Abstract
Phacomatosis pigmentovascularis is a rare, congenital condition characterized by a combination of cutaneous melanocytic lesions and vascular malformation. We discuss an entirely unique case of Phacomatosis pigmentovascularis with nevus of Ota, extensive Mongolian spot, nevus flammeus, nevus anemicus and cutis marmorata telangiectatica congenita, which may represent a heretofore undescribed variant of phacomatosis pigmentovascularis.
Keywords: Hemangioma; Mongolian spot; Nevus of ota; Nevus, pigmented; Port-Wine Stain
INTRODUCTION
Phacomatosis pigmentovascularis is a rare, congenital condition characterized by a combination of cutaneous melanocytic lesions and vascular malformation. Most cases have been reported in Argentinian and Japanese patients, and it is rare in white-skinned individuals.1 We describe a unique, Chinese case of phacomatosis pigmentovascularis with nevus of Ota, extensive Mongolian spot, nevus flammeus, nevus anemicus and cutis marmorata telangiectatica congenita (CMTC), which cannot be classified as one of the currently accepted types of PPV.
CASE REPORT
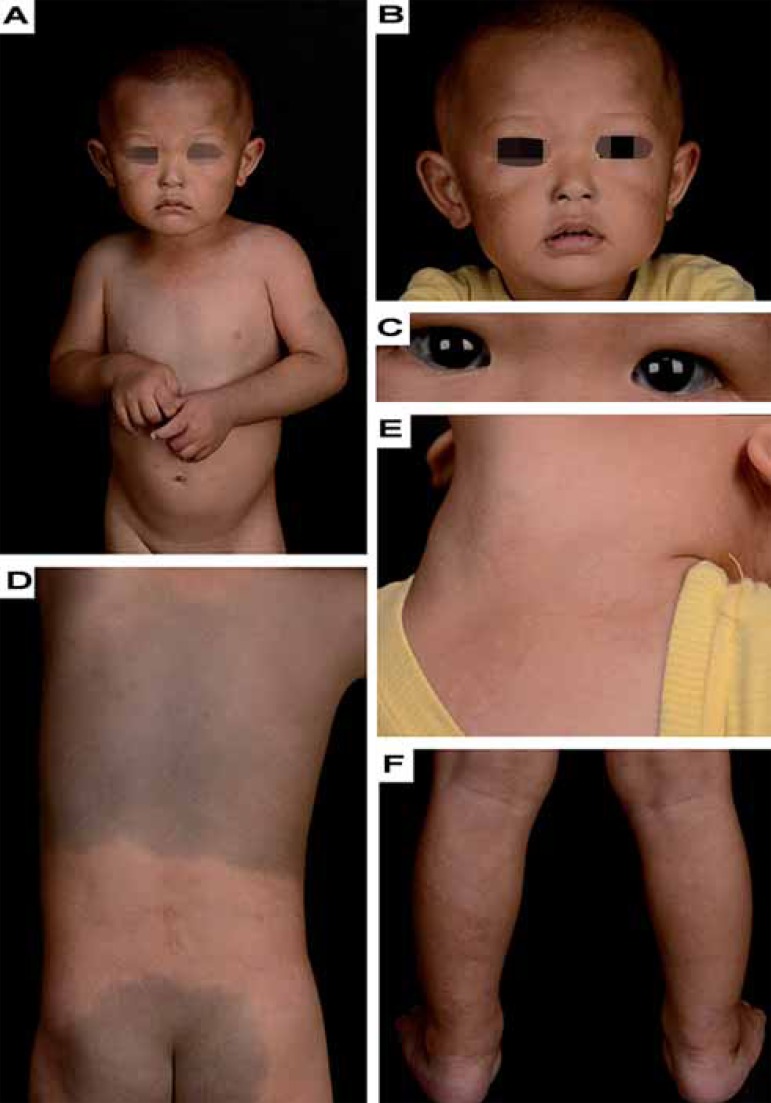
A 20-month-old boy was referred to our department for evaluation of congenital cutaneous abnormalities. On examination, black-brown pigmentation patches (nevus of Ota) affected bilateral skin of the forehead, upper eyelid, alae of the nose, zygomatic region, temporal region, cheek and anterior auricle, i.e. the innervation area of both the second and third branches of the trigeminal nerve and terminal infraorbital nerve (Figures 1A and B). Opthalmic examination revealed blue spots on the cornea, conjunctiva, and blue sclera (Figure 1C). Light blue spots were also seen on the nasal mucosa. We observed demarcated greyish-blue hyperpigmentation with clear-cut margins (Mongolian spot) affecting his trunk, back, buttocks, arms and right shoulder (Figures 1A and 1D). Erythematous patches (nevus flammeus) were noted on the regio cervicalis anterior, left shoulder and upper limb (Figure 1E). Isolated CMTC, consistent with irregular, pale macules and patches (nevus anemicus) were present on his left leg calf, and nevus anemicus might be most obvious on the rear side of the right ankle (Figure 1F). The child was born full-term through vaginal delivery, weighing 3000g. Both the pregnancy and labor were uneventful. He did not suffer from chronic diseases. His family and personal history were unremarkable. At the time of writing, no alterations in neuropsychomotor development were observed, and the extremities were symmetrical, without atrophy or hypertrophy signs in the soft tissues. The blood and urine routine, biochemistry, electrocardiography and electroencephalogram were all within normal limits.
FIGURE 1.
(A and B) Bilateral nevus of Ota on the face. (C) Blue spots on the cornea and conjunctiva. (D) Demarcated greyish-blue hyperpigmentation over the back and buttocks. (E) Erythematous patches on the regio cervicalis anterior. (F) Localized reticulated erythema and bluish-grey macules consistent with irregular pale macules and patches over the left leg calf; note that pale macules and patches might be more obvious on the rear side of the right ankle
DISCUSSION
PPV had originally been classified into four major types.2 A fifth type, in which the vascular lesion is cutis marmorata telangiectatica congenita (CMTC), was subsequently added.3 Each type was further categorized according to the absence or presence of associated extracutaneous signs as types (a) and (b), respectively. In 2005, Happle proposed a new, simplified classification encompassing four groups, using descriptive terms: phacomatosis cesioflamea; phacomatosis spilorosea; phacomatosis cesiomarmorata and phacomatosis pigmentovascularis of non-classifiable type.4 In contrast to the traditional classification, this involves no subdivision between presentation with or without systemic symptoms. Furthermore, type I is excluded because there are no reported cases to date. chart 1 synthesizes the two classifications.5
CHART 1.
Classification of phacomatosis pigmentovascularis
| Type (according to Happle) | Type (according to Hasegawa*) | Vascular lesion | Pigmentary lesion |
|---|---|---|---|
| excluded nevus | I | Nevus flammeus | Verrucous and pigmented |
| Cesioflammea | II | Nevus flammeus ± anemic nevus | Mongolian spot |
| Spilorosea | III | Nevus flammeus ± anemic nevus | Nevus spilus |
| Non-classifiable | IV | Nevus flammeus ± anemic nevus | Mongolian spot, Nevus spilus |
| Cesiomarmorata | V | Cutis marmorata telangiectatica congenita | Mongolian spot |
Adapted from: Hasegawa Y, 1985.2 ; Happle R, 2005.4 and Segatto MM, 2013. 5
All subtypes, in accordance with Hasegawa, are subdivided into types (a) or (b) - with and without systemic involvement, respectively.
CMTC is a localized or widespread vascular anomaly, usually present at birth, and characterized by a persistent reticular vascular pattern with a marble-like, bluish or deep purple appearance. But it is believed that isolated CMTC is more common than suspected, as many patients may be overlooked.3 Similarly, in this case, localized CMTC consistent with nevus anemicus over the left leg calf was easily ignored.
Our patient exhibited nevus of Ota, extensive Mongolian spot, nevus flammeus, nevus anemicus and CMTC. This constellation does not fit with any of the traditional categories of PPV. In addition, this patient does not fulfill the criteria for any of the three types proposed by Happle, and can only be included in the unclassifiable category (Chart 1). To our knowledge, this is a totally different PPV case from the aforementioned, cutaneous abnormities, and it may represent a heretofore undescribed variant of PPV.
The pathogenesis of PPV is not completely clear yet, but it is commonly believed to be an abnormality in the development of melanocytic nevus and vasomotor neural cells derived from the neural crest. The thesis of 'twin spots' is the best accepted, genetic model to explain PPV, which involves two different recessive mutations of non-allelic genes, producing a doubly heterozygous embryo. Subsequently, mitotic recombination during early embryogenesis results in two homozygous daughter cell lines that migrate to different parts of the body and form a mosaic pattern of vascular and melanocytic lesions, namely, 'twin spots'.6
PPV without systemic presentations has a benign course, and does not need treatment. Nonetheless, treatment is performed mainly for aesthetic reasons, in order to enhance the quality of life of PPV patients. A Q-switched ruby laser and flashlamp-pumped, pulsed-dye laser, or a combination of the two, helps to improve skin lesions. Further, the best time for treatment is before school age.7
Footnotes
Financial Support: None.
How to cite this article: Ma H, Liao M, Qiu S, Luo R, Lu R, Lu C. The case of a boy with nevus of Ota, extensive Mongolian spot, nevus flammeus, nevus anemicus and cutis marmorata telangiectatica congenita: a unique instance of phacomatosis pigmentovascularis. An Bras Dermatol. 2015;90(3 Suppl 1):S10-12.
Work performed at the Third Affi liated Hospital, Sun Yat-sen University, Guangzhou, Guangdong, China.
References
- 1.Chang BP, Hsu CH, Chen HC, Hsieh JW. An infant with extensive Mongolian spot, naevus flammeus and cutis marmorata telangiectatica congenita: a unique case of phakomatosis pigmentovascularis. Br J Dermatol. 2007;156:1068–1071. doi: 10.1111/j.1365-2133.2007.07798.x. [DOI] [PubMed] [Google Scholar]
- 2.Hasegawa Y, Yasuhara M. Phakomatosis pigmentovascularis type IVa. Arch Dermatol. 1985;121:651–655. [PubMed] [Google Scholar]
- 3.Torrelo A, Zambrano A, Happle R. Cutis marmorata telangiectatica congenita and extensive Mongolian spots: type 5 phacomatosis pigmentovascularis. Br J Dermatol. 2003;148:342–345. doi: 10.1046/j.1365-2133.2003.05118.x. [DOI] [PubMed] [Google Scholar]
- 4.Happle R. Phacomatosis pigmentovascularis revisited and reclassified . Arch Dermatol. 2005;141:385–388. doi: 10.1001/archderm.141.3.385. [DOI] [PubMed] [Google Scholar]
- 5.Segatto MM, Schmitt EU, Hagemann LN, Silva RC, Cattani CA. Phacomatosis pigmentovascularis type IIa-case report. An Bras Dermatol. 2013;88:85–88. doi: 10.1590/abd1806-4841.20132248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Happle R1, Steijlen PM. Phacomatosis pigmentovascularis interpreted as a phenomenon of twin spots. Hautarzt. 1989;40:721–724. [PubMed] [Google Scholar]
- 7.Adachi K, Togashi S, Sasaki K, Sekido M. Laser therapy treatment of phacomatosis pigmentovascularis type II: two case reports. J Med Case Rep. 2013;7:55–55. doi: 10.1186/1752-1947-7-55. [DOI] [PMC free article] [PubMed] [Google Scholar]