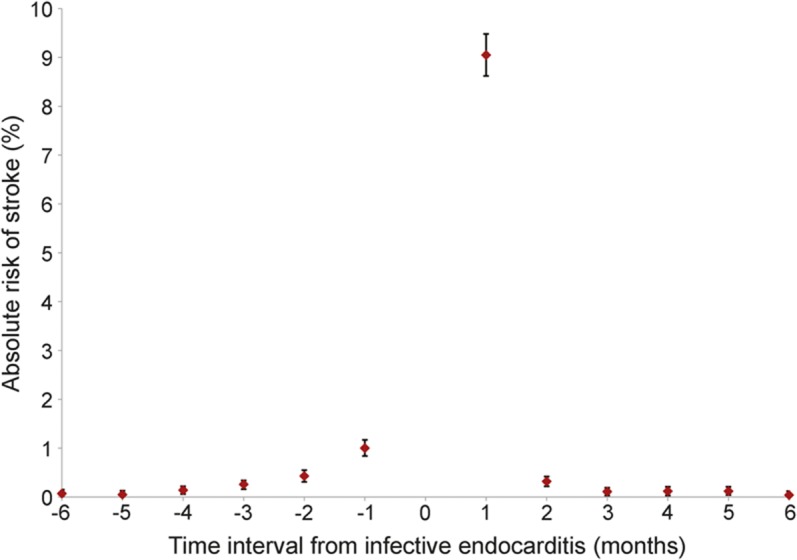
Absolute increases in stroke risk during the 6 months before through 6 months after a diagnosis of infective endocarditis.
Similar to all strokes, the risk of ischemic stroke was highest in the month after the IE diagnosis (1,376 events vs 17), corresponding to an absolute increase in risk of 7.6% (95% CI 7.2%–8.0%) and an OR of 80.9 (95% CI 50.4–139.4) (table 2). Ischemic stroke risk increased in the fourth month before the IE diagnosis (OR 2.9; 95% CI 1.5–6.2) and persisted through the third month afterward (OR 2.3; 95% CI 1.1–4.9) (table 2). A similar temporal pattern was found for hemorrhagic stroke, although the peak increase in absolute risk during the month after IE was more modest (1.8%; 95% CI 1.6%–2.0%) than for ischemic stroke (table 2). Similar patterns were seen in sensitivity analyses in which the likelihood of stroke was compared with the same period 1 year earlier.
DISCUSSION
Using a large, population-based cohort, we found that stroke risk began to increase approximately 4 months before a diagnosis of IE, peaked in the 1-month period after IE, and then attenuated and normalized by 5 months afterward. Ischemic stroke was much more common than hemorrhagic stroke, although both were dramatically increased (more than 80-fold) in the 1-month period after IE. The heightened stroke risk in the 1-month period after IE is consistent with the results of prior studies, which show that the majority of IE-related strokes occur in the immediate period surrounding IE diagnosis and treatment.3
Our results build on prior studies regarding the temporal association between stroke and IE. Previous reports describe strokes occurring up to 40 days before the diagnosis of IE and as late as 5 weeks after the initiation of antibiotics, but these studies were from significantly smaller cohorts.3,4,6 More recently, a European cohort study found a substantially increased risk of myocardial infarction or ischemic stroke within 30 days of community-acquired bacteremia and a modestly increased risk from 31 to 180 days after bacteremia.9 Although not all patients with bacteremia develop endocarditis, these results support our finding that IE increases stroke risk for longer periods of time than previously considered.
In addition to a prolonged period of increased stroke risk after the diagnosis of IE, we found that the stroke risk began to increase approximately 4 months before the IE diagnosis was established. In some cases, strokes occurring before the diagnosis of IE may be a manifestation of occult IE, particularly the subacute form.6–8 Other cases of stroke that precede IE may reflect the presence of shared risk factors for both stroke and IE, such as cardiac valve surgery, or poststroke risk factors that may predispose to IE, such as poststroke immunodepression or use of central venous catheters after stroke.20–25 The nature of our data prevents us from determining the mechanistic basis for these findings, but future analyses should aim to delineate the specific pathophysiologic processes underlying the complex relationship between IE and stroke.
The increased stroke risk before the diagnosis of IE supports a potential causal link between inflammation and stroke. Research has shown that inflammatory mechanisms contribute to the pathogenesis and progression of atherosclerosis, plaque rupture, and thrombotic events.26,27 Furthermore, inflammatory biomarkers such as high-sensitivity C-reactive protein have been identified as predictors of stroke in various populations.28 Infections may contribute to inflammation and subsequently increase stroke risk. In addition, hospitalization for infection is associated with an elevated short-term risk of stroke,29 and serologic evidence of chronic infection has been correlated with stroke risk.30 In our cohort, preceding infections such as dental caries or sinusitis may have directly led to IE, but also could have increased stroke risk via inflammatory mechanisms.
Our study has several important limitations. First, our study design and the nature of our data precluded us from resolving the causal direction of the relationship between IE and stroke. Our results indicate that the temporal relationship between IE and stroke is more complex than currently appreciated, but further work is needed to elucidate the mechanisms at play. Second, our matched design relied on estimates of baseline stroke risk from 2 years before the diagnosis of IE, and it is therefore possible that our estimates of stroke risk were confounded by the interim effects of aging or the development of other illnesses unrelated to IE. We think this is unlikely to explain our findings because our results were not substantially changed in sensitivity analyses in which stroke risk was compared to a period 1 year before IE. Third, we lacked data on ambulatory visits, and therefore captured only cases of IE or stroke resulting in hospitalization. However, these serious illnesses would typically result in hospitalization, and therefore it is unlikely that we misascertained a significant number of diagnoses. Fourth, we were unable to resolve the temporal association of cases of IE and stroke that were diagnosed during the same hospitalization, and therefore the temporal extent of the association between IE and stroke may be even more dispersed than we have found. Finally, because patients were identified using administrative claims data, we were unable to account for certain clinical information such as stroke mechanism, type and duration of antibiotic usage, type of valve replacement (bioprosthetic vs mechanical), temporal relationship between valve surgery and stroke, type of microorganism, and vegetation location and size.
We have found that the association between IE and stroke persists for longer than previously reported. The highest risk of stroke is in the 1 month following a diagnosis of IE, but a period of increased stroke risk becomes apparent several months before the diagnosis of IE and lasts for several months afterward.
GLOSSARY
- CI
confidence interval
- ED
emergency department
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- IE
infective endocarditis
- OR
odds ratio
AUTHOR CONTRIBUTIONS
Alexander E. Merkler conceived and designed the study, analyzed and interpreted the data, and drafted and revised the manuscript for intellectual content. Stacy Y. Chu designed the study, analyzed and interpreted the data, and drafted and revised the manuscript for intellectual content. Michael P. Lerario analyzed and interpreted the data, and revised the article critically for important intellectual content. Babak B. Navi designed the study, analyzed and interpreted the data, and revised the article critically for important intellectual content. Hooman Kamel designed the study, analyzed and interpreted the data, and revised the article critically for important intellectual content.
STUDY FUNDING
Supported by an NIH K23 grant (Kamel) from the National Institute of Neurological Disorders and Stroke, an NIH KL2 grant administered through the Weill Cornell Clinical and Translational Science Center (Navi), the Michael Goldberg Stroke Research Fund (Kamel), and the Florence Gould Endowment for Discovery in Stroke (Navi).
DISCLOSURE
A. Merkler, S. Chu, and M. Lerario report no disclosures relevant to the manuscript. B. Navi is supported by grant KL2TR000458-06 from the NIH administered through the Weill Cornell Clinical and Translational Science Center and the Florence Gould Endowment for Discovery in Stroke. H. Kamel is supported by grant K23NS082367 from the National Institute of Neurological Disorders and Stroke and the Michael Goldberg Stroke Research Fund. Outside the submitted work, Dr. Kamel has served on a medical advisory board and on a speakers bureau for Genentech and is an associate editor for Journal Watch Neurology. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Mylonakis E, Calderwood SB. Infective endocarditis in adults. N Engl J Med 2001;345:1318–1330. [DOI] [PubMed] [Google Scholar]
- 2.Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis–Prospective Cohort Study. Arch Intern Med 2009;169:463–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.García-Cabrera E, Fernández-Hidalgo N, Almirante B, et al. Neurologic complications of infective endocarditis: risk factors, outcome, and impact of cardiac surgery: a multicenter observational study. Circulation 2013;127:2272–2284. [DOI] [PubMed] [Google Scholar]
- 4.Dickerman SA, Abrutyn E, Barsic B, et al. The relationship between the initiation of antimicrobial therapy and the incidence of stroke in infective endocarditis: an analysis from the ICE Prospective Cohort Study (ICE-PCS). Am Heart J 2007;154:1086–1094. [DOI] [PubMed] [Google Scholar]
- 5.Novy E, Sonneville R, Mazighi M, et al. Neurological complications of infective endocarditis: new breakthroughs in diagnosis and management. Med Mal Infect 2013;43:443–450. [DOI] [PubMed] [Google Scholar]
- 6.Epaulard O, Roch N, Potton L, Pavese P, Brion JP, Stahl JP. Infective endocarditis-related stroke: diagnostic delay and prognostic factors. Scand J Infect Dis 2009;41:558–562. [DOI] [PubMed] [Google Scholar]
- 7.Thuny F, Avierinos JF, Tribouilloy C, et al. Impact of cerebrovascular complications on mortality and neurologic outcome during infective endocarditis: a prospective multicentre study. Eur Heart J 2007;28:1155–1161. [DOI] [PubMed] [Google Scholar]
- 8.Heiro M, Nikoskelainen J, Engblom E, Kotilainen E, Marttila R, Kotilainen P. Neurologic manifestations of infective endocarditis: a 17-year experience in a teaching hospital in Finland. Arch Intern Med 2000;160:2781–2787. [DOI] [PubMed] [Google Scholar]
- 9.Dalager-Pedersen M, Søgaard M, Schønheyder HC, Nielsen H, Thomsen RW. Risk for myocardial infarction and stroke after community-acquired bacteremia: a 20-year population-based cohort study. Circulation 2014;129:1387–1396. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality. Healthcare cost and utilization project. Available at: http://hcupnet.ahrq.gov. Accessed August 20, 2014.
- 11.Agency for Healthcare Research and Quality. Hcup methods series: methodological issues when studying readmissions and revisits using hospital administrative data. Available at: http://www.hcup-us.ahrq.gov/reports/methods/2011_01.pdf. Accessed August 20, 2014.
- 12.Cabell CH, Heidenreich PA, Chu VH, et al. Increasing rates of cardiac device infections among Medicare beneficiaries: 1990–1999. Am Heart J 2004;147:582–586. [DOI] [PubMed] [Google Scholar]
- 13.Rogers AM, Schiller NB. Impact of the first nine months of revised infective endocarditis prophylaxis guidelines at a university hospital: so far so good. J Am Soc Echocardiogr 2008;21:775. [DOI] [PubMed] [Google Scholar]
- 14.Mendiratta P, Tilford JM, Prodhan P, Cleves MA, Wei JY. Trends in hospital discharge disposition for elderly patients with infective endocarditis: 1993 to 2003. J Am Geriatr Soc 2009;57:877–881. [DOI] [PubMed] [Google Scholar]
- 15.Fedeli U, Schievano E, Buonfrate D, Pellizzer G, Spolaore P. Increasing incidence and mortality of infective endocarditis: a population-based study through a record-linkage system. BMC Infect Dis 2011;11:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bikdeli B, Wang Y, Kim N, Desai MM, Quagliarello V, Krumholz HM. Trends in hospitalization rates and outcomes of endocarditis among Medicare beneficiaries. J Am Coll Cardiol 2013;62:2217–2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000;30:633–638. [DOI] [PubMed] [Google Scholar]
- 18.Ferrieri P, Gewitz MH, Gerber MA, et al. Unique features of infective endocarditis in childhood. Pediatrics 2002;109:931–943. [DOI] [PubMed] [Google Scholar]
- 19.Tirschwell DL, Longstreth WT. Validating administrative data in stroke research. Stroke 2002;33:2465–2470. [DOI] [PubMed] [Google Scholar]
- 20.Klehmet J, Harms H, Richter M, et al. Stroke-induced immunodepression and post-stroke infections: lessons from the preventive antibacterial therapy in stroke trial. Neuroscience 2009;158:1184–1193. [DOI] [PubMed] [Google Scholar]
- 21.Haeusler KG, Schmidt WU, Föhring F, et al. Cellular immunodepression preceding infectious complications after acute ischemic stroke in humans. Cerebrovasc Dis 2008;25:50–58. [DOI] [PubMed] [Google Scholar]
- 22.Hug A, Dalpke A, Wieczorek N, et al. Infarct volume is a major determiner of post-stroke immune cell function and susceptibility to infection. Stroke 2009;40:3226–3232. [DOI] [PubMed] [Google Scholar]
- 23.Bucerius J, Gummert JF, Borger MA, et al. Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg 2003;75:472–478. [DOI] [PubMed] [Google Scholar]
- 24.Sykora M, Diedler J, Poli S, et al. Autonomic shift and increased susceptibility to infections after acute intracerebral hemorrhage. Stroke 2011;42:1218–1223. [DOI] [PubMed] [Google Scholar]
- 25.Alsumrain M, Melillo N, Debari VA, et al. Predictors and outcomes of pneumonia in patients with spontaneous intracerebral hemorrhage. J Intensive Care Med 2013;28:118–123. [DOI] [PubMed] [Google Scholar]
- 26.Elkind MS. Inflammatory mechanisms of stroke. Stroke 2010;41:S3–S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paoletti R, Gotto AM, Hajjar DP. Inflammation in atherosclerosis and implications for therapy. Circulation 2004;109:20–26. [DOI] [PubMed] [Google Scholar]
- 28.Kaptoge S, Di Angelantonio E, Lowe G, et al. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet 2010;375:132–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elkind MS, Carty CL, O'Meara ES, et al. Hospitalization for infection and risk of acute ischemic stroke: the Cardiovascular Health Study. Stroke 2011;42:1851–1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elkind MS, Ramakrishnan P, Moon YP, et al. Infectious burden and risk of stroke: the Northern Manhattan Study. Arch Neurol 2010;67:33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]


