Sensations of self-motion and vertigo are common among patients and technologists near MRI scanners and especially near stronger magnetic fields.1,2 It was recently discovered that all humans with intact vestibular function have nystagmus the entire time they are in a 7T MRI. This nystagmus is due to a Lorentz force arising from the interaction between the MRI magnetic field and normal ionic currents in the inner ear, which induces labyrinthine stimulation by pushing the endolymph onto the semicircular canal cupula.3–5 The force scales with magnetic field strength, but nystagmus can be seen in magnetic fields of strengths as low as 1.5T.3
Case report.
Following a fall in February 2009, a 60-year-old woman underwent a head CT scan and an incidental pituitary macroadenoma was found. MRI revealed a sellar and suprasellar lesion extending into the right cavernous sinus, measuring 1.6 × 1.6 × 1.4 cm. Initially, this nonsecreting tumor was managed expectantly but on follow-up imaging the mass increased in size and displaced the optic chiasm. In November 2013, the tumor was resected through an endoscopic endonasal approach using stereotactic navigation.
During surgery, a pinhole CSF leak was identified and repaired using multiple layers. Postoperatively, the patient was monitored in the neurocritical care unit, where she had no nausea and no evidence of nasal or oropharyngeal drainage. Thirty hours after surgery, she was taken for a routine, postoperative MRI. While entering the 3T MRI scanner, she shut her eyes and experienced a transient sense of self-motion. After exiting the MRI and opening her eyes, she was overcome by nausea and vertigo, followed by vomiting. While the vertigo resolved within seconds, the vomiting was immediately followed by persistent, clear nasal discharge. The fluid was positive for β-2 transferrin, confirming a postoperative CSF leak. Management of this CSF leak included placement of a temporary lumbar drain. Formal intracranial pressure monitoring excluded intracranial hypertension or hypotension. She had no hearing complaints. She was discharged home feeling well on postoperative day 9.
Results.
A surveillance MRI was performed 8 months later using the same magnetic field strength (3T). During a time when no images were being taken, her eye movements were recorded inside the magnetic field in darkness (preventing fixation) using infrared video-oculography (figure). She showed an increase in a small baseline horizontal nystagmus in the MRI scanner and stronger nystagmus when taken out of the MRI scanner, consistent with labyrinthine stimulation from the magnetic field and subsequent adaptation.3 The eyes drifted right and beat left inside the magnet and reversed direction upon exiting, drifting left and beating right. She again experienced a transient sense of motion upon both entering and exiting the magnet, though this time without nausea or vomiting.
Figure. Nystagmus around a 3T MRI scanner.
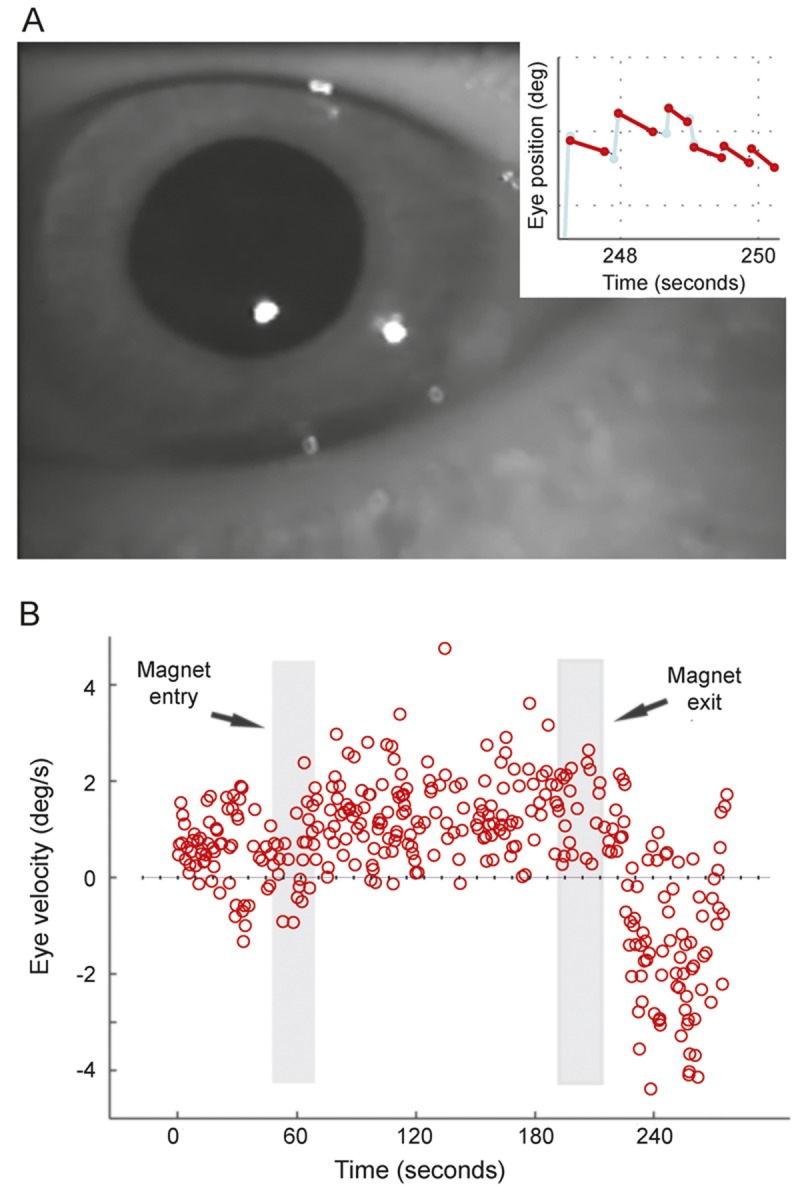
Eye movements were measured in darkness with infrared light by tracking the pupil (A). Characteristic saw tooth (jerk) pattern of nystagmus was observed (inset). (B) Eye velocity over time is shown. Dots represent eye velocity of the slow-phase component of nystagmus. The eye drifts to the left (up on graph) inside the magnet, then reverses direction—drifting to the right and beating to the left—immediately after exiting the magnet.
Discussion.
The perception of vertigo in an MRI scanner usually lasts less than a minute,3 as occurred in this patient. The nystagmus, however, persists while the subject is in the magnetic field, though it may partially adapt and decrease in intensity. Upon exiting the magnet, there is a characteristic direction reversal for both perception and nystagmus, which can be quite strong (figure).3,4 Labyrinthine stimulation can induce nausea and vomiting. In this case, labyrinthine stimulation by the MRI magnetic field caused vomiting, and the associated increase in intracranial pressure resulted in reopening of a CSF leak. This patient had a negative Dix-Hallpike examination, suggesting her symptoms were not caused by benign paroxysmal positional vertigo, which can be induced after being supine for a prolonged period. She reported a history motion sickness that may have predisposed her to the nausea and vomiting after the unnatural labyrinthine stimulation in the MRI.
MRI scanners are considered safe if guidelines are followed regarding metal exposure and use of IV contrast. We present a novel case of a patient experiencing a complication due to vertigo and vomiting induced from labyrinthine stimulation in an MRI scanner. In this instance, the CSF leak, which was reopened by the vomiting associated with the MRI, considerably prolonged her hospitalization. In the future, and especially as stronger MRI scanners are applied clinically, one might consider prophylactic antiemetics in patients who must undergo an MRI, particularly if they have a propensity for motion sickness or have had a procedure in which vomiting might induce a complication. Further study is necessary to determine how frequently vomiting occurs during MRI and under what conditions antiemetic therapy might be prophylactically administered.
Acknowledgments
Acknowledgment: The authors thank Dale Roberts for help with data collection and Krysta Bearish, PA, and Yemissi Sanni for assistance in coordinating the patient's care.
Footnotes
Author contributions: Bryan K. Ward: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and final approval, acquisition of data, study supervision. David S. Zee: drafting/revising the manuscript, study concept or design, accepts responsibility for conduct of research and final approval. David Solomon: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and final approval, acquisition of data. Gary L. Gallia: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and final approval, study supervision. Douglas D. Reh: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and final approval, study supervision.
Study funding: No targeted funding reported.
Disclosure: The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
References
- 1.Schaap K, Christopher-de Vries Y, Mason CK, de Vocht F, Portengen L, Kromhout H. Occupational exposure of healthcare and research staff to static magnetic stray fields from 1.5–7 Tesla MRI scanners is associated with reporting of transient symptoms. Occup Environ Med 2014;71:423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heilmaier C, Theysohn JM, Maderwald S, Kraff O, Ladd ME, Ladd SC. A large-scale study on subjective perception of discomfort during 7 and 1.5T MRI examinations. Bioelectromagnetics 2011;32:610–619. [DOI] [PubMed] [Google Scholar]
- 3.Roberts DC, Marcelli V, Gillen JS, Carey JP, Della Santina CC, Zee DS. MRI magnetic field stimulates rotational sensors of the brain. Curr Biol 2011;21:1635–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glover PM, Li Y, Antunes A, Mian OS, Day BL. A dynamic model of the eye nystagmus response to high magnetic fields. Phys Med Biol 2014;59:631–645. [DOI] [PubMed] [Google Scholar]
- 5.Ward BK, Roberts DC, Della Santina CC, Carey JP, Zee DS. Magnetic vestibular stimulation in subjects with unilateral labyrinthine disorders. Front Neurol 2014;5:28. [DOI] [PMC free article] [PubMed] [Google Scholar]


