PERIMENOPAUSAL PRESENTATIONS
Perimenopausal patients present with vasomotor, psychological, and urological symptoms as well as disturbance of their bleeding pattern. Pregnancy risk is not always something they are aware of and consequently can sometimes be overlooked. Similarities and overlap exist between products used for contraception and those used as hormone replacement, but as yet no product is licensed for both.
MISMATCH OF DEFINITIONS
A complicating factor in these consultations is that when clinicians use the word ‘menopause’ they mean cessation of ovulation, whereas patients use the same word to describe the symptoms they are suffering (Box 1).1 Patients often recount ‘early menopause’ in family members, but are not describing early cessation of menses, indeed the actual date of final menstrual period (FMP) is often unknown, as many women have been taking cyclical hormone replacement therapy (HRT) or hormonal contraception. Clarification of these definitions at an early stage in the consultation is important, as genuine early or premature menopause is a risk factor for osteoporosis, heart disease, and dementia; these patients need to understand the benefits of HRT up until at least the age of 50 years.2
Box 1. Medical definitions1.
Perimenopause/climacteric
Phase of life, inverse of puberty
From onset of symptoms/menstrual irregularity until 1 year after menopause
Average age 45–55 years, timing of onset and duration very variable
Menopause
Single point in time
Final menstrual period (FMP)
Average age 52 years in UK (80% by 54 years)
Diagnosed in retrospect 2 years after FMP if <50 years; 1 year if >50 years
Postmenopause
The rest of a woman’s life after FMP, often one-third or potentially half of her life
Premature menopause
SEX IN THE OVER 40s
Mid-40s is the peak age for divorce in the UK, often corresponding to renewed interest in sexual relationships. In some respects midlife has become the new teenage and in both age groups a higher than average proportion of pregnancies end in abortion. Our role therefore is to emphasise that the onset of perimenopausal symptoms does not herald an end to fertility.
CESSATION OF CONTRACEPTIONS
A woman can be regarded as safe from pregnancy risk a year after her FMP if she was >50 years, or 2 years after her FMP if she was <50 years. This is useful only if she was using a non-hormonal method of contraception, as with hormonal methods she cannot be sure if her amenorrhoea was natural or method induced. Current recommendation is for women using combined methods or the Depo-Provera® (Pfizer) injection to change to an alternative method at age 50 years, but the other methods of contraception do not have any upper age restriction.3
BLOOD TESTS
Follicle stimulating hormone (FSH) levels are useful in women wishing to cease progestogen-only contraception (POC) (but not oestrogen-containing products): two FSH levels ≥30 iu/l, 6 weeks apart show a woman is post-menopausal and she then needs to wait 1 year before safely stopping contraception.3
FSH levels are also indicated in women who have ceased menstruating aged <45 years, so that management of premature menopause can be offered. Testing FSH levels in women who are still menstruating, however, is both unhelpful and misleading as the levels can vary markedly even on a daily basis. Whether to offer HRT or not should be based on symptoms; FSH levels do not assist with this decision and if raised may give false reassurance regarding pregnancy risk.
MANAGEMENT OPTIONS
HRT offers excellent control of perimenopausal symptoms, but it can exacerbate bleeding problems and does not offer contraception. Management options to address all three problems include: combined hormonal contraception (CHC); Mirena® (Bayer) plus oestrogen replacement (ERT); or HRT plus POC.
Combined hormonal contraception
CHC is a safe, effective alternative to HRT in healthy, non-smoking, perimenopausal women and offers additional benefits, including: control over bleeding, contraception, and protection against ovarian and uterine cancers.3
Original CHC products contained >100 μg of ethinylestradiol (EE), whereas products today contain between 15 μg and 35 μg. The lowest dose is provided by the vaginal ring (NuvaRing® [MSD]), which also offers the greatest degree of bleeding control.
Since the 1960s CHC has been designed to offer 21 treatment days, followed by a 7-day hormone-free interval (HFI), giving a false 28-day cycle. This can cause problems with longer bleeds, mood swings, headaches, and in perimenopausal women, exacerbation of vasomotor symptoms in the HFI. More favourable regimens include offering fewer or shorter HFI.4 ‘Tricycling’ or running three strips of pills consecutively provides just five HFI/bleeds annually, rather than 13. Shorter HFIs are available with the newest pills: Qlaira® (2-day [Bayer]) and Zoely® (4-day [MSD]). These pills also contain estradiol (E2) rather than EE, just like HRT.
CHC however, unlike Mirena or HRT, is contraindicated in certain women: smokers >35 years, those with hypertension, focal migraine (transdermal HRT recommended), and complicated diabetes.4
Mirena plus ERT
Mirena is licensed for contraception, heavy menstrual bleeding (HMB), and as the progestogen element of HRT. Amenorrhoea or decreased bleeding is achieved in 65% of Mirena users in the first year of use. Mirena has been shown to be more effective in reversing anaemia than CHC and its increasing use in the treatment of heavy menstrual bleeding has led to a significant decrease in hysterectomies in the UK.5 Mirena plus ERT provide the only form of continuous combined (potentially bleed-free) HRT licensed in perimenopausal women.
An area for possible confusion for Mirena users is the timing of removal or replacement. If fitted at the age of <45 years in a woman requiring contraception the Mirena should be changed after 5 years; the Faculty of Sexual and Reproductive Healthcare (FSRH)3,6 supports extended use if fitted at >45 years. If fitted for HMB alone, the device needs only to be changed if unacceptable bleeding returns. If, however, the device is being used as the progestogen element of HRT (for endometrial protection) it has to be changed at 5 years (licence states 4 years, but FSRH support 5 years) regardless of bleeding or contraceptive need.3,6 It is important, therefore, to ascertain at each follow-up visit whether contraceptive need has changed (for example if the woman has a new partner without vasectomy); or if ERT has been commenced (Figure 1).
Figure 1.
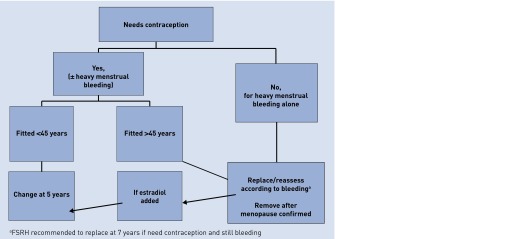
Algorithm for timing of Mirena removal or replacement.3,6 ©Pulse. Adapted with permission. (http://pulse-learning.co.uk/clinical-modules/women-s-health/larc).
HRT plus POC
Some experts advocate that all POC (including pills and implant) can be used in the same manner as the Mirena, as endometrial protection alongside ERT; however, this is not currently accepted practice in the UK. FSRH3 recommend that a progestogen-containing HRT should be used alongside all POC.
CONCLUSION
Most women experience perimenopausal symptoms (70%),1 classically between the ages of 45 and 55 years, and many seek help. These symptoms along with chaotic bleeding can be embarrassing, and cause sleep deprivation, lethargy, and low mood in women, often at the busiest time of their working lives; these are the women for whom HRT is prescribed in the UK. As most are also sexually active, we need to address this triad of needs holistically, offering those who have not undergone hysterectomy or sterilisation help across all three parameters: vasomotor symptoms, dysfunctional bleeding, and risk of pregnancy.
Mirena plus ERT is the gold standard, offering potentially bleed-free, contraceptive HRT with no upper age limit. For those <50 years who decline a Mirena and who have no contraindications, CHC may offer the best all-round treatment option, providing important lifestyle benefits as well as long-term health benefits. If neither Mirena nor CHC is suitable, our task is to find an HRT product that suits and to remember to prescribe a POC alongside.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
Jenny Brotherston has received sponsorship for educational meetings from pharmaceutical companies including Bayer Schering Pharma (BSP) and Merck, Sharp Dohme (MSD).
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Rees M, Stevenson J, Hope S, et al. Management of the menopause. 5th edn. Boca Raton, FL: CRC Press; 2011. [Google Scholar]
- 2.Shah D, Nagarajan N. Premature menopause — meeting the needs. Post Reproductive Health. 2014;20(2):62–68. doi: 10.1177/2053369114531909. [DOI] [PubMed] [Google Scholar]
- 3.FSRH Clinical Effectiveness Unit Contraception for women aged over 40 years. Clinical Guidance. 2010 http://www.fsrh.org/pdfs/ContraceptionOver40July10.pdf (accessed 6 Aug 2015). [Google Scholar]
- 4.FSRH Clinical Effectiveness Unit Combined hormonal contraception. Clinical Guidance 2011 (update 2012). http://www.fsrh.org/pdfs/CEUGuidanceCombinedHormonalContraception.pdf (accessed 27 Jul 2015).
- 5.National Institute for Health and Care Excellence Long acting reversible Contraception (NICE Clinical Guideline 30). 2005 (update 2013). http://www.nice.org.uk/CG030NICE (accessed 28 Jul 2015).
- 6.FSRH Clinical Effectiveness Unit Intrauterine Contraception. Clinical Guidance 2015. http://www.fsrh.org/pdfs/CEUGuidanceIntrauterineContraception.pdf (accessed 28 Jul 2015).


