Abstract
Background
Survival is less than 10% for pediatric patients following out-of-hospital cardiac arrest. It is not known if more time on the scene of the cardiac arrest and advanced life support interventions by emergency services personnel are associated with improved survival.
Aim
This study was performed to determine which times on the scene and which prehospital interventions were associated with improved survival.
Methods
We studied patients aged 3 days to 19 years old with out-of-hospital cardiac arrest, using the Resuscitation Outcomes Consortium cardiac arrest database from 11 North American regions, from 2005 to 2012. We evaluated survival to hospital discharge according to on-scene times (< 10, 10 to 35 and > 35 minutes).
Results
Data were available for 2244 patients (1017 infants, 594 children and 633 adolescents). Infants had the lowest rate of survival (3.7%) compared to children (9.8%) and adolescents (16.3%). Survival improved over the 7 year study period especially among adolescents. Survival was highest in the 10 to 35 minute on-scene time group (10.2%) compared to the > 35 minute group (6.9%) and the < 10 minute group (5.3%, p=0.01). Intravenous or intra-osseous access attempts and fluid administration were associated with improved survival, whereas advanced airway attempts were not associated with survival and resuscitation drugs were associated with worse survival.
Conclusions
In this observational study, a scene time of 10 to 35 minutes was associated with the highest survival, especially among adolescents. Access for fluid resuscitation was associated with increased survival but advanced airway and resuscitation drugs were not.
1. Introduction
Survival following pediatric out-of-hospital cardiac arrest is less than 10% and, for those who survive, many have an unfavorable neurological outcome.1–10 Older age, a shockable first rhythm, and a witnessed arrest are non-modifiable factors associated with improved survival in pediatric patients.1, 3, 6–8, 11–15 Bystander cardiopulmonary resuscitation, the early arrival of emergency medical service personnel on the scene and early defibrillation are modifiable factors associated with improved survival.15–20
The level of training of emergency medical services personnel, who respond to the emergency, is also a modifiable factor which has been the focus of several studies.17, 21–24 Spending more time at the scene of the arrest to provide basic life support may improve the quality of cardiopulmonary resuscitation25, 26 and outcomes.27 With advanced life support training paramedics have learned to perform endotracheal intubation, insert intravenous catheters or intra-osseous needles and to deliver resuscitation fluids and medications. However, a paramedic’s success with endotracheal intubation in a child is variable2, 4, 28 and complication rates are high.29, 30 The procedure leads to interruptions in chest compressions31, 32 and may also delay timely transfer to a hospital.17, 33, 34 It is not known if length of time on scene, level of care (basic versus advanced life support) or administration of intravenous fluids or medications are associated with improved survival for pediatric patients with out-of-hospital cardiac arrest.
We hypothesized that longer times on scene to deliver advanced life support interventions would be associated with improved survival. To address this hypothesis we performed a retrospective study using data from the Resuscitation Outcomes Consortium (ROC) database.35
2. Methods
This is a retrospective observational analysis of data collected prospectively according to pre-defined and consistently applied data definitions.35
2.1. Patient population
Data for all 9-1-1 calls for non-traumatic cardiac arrest leading to emergency medical services response within 8 American and 3 Canadian regions were submitted to the ROC Epistry-Cardiac Arrest database at the data coordinating center at the University of Washington. The ROC regions include an urban, suburban and rural population of approximately 24 million. Inclusion criteria were patients with out-of-hospital cardiac arrest who were 3 days to 19 years old treated by participating emergency medical services agencies for cardiac arrest and who had attempts at external defibrillation and/or chest compressions by emergency medical services personnel. Patients were excluded if the cardiac arrest was not treated, the cause of the cardiac arrest was perinatal or traumatic, the patient was enrolled in an ongoing ROC therapeutic trial, or if scene time or survival-to-hospital-discharge data were missing. Criteria for attempting or terminating resuscitation by emergency medical services personnel were determined by local regulations and were not standardized among study sites. These data were collected as part of an observational study that met the requirements for minimal risk research in the United States and Canada and was approved by 134 Research Ethics or Institutional Review Boards. Additional memoranda of understanding for data sharing were acquired from 24 hospitals and 94 Emergency Medical Services agencies.
2.2. Data collection
We studied patients with cardiac arrest occurring from December, 2005 to December, 2012 with outcomes measured until April, 2013. Data included the following variables: aetiology of the arrest, basic resuscitation measures attempted (assisted ventilation, chest compressions, defibrillation), first monitored rhythm, witnessed arrest (by lay person or health care provider), bystander cardiopulmonary resuscitation (CPR), interventions (attempts at advanced airway placement, intravenous and intra-osseous access, fluid administration and resuscitation drug delivery, including adrenaline, atropine and bicarbonate), level of training of emergency medical services personnel (basic life support with defibrillation or advanced life support), and time intervals (time to emergency medical services arrival, scene time, and transport time). Data on successful completion of the attempted interventions was not available. Scene time was defined as the time between when the first emergency medical services crew arrived at the scene to the time of departure from the scene with the patient or to the time of patient death if declared dead at the scene.
The primary outcome was survival to hospital discharge. The secondary outcome was pre-hospital return of spontaneous circulation (ROSC).
2.3. Statistical analysis
Descriptive analyses were performed for baseline and cardiac arrest characteristics, interventions, and outcomes according to scene time and age categories. Categories of scene time (< 10, 10 to 35 and > 35 minutes) were chosen based on histograms of scene times in our population and clinical rationale. In a previous study, scene times < 10 minutes were defined as a “scoop and run” approach.1 The age categories (infants < 1 year, children aged 1 to 11 years and adolescents aged 12 to 19 years) were chosen based on clinical rationale and to match a previous ROC epidemiologic study.1 Characteristics of emergency medical services arrival time, scene time and departure and transport times were also analyzed by scene time and age categories. Emergency medical services arrival time categories (< 5, 5 to 7, > 7 minutes) were chosen based on published evidence of best outcome for arrival at the scene in < 5 minutes16, 36 and the widely accepted goal of arrival at the scene in < 8 minutes.37 To minimize selection bias, we included all patients if they had attempts at resuscitation, even if they were declared dead on the scene. The rationale for this decision was that at the start of resuscitation, for pediatric patients, an emergency medical services team will not have decided whether or not to continue resuscitation efforts or declare death. Protocols for declaration of death in the field differed between study sites.
All variables in our regression models were chosen a priori and based on scientific rationale. We designed the first regression model to study factors that may be associated with scene time as a continuous outcome. In this linear regression model, we included age category, gender, aetiology of arrest, bystander witnessed arrest, study site, initial rhythm, emergency medical services arrival time, intravenous or intra-osseous attempts, and advanced airway attempts as we reasoned that these variables would be associated with scene time.
To study scene-related factors associated with survival we developed a second model using logistic regression with categorical scene time as the predictor of interest and survival to hospital discharge as the outcome. This model was adjusted for age, gender, aetiology of arrest, witnessed status, initial rhythm, emergency medical services arrival time, advanced life support arrival at > 7 minutes, defibrillation attempted, intravenous or intra-osseous attempts, fluid administration, advanced airway attempts, resuscitation medications, and ROC study site. This analysis was completed first for all patients and then was stratified by age category. For both models, coefficients were estimated using maximum likelihood methods and 95% confidence intervals were calculated using Huber-White robust estimates of the standard error. For coefficients for binary variables we used the Wald test with Huber-White standard error estimates and for categorical variables with greater than two values we used likelihood ratio tests.
We developed adjusted curves to visualize the relationships between survival and scene time, for all patients and for the three age groups, using quadratic equations. We also measured survival to hospital discharge and ROSC across the 7 years of the study for the three age groups and estimated the linear association between the year and the outcome. Statistical analyses were performed using R, version 2.15.1, and SAS, version 9.3.
3. Results
3.1. Patient characteristics
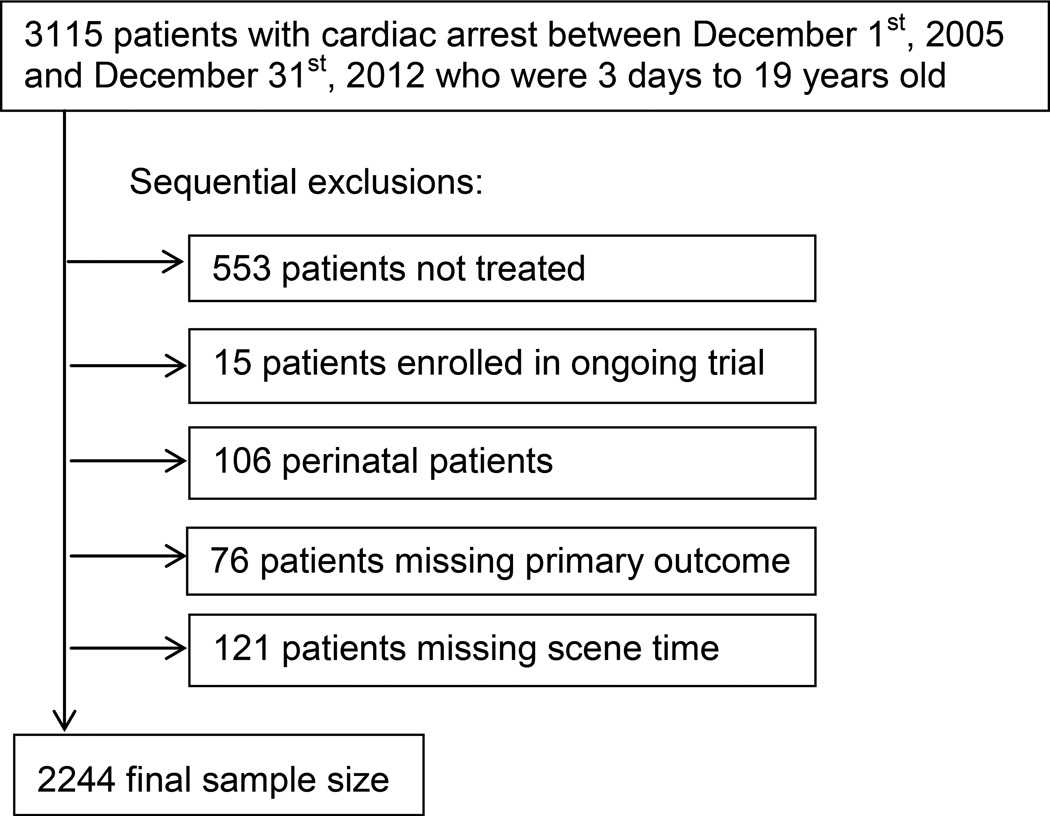
During the 7 year study period, there were 3115 paediatric cardiac arrest victims of which 2244 were eligible for the study (Fig. 1). Patient and cardiac arrest characteristics are listed according to scene time categories in Table 1 and according to age categories in Appendix Table 1. Data was missing on less than 5% of cases for each variable individually. No obvious cause was listed most commonly (74.8%) as the aetiology of the cardiac arrest and only 82 (3.7%) patients had respiratory cause chosen as the aetiology of the cardiac arrest. Just over a third (37.4%) of all patients received bystander cardiopulmonary resuscitation. Asystole was the most common initial monitored rhythm (65.9%). The majority of patients had bag-valve-mask ventilation [2105 of 2244 (93.8%)] and an advanced airway was attempted in 1526 (68.0%) of patients. Intravenous or intra-osseous access was attempted in 1786 (79.6%) of patients, fluid was administered in 1461 (65.1%), and adrenaline (epinephrine) was given to 1530 (68.2%) patients.
Fig. 1. Enrollment.
Table 1.
Demographics, event characteristics, interventions and time intervals according to scene time categories.
| Characteristic n (%) | < 10 minutes (n=486) |
10 to 35 minutes (n=1542) |
> 35 minutes (n=216) |
Total (n=2244) |
|---|---|---|---|---|
| Age | ||||
| Infant | 311 (64.0) | 629 (40.7) | 77 (35.6) | 1017 (45.3) |
| Child | 126 (25.9) | 427 (27.7) | 41 (19.0) | 594 (26.5) |
| Adolescent | 49 (10.1) | 486 (31.5) | 98 (45.4) | 633 (28.2) |
| Gender | ||||
| Male | 301 (61.9) | 927 (60.2) | 137 (63.4) | 1365 (60.9) |
| Aetiology of arrest* | ||||
| No obvious cause | 394 (81.1) | 1145 (74.3) | 140 (64.8) | 1679 (74.8) |
| Respiratory | 12 (2.5) | 55 (3.6) | 15 (6.9) | 82 (3.7) |
| Submersion | 21 (4.3) | 91 (5.9) | 15 (6.9) | 127 (5.7) |
| Other | 58 (11.8) | 249 (16.1) | 45 (20.8) | 352 (15.7) |
| Unknown | 1 (0.2) | 2 (0.1) | 1 (0.5) | 4 (0.2) |
| Witnessed | 95 (19.5) | 427 (27.7) | 64 (29.6) | 586 (26.1) |
| Layperson/Bystander | 84 (17.3) | 359 (23.3) | 53 (24.5) | 496 (22.1) |
| EMS | 11 (2.3) | 68 (4.4) | 11 (5.1) | 90 (4.0) |
| Bystander CPR | 188 (38.7) | 569 (36.9) | 83 (38.4) | 840 (37.4) |
| Initial rhythm | ||||
| VF/VT | 17 (3.5) | 133 (8.6) | 18 (8.3) | 168 (7.5) |
| PEA | 37 (7.6) | 198 (12.8) | 39 (18.5) | 275 (12.3) |
| Asystole | 314 (64.6) | 1038 (67.3) | 129 (59.7) | 1476 (65.9) |
| Undetermined | 52 (10.7) | 136 (8.8) | 20 (9.3) | 208 (9.3) |
| EMS defibrillation | 22 (4.5) | 205 (13.3) | 45 (20.8) | 272 (12.1) |
| Interventions† | ||||
| IV/IO attempted | 235 (48.4) | 1349 (87.5) | 202 (93.5) | 1786 (79.6) |
| Fluids administered | 184 (37.9) | 1093 (70.9) | 184 (85.2) | 1461 (65.1) |
| Adrenaline | 153 (31.5) | 1187 (77.0) | 190 (88.0) | 1530 (68.2) |
| Atropine | 32 (6.6) | 489 (31.7) | 108 (50.0) | 629 (28.0) |
| Bicarbonate | 6 (1.2) | 182 (11.8) | 82 (38.0) | 270 (12.0) |
| Any drug | 155 (31.9) | 1199 (77.8) | 192 (88.9) | 1546 (68.9) |
| Two or more drugs | 32 (6.6) | 578 (37.9) | 135 (62.5) | 745 (33.2) |
| Bag valve mask ventilation | 428 (88.1) | 1476 (95.7) | 201 (93.1) | 2105 (93.8) |
| Supraglottic airway | 7 (1.4) | 86 (5.6) | 16 (7.4) | 109 (4.9) |
| Oral/Nasal ETT | 151 (31.1) | 1119 (72.6) | 179 (82.9) | 1449 (64.6) |
| Minutes, median (IQR) | ||||
| Scene time | 6.4 (4.4, 8.2) | 20.6 (15.4, 26.0) | 42.0 (38.2, 48.7) | 18.6 (11.0, 26.9) |
| 9-1-1 to EMS arrival | 5.2 (4.1, 6.8) | 5.1 (4.0, 6.5) | 5.3 (4.0, 7.0) | 5.1 (4.0, 6.7) |
| 9-1-1 to ALS arrival | 6.0 (4.5, 8.0) | 6.7 (4.9, 9.5) | 8.4 (5.9, 12.7) | 6.7 (4.9, 9.3) |
| EMS to CPR‡ | 1.1 (0.6, 2.3) | 1.6 1.0, 3.0) | 1.9 (1.0, 3.5) | 1.5 (0.9, 2.9) |
| Transport time§ | 7.0 (4.4, 10.1) | 7.0 (4.6, 10.0) | 9.3 (5.0, 16.0) | 7.1 (4.6, 10.5) |
EMS denotes emergency medical services; CPR, cardiopulmonary resuscitation; VF/VT, ventricular fibrillation or ventricular tachycardia; PEA, pulseless electrical activity; ETT, endotracheal tube; IV, intravenous; IO, intra-osseous; ALS, advanced life support; IQR, interquartile range
Aetiology of arrest is defined as clinical impression of emergency medical services personnel
The intervention was attempted, not necessarily successful
Emergency medical services personnel arrival to initiation of CPR
Scene departure to emergency department arrival at first hospital. Transport time not available for patients declared dead at the scene.
3.2. Scene time
There was a significant inter-site variability in scene time but mean scene time was stable across the seven years of the study (Appendix Fig. 1). The majority of patients [1542 of 2244 (68.7%)] had a scene time between 10 and 35 minutes (Table 1). For scene time < 10 minutes, there were fewer witnessed events, shockable rhythms, attempts to establish an advanced airway, intravenous or intra-osseous access attempts and fewer drugs given compared to the longer scene time categories (Table 1). The variables that were independently associated with scene time in the first regression model were age, interventions, and site (Appendix Table 2).
3.3. Age
Children and adolescents had more witnessed events (34.8% and 37.8%, respectively) than infants (13.8%, Appendix Table 1). Emergency medical services personnel arrived and commenced cardiopulmonary resuscitation more quickly for infants compared to adolescents. Adolescents more frequently had ventricular fibrillation or ventricular tachycardia as the initial rhythm (19.1%) compared to both children and infants (< 5%).
3.4. Survival to hospital discharge
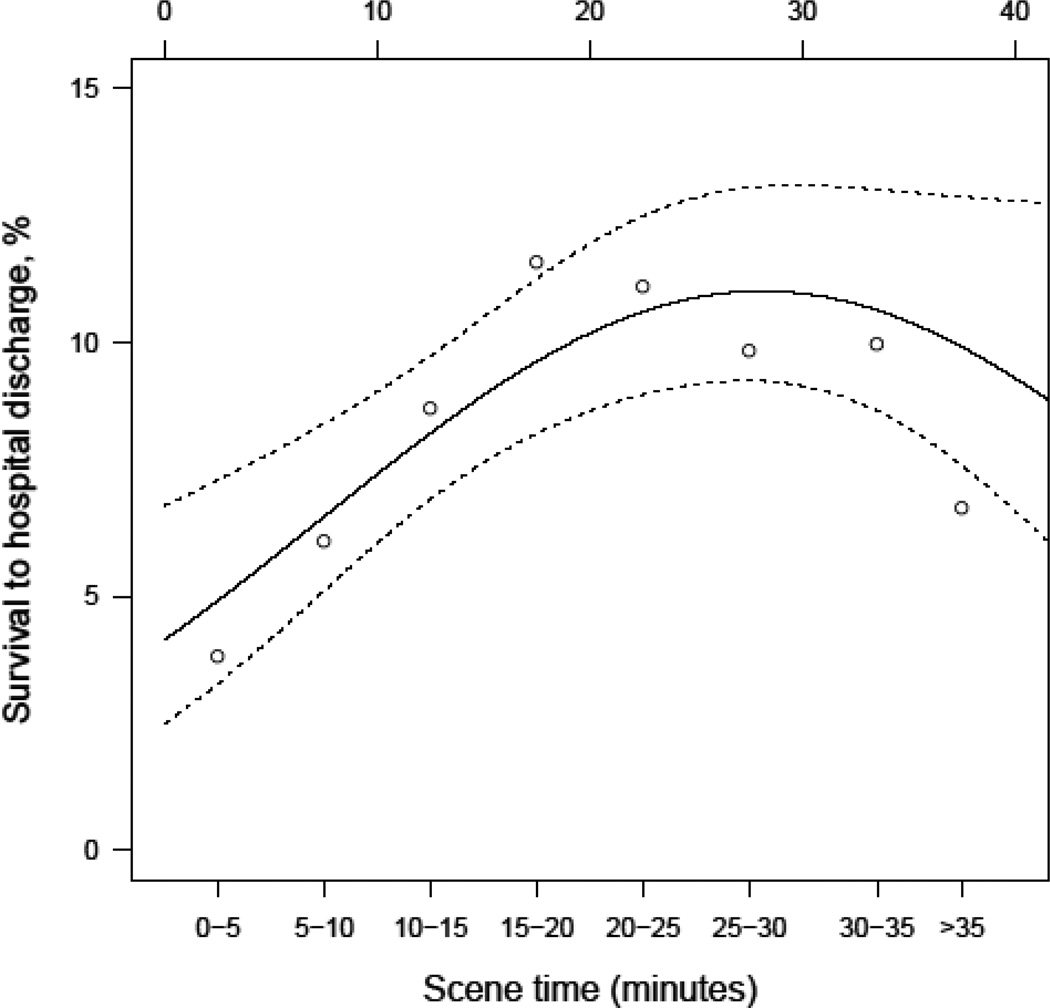
Survival to hospital discharge was highest (10.2%) in the 10 to 35 minute scene time group compared to 6.9% in the > 35 minute group and 5.3% in the < 10 minute group (Table 2). When survival was analyzed by scene time divided into five minute intervals the highest survival was 11.6% at 15 to 20 minutes (Fig. 2) but the association between scene time and survival differed between the different age groups (Appendix Fig. 2).
Table 2.
Outcomes according to scene time and age categories.
| Characteristic n (%) | < 10 minutes (n=486) |
10 to 35 minutes (n=1542) |
> 35 minutes (n=216) |
Total (n=2244) |
|---|---|---|---|---|
| Any prehospital ROSC | 21 (4.3) | 299 (19.4) | 76 (35.2) | 396 (17.6) |
| Survival* | 26 (5.3) | 158 (10.2) | 15 (6.9) | 199 (8.9) |
| Characteristic n (%) | Infant (n=1017) 3 days to < 1 year | Child (n=594) 1 to 11 years | Adolescent (n=644) 12 to 19 years | Total (n=2244) |
| Any prehospital ROSC | 73 (7.2) | 102 (17.2) | 221 (34.9) | 396 (17.6) |
| Survival* | 38 (3.7) | 58 (9.8) | 103 (16.3) | 199 (8.9) |
ROSC indicates return of spontaneous circulation
ED denotes emergency department
Survival to hospital discharge
Fig. 2. Survival to hospital discharge according to scene times.
Data are the percent survival to hospital discharge by scene time in 5 minute intervals for all patients. The curved, solid line represents a quadratic fit to the observed survival rates treating the scene time as continuous. The quadratic fit makes an assumption about the shape of the relationship between scene time and survival and should be interpreted with caution. The dotted lines represent the lower and upper boundaries of a 95% confidence interval.
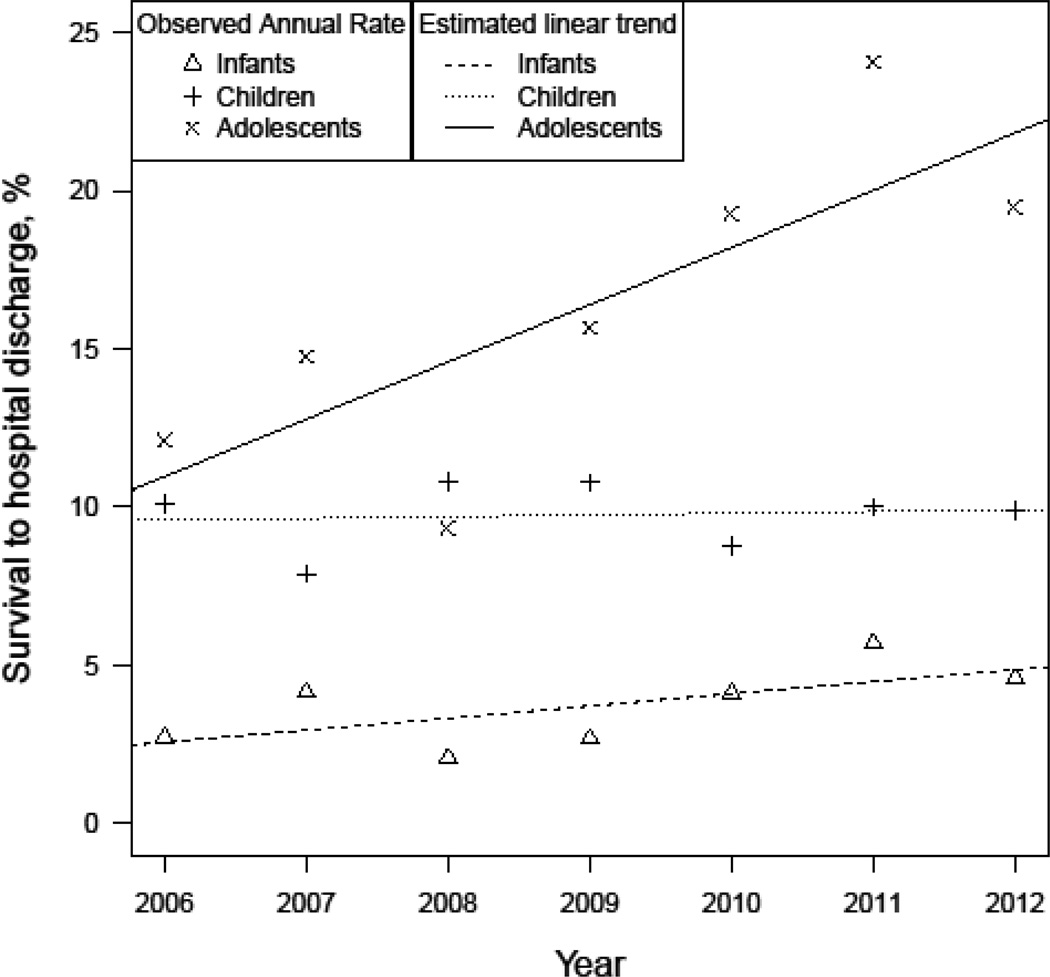
Infants had the lowest rate of survival to hospital discharge (3.7%) compared to children (9.8%) and adolescents (16.3%) (Table 2). Adolescent survival increased from 12.1% to 19.5% (range 9.3 to 24.1%) over the study period (Fig. 3). This trend was not observed in children and only slightly in infants.
Fig. 3. Survival to hospital discharge according to age categories over the study period.
Data shown are the percent survival to hospital discharge from 2006 - 2012 for infant, child, and adolescent age categories. Points represent the observed survival to hospital discharge rate for the specific age group and the lines are the estimated linear associations between year and survival for each age category. 2005 was removed from this plot as our data collection only included 1 month in that year (December).
The inclusion of the three categories of scene time in the adjusted multi-variable regression model of scene-related factors associated with survival significantly improved the model at p=0.01 (Table 3). Other variables which were significantly associated with survival in the multi-variable regression model included site, older age category, aetiology of arrest as drowning, witnessed arrest, the initial monitored rhythm of ventricular fibrillation or ventricular tachycardia, intravenous or intra-osseous attempts and fluid administration (Table 3). There was a negative association with resuscitation medication delivery and survival (Table 3). Defibrillation, and advanced airway attempts were not associated with survival (Table 3). A subgroup analysis was performed for survival in the adolescent group and attempts at an advanced airway and defibrillation again were not associated with survival.
Table 3.
Multivariable regression model for survival to hospital discharge.
| Characteristic | Odds Ratio (95th CI) |
|---|---|
| Scene Time (reference: 10 to 35 minutes)* | |
| < 10 minutes | 0.69 (0.36, 1.31) |
| > 35 minutes | 0.37 (0.17, 0.77) |
| Age (reference: infant)* | |
| Child | 2.12 (1.18, 3.77) |
| Adolescent | 2.40 (1.33–4.30) |
| Gender (reference: female) | |
| Male | 0.83 (0.56, 1.22) |
| Aetiology of arrest (reference: no obvious cause)* | |
| Respiratory | 1.07 (0.44, 2.63) |
| Submersion | 3.48 (1.71, 7.10) |
| Other | 1.26 (0.71, 2.26) |
| EMS or bystander witnessed | 3.87 (2.55, 5.89)* |
| Initial rhythm (reference: VF/VT)* | |
| PEA | 0.39 (0.20, 0.78) |
| Asystole | 0.10 (0.05, 0.20) |
| Undetermined | 0.64 (0.26, 1.60) |
| EMS arrival time (reference: < 5 minutes) | |
| 5 to 7 minutes | 0.68 (0.43, 1.06) |
| > 7 minutes | 0.55 (0.27, 1.14) |
| ALS arrival time > 7 minutes | 0.69 (0.43, 1.13) |
| Interventions (reference: none) | |
| Defibrillation† | 1.66 (0.88, 3.10) |
| IV/IO attempt | 2.40 (1.20, 4.81)* |
| Fluid administration | 1.73 (1.07, 2.80)* |
| Advanced airway attempts | 0.69 (0.43, 1.10) |
| Resuscitation drug‡ | 0.24 (0.15, 0.39)* |
| ROC Study Site§ | N/A* |
EMS denotes emergency medical services; VF/VT, ventricular fibrillation or ventricular tachycardia; PEA, pulseless electrical activity; ALS, advanced life support; ROC, Resuscitation Outcomes Consortium; CI, confidence interval
p < 0.05
By emergency medical services personnel or public access defibrillation
Any resuscitation drug including adrenaline, atropine or bicarbonate
Odds Ratio not relevant, one random site chosen as reference
Neither the arrival time for emergency medical services nor the arrival of advanced life support providers first on the scene was associated with survival (Table 3). Almost all patients [2178 of 2244 (97.1%)] in our study were cared for by personnel with advanced life support training. We were therefore unable to compare the effects of advanced versus basic life support training of emergency medical services personnel on survival.
3.5. Secondary outcome
Infants had the lowest rates of prehospital ROSC (7.2%) compared to children (17.2%), and adolescents (34.9%) (Table 2). Pre-hospital ROSC increased for all three age groups, over the study period (Appendix Fig. 3).
4. Discussion
Using data from the largest cohort of children with non-traumatic out-of-hospital cardiac arrest in the United States and Canada, our study demonstrated that scene time was significantly associated with survival to hospital discharge. The highest survival occurred with a scene time of 10 to 35 minutes (10.2 %) followed by scene times of greater than 35 minutes (6.9 %) and less than 10 minutes (5.3 %).We also showed that only certain interventions were associated with survival. Attempts at placement of intravenous and/or intra-osseous catheters or needles and administration of intravascular fluids were associated with improved survival whereas attempts at placement of an advanced airway was not and resuscitation drug delivery was negatively associated with survival. Times on scene of greater than 10 minutes were associated with more interventions suggesting that a scoop and run approach of less than 10 minutes on scene does not allow enough time to apply interventions that may benefit the patient.
Survival among adolescents increased, although there was no significant change in scene time, over the 7 years of the study. Adolescents had the highest rate of survival, followed by children, and then infants. Infants also had the shortest scene time and fewest interventions. Infants also had the lowest rate of witnessed events (13.8%) and the cause of the arrest listed as unknown was the highest (82.4%). Therefore, there may be a large number of infants who had sudden infant death syndrome but were not declared dead at the scene. This may have contributed to the higher rate of scoop and run responses for infants (64.0%).
Longer times on the scene (> 35 minutes) were associated with the highest rates of ROSC but lower rates of survival compared to 10 to 35 minutes on the scene. Emergency medical services personnel must be aware of this paradox, weighing the potential benefits of spending more time on the scene to achieve ROSC with decreasing survival due to longer ischemic times, when deciding when to depart the scene.
Our results that attempts at placement of an advanced airway by paramedics in pediatric out-of-hospital cardiac arrest is not associated with improved survival are supported by a previous study.29 Securing an advanced airway results in interruptions in CPR and may lead to harmful hyperventilation. Furthermore, there are significant anatomical differences in infants and children making intubation in younger patients more prone to error and complications. In a previous study conducted in an urban setting, paramedics had infrequent opportunities to intubate a child; once every 3 years.38 More research is needed to determine optimal airway management in infants and children with out-of-hospital cardiac arrest.
Interestingly, we found that attempting to place intravenous or intra-osseous access by emergency medical services personnel was associated with improved survival whereas drug delivery was associated with worse survival. There are several factors that may help to explain this paradox. The establishment of an intravenous or intra-osseous needle allows for timely post-resuscitation therapies that are likely to benefit the patient. These include administration of fluid boluses or continuous infusion of inotropes and vasoactive medications. Data on inotrope and vasoactive drug infusions were inconsistently recorded in the ROC database. The administration of resuscitation drugs is known to be associated with more prolonged cardiac arrest and therefore worse outcomes in pediatric patients with in-hospital cardiac arrest.39 Multiple doses of resuscitation drugs, given in the emergency department, were also associated with a high mortality and poor neurological outcome among survivors in previous studies of children and adolescents with out-of-hospital cardiac arrest.3, 40
Survival to hospital discharge in our study (8.9%) is slightly higher than reported from ROC in 2009 (7.8%) suggesting an improvement in survival over the past 5 years.1 In a systematic review of 41 pediatric articles spanning 30 years to 2004, the survival to hospital discharge from pediatric out-of-hospital cardiac arrest was 6.7%.7 We also showed a trend of increased survival among adolescents over the study period. Our study is unique in that the emergency medical services providers were participating in a large consortium with several adult cardiac arrest trials underway. Training and feedback may have strengthened the resuscitation efforts of participating emergency medical services leading to improved survival over time especially among the adolescents who are more adult-like in anatomy and physiology compared to infants and children.
Our study has several strengths. Our sample size was large whereas most other studies in pediatric out-of-hospital cardiac arrest have small numbers of patients. Our study was based on a uniform definition of cardiac arrest, well defined and validated data variables as well as regular data entry quality assessments and quality improvement. Thus, the validity, accuracy and conclusions of our study may have greater strength compared to many other studies in pediatric out-of-hospital cardiac arrest.
There are inherent limitations to observational database research. Despite the data being collected prospectively, causality could not be proven. Specific details about the interventions, such as number of attempts and rates of success, were not consistently available. Furthermore, aetiology of arrest and neurologic outcomes were unknown for many subjects limiting the potential analyses of these variables. We studied a heterogeneous population and, even though we controlled for important variables in our regression models, we could not account for unmeasured confounders. Limitations specific to this study included unmeasured site differences in practices by emergency medical services and hospital post-resuscitation care. We were therefore unable to measure how these confounding variables were associated with survival.
5. Conclusions
In this large observational study of pediatric out-of-hospital cardiac arrest there was a significant association between scene time and survival. The highest survival (10.2%) occurred with a time on scene of 10 to 35 minutes. Attempts at placement of intravenous or intra-osseous needles or catheters and fluid administration were associated with improved survival. Attempts at placement of an advanced airway were not associated with survival and administration of resuscitation drugs was associated with worse survival. Survival improved over the 7 year study period especially among adolescents.
Supplementary Material
Acknowledgements
The authors would like to thank Umberto Lenzi for organizing and providing technical assistance for writing group teleconference sessions and to Dr. M. Drake for helping to review the literature. We thank Dr. Brian Kavanagh for his critical review of the manuscript. The ROC is supported by a series of cooperative agreements to nine regional clinical centers and one Data Coordinating Center (5U01 HL077863-University of Washington Data Coordinating Center, HL077866-Medical College of Wisconsin, HL077867-University of Washington, HL077871-University of Pittsburgh, HL077872-St. Michael’s Hospital, HL077873-Oregon Health and Science University, HL077881-University of Alabama at Birmingham, HL077885-Ottawa Hospital Research Institute, HL077887-University of Texas SW Medical Ctr/Dallas, HL077908-University of California San Diego) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defence Research and Development Canada and the Heart, Stroke Foundation of Canada and the American Heart Association. The study sponsors were not involved in the study design, data collection, analysis or interpretation, in the writing of the manuscript, nor in the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
The authors have no conflicts of interest to disclose.
References
- 1.Atkins DL, Everson-Stewart S, Sears GK, et al. Resuscitation Outcomes Consortium Investigators. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119:1484–1491. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foltin GL, Richmond N, Treiber M, et al. Pediatric prehospital evaluation of NYC cardiac arrest survival (PHENYCS) Pediatr Emer Care. 2012;28:864–868. doi: 10.1097/PEC.0b013e3182675e70. [DOI] [PubMed] [Google Scholar]
- 3.Young KD. A Prospective, Population-Based Study of the Epidemiology and Outcome of Out-of-Hospital Pediatric Cardiopulmonary Arrest. Pediatrics. 2004;114:157–164. doi: 10.1542/peds.114.1.157. [DOI] [PubMed] [Google Scholar]
- 4.Sirbaugh PE, Pepe PE, Shook JE, et al. A prospective, population-based study of the demographics, epidemiology, management, and outcome of out-of-hospital pediatric cardiopulmonary arrest. Ann Emerg Med. 1999;33:174–184. doi: 10.1016/s0196-0644(99)70391-4. [DOI] [PubMed] [Google Scholar]
- 5.Engdahl J, Axelsson A, Bang A, Karlson BW, Herlitz J. The epidemiology of cardiac arrest in children and young adults. Resuscitation. 2003;58:131–138. doi: 10.1016/s0300-9572(03)00108-4. [DOI] [PubMed] [Google Scholar]
- 6.Deasy C, Bernard SA, Cameron P, et al. Epidemiology of paediatric out-of-hospital cardiac arrest in Melbourne, Australia. Resuscitation. 2010;81:1095–1100. doi: 10.1016/j.resuscitation.2010.04.029. [DOI] [PubMed] [Google Scholar]
- 7.Donoghue AJ, Nadkarni V, Berg RA, et al. CanAm Pediatric Cardiac Arrest Investigators. Out-of-hospital pediatric cardiac arrest: an epidemiologic review and assessment of current knowledge. Ann Emerg Med. 2005;46:512–522. doi: 10.1016/j.annemergmed.2005.05.028. [DOI] [PubMed] [Google Scholar]
- 8.Herlitz J, Svensson L, Engdahl J, et al. Characteristics of cardiac arrest and resuscitation by age group: an analysis from the Swedish Cardiac Arrest Registry. Am J Emerg Med. 2007;25:1025–1031. doi: 10.1016/j.ajem.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 9.Park CB, Shin SD, Suh GJ, et al. Pediatric out-of-hospital cardiac arrest in Korea: A nationwide population-based study. Resuscitation. 2010;81:512–517. doi: 10.1016/j.resuscitation.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 10.Gerein RB, Osmond MH, Stiell IG, Nesbitt LP, Burns S, Group OS. What are the etiology and epidemiology of out-of-hospital pediatric cardiopulmonary arrest in Ontario, Canada? Acad Emerg Med. 2006;13:653–658. doi: 10.1197/j.aem.2005.12.025. [DOI] [PubMed] [Google Scholar]
- 11.Akahane M, Tanabe S, Ogawa T, et al. Characteristics and outcomes of pediatric out-of-hospital cardiac arrest by scholastic age category. Pediatr Crit Care Med. 2013;14:130–136. doi: 10.1097/PCC.0b013e31827129b3. [DOI] [PubMed] [Google Scholar]
- 12.Meyer L, Stubbs B, Fahrenbruch C, et al. Incidence, causes, and survival trends from cardiovascular-related sudden cardiac arrest in children and young adults 0 to 35 years of age: a 30-year review. Circulation. 2012;126:1363–1372. doi: 10.1161/CIRCULATIONAHA.111.076810. [DOI] [PubMed] [Google Scholar]
- 13.Nitta M, Iwami T, Kitamura T, et al. Age-specific differences in outcomes after out-of-hospital cardiac arrests. Pediatrics. 2011;128:e812–e820. doi: 10.1542/peds.2010-3886. [DOI] [PubMed] [Google Scholar]
- 14.Goto Y, Maeda T, Nakatsu-Goto Y. Decision tree model for predicting long-term outcomes in children with out-of-hospital cardiac arrest: a nationwide, population-based observational study. Crit Care. 2014;18:R133. doi: 10.1186/cc13951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nagata T, Abe T, Noda E, Hasegawa M, Hashizume M, Hagihara A. Factors associated with the clinical outcomes of paediatric out-of-hospital cardiac arrest in Japan. BMJ open. 2014;4:e003481. doi: 10.1136/bmjopen-2013-003481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Maio VJ, Stiell IG, Wells GA, Spaite DW. Optimal defibrillation response intervals for maximum out-of-hospital cardiac arrest survival rates. Ann Emerg Med. 2003;42:242–250. doi: 10.1067/mem.2003.266. [DOI] [PubMed] [Google Scholar]
- 17.Stiell IG, Wells GA, Field B, et al. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med. 2004;351:647–656. doi: 10.1056/NEJMoa040325. [DOI] [PubMed] [Google Scholar]
- 18.Kitamura T, Iwami T, Kawamura T, et al. implementation working group for All-Japan Utstein Registry of the Fire and Disaster Management Agency. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet. 2010;375:1347–1354. doi: 10.1016/S0140-6736(10)60064-5. [DOI] [PubMed] [Google Scholar]
- 19.Kitamura T, Kiyohara K, Nitta M, Nadkarni VM, Berg RA, Iwami T. Survival following witnessed pediatric out-of-hospital cardiac arrests during nights and weekends. Resuscitation. 2014;85:1692–1698. doi: 10.1016/j.resuscitation.2014.08.035. [DOI] [PubMed] [Google Scholar]
- 20.Goto Y, Maeda T, Goto Y. Impact of dispatcher-assisted bystander cardiopulmonary resuscitation on neurological outcomes in children with out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. J Am Heart Assoc. 2014;3:e000499. doi: 10.1161/JAHA.113.000499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Markel DT, Gold LS, Fahrenbruch CE, Eisenberg MS. Prompt advanced life support improves survival from ventricular fibrillation. Prehosp Emerg Care. 2009;13:329–334. doi: 10.1080/10903120802706245. [DOI] [PubMed] [Google Scholar]
- 22.Bakalos G, Mamali M, Komninos C, et al. Advanced life support versus basic life support in the pre-hospital setting: a meta-analysis. Resuscitation. 2011;82:1130–1137. doi: 10.1016/j.resuscitation.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 23.Pitetti R, Glustein JZ, Bhende MS. Prehospital care and outcome of pediatric out-of-hospital cardiac arrest. Prehosp Emerg Care. 2002;6:283–290. doi: 10.1080/10903120290938300. [DOI] [PubMed] [Google Scholar]
- 24.Ma MH, Chiang WC, Ko PC, et al. Outcomes from out-of-hospital cardiac arrest in Metropolitan Taipei: does an advanced life support service make a difference? Resuscitation. 2007;74:461–469. doi: 10.1016/j.resuscitation.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 25.Sunde K, Wik L, Steen PA. Quality of mechanical, manual standard and active compression-decompression CPR on the arrest site and during transport in a manikin model. Resuscitation. 1997;34:235–242. doi: 10.1016/s0300-9572(96)01087-8. [DOI] [PubMed] [Google Scholar]
- 26.Olasveengen TM, Wik L, Steen PA. Quality of cardiopulmonary resuscitation before and during transport in out-of-hospital cardiac arrest. Resuscitation. 2008;76:185–190. doi: 10.1016/j.resuscitation.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 27.Shin SD, Kitamura T, Hwang SS, et al. Seoul-Osaka Resuscitation Study (SORS) Group. Association between resuscitation time interval at the scene and neurological outcome after out-of-hospital cardiac arrest in two Asian cities. Resuscitation. 2014;85:203–210. doi: 10.1016/j.resuscitation.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 28.De Maio VJ, Osmond MH, Stiell IG, Nadkarni V, Berg R, Cabanas JG CanAm Pediatric Study Group. Epidemiology of out-of hospital pediatric cardiac arrest due to trauma. Prehosp Emerg Care. 2012;16:230–236. doi: 10.3109/10903127.2011.640419. [DOI] [PubMed] [Google Scholar]
- 29.Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. JAMA. 2000;283:783–790. doi: 10.1001/jama.283.6.783. [DOI] [PubMed] [Google Scholar]
- 30.Eich C, Roessler M, Nemeth M, Russo SG, Heuer JF, Timmermann A. Characteristics and outcome of prehospital paediatric tracheal intubation attended by anaesthesia-trained emergency physicians. Resuscitation. 2009;80:1371–1377. doi: 10.1016/j.resuscitation.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 31.Wang HE, Simeone SJ, Weaver MD, Callaway CW. Interruptions in cardiopulmonary resuscitation from paramedic endotracheal intubation. Ann Emerg Med. 2009;54:645–652. doi: 10.1016/j.annemergmed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 32.Kramer-Johansen J, Wik L, Steen PA. Advanced cardiac life support before and after tracheal intubation--direct measurements of quality. Resuscitation. 2006;68:61–69. doi: 10.1016/j.resuscitation.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 33.Donovan PJ, Cline DM, Whitley TW, Foster C, Outlaw M. Prehospital care by EMTs and EMT-Is in a rural setting: prolongation of scene times by ALS procedures. Ann Emerg Med. 1989;18:495–500. doi: 10.1016/s0196-0644(89)80831-5. [DOI] [PubMed] [Google Scholar]
- 34.Woodall J, McCarthy M, Johnston T, Tippett V, Bonham R. Impact of advanced cardiac life support-skilled paramedics on survival from out-of-hospital cardiac arrest in a statewide emergency medical service. Emerg Med J. 2007;24:134–138. doi: 10.1136/emj.2005.033365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morrison LJ, Nichol G, Rea TD, et al. ROC Investigators. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008;78:161–169. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pons PT, Haukoos JS, Bludworth W, Cribley T, Pons KA, Markovchick VJ. Paramedic response time: does it affect patient survival? Acad Emerg Med. 2005;12:594–600. doi: 10.1197/j.aem.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 37.Eisenberg MS, Bergner L, Hallstrom A. Cardiac resuscitation in the community. Importance of rapid provision and implications for program planning. JAMA. 1979;241:1905–1907. doi: 10.1001/jama.241.18.1905. [DOI] [PubMed] [Google Scholar]
- 38.Babl FE, Vinci RJ, Bauchner H, Mottley L. Pediatric pre-hospital advanced life support care in an urban setting. Pediatr Emer Care. 2001;17:5–9. doi: 10.1097/00006565-200102000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Doherty DR, Parshuram CS, Gaboury I, et al. on behalf of the Canadian Critical Care Trials Group. Hypothermia therapy after pediatric cardiac arrest. Circulation. 2009;119:1492–1500. doi: 10.1161/CIRCULATIONAHA.108.791384. [DOI] [PubMed] [Google Scholar]
- 40.Schindler MB, Bohn D, Cox PN, et al. Outcome of out-of-hospital cardiac or respiratory arrest in children. N Engl J Med. 1996;335:1473–1479. doi: 10.1056/NEJM199611143352001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.