Abstract
Proliferating pilomatricoma is proliferative, rare tumor variant of pilomatricoma. It is a benign neoplasm of hair matrix that can have potentially involve local recurrence. We report the case of a 60-year-old man who presented an asymptomatic nodule on the scalp. Histological exam demonstrated a basaloid epithelium at the periphery, filled with eosinophilic cornified material containing shadow cells. The tumor was excised and there was no evidence of recurrence one year later.
Keywords: Neoplasms, Pilomatrixoma, Scalp
INTRODUCTION
Proliferating pilomatricoma (PP) is a proliferative variant of pilomatricoma, first described by Kaddu S. et al in 1997. 1,2 It is considered a benign tumor, but local recurrence may occur if excision is incomplete. Very few cases of this rare neoplasm have been reported in the world. However, to the best of our knowledge, no case had previously been described in Brazil. We report a case of PP in the scalp without evidence of local recurrence one year after surgical treatment.
CASE REPORT
A 60-year-old Caucasian male hada had a three-year history of an asymptomatic nodular mass on the right temporal region of scalp. The patient reported gradual enlargement, but that quickly increased this size in the previous two months.
Dermatological examination revealed the firm mass, red, painless mass, measuring about 7cm x 3.5 cm, near the right supra-auricular area (Figure 1). The regional lymph nodes were not enlarged.
FIGURE 1.

Firm, red, nodular mass on the right temporal region of the scalp
Macroscopic examination: the tumor was well-circumscribed, nodular, dull white, surrounded by slightly compressed fibrous tissues, measuring about 6 x 3 x 2.3 cm (Figure 2).
FIGURE 2.

Macroscopic examination: well-circumscribed, nodular, dull white, surrounded by slightly compressed fibrous tissues
Microscopic examination: lesion predominantly composed of a lobular proliferation of basaloid epithelium at the periphery, filled with eosinophilic cornified material and shadow cells (Figures 3, 4 and 5).
FIGURE 3.
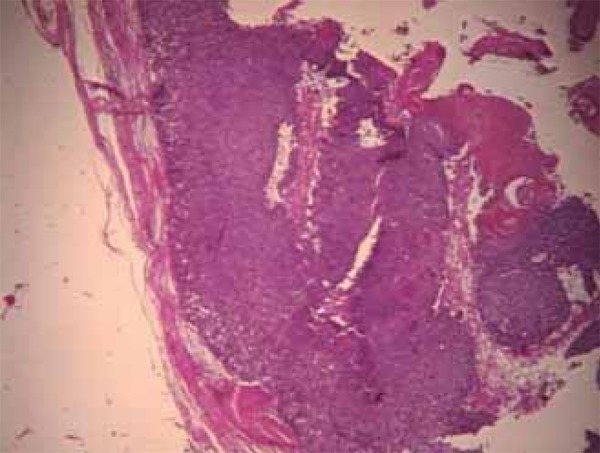
Lesion lined by a basaloid epithelium at the periphery, filled with eosinophilic cornified material and shadow cells (HE 200x)
FIGURE 4.
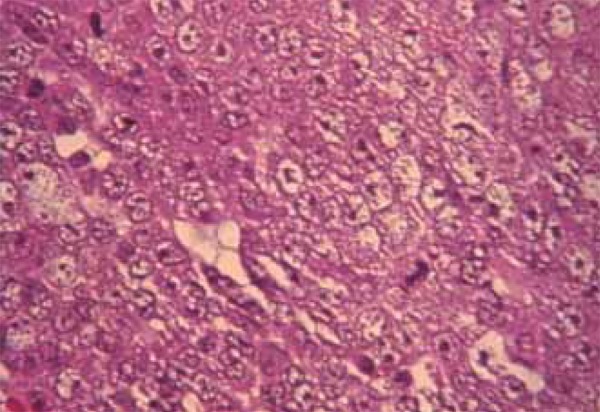
Lesion with area of basaloid cells with mitotic figures (HE 400x)
FIGURE 5.
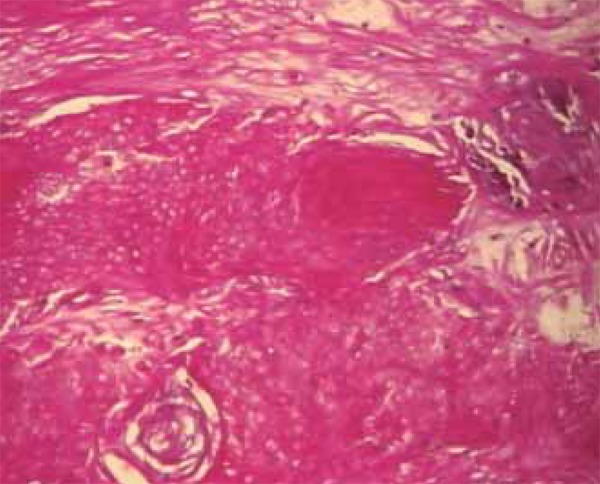
Detail of the cornified material and shadow cells with fibrotic stroma (HE 400x)
DISCUSSION
Proliferating pilomatricoma (PP) was diagnosed based on clinical and histopathological findings.
Pilomatricoma or calcifying epithelioma of Malherb (CEM), first described in 1880 by Malherb and Chenantais, represents approximately 1% of all benign skin tumors and it is the second most common cutaneous neoplasm in childhood and youth. It is a slow-growing, firm, dermal or subcutaneous neoplasm, usually measuring under 3 cm in diameter. Pilomatricomas are considered benign and rarely recur after surgical excision. 3-7 However, cases of CEM with a tendency for focal invasiveness and local recurrence have been reported and designated firstly as aggressive pilomatricomas. 1,2
In 1997 Kadduet al. examined retrospectively cases of CEM and found instances of unusual, architectural, histopathologic features. On clinical examination, most patients were elderly individuals; the lesions were found to be painless, dome- shaped, solitary, painless, medium- to large-sized nodules on the head and neck regions. Histopathological evaluation revealed relatively large lesions predominantly composed of a lobular proliferations of basaloid cells, exhibiting variable nuclear atypia and mitotic figures, focal areas containing eosinophilic, cornified material, along with shadow cells. Proliferating pilomatricoma was proposed by these authors as a histopathologically distinctive subset of pilomatricoma and it was considered a proliferative variant of CEM.1,2
Kadduet al. considered PP a benign tumor because of a histopathological profile that implied benignancy: relative symmetry, sharp circumscription, lack of ulceration in the majority of cases, a fibrous tissue arranged compactly around the neoplasm, and lack of perineural or intravascular involvement by basaloid cells. 1
Current incidence and prevalence is unknown due to the low number of cases reported.1 However, Satohet al.1 compiled the available clinical data from all previously reported cases. Although it was a small series, some aspects are nevertheless noticeable and some clinical information was highlighted: there were 7 males and 8 females (men and women are almost equally affected); patients appeared to be older than those with classical pilomatricoma (ranging from 18 to 88 years); the lesions measured 1.5 to 5.5 cm in diameter, typically larger than in classical CEM (0.5-1.6 cm); nodules situated mostly on the head and neck. Our case entailed the afore mentioned clinical aspects.
Differential diagnoses for PP include: basal-cell carcinoma, epidermal cyst, pyogenic granuloma, other neoplasms with metrical differentiation, and matrical carcinoma (pilomatrix carcinoma). 2,8-10
Malignant transformation of CEM in to a pilomatrix carcinoma should be suspected in cases with repeated local recurrences. 5,10 Hence, theorically, PP may develop in to pilomatrix carcinoma.
The treatment of choice for PP is complete surgical lesion resection, as in the present case. 1 The lesion was removed with a 3-mm margin. Local recurrence may occur if excision is incomplete. 1,2 Our patient showed no signs of local recurrence one year after the excision (Figure 6).
FIGURE 6.

Patient showing no evidence of local recurrence one year after surgical treatment
Footnotes
Financial Support: None.
How to cite this article: Kondo RN, Pontello Junior R, Belinetti FM, Cilião C, Vasconcellos VRB, Grimald DM. Proliferating pilomatricoma - Case report. An Bras Dermatol. 2015;90 (3 Suppl 1):S94-6.
Work performed at the Serviço de Dermatologia do Hospital Universitário Regional do Norte do Paraná da Universidade Estadual de Londrina (HU-UEL)- Paraná (PR), Brazil.
References
- 1.Satoh M, Ookouchi M, Yamamoto T. Photoletter to the editor: Proliferating pilomatricoma with no recurrence during a 3-year follow-up. J Dermatol Case Rep. 2012;6:127–129. doi: 10.3315/jdcr.2012.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sakai A, Maruyama Y, Hayashi A. Proliferating pilomatricoma: a subset of pilomatricoma. J Plast Reconstr Aesthet Surg. 2008;61:811–814. doi: 10.1016/j.bjps.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Kaddu S, Kerl H. Appendage tumors of the skin. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick's Dermatology in General Medicine. 6th ed. New York, NY: McGraw-Hill Co; 2003. pp. 785–808. [Google Scholar]
- 4.Fonseca RPL, Andrade JS, Filho, Araujo IC, Silva AF, Filho, Pereira NA, Carvalho EES, et al. Pilomatricoma: epitelioma calcificado de Malherbe. Rev Bras Cir Plast. 2012;27:605–610. [Google Scholar]
- 5.Pant I, Joshi SC, Kaur G, Kumar G. Pilomatricoma as a diagnostic pitfall in clinical practice: report of two cases and review of literature. Indian J Dermatol. 2010;55:390–392. doi: 10.4103/0019-5154.74566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaddu S, Soyer HP, Hödl S, Kerl H. Morphological stages of pilomatricoma. Am J Dermatopathol. 1996;18:333–338. doi: 10.1097/00000372-199608000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Hernández-Núñez A, Nájera Botello L, Romero Maté A, Martínez-Sánchez C, Utrera Busquets M, Calderón Komáromy A, et al. Estudio retrospectivo de pilomatricomas: 261 tumores en 239 pacientes. Actas Dermosifiliogr. 2014;105:699–705. doi: 10.1016/j.ad.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Hague JS, Maheshwari M, Ryatt KS, Abdullah A. Proliferating pilomatricoma mimicking pyogenic granuloma. J Eur Acad Dermatol Venereol. 2007;21:688–689. doi: 10.1111/j.1468-3083.2006.01985.x. [DOI] [PubMed] [Google Scholar]
- 9.Barbosa AA, Júnior, Guimarães NS, Sadigursky M, Dantas RJ, Júnior, Tavares I, Brandão M. Pilomatrix carcinoma (malignant pilomatricoma): a case report and review of the literature. An Bras Dermatol. 2000;75:581–585. [Google Scholar]
- 10.Sassmannshausen J, Chaffins M. Pilomatrix carcinoma: a report of a case arising from a previously excised pilomatrixoma and a review of the literature. J Am Acad Dermatol. 2001;44:358–361. doi: 10.1067/mjd.2001.105474. [DOI] [PubMed] [Google Scholar]


