Abstract
Background
There is a debate in medicine about the value of self-disclosure by the physician as a communication tool.
Aim
To review the empirical literature of self-disclosure in primary care.
Design and setting
Systematic review of empirical literature relating to self-disclosure by primary care physicians (including US paediatricians) from seven electronic databases (MEDLINE®, Scopus, PsycINFO, Embase, Social Sciences Citation Index, EBSCOhost, and Cochrane Central Register of Controlled Trials [CENTRAL]).
Method
Databases were searched for empirical studies on self-disclosure and primary care published from 1946 to 28 November 2014, as well as references from primary studies. The search was extended to include working papers, theses, and dissertations.
Results
Nine studies were identified, with response rates ranging from 34% to 100%, as well as several not reported. Self-disclosure occurred in 14–75% of consultations, the most from paediatricians. Self-disclosure had intended benefit; however, one standardised patient study found that 85% of self-disclosures were not useful as reported by the transcript coders. Conflicting data emerged on the self-disclosure outcome.
Conclusion
This is the first systematic review of self-disclosure in primary care and medicine. Self-disclosure appears to be common and has the potential to be helpful when used judiciously. Few studies examined the impact on patients, and no studies considered the individual patient perspective nor the content which results in benefit or harm. No evidence was found of any training into how to deal with self-disclosure.
Keywords: medicine, physicians, physician patient relations, primary care, self disclosure
INTRODUCTION
To what extent should physicians reveal information about their own lives and experiences to patients? The present study was prompted by discussions with some GP colleagues who felt strongly that doctors should not self-disclose. Most therapists are trained not to self-disclose, and, although most of the empirical work resides in psychological literature, there is still little consensus on the role of physician self-disclosure.1,2 There is less empirical work in medicine and it remains a controversial topic. Self-disclosure has been described by some as a boundary violation,2 and by others as a method to build trust and rapport.1,3 Candib describes the traditional view where a physician is meant to have a:
‘... professional attitude … reluctant to admit to transgressing this standard by the sharing of personal life details with patients.’ 3
She also says that, although it is not always ideal, self-disclosure:
‘... reveals the physician as an authentic person … it can be a powerful force for growth in the doctor–patient relationship.’ 3
As part of some empirical work on the issue of self-disclosure in primary care, a literature search was conducted to see what was available on self-disclosure and primary care. No reviews or guidelines were found. Reviews on important topics in general practice are interesting to colleagues and can guide future research. With no current guidelines, the complex decision of whether to self-disclose is left up to doctors. It is known that the language used in the primary care consultation can alter the outcome in a consultation. For example, use of the words ‘something else’ rather than ‘anything else’ (‘Is there something else you want to discuss in the visit today?’) resulted in a 74% reduction in unmet concerns in a randomised controlled trial in family practice consultations.4 Specific self-disclosures could well have a significant impact on consultation outcomes. This current review aimed to explore the evidence in empirical research on self-disclosure in medicine, with a focus on primary care, to enhance understanding of the decision and purpose of self-disclosure, the context, type, and amount of self-disclosure that may be beneficial or harmful and its implications. This is the first systematic review on the topic of medical self-disclosure and hence a valuable addition to the literature.
METHOD
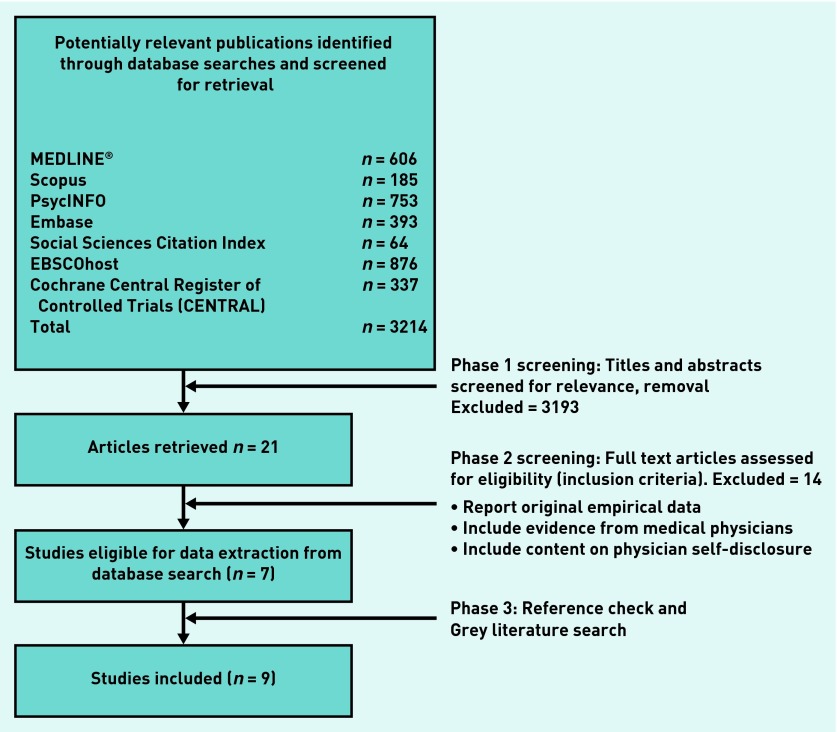
A search was undertaken for empirical research from 1 January 2000 to 28 November 2014 to identify literature on self-disclosure by primary care physicians (Figure 1). MEDLINE® was searched from 1946 to 28 November 2014 and all retrieved articles had their reference section checked for relevant articles. The search used seven electronic databases (MEDLINE, Scopus, PsycINFO, Embase, Social Sciences Citation Index, EBSCOhost, and Cochrane Central Register of Controlled Trials [CENTRAL]) using the terms self-disclosure, physician/doctor/general practitioner/family practitioner/family physician and also paired these terms with patient, physician–patient relationship, and medicine. Also, authors of primary articles were contacted to source working papers and the online search was extended to include theses and dissertations.
Figure 1.
Flow chart of studies included in the review.
How this fits in
This is the first systematic review of physician self-disclosure during clinical consultations, reporting mixed views on its value. Specific patient reactions to self-disclosure were conspicuously absent. Presenting current data on this subject in primary care enhances understanding of the decision, purpose, and outcome of physician self-disclosure. This informs and guides GPs and recognises gaps in knowledge to direct future research.
Selection process
To be included in the review the literature needed to meet three inclusion criteria: studies must report original empirical data, thus reviews, opinion pieces, accounts of personal experiences, editorials, and commentaries were excluded; studies needed to include evidence from primary care physicians or patients in primary care. Paediatricians from the US were included on the basis that they could provide primary care to children; lastly, studies had to include content on self-disclosure to patients or their families where self-disclosure is defined to include disclosure of personal and/or professional experiences. Both authors checked the abstracts and full texts of articles.
Data extraction
Data extraction was carried out independently by the two authors using previously agreed criteria, and disagreements were resolved by discussion. Results were classified into three categories relating to self-disclosure, which were theorised as valuable components from review of the literature; these were decision and reasoning for self-disclosure, the degree and type of self-disclosure, and the resulting effects of self-disclosure on the patient and the physician–patient relationship. In terms of specific outcome measures, the aim was to find measures of occurrence and patient reaction/satisfaction.
RESULTS
From the 3214 studies identified, 21 were extracted for further screening based on relevance in the title and/or abstract and after removal of duplicates (Figure 1). Nothing was found in the grey or thesis literature. From these, seven met the previously described inclusion criteria. Subsequently, through emailing of authors and the Society of Teachers of Family Medicine, two additional articles were located. No working papers or other forms of grey literature were identified that met the inclusion criteria. Of the nine studies, three were mixed methods, three were qualitative, two were cross-sectional, and one was a randomised controlled trial.
Descriptions of the studies are summarised in Table 1. The number of participants ranged from 4 to 131. Of the nine studies, four had >100 participants while three had samples with <12. One study failed to report the number of subjects.3 Several studies had methodological weaknesses relating to the participant response rate, with two of the nine studies1,5 reporting a response rate of ≤50%. Four of the studies3,6,7 did not report response rates. All but one study,1 which included patients recruited from a primary care clinic, comprised physicians from primary care. Participants from other professions including psychology (a minority of samples), dentistry, sociology, and surgery were also included in three of the studies.6,8,9
Table 1.
Descriptions and participant characteristics of studies related to physician self-disclosure (ordered by method and year)
| Source [Design] | Year of publication | Participants (Location) | Participants n | Participant response rate | Participant characteristics | Data collection method | Study question |
|---|---|---|---|---|---|---|---|
| Holmes et al [MM]10 | 2010 | Paediatricians (Southern University paediatric department US) | 4 | 100% | Physicians: 2 female, 2 male, all white. Parents 85% female, 85% white, and 11% African American | Audiotapes of 80 parent visits | Is there a relationship between paediatrician SD and parent satisfaction? |
| McDaniel et al [MM]5 | 2007 | Primary care physicians (Rochester, NY, US) | 100 | 34% | Mean age 45 years, 77% male, 47% family medicine, 53% internal medicine, 76% group practice, 68% urban/suburban | Audiotapes of 113 standardised patient visits. Coding agreed by consensus | What are the antecedents, delivery, and effects of SD in primary care visits? |
| Beach et al [MM]9 | 2004 | Primary care physicians and surgeons (Colorado and Oregon, US) | 125 physicians: 66 surgeons (general and orthopaedic) 59 primary care (general internist and family physicians) | Surgeons 89% and primary care 74% Patients 80% | Physicians: graduated 13 years, white, 94% male, 93% in practice 18 years Patients: >18 years, English-speaking, not distressed; white 86%, female 57%, age 53 years, 27% college graduated | Audiotapes of, 265 patient visits. Analysis coder reliability 0.94 | What do physicians disclose about themselves to patients? Not designed as a study on SD |
| Beach et al [CS]8 | 2004 | As Beach et al above | As Beach et al above | As Beach et al above | As Beach et al above | As above but with patient completed surveys | Is physician SD related to patient evaluation of office visits? Not designed as a study on SD |
| Allen et al [Q]11 | 2015 | GPs (Auckland, New Zealand) | 16 | 33% | 8 female | Audiotapes on SD. Coding by consensus | What are your views on SD? |
| Malterud et al [Q]7 | 2009 | GPs (Norway) | 12 | 100% | Physicians: 5 males, 7 females; aged 30–68 years; Experience 1–39 years | Audiotapes of two 90-minute group discussions with participants. No reliability assessment | What are the conditions in which disclosure of a doctor’s vulnerability is beneficial to patients? |
| Malterud and Hollnagel [Q]6 | 2005 | GPs, psychologists, sociologists/patients (Denmark) | 7 GPs/psychologists, 2 sociologists; either as clinicians or their own patient experience | 100% | Physicians: 2 males, 7 females; aged 36–61 years. | Memory stories and audiotapes of group discussions. No reliability assessment | How can exposing doctor’s vulnerability be of benefit to patients? |
| Candib [Q]3 | 1987 | Experienced family physicians known to the author, (UK) | N/R | N/R | Most family physicians, varied ages, substantial practice experience | Conversations with participants by the author wherever the participants could be approached | What do doctors share with patients and what are the implications of such disclosures for the relationship? |
CS = cross sectional. MM = mixed methods. N/R = not reported. Q = qualitative. SD = physician self-disclosure. Coders refers to those analysing the audiotranscripts.
There were three data collection methods. The first was to capture occurrences of self-disclosure using audiotapes of patient consultations.5,8–11 The second approach used retrospective self-reporting by physicians of self-disclosure, acquired through interviews or group discussions.3,6,7 Lastly, the patient perspective was collected through patient surveys to assess satisfaction or self-disclosure influence.1,8,10 Definitions of self-disclosure are summarised in Table 2. The descriptions of self-disclosure were similar across all studies with each describing self-disclosure, in some form, as the revelation by the physician of personal experiences. Some studies expanded their description to include disclosure of emotions,6,7,10 as well as attitudes and opinions.10 Another study more specifically focused on physician disclosure of their own healthy behaviours.1 Results are also summarised in Table 2 according to their classification into one of three categories outlined in the Method section. Five of the nine studies reported that reliability or consensus checks were made on data extraction. Table 3 reports the details of the randomised controlled trial.
Table 2.
Definition of physician self-disclosure and summary of findings from studies containing empirical data of physician self-disclosure (ordered by method and year)
| Source (Year) [Method] | Definition of physician self-disclosure | Findings related to physician decision and reasoning to self-disclose or not to self-disclose | Findings related to type, content and magnitude of self-disclosure | Findings related to the outcomes on patients and/or physician–patient relationship |
|---|---|---|---|---|
| Holmes et al (2010) [MM]10 | Physician statements about their own personal or professional experience including statements that would disclose the physician’s emotions, attitudes, or opinions | N/R | 75% of visits contained SD, median 3 per visit |
|
| McDaniel et al (2007) [MM]5 | Physician statements about his or her own personal or professional experience | N/R | SD common (34%), spontaneous (86%), and physician focused (60%) |
|
| Beach et al (2004) [MM]9 | Any statement made to a patient that describes the physician’s personal experience in areas which have medical and/or emotional relevance for the patient | N/R |
|
N/R |
| Beach et al (2004) [CS]8 | As Beach et al above | N/R |
|
|
| Allen et al (2015) [Q]11 | Physician disclosure of emotions and personal experiences | Enhances patient support and empathy, closeness, improve patient motivation and adherence. Develops trust and mutuality, reduces any power imbalance. Disadvantages also reported | Would disclose physical to psychological. None would disclose hypothetical criminal issues | GPs felt that SD is mainly beneficial |
| Malterud et al (2009) [Q]7 | Physician disclosure of emotions and personal experiences sometimes disclosed to patients | Awareness and capacity for interpretation, creative solutions, and compassion had been enhanced through SD of a shared experience | N/R | Vulnerability of physician may benefit patient but needs to be used with caution |
| Malterud and Hollnagel (2005) [Q]6 | Physician disclosure of emotions and personal experiences | Physician hesitation prior to SD (? considering the possible outcomes) |
|
|
| Candib (1987) [Q]3 | Offering of personal information by physicians |
|
|
|
CS = cross sectional. MM = mixed methods. N/R = not reported. Q = qualitative. SD = physician self-disclosure.
Table 3.
Summary of findings from randomised control trial
| Study | Participants | Intervention | Control | Method | Outcome |
|---|---|---|---|---|---|
| Frank et al 20001 | Age 66 years; white 62%; heart disease 20%; 22% smokers; exercise 72% | Non-clinic physician video of diet and exercise; and has a bike helmet and apple on desk | As for intervention but no picture of helmet and apple | Concealment of randomisation not mentioned and blinding not reported | Questionnaire after visit showed video which included SD was more likely to improve healthy behaviours |
SD = physician self-disclosure.
Decision and reasoning for self-disclosure
Conversations with experienced GPs3 uncovered similar motivations for self-disclosure, which included making their recommendations more credible, and raising adherence, as well as a means to convey empathy. Similarly, GPs who had exposed their vulnerability through self-disclosure, and had seen this as beneficial,7 reasoned that their ability to interpret a patient’s experience and offer solutions and compassion had been enhanced. A few experienced GPs described self-disclosure as a type of self-therapy, such that it allows the patient to offer comfort or guidance.3
Descriptions of circumstances where physicians decided against self-disclosure were also given.3 Several physicians in one study3 alluded to the potential for self-disclosure to be coercive. The same study3 revealed that some physicians will generally avoid self-disclosing to patients whom they feel have expressed a dependency or a high interest in their personal lives.
Type, content, and amount of self-disclosure
Studies of patient visits with physicians suggest that self-disclosure is common.5,8–10 Self-disclosures occurred in 17% of primary care and 14% of surgical visits; with a median number of two per visit.8 It was also noted that 71% of physicians self-disclosed during at least one visit. Of visits from undetected and standardised patients to primary care physicians, 34% contained at least one self-disclosure statement.5 The highest measured self-disclosure statements occurred during visits between paediatricians and their patients’ parents,10 with 75% containing a self-disclosure statement with a median of three per visit.
Analysis of patient visits with primary care physicians and surgeons led to classification of self-disclosure statements.9 Around 29% were classified as reassurance (physicians disclosing that they had a similar experience to the patient), around 25% as counselling (physician disclosure of a similar experience that could help guide patient actions), 23% as rapport building (physician using humorous and empathetic self-disclosures), 13% as casual (physician self-disclosures with little relevance to patient), 6% intimate (physician disclosing physical or emotional aspects of their life), and 4.5% as extended narratives (a long description of the physician’s experience with little relevance to the patient). This last self-disclosure category is an obvious misuse of patient time and it is recommended to avoid disclosures of this type. An older study of GPs made some equivalent classifications.3 Statements that revealed personal aspects that could be used to guide patients were described as ‘role-model’ statements, and are equivalent to counselling self-disclosure previously mentioned. Additionally, self-disclosure statements were also reported to be a ‘relationship-enhancing’ tool to advance mutuality and closeness, thus can be likened to rapport-type self-disclosure described above.
Only one study explored the antecedents of self-disclosure in primary care using standardised patients.5 Interestingly, 67% of self-disclosure statements made by the primary care physicians were preceded by a patient’s account of their symptoms or family/personal issues. Although triggered by a preceding patient statement, the content of self-disclosure was unrelated to the preceding statement 40% of the time.5
Outcomes of self-disclosure on the patient and the physician–patient relationship
Audiotapes of routine patient visits to primary care physicians and surgeons used patient surveys in an attempt to examine the relationship between self-disclosure and patient satisfaction.8 Patients of the primary care physicians were less satisfied in terms of warmth, friendliness, comfort, and reassurance after visits with self-disclosure. Conversely, in the surgical setting, patients were more likely to report higher satisfaction when the surgeon self-disclosed. Results from standardised patient visits to primary care physicians, where there is an absence of a doctor–patient relationship,5 reported negative results as 85% of self-disclosures were not considered to be useful according to the study coders. Only 21% of physicians returned to the patient’s prior concern, while 60% of the self-disclosures that occurred were categorised as physician-focused and none were thought to be patient-focused. Also concerning was the finding that only 4% of the self-disclosures were deemed useful to the patient, while 10% were regarded as disruptive and detrimental.
Conversations with experienced GPs3 indicated that self-disclosure could be disruptive in the setting of an inadequate physician–patient relationship. Some physicians with medical conditions12 suggested that disclosure of their own illnesses and issues distorts the carer–patient relationship and steals patient focus.
Other studies reported instances where self-disclosure has resulted in benefit. Where there is an adequate relationship, GPs feel self-disclosure creates an environment in which patients feel more comfortable sharing.3 Visits between paediatricians and their patients’ parents showed that 98.2% of parents strongly agreed they were satisfied with the visit when the paediatrician self-disclosed compared with 70% when they did not.10 A randomised controlled trial into whether self-disclosure of personal healthy behaviours would enhance counselling of patients found that those participants who viewed a video that included self-disclosure (visual display of a bicycle helmet and apple on desk) judged the physician to be healthier, slightly more believable, and motivating than the control group.1 There were no studies of individual patient response to specific self-disclosure.
DISCUSSION
Summary
Empirical support was found that self-disclosure is a common occurrence in medical practice,5,8–10 and that, despite its good intentions, it may not always be useful.3,5,8 The occurrence of self-disclosure was surprising, given that the stimulus for this study was colleagues who felt that clinicians should never self-disclose. The reviewed studies also highlighted the potential for self-disclosure to enhance patient satisfaction or the physician–patient relationship.3,5,6,9,10 There are conflicting data relating to the consequences of self-disclosure, which are likely to be a result of variations in the context in which self-disclosure occurs, the nature of the physician–patient relationship to begin with, and the content of the self-disclosure made. Patient satisfaction measured by surveys is generally positive, but coders of a patient simulation study were generally negative. It is difficult to reconcile this disparity without more research but this may indicate a problem with simulated patients. One of the authors of the patient simulation study offered a suggestion in a commentary paper that ‘physicians can replace the disclosure with a more effective, empathic statement or make the self-disclosure more effective by keeping it brief and transitioning quickly back to the patient.’13 Although this seems reasonable, it is not based on empirical data and may explain the generally negative comments in the empirical study.5 The present authors’ view is that all authors should state their biases/preferences for qualitative research (where it is often done) and quantitative research (where it is rarely done). Malterud et al described self-disclosure as a complex communicative behaviour that is not necessarily good or bad.7 What was missing in the definition of self-disclosure was the use of the term ‘spontaneous.’ It is not clear if any physician consciously uses self-disclosure but that would make for an important intervention study.
Strengths and limitations
A physician’s reflection that their self-disclosure is of benefit to the patient is reliant on their correct interpretation of the patient’s response: this may lead to the incorrect assumption that an act of self-disclosure has had a positive impact.3,5–7,11 Most of the physicians were GPs or each study contained GPs or primary care physicians. This is appropriate as this is a group where self-disclosure may be more common; for example because of a wide range of conditions and more established doctor–patient relationships. Examination of other specialities, however, would enrich the field. There is also little evidence regarding the influence of the mix of patient and physician demographics on the likelihood and nature of self-disclosure. Most data collection methods involved group discussions, participant interviews, or patient visits for which the physician was aware they were being recorded. These methods are potentially problematic as they may alter the participant performance. Context is also important as a close physician–patient relationship may mean patients feel more satisfied with self-disclosure than in research situations, such as standardised patient visits, where that is not present. The other issue with standardised patients is the patient is inevitably new to the practice and physicians may be more inclined to self-disclose, appropriately or inappropriately, to make the patient feel welcome. Additionally, many of the studies derived results from limited population samples and most had poor or absent response rates. The one randomised controlled trial was of limited scope but more use could be made of the clinical trial. The aim of this study was to include all studies irrespective of their quality; however, the studies were so disparate that it was not possible to compare one with the other. There were not even two studies of similar methods and subjects with which to make any direct comparisons.
A strength of this review is that seven databases were searched, the grey literature, and authors of included studies contacted to seek any work in press or known to them and unpublished. The papers and the contents were independently assessed. The main limitation of this review is the disparate methods of data collection, different contexts, and absence of the patient-specific voice on the value of self-disclosure.
Comparison with existing literature
The present study suggests that it is commonplace for doctors to self-disclose but the impact on patients is not well understood or quantified. Self-disclosure has the potential to make the doctor seem more human and approachable but also to derail a consultation. A self-disclosure resulting from frustration with a patient is not sanctioned by the present authors. It is recommended to avoid extended narratives which have little patient relevance and use up precious patient time. Klitzman et al advise that clinicians:
‘... consider carefully pros and cons involved … [and] ensure that any disclosures benefit the patient.’ 12
They also make the point that patients may have a genuine concern about the health and wellbeing of a trusted physician and that physician non-disclosure may impact patients too.
Implications for research and practice
Although communication skills are part of medical training, self-disclosure and its place in medicine are currently absent from formal medical teaching. Medical students need to be made aware of the existence of self-disclosure as most will almost certainly do this at some point in their career. Finally, medical students need to be forewarned that patients may ask them direct questions on personal health and social matters, and they must therefore be offered the necessary support and guidance to effectively deal with these questions.
Further research into this area needs to be more systematic. Each study could consider the same physicians with simulated patients and regular patients along with patient questionnaires and ways of assessing the patient experience. Consideration could be given to asking patients to listen to the consultation transcripts and comment on the value of self-disclosures. Some simple answers would be welcome such as, are clinicians aware or unaware that they self-disclose or do not self-disclose? Additionally, a mix of contexts of different clinical specialities to compare with primary care should be studied, along with a range of physician and patient demographics. Some structure could be used enabling randomised controlled trials to assess different aspects of self-disclosure.
Self-disclosure is practised by many GPs. The value of it for patients remains uncertain, although judicious use seems to be sanctioned by many investigators.13 The present authors recommend that medical students are informed of the practice and given some training. Future research needs to consider the patient views related to specific consultations containing self-disclosure (rather than group satisfaction) and to systematically fill gaps in the literature.
Funding
Emily-Charlotte Frances Allen received a summer student allowance from the University of Auckland.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Frank E, Breyan J, Elon L. Physician disclosure of healthy personal behaviors improves credibility and ability to motivate. Arch Fam Med. 2000;9(3):287–290. doi: 10.1001/archfami.9.3.287. [DOI] [PubMed] [Google Scholar]
- 2.Gabbard GO, Nadelson C. Professional boundaries in the physician-patient relationship. JAMA. 1995;273(18):1445–1449. [PubMed] [Google Scholar]
- 3.Candib LM. What should physicians tell about themselves to patients? Am Fam Physician. 2001;63(7):1440–1442. [PubMed] [Google Scholar]
- 4.Heritage J, Robinson JD, Elliott MN, et al. Reducing patients’ unmet concerns in primary care:the difference one word can make. J Gen Intern Med. 2007;22(10):1429–1433. doi: 10.1007/s11606-007-0279-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDaniel SH, Beckman HB, Morse DS, et al. Physician self-disclosure in primary care visits: Enough about you, what about me? Arch Int Med. 2007;167(12):1321–1326. doi: 10.1001/archinte.167.12.1321. [DOI] [PubMed] [Google Scholar]
- 6.Malterud K, Hollnagel H. The doctor who cried: a qualitative study about the doctor’s vulnerability. Ann Fam Med. 2005;3(4):348–352. doi: 10.1370/afm.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malterud K, Fredriksen L, Gjerde MH. When doctors experience their vulnerability as beneficial for the patients. Scand J Prim Health Care. 2009;27(2):85–90. doi: 10.1080/02813430802661811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beach MC, Roter D, Rubin H, et al. Is physician self-disclosure related to patient evaluation of office visits? J Gen Intern Med. 2004;19(9):905–910. doi: 10.1111/j.1525-1497.2004.40040.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beach MC, Roter D, Larson S, et al. What do physicians tell patients about themselves? J Gen Intern Med. 2004;19(9):911–916. doi: 10.1111/j.1525-1497.2004.30604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holmes GN, Harrington NG, Parrish AJ. Exploring the relationship between pediatrician self-disclosure and parent satisfaction. Communication Research Reports. 2010;27(4):365–369. [Google Scholar]
- 11.Allen E, Arroll B. Physician self-disclosure in primary care: a mixed methods study into GP attitudes, skills, and behaviour. Br J Gen Pract. 2015 doi: 10.3399/bjgp15X686521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klitzman R, Weiss J. Disclosures of illness by doctors to their patients: a qualitative study of doctors with HIV and other serious disorders. Patient Educ Couns. 2006;64(1–3):277–284. doi: 10.1016/j.pec.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Morse DS, McDaniel SH, Candib LM, Beach MC. ‘Enough about me, let’s get back to you’: physician self-disclosure during primary care encounters. Ann Intern Med. 2008;149(11):835–837. doi: 10.7326/0003-4819-149-11-200812020-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]