Abstract
Context
Little is known about the impact of low health literacy among patients with heart failure (HF), a condition that requires self-management and frequent interactions with the healthcare system.
Objective
Evaluate the association between low health literacy and all-cause rehospitalization and mortality among outpatients with HF.
Design and Setting
Retrospective cohort study performed at Kaiser Permanente Colorado, an integrated managed care organization. Patients with HF were identified between Jan, 2001 and May, 2008 and followed for a mean of 1.2 years. Patients were surveyed. Health literacy was assessed using three established screening questions and categorized as adequate or low.
Patients
Outpatients with HF.
Main Outcomes
All-cause mortality and hospitalization.
Results
The survey response rate was 72%. Of 1494 patients, 262 (17.5%) had low health literacy. Patients with low health literacy were older, of lower socioeconomic status, less likely to have at least a high school education and had higher rates of coexisting illnesses. In multivariable Cox regression, low health literacy was independently associated with higher mortality (unadjusted 17.6% vs. 6.3%; adjusted hazard ratio [HR]: 1.61; 95% CI 1.06–2.43; p=0.026), but not hospitalization (30.5% vs. 23.2%; HR:1.04; 95% CI 0.79–1.37; p=0.760).
Conclusions
Among patients with HF in an integrated managed care organization, low health literacy was significantly associated with higher all-cause mortality.
INTRODUCTION
As defined by the Institute of Medicine, health literacy is “the degree to which individuals can obtain, process and understand basic health information and services needed to make appropriate health decisions.”(1) Because health literacy encompasses more than simply the ability to read, patients may have proficient general literacy but low health literacy. Many Americans and as many as one in three Medicare enrollees have low health literacy.(2)The economic implications of low health literacy are substantial, in some estimates accounting for up to 5% of healthcare costs annually.(3)
Heart failure (HF) is a common and complex chronic disease with high morbidity and mortality and thus has the attention of policy-makers as a high-priority condition. Although patients with HF are frequently hospitalized, much of HF care is performed on a daily basis by individual patients outside of the hospital. This self-care requires integration and application of knowledge and skills.(4) Thus, an adequate level of health literacy is likely critical in ensuring patient compliance and proficiency in self-management.
Little is known about the association between health literacy and outcomes among patients with HF.(5) While some studies suggest an association between health literacy and outcomes in relatively healthy general populations, these studies evaluated health literacy with complex time-consuming measures that are not conducive to routine use in clinical practice.(6–9) Further, prior studies were not able to adjust adequately for coexisting illnesses, which are important factors related to hospitalization and mortality. Therefore, the objective of this study was to evaluate the association between low health literacy and all-cause hospitalization and mortality among an outpatient population of patients with HF using three brief screening questions that can easily be incorporated into clinical practice.
METHODS
Study Population
All patients were enrolled in Kaiser Permanente of Colorado (KPCO), a nonprofit managed care organization that provides medical services (inpatient, outpatient, pharmacy) to more than 480,000 persons. The study cohort included patients with a primary hospital discharge diagnosis for HF (International Classification of Diseases Ninth Revision [ICD-9] codes of 428.xx, 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93 or a Diagnosis Related Group [DRG] of 127), patients who had at least two secondary hospital discharge diagnoses of HF where the primary discharge diagnosis was related to cardiovascular disease (ICD-9 codes of 410, 412, 413 or 414), or three or more emergency department visits with a diagnosis of HF between January 1, 2001 and May 31, 2008. Prior literature suggests that these administrative coding algorithms have a high positive predictive value for a diagnosis of HF when validated with chart review.(10–12) Patients were followed through March 31, 2009 for subsequent events.
Survey
The survey was mailed, with a second mailing sent to non-responders. Those not responding to the second mailing were called. Up to ten attempts were made to contact non-responders. If participants were reached, they were given the option of completing the survey by telephone interview.
Health Literacy
Health literacy was assessed using three brief screening questions with established validity for identifying patients with limited and marginal health literacy skills.(13–16) The questions were: 1) “How often do you have someone help you read hospital materials?” 2) “How often do you have problems learning about your medical condition because of difficulty reading hospital materials?” and 3) “How confident are you filling out forms by yourself?” Each question was scored by patients on a 5-point scale in which higher scores indicated lower literacy. The performance characteristics of each of these questions has been previously evaluated and compared against the Short-Test of Functional Health Literacy in Adults (S-TOFHLA) or Rapid Estimate of Adult Literacy in Medicine (REALM) as the reference standard.(13–17)
Health literacy was evaluated as a continuous, ordinal and dichotomous variable. The different specifications were found to explain similar amounts of variance, so the simplest specification (adequate vs. low) was used in the statistical models. Based on prior literature (13;17), scores were summed and dichotomized a priori such that a total score >10 was categorized as low health literacy and a score ≤ 10 was adequate health literacy.
Outcomes
The primary outcomes of interest were all-cause mortality and all-cause hospitalization. These outcomes were chosen because they are patient centered and are quality measures used by the Centers for Medicare and Medicaid (CMS) for hospital HF-related quality assessment and reporting. Therefore, these outcomes are important targets for quality improvement efforts. Vital status was ascertained from KPCO databases and validated by comparison with death certificates registered with the State of Colorado. Hospitalizations were identified using claims data. Hospitalizations outside of the managed care organization are also captured in the administrative claims data.
Other Variables
The following covariates were also collected and included in the model: age, gender, race, socioeconomic status, self-reported education level, self-reported physical function, residential status (independent vs. nursing facility or hospice care), serum creatinine, left ventricular ejection fraction, year of cohort entry and history of the following coexisting illnesses: angina, liver disease, chronic obstructive pulmonary disease, dementia, diabetes, history of myocardial infarction, hypertension, major psychiatric disorder, metastatic cancer, peripheral vascular disease, stroke and valvular heart disease. All covariates were determined at the time of the survey, except for residence in a nursing facility or enrollment in hospice, which was determined at any time in the following year.
Patient demographics, residence in a nursing facility, enrollment in hospice and laboratory data were derived from automated KPCO databases. Comorbidities were defined using ICD-9 codes within KPCO automated databases. Medication dispensings were determined from automated KPCO pharmacy databases. Socioeconomic status was determined by matching residential address with census data. Low socio-economic status was defined as living in an area where at least 20% of individuals had household incomes below the poverty level, or if at least 25% of the people in that area had a high school education or less. Ejection fraction was obtained by chart review. Education level was ascertained through the survey. Physical function was assessed using the physical function subscale of the Kansas City Cardiomyopathy Questionnaire (KCCQ) which was administered as part of the survey.(18)
Statistical Analysis
To determine whether a summed unidimensional health literacy scale could be used, we evaluated whether the three questions were measuring a single construct by 1) viewing item-to-total correlations and 2) calculating Cronbach’s Alpha, which is a measure of consistency among individual items.
Among those completing the survey, 47 (3.2%) were missing 1 and 3 (0.2%) were missing 2 health literacy questions. For the few individuals answering only 1 or 2 of the 3 questions, the score for those questions was multiplied by 3 and 1.5 respectively.
Baseline characteristics were compared across levels of health literacy using the chi-square test for categorical variables and t-tests for continuous variables. The bivariate relationships between health literacy and the outcomes of all-cause mortality and hospitalization were each assessed using Kaplan-Meier survival plots using time of survey completion as time-zero and evaluated with the log-rank test. To determine the independent association of health literacy with all-cause mortality and hospitalization, multivariable Cox proportional hazards models were constructed for each outcome. All variables were selected a priori based on prior literature and clinical significance. All covariates were included in the models except for medications. Medications were not included in the models because of concerns that medication adherence might, to some extent, mediate the relationship between health literacy and outcomes. In the case of missing values for a given variable, a separate missing category was created and included in the models. The rate of missing data was less than 3% for race/ethnicity, SES, education and living status and 6% for left ventricular ejection fraction. The rate of missing data for the physical limitation scale of the KCCQ was 5%. Missing KCCQ physical limitation variables were estimated using multiple imputation. Deaths were censored in the analyses of hospitalization. The Cox proportional hazards assumption was tested and verified for all proportional hazards models by calculating and graphing Schoenfeld residuals by survival time.(19)
In addition, we tested for differences in the relationship between health literacy and outcomes among the pre-specified subgroups of those living independently versus those in a nursing facility or receiving hospice care at the time of the survey or at any point in the year following. We hypothesized that hospitalizations among patients either in nursing facilities or receiving hospice care would be independent of health literacy level because many self-care activities would be supported or assumed by others. Furthermore, we hypothesized that for those in hospice, the goals of care would focus on symptom management rather than disease management and include avoiding hospitalization. Therefore, we examined for an interaction between those living and independently and those in a nursing facility or receiving hospice care. We used the same multivariable modeling approach as the primary model, stratified by living independently versus living in a nursing facility or receiving hospice care. The statistical significance of difference among strata was tested with a two-way interaction term in the full model.
The study was approved by the Kaiser Permanente Colorado Institutional Review Board. For each analysis, the null hypothesis was evaluated at a two-sided significance level of 0.05, with 95% confidence intervals (CIs). All analyses were performed using the SAS statistical package version 9.1 (SAS Institute, Cary, NC).
RESULTS
All patients identified as having HF who were still alive between 2007 and 2008 were surveyed. Among 2,156 patients surveyed, 1,547 patients responded for a 72% response rate. Survey non-responders were older (77 yrs vs. 74 yrs; p<0.001). No statistically significant differences existed between responders and non-responders with regard to gender, race, SES or comorbidity burden. Of those completing the survey, patients were excluded if they did not complete at least one health literacy question (n=40) or if they did not have at least one year of enrollment prior to the survey date (n=13). A total of 1494 patients were included in the study cohort.
We evaluated a summed health literacy scale using all three health literacy questions. The single item-to-total correlations were 0.62, 0.53 and 0.60 for questions 1–3 respectively, and all three items were positively correlated with each other (Pearson’s correlation coefficients ranged from 0.46–0.56). The Cronbach’s Alpha for the summed score was 0.75, indicating high internal consistency. Thus, the summed scale was used for analyses.
Of the 1494 patients in the cohort, 262 (17.5%) had low health literacy. Patients with low health literacy were older, of lower socioeconomic status, and less likely to have at least a high school education (Table 1). They were also more likely to have comorbidities such as diabetes, hypertension, chronic pulmonary disease and stroke.
Table 1.
Baseline characteristics by level of health literacy.
| Total Cohort N=1494 |
Adequate Health Literacy N=1232 |
Low Health Literacy N = 262 |
p-value | |
|---|---|---|---|---|
|
| ||||
| Age: mean (SD) | 74.9 (10.7) | 74.2 (10.6) | 78.6 (10.3) | <0.001 |
|
| ||||
| Male (%) | 46.8 | 47.8 | 42.0 | 0.086 |
|
| ||||
| Race/Ethnicity | ||||
| White | 82.0 | 83.1% | 77.2 | 0.114 |
| Hispanic | 9.5 | 8.9 | 12.4 | |
| Black | 5.3 | 5.2 | 5.8 | |
| Other | 3.1 | 2.8 | 4.6 | |
| race/ethnicity missing | 2.0 | 2.2 | 1.2 | 0.273 |
|
| ||||
| Low SES (%)* | 21.4 | 19.7 | 29.3 | 0.001 |
| SES missing | 2.3 | 2.6 | 1.2 | 0.158 |
|
| ||||
| Less than High School Education (%)* | 16.5 | 12.5 | 35.0 | <0.001 |
| education missing | 1.5 | 1.7 | 0.8 | 0.261 |
|
| ||||
| Hospice or Nursing Home | 11.8 | 9.9 | 20.6 | < 0.001 |
|
| ||||
| Lives alone | 31.8 | 31.7 | 32.4 | 0.81 |
| lives alone missing | 1.5 | 1.5 | 1.2 | 0.63 |
|
| ||||
| Comorbidities | ||||
|
| ||||
| Ejection Fraction* | 0.859 | |||
| Normal | 59.1 | 58.9 | 60.4 | |
| Mild dysfunction | 13.9 | 14.1 | 12.9 | |
| Moderate dysfunction | 13.7 | 13.5 | 14.6 | |
| Severe dysfunction | 13.3 | 13.5 | 12.1 | |
| Ejection fraction missing | 6.2 | 5.7 | 8.4 | 0.097 |
|
| ||||
| Cancer | 4.1 | 3.7 | 6.1 | 0.068 |
|
| ||||
| Dementia | 11.6 | 8.6 | 25.6 | <0.001 |
|
| ||||
| Diabetes | 52.7 | 50.8 | 61.8 | 0.001 |
|
| ||||
| History of MI | 20.2 | 19.2 | 25.2 | 0.027 |
|
| ||||
| Angina | 33.2 | 32.5 | 36.3 | 0.247 |
|
| ||||
| Hypertension | 93.6 | 92.9 | 96.6 | 0.030 |
|
| ||||
| COPD | 44.5 | 42.9 | 51.9 | 0.008 |
|
| ||||
| Chronic liver disease | 2.7 | 2.4 | 4.2 | 0.093 |
|
| ||||
| PVD | 38.4 | 36.6 | 46.9 | 0.002 |
|
| ||||
| Stroke | 17.1 | 15.7 | 23.7 | 0.002 |
|
| ||||
| Psychiatric disorder | 26.4 | 24.7 | 34.7 | 0.001 |
Abbreviations: SD=standard deviation; SES=socio-economic status; MI=myocardial infarction; COPD=chronic obstructive pulmonary disease; PVD=peripheral vascular disease
The median length of follow-up was 1.2 years (IQR 0.25–1.25). There were a total of 124 deaths during follow-up, with 46 (17.6%) deaths in the low health literacy group and 78 (6.3%) deaths in the adequate health literacy group. In Kaplan Meier analysis, the unadjusted rate of mortality was higher among those with low health literacy (log rank p < 0.001, Figure 1; unadjusted HR 2.96; 95% CI 2.05–4.25). Similarly, there were a total of 366 hospitalizations during follow-up, with 80 (30.5%) hospitalizations in the low health literacy group and 286 (23.2%) hospitalizations in the adequate health literacy group. The unadjusted rate of hospitalization was higher among those with low health literacy (log rank p <0.001, Figure 2; unadjusted HR 1.45; 95% CI 1.13–1.86).
Figure 1.
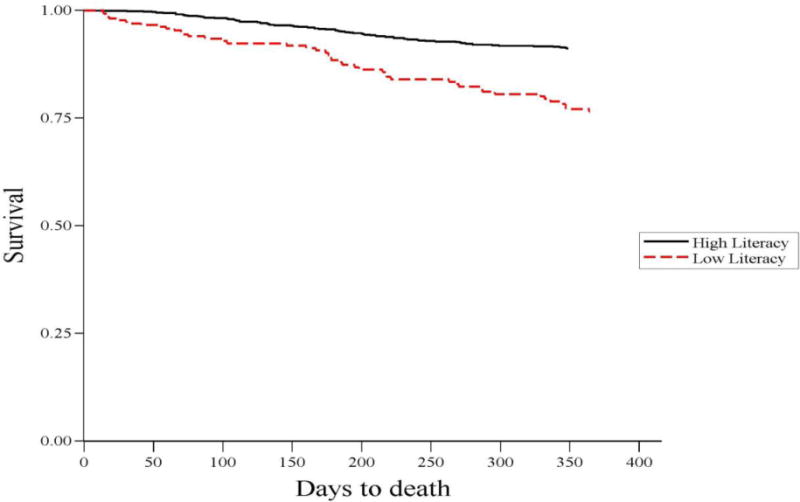
Health literacy and time to death
Figure 2.
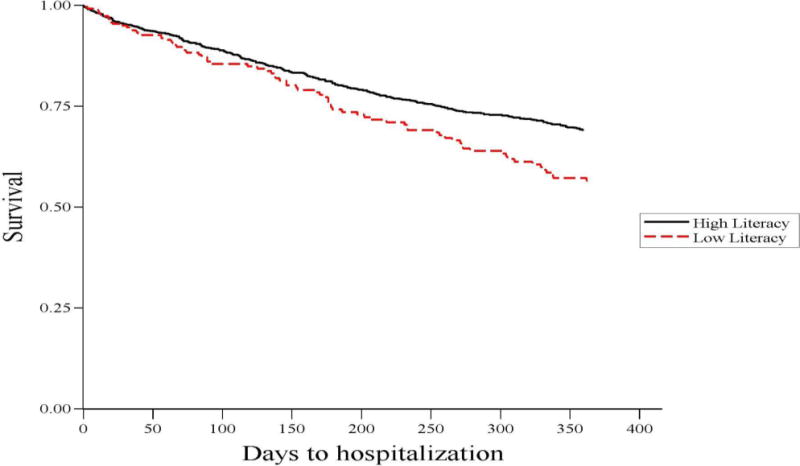
Health literacy and time to hospitalization
After adjusting for demographic variables, socioeconomic status, education, physical function, comorbidities, year of cohort entry and left ventricular ejection fraction, low health literacy remained independently associated with an increased risk of mortality (HR 1.61; 95% CI 1.06–2.43; p=0.026). In fully adjusted models, low health literacy was not significantly associated with all-cause hospitalization (HR 1.04; 95% CI 0.79–1.37; p=0.760).
In stratified analyses according to living independently versus residence in a nursing facility or receipt of hospice, there was no difference in the association between health literacy and mortality (p for interaction = 0.18). However, the association between low health literacy and all-cause hospitalization differed among the two strata. Low health literacy was associated with a lower risk of hospitalization among persons in nursing facilities or receiving hospice care (HR 0.51; 95% CI 0.30–0.87) compared with persons living independently (HR 1.26; 95% CI 0.93–1.72; p for interaction = 0.003)
DISCUSSION
In this insured population with HF, low health literacy, as assessed by three brief screening questions, was present in more than one in six patients and was associated with a significantly increased risk of mortality. These findings suggest that these questions can be used to identify patients with low health literacy who are vulnerable to adverse outcomes.
To our knowledge, no prior study has evaluated the association between health literacy and outcomes among patients with HF using brief screening questions.(5;20) Prior studies of health literacy and outcomes have used more complex, interviewer-administered instruments to measure health literacy that are impractical for use in busy clinical settings. Our results are consistent with prior studies that identified limited health literacy as a risk factor for mortality among healthy community dwelling elderly patients.(8;9) Our results are in contrast to prior studies that found a significant association with hospitalization among a younger healthier population and among community dwelling Medicare managed care enrollees.(6;7) The factors that go into the decision to hospitalize a patient are complex, and it may be that clinical factors carry more weight in determining hospitalization among this older sicker population of patients with HF. It is of interest that in stratified analyses, those with low health literacy in a nursing facility or hospice were less likely to be hospitalized. In these settings, the three screening questions may serve to identify patients with greater limitations who are more completely reliant on care takers or for whom avoiding hospitalization is a primary goal of care.
Routine assessment of health literacy may help to identify a greater number of patients at risk for adverse outcomes. Many, including the Heart Failure Society of America, suggest that health literacy levels be documented in the medical record.(5) However, methods of identifying patients with low health literacy need to be refined.(5;17) While patient demographics such as older age, minority race/ethnicity and low socioeconomic status have been correlated with low health literacy, identification using these factors alone is inadequate.(14) Further, others have demonstrated that use of education level as a surrogate measure of health literacy is also inadequate.(8) This is consistent with our finding that health literacy was associated with adverse outcomes independent of education level. Prior research studies have used more extensive questionnaires such as the Test of Functional Health Literacy in Adults (TOFHLA) or the Rapid Estimate of Adult Literacy in Medicine (REALM) to identify patients with low health literacy.(21;22) However, these measures are relatively time consuming and were designed to be administered by an interviewer, and therefore not conducive to use in routine clinical settings. Additionally, because these measures are designed for administration by means of an in-person interview, they may be more likely to invoke feelings of shame, which are common in patients with low health literacy.(23) Assessment of health literacy should be performed with care and sensitivity, as the social implications of identifying a patient of being of low health literacy could be counterproductive. Therefore, we assessed health literacy using three brief screening questions that could be easily incorporated into clinical practice. To our knowledge, this is the first study to demonstrate the prognostic value of these screening questions.
Health literacy may affect health and outcomes through a number of mediating processes, including patients’ health actions outside of the health system, such as understanding and adhering to disease management and treatment strategies. Prior studies have shown that low health literacy is associated with lower knowledge of one’s chronic disease (24), a greater misunderstanding of medications (25;26) and therefore less ability to perform successful self-management of chronic disease. Among patients with HF, the ability to read prescription labels – not a measure of health literacy per se – was associated with clinical decompensation and healthcare utilization.(27)
Low health literacy may also influence the provider-patient interaction. For example, patients with low health literacy may be reluctant to ask questions of providers and be less likely to participate in making decisions about clinical treatment.(23) Further, providers may lack competencies to help patients with low health literacy engage in a shared decision making process. At a minimum, providers should be trained to use appropriate teaching methods, reinforce education over time, and check for understanding among all patients with chronic disease. One study found that when informed of their patient’s limited health literacy, physicians were more likely to use recommended communication strategies, underscoring the importance of identifying those with low health literacy.(28) More work is needed to incorporate interactive communication and facilitate health education in the patient provider interaction, recognizing the responsibility of providers in improving these interactions.
Health literacy may also influence one’s ability to obtain health care through a lack of insurance or impaired access to care. A strength of this study is that all patients were members of Kaiser Permanente of Colorado (i.e. all were insured), minimizing differences among subjects in the availability of health care and health information. Therefore, lack of insurance and the associated lack of access to care is not a likely explanation for our results. Yet, we found that even in this population with health insurance in an integrated delivery system, the prevalence of low health literacy was one in six and was associated with adverse outcomes. The effect of low health literacy likely differs depending on characteristics of the health care system and patient population. The adverse effect of low health literacy would, if anything, exert a more pronounced effect for individuals who do not have a regular provider or who face other significant barriers to obtaining care.
Given the keen focus on reducing readmissions among patients with chronic conditions like HF with health reform, the findings of this study are particularly timely and relevant. Further, we found a strong association between low health literacy and mortality. Although this study cannot demonstrate a causal relationship between health literacy and outcomes, it does justify further investigation of health literacy as a potentially modifiable risk factor for adverse outcomes in HF. Indeed, we and others believe that an individual’s level of health literacy is not a fixed trait, but rather a state that, at least in part, reflects the summed context of the demands of one’s illness(s), the predominantly paternalistic communication style of the medical community and the complex structure of the healthcare system.(29;30) Interventions addressing literacy have been shown to be beneficial in improving quality of life and self-care and suggest possible benefits in reducing hospitalization and mortality among patients with HF, further supporting that health literacy may be a modifiable risk factor.(5;31–33)
The three brief screening questions can be used to identify HF patients to whom interventions should be targeted. Ensuring a patient understands should be a standard part of medical care for all patients. However, limited resources may preclude broad application of activities and structures to address low health literacy and interventions may need to be targeted to those at highest risk. Potential means of addressing low health literacy for patients with HF at the system and provider level have been proposed and include 1) tailoring of educational materials, 2) use of teach to goal, an iterative educational process, 3) structured follow-up and 4) inter-visit surveillance and support.(29;31) An intervention incorporating these elements is currently being evaluated in an ongoing multicenter trial.(31)
Several factors should be considered in the interpretation of our findings. First, we did not use a more detailed tool to validate low health literacy, and the three brief questions may reflect other constructs or be markers of impaired vision, frailty or cognitive impairment. However, even if these three questions measure other constructs, they can easily be incorporated into routine practice and are useful for identifying higher-risk patients. Further, to the extent that the 3-question survey may be more specific than sensitive for literacy compared with more detailed instruments as the criterion standard, we would expect that our results would be biased towards the null.(13;17) Second, our study population consisted of members of a managed care organization which may limit the generalizability of our findings. However, as previously discussed, we would expect that the effect of low health literacy would, if anything, be attenuated in this population and may be even greater in different populations. Third, this study was performed only among English speaking patients and may not be generalizable to non-English speakers. Prior studies have found that health literacy is even poorer among non-English speakers.(7;8) However, the exclusion of those who do not speak English removes language barriers as potential confounders. Finally, responder bias is a natural limitation of any survey study. However, the survey response rate was high, and responders and non-responders did not differ with regard to gender, race, SES or comorbidity burden.
In conclusion, this study demonstrates that even among those with health insurance and access to health information, low health literacy as assessed by three brief screening questions is associated with higher mortality. This finding supports efforts to determine whether interventions to screen for and address low health literacy can improve important health outcomes in HF.
Acknowledgments
Funding/Support: Dr Pamela Peterson was supported by an American Heart Association Pharmaceutical Roundtable grant 067001N. Dr. Chan is supported by a Career Development Grant Award (K23HL102224) from the NHLBI.
Footnotes
Dr. Peterson had full access to all of the data in the study and takes full responsibility for the integrity of the data and accuracy of the analysis.
Study Concept and Design: Peterson, Magid, Masoudi
Acquisition of Data: Shetterly, Clarke
Analysis and Interpretation of Data: Peterson, Shetterly, Clarke, Bekelman, Chan, Allen, Matlock, Magid, Masoudi
Drafting of Manuscript: Peterson, Masoudi
Critical Revision of Manuscript for Important Intellectual Content: Peterson, Bekelman, Chan, Allen, Matlock, Magid, Masoudi
Statistical Analysis: Shetterly, Clarke
Obtained Funding: Magid, Masoudi
Financial Disclosures: Dr. Frederick Masoudi has contracts with the Oklahoma Foundation for Medical Quality and the American College of Cardiology Foundation. Dr. Larry Allen serves as a consultant for Amgen/Cytokinetics and for the Robert Wood Johnson Foundation.
Role of Sponsors: None of the funders had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. The views in this article are those of the authors and do not necessarily reflect the views of the Department of Veterans Affairs.
References
- 1.Institute of Medicine. A Prescription to End Confusion. Washington, DC: National Academy Press; 2004. Ref Type: Report. [Google Scholar]
- 2.Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006-483) U.S. Departmentof Education; Washington, DC: 2006. National Center for Education Statistics. Ref Type: Report. [Google Scholar]
- 3.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. Journal of General Internal Medicine. 2005;20(2):175–184. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281(6):545–51. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 5.Eichler K, Wieser S, Brugger U. The costs of limited health literacy: a systematic review. International Journal of Public Health. 2009;54(5):313–24. doi: 10.1007/s00038-009-0058-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riegel B, Moser DK, Anker SD, Appel LJ, Dunbar SB, Grady KL, et al. State of the Science: Promoting Self-Care in Persons With Heart Failure: A Scientific Statement From the American Heart Association. Circulation. 2009;120(12):1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 7.Evangelista LS, Rasmusson KD, Laramee AS, Barr J, Ammon SE, Dunbar S, et al. Health Literacy and the Patient With Heart Failure–Implications for Patient Care and Research: A Consensus Statement of the Heart Failure Society of America. Journal of Cardiac Failure. 2010;16(1):9–16. doi: 10.1016/j.cardfail.2009.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 9.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158(2):166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 10.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165(17):1946–52. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 11.DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. Journal of General Internal Medicine. 2004;(19):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knmler T, Gislason GH, Kirk V, Bay M, Nielsen OW, K°ber L, et al. Accuracy of a heart failure diagnosis in administrative registers. European Journal of Heart Failure. 2008;10(7):658–660. doi: 10.1016/j.ejheart.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 13.Lee DSM*, Donovan LM, Austin PCP, Gong YM, Liu PPM, Rouleau JLM, et al. Comparison of Coding of Heart Failure and Comorbidities in Administrative and Clinical Data for Use in Outcomes Research. Medical Care. 2005;43(2):182–188. doi: 10.1097/00005650-200502000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Go AS, Yang J, Ackerson LM, Lepper K, Robbins S, Massie BM, et al. Hemoglobin Level, Chronic Kidney Disease, and the Risks of Death and Hospitalization in Adults With Chronic Heart Failure: The Anemia in Chronic Heart Failure: Outcomes and Resource Utilization (ANCHOR) Study. Circulation. 2006;113(23):2713–2723. doi: 10.1161/CIRCULATIONAHA.105.577577. [DOI] [PubMed] [Google Scholar]
- 15.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family Medicine. 2004;36(8):588–94. [PubMed] [Google Scholar]
- 16.Wallace LS, Rogers ES, Roskos SE, Holiday DB, Weiss BD. BRIEF REPORT: Screening Items to Identify Patients with Limited Health Literacy Skills. Journal of General Internal Medicine. 2006;21(8):874–877. doi: 10.1111/j.1525-1497.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wallace LS, Cassada DC, Rogers ES, Freeman MB, Grandas OH, Stevens SL, et al. Can Screening Items Identify Surgery Patients at Risk of Limited Health Literacy? Journal of Surgical Research. 2007;140(2):208–213. doi: 10.1016/j.jss.2007.01.029. [DOI] [PubMed] [Google Scholar]
- 18.Chew L, Griffin J, Partin M, Noorbaloochi S, Grill J, Snyder A, et al. Validation of Screening Questions for Limited Health Literacy in a Large VA Outpatient Population. Journal of General Internal Medicine. 2008;23(5):561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powers BJ, Trinh JV, Bosworth HB. Can This Patient Read and Understand Written Health Information? JAMA. 2010;304(1):76–84. doi: 10.1001/jama.2010.896. [DOI] [PubMed] [Google Scholar]
- 20.Cox D. Regression models and life tables. J R Stat Soc B. 1972;34(187) [Google Scholar]
- 21.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health Literacy and Mortality Among Elderly Persons. Arch Intern Med. 2007;167(14):1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 22.Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. Journal of General Internal Medicine. 2006;21(8):806–12. doi: 10.1111/j.1525-1497.2006.00539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. Journal of General Internal Medicine. 1998;13(12):791–8. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, et al. Functional Health Literacy and the Risk of Hospital Admission Among Medicare Managed Care Enrollees. Am J Public Health. 2002;92(8):1278–1283. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davis TC, Wolf MS, Bass PF, III, Thompson JA, Tilson HH, Neuberger M, et al. Literacy and Misunderstanding of Prescription Drug Labels. Ann Intern Med. 2006;145(12):887–94. doi: 10.7326/0003-4819-145-12-200612190-00144. [DOI] [PubMed] [Google Scholar]
- 26.Kripalani S, Henderson LE, Chiu EY, Robertson R, Kolm P, Jacobson TA. Predictors of Medication Self-management Skill in a Low-literacy Population. Journal of General Internal Medicine. 2006;21(8):852–856. doi: 10.1111/j.1525-1497.2006.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.von Wagner C, Steptoe A, Wolf MS, Wardle J. Health Literacy and Health Actions: A Review and a Framework From Health Psychology. Health Education & Behavior. 2009;36(5):860–877. doi: 10.1177/1090198108322819. [DOI] [PubMed] [Google Scholar]
- 28.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. Journal of General Internal Medicine. 1995;10(10):537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 29.Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Family Medicine. 1993;25(6):391–5. [PubMed] [Google Scholar]
- 30.Cavanaugh K, Wallston KA, Gebretsadik T, Shintani A, Huizinga MM, Davis D, et al. Addressing Literacy and Numeracy to Improve Diabetes Care. Diabetes Care. 2009;32(12):2149–2155. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weiss BD, Francis L, Senf JH, Heist K, Hargraves R. Literacy education as treatment for depression in patients with limited literacy and depression: a randomized controlled trial. Journal of General Internal Medicine. 2006;21(8):823–8. doi: 10.1111/j.1525-1497.2006.00531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


