Abstract
Background
Expectations continue to rise for residency programs to provide integrated simulation training to address clinical competence. How to implement such training sustainably remains a challenge. We developed a compact module for first-year surgery residents integrating theory with practice in high-fidelity simulations, in order to reinforce the preparedness and confidence of junior residents in their ability to manage common emergent patient care scenarios in trauma and critical care surgery.
Methods
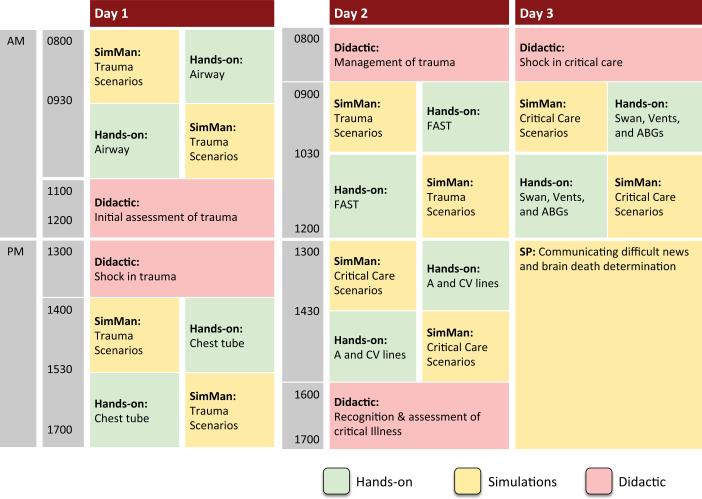
The three-day module features a combination of simulated patient encounters using standardized patients and electronic manikins, didactic sessions, and hands-on training. Manikin-based scenarios developed in-house were used to teach trauma and critical care management concepts and skills. Separate scenarios in collaboration with the regional organ donation program addressed communication in difficult situations such as brain death. Didactic material based on contemporary evidence, as well as skills stations were developed to complement the scenarios. Residents were surveyed before and after training on their confidence in meeting the fourteen learning objectives of the curriculum on a 5-point Likert scale.
Results
Data from 15 residents that underwent this training shows an overall improvement in confidence across all learning objectives defined for the module, with confidence scores pre to post-training improving significantly from 2.8 (σ=0.85, median 3) to 3.9 (σ=0.87, median 4) out of 5, p<0.001. While female residents reported higher post-training confidence scores compared to male residents (average 4.2 female vs 3.8 male, p=0.002), there were no other significant differences in confidence scores or changes to scores due to resident gender or program status (categorical or preliminary).
Conclusion
We successfully implemented a multimodal simulation-based curriculum that provides skills training integrated with the clinical context of managing trauma and critical care patients, simultaneously addressing a range of clinical competencies. Results to date show consistent improvement in residents’ confidence in meeting learning objectives. Development of the curriculum continues for sustainability, as well as measures to embed objective evaluations of resident competence.
Keywords: Simulation, surgery, education, residency, standardized patient
Background
Graduate medical education and training has traditionally relied heavily on experiential learning from patient encounters as part of clinical practice and service. Contemporary patient safety and ethical imperatives firmly focus on protecting the patient, in effect forbidding learning through trial and error on real patients. Simulated encounters can provide integrated training without risk to patients, and simulation-based education for trauma and surgical critical care has evolved rapidly with many available modalities, as well as emerging methods for assessment1. Use of patient simulation has become a mainstay in trauma education through the Advanced Trauma Life Support (ATLS®) course, which the American Board of Surgery has required for applications for General Surgery Certification in the 2009-2010 academic year or thereafter2. Our institution has also integrated patient simulation into the Fundamental Critical Care Support (FCCS) course promoted by the Society for Critical Care Medicine3.
Education is a particularly pressing issue in fields like trauma and surgical critical care, where the volume of clinical experience is limited to a small number of patient encounters in select institutions. Exposure to immediately life-threatening time-critical trauma is uncommon, yet even entry-level providers are expected to be competent every time they are called upon to manage such patients4. Despite this, the specifics of organizing such curricula, best practices and strategies for integrating simulation, as well as suggestions for sustainability have yet to be established and are left to individual institutions. Training programs today face complex issues such as duty hour standards, combined with ever-increasing demand to staff clinical services4. This creates significant tension between the need to provide accountable education, and the need to safely render health care services and maintain the institution's bottom line.
As part of an effort to accelerate competence of general surgery residents, we describe the design, implementation, and results from the first year of a modular simulation curriculum for Trauma and Surgical Critical Care. Our approach balances the need to provide targeted education for residents while being cognizant of the perceived opportunity cost to the health system of sequestering frontline providers – both residents and faculty – for dedicated educational programs.
Methods
Protection of Human Subjects
This research was conducted within the residency program in general surgery at the Hospital of the University of Pennsylvania. We submitted our protocol to the Institutional Review Board and received confirmation of exemption under 45 CFR 46.101, category 1 for human subjects research regarding the effectiveness of instructional curricula in established educational settings. Furthermore, written consent was sought from all participating first-year residents regarding the video recording and collection of data regarding their educational experience and simulated clinical performance for the purpose of research and publication, with the understanding that their consent or refusal would not have any impact on the provided educational content or their standing as a resident in the program.
Scheduling of Residents
Finding a balance between service and training is a recurring issue in contemporary graduate medical education. The reality of any clinical training program is that trainees are also essential to the staffing of clinical services, meaning only a limited number at a time may be assigned to non-clinical duties. Furthermore, participation in this simulation-based curriculum is not considered ‘time free of duty’ – it is an educational assignment integral to the residency program and is subject to duty hour regulations5.
Our simulation curriculum was implemented in a modular manner, where residents are scheduled for blocks of three weekdays, distributed throughout the year. This modular implementation accommodates residents in small groups to minimize staffing disruptions. Other residents, physician assistants, and non-physician practitioners on the team cover resident duties while they take part in simulation education. These compact three-day modules can be repeated over the course of the year to ensure the entire resident class, categorical and preliminary residents alike, are given equal access to this educational opportunity.
The three iterations of the module occurred in September (n=6), February (n=5), and April (n=4), with resident assignments based purely on the logistics of drafting them from clinical service rotations. The possibility of ‘just in time’ training synchronized with clinical rotations was considered, but was incompatible with clinical service demands. This resulted in a pseudorandom crossover of residents’ level of clinical exposure to Trauma and Critical Care experiences. For example, some participating residents had yet to rotate through Trauma, while others had already done so earlier in the year, and some were currently on their Trauma rotation.
The Module
Trauma and critical care surgery was selected as one of six surgical specialty areas in which first-year residents would benefit most from simulation-based training (the others being acute care, biliary, cardiovascular, colorectal, and foregut). The surgery simulation program director (RA) consulted with faculty in the Division of Traumatology, Surgical Critical Care and Emergency Surgery (NDM and JLP) to outline learning objectives for the module.
Established national programs served as a starting point for the selection of level-appropriate curricular content. For the Trauma aspect of the module, the ATLS® program6 and course objectives, as well as the PGY-1 level Trauma content from the SCORE (Surgical Council on Resident Education) Portal7 were referenced. For Surgical Critical Care, the Society of Critical Care Medicine's Fundamental Critical Care Support (FCCS) course objectives and topics3, as well as the relevant SCORE Portal content at the PGY-1 level were referenced. Topics were selected based on perceived importance and relevance to trainees’ practice at our institution. Table 1 shows the primary source of course objectives and topics selected for inclusion in the curriculum. Priority was given to reinforce topics and skills that are expected to be a routine part of the residents’ immediate practice. For example, determining and arranging for interhospital transfer is a prominent objective in ATLS as well as FCCS. While these skills may well be required later in the one's career as surgeons, they are of less immediate relevance to residents at our institution, which is a Level I Trauma Center. Instead, particular focus was given to performing initial assessments, as well as management of shock – hemorrhagic and septic – which are both quite commonly encountered by residents.
Table 1.
Basis for selection of module content
| Session | SCORE | ATLS | FCCS |
|---|---|---|---|
| Initial assessment of trauma | ✓ | ✓ | |
| Management of trauma | ✓ | ✓ | |
| Recognition of critical illness | ✓ | ✓ | |
| Shock in Trauma (Hypovolemic shock) | ✓ | ✓ | |
| Shock in Critical Care (Septic shock) | ✓ | ✓ | |
| Skill: Endotracheal Intubation | ✓ | ✓ | |
| Skill: Thoracostomy | ✓ | ✓ | |
| Skill: FAST (Focused Assessment with Sonography in Trauma) | ✓ | ✓ | |
| Skill: Arterial lines | ✓ | ||
| Skill: Central lines | ✓ | ||
| Communication | ✓ |
Subsequently, the surgery simulation fellow (KWM) constructed a three-day sequence of sessions to deliver training in a realistic clinical context while taking into account real-world logistical constraints such as the availability of space, equipment, instructors, and other resources.
The three-day module features a combination of simulated patient encounters using electronic manikins and standardized patients, as well as hands-on skills training and didactic sessions. Didactic material was developed to be consistent with the latest national curricula and guidelines. Five trauma and five critical care clinical scenarios were selected, from a library of scenarios developed in-house8 for the SimMan® 3G patient simulator to teach trauma and critical care management concepts and skills (Table 2). Hands-on skills stations were developed to complement the skills required within the scenarios, and included topics such as endotracheal intubation, thoracostomy, focused assessment with sonography for trauma (FAST), arterial line placement and blood gas interpretation, as well as the placement of central venous and pulmonary artery catheters.
Table 2.
Summary of Simulated Scenarios
| Scenario # | Trauma Scenarios | Critical Care Scenarios |
|---|---|---|
| 1 | 43M, multiple gunshot wounds in drive-by shooting | 40M, rapid response team call for respiratory distress following central line placement |
| 2 | 42M, fall from 15 ft on hard dirt | 42F, rapid response team call for acute change in mental status (History: Renal transplant) |
| 3 | 48M, motor vehicle collision with rollover, restrained driver, no airbag with loss of consciousness | 32M, hypotension and hypoxia, splenectomy post-operative day 2 in surgical intensive care unit |
| 4 | 24F, stabbed in neck with screwdriver | 45M, decreased responsiveness in surgical intensive care unit |
| 5 | 35F, assault to torso, head, neck, extremities by multiple assailants | 70F, shortness of breath and chest pain, tib-fib and femoral neck fracture, post-operative day 8 in surgical intensive care unit after open reduction and internal fixation |
Formal training in end-of-life care, not explicitly part of any of the aforementioned curricula, has been noted as a national concern9. Our institution has one of the largest organ transplantation programs in the country, and training of residents to address brain death and other grave prognoses was identified as an area of educational value.
The regional organ donation program volunteered their services to address communication in difficult situations such as brain death. The Gift of Life Donor Program is the nonprofit organization responsible for coordinating the organ and tissue donation and transplant processes in Pennsylvania, New Jersey and Delaware10. As part of their outreach, the organization provides educational resources not only to the public, but to area hospitals as well. Transplant coordinators from the organization gave an introduction to their services, and discussed the resident's role in explaining prognoses such as brain death. They also acted as family members of patients for a series of simulated scenarios. Residents were given the task of explaining a patient's death to the family member, respectfully addressing some of the common misconceptions that arise surrounding brain death.
The final module sought to address the 14 listed learning objectives (Table 3) thought to be most important and relevant to first-year surgery residents at our institution.
Table 3.
Resident confidence in achieving learning objectives
| Learning Objective | Day 1 Mean (Median) | Day 3 Mean (Median) | p-value | |
|---|---|---|---|---|
| 1 | Ability to rapidly and accurately assess a critically ill/injured patient | 3.1 (3) | 4.1 (4) | 0.0011 |
| 2 | Ability to resuscitate and stabilize the patient according to priorities | 3.1 (3) | 4.2 (4) | 0.0006 |
| 3 | Ability to accurately utilize fluid management strategies | 3.1 (3) | 4.3 (4) | 0.0015 |
| 4 | Ability to recognize surgical diseases and complications in a timely manner | 3.3 (3) | 4.1 (4) | 0.0011 |
| 5 | Ability to recognize the need for bedside procedures in the intensive care unit | 3.0 (3) | 4.1 (4) | 0.0009 |
| 6 | Ability to safely perform bedside procedures in the intensive care unit | 2.7 (3) | 3.7 (4) | 0.0014 |
| 7 | Ability to communicate in ethically challenging end-of-life situations | 2.7 (3) | 4.1 (4) | 0.0038 |
| 8 | Technical skills for endotracheal intubation and surgical airway access | 2.5 (3) | 3.6 (4) | 0.0089 |
| 9 | Technical skills for thoracostomy and chest tube placement | 2.6 (3) | 3.6 (4) | 0.0036 |
| 10 | Knowledge of arterial blood gas analysis and interpretation | 3.6 (4) | 4.4 (4) | 0.0054 |
| 11 | Knowledge and technical skills of mechanical ventilation | 2.4 (2) | 3.6 (4) | 0.0087 |
| 12 | Technical skills for pulmonary artery catheter placement | 1.6 (1.5) | 2.7 (3) | 0.0095 |
| 13 | Technical skills for peripheral arterial catheter placement | 2.9 (3) | 3.8 (4) | 0.0094 |
| 14 | Technical skills for central venous catheter placement | 3.0 (3) | 3.7 (4) | 0.0101 |
| Pooled responses for objectives 1-14 | 2.8 (3) | 3.9 (4) | 0.0000 |
Scheduling of Teaching Faculty
One faculty member from the Division of Traumatology, Surgical Critical Care, and Emergency Surgery was assigned to each day of the module, with the assignments listed and enforced as part of the division's schedule. The simulation center staff educator and technicians familiar with the electronic manikin technology and scenarios were retained to run the simulated encounters. The simulation fellow (KM), research student (JB) as well as a volunteer faculty instructor (an intensivist on medical leave) were responsible for delivering the concurrent hands-on sessions.
Evaluation of the Module
Residents were surveyed before and after training on their confidence in meeting the fourteen learning objectives of the curriculum on a 5-point Likert scale. Responses were collected and entered into STATA (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP.) for statistical analysis.
Results
A total of 15 first-year residents completed the curriculum. Residents consisted of all seven categorical residents and eight preliminary general surgery residents, as well as one first-year urology resident training in the general surgery program. Overall results showed an improvement in confidence across all learning objectives defined for the module, with confidence scores pre to post-training improving significantly from 2.8 (σ=0.85, median 3) to 3.9 (σ=0.87, median 4) out of 5, p<0.01 using the Wilcoxon matched-pairs signed-rank test. Breakdowns of each individual learning objective also showed a significant (p<0.01) increase in confidence level.
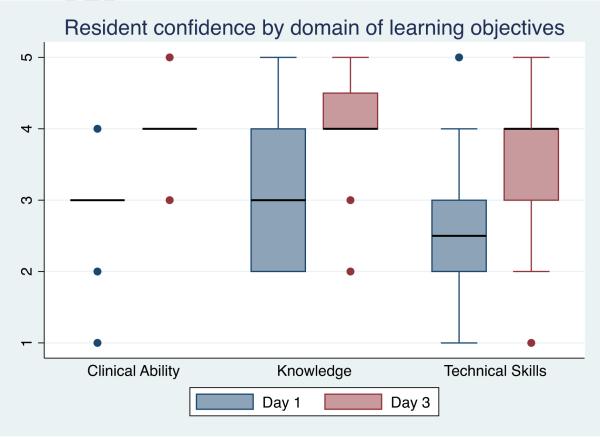
Learning objectives designated three domains - clinical ability (#1-7), knowledge (#10, 11), and technical skills (#8, 9 and 12-14). Average confidence in meeting learning objectives concerning clinical ability improved from 3.0 to 4.1, a 1.1-point (p<0.01) increase. Confidence in meeting learning objectives for knowledge improved from 3.0 to 4.0 (p<0.01), similar to technical skill, which improved 1.1 points from 2.5 to 3.5 (p<0.01). Pre-training residents reported lower confidence scores for technical skills compared to clinical ability (p<0.01). While confidence increased significantly in all three domains, post-training confidence in technical skills remained lower than that for knowledge (p<0.05). Trends for resident confidence by domain are shown in Figure 2.
Figure 2.
Resident pre- and post-training confidence in meeting the 14 defined learning objectives is shown grouped by domain: Clinical Ability (7), Knowledge (2), and Technical Skills (5).
Residents and faculty attended all modules and sessions within 30 minutes of the scheduled times. There was a deviation during one of the module iterations, which resulted in cancellation of one of the hands-on sessions due to heavy snowfall restricting access to the simulation center. The impact can be seen in the form of outliers in post-training confidence scores for technical skills. There were no discernible differences in levels of resident confidence between the three module iterations occurring at different times of the year. Resident gender (female, male) or program status (categorical, preliminary) did not significantly affect baseline confidence scores or changes in confidence, though female residents reported higher post-training confidence scores (average 3.8 male vs 4.2 female, p<0.01.
Costs
The direct cost associated with each three-day event was estimated at $14,800, or an average cost of $2,960 per resident trained. The charge for exclusive use of simulation center facilities, stock supplies, and support staff for the duration of each module was the greatest expense at approximately $10,000, billed internally from institutional education funds. The value associated with faculty teaching time was second at an estimated at $4,800 based on a rate of $200.00 per hour. Faculty compensation occurred via an internal relative value unit system. The above estimate does not include indirect costs such as capital expenditures for simulation facilities, overhead for employment outside these three-day blocks, and the initial curriculum development effort invested by various stakeholders.
Discussion
Simulation education for surgical trainees has tended to focus on specific skills in isolation, with particular focus on operative skills. While technical skill is a desirable characteristic of surgeons at any level, first-year trainees are generally not expected to be proficient independent operators. Conversely, interns are routinely entrusted with the medical management of patients on surgical wards and are expected to provide appropriate vigilance in the perioperative period with minimal supervision. They are also expected to perform various diagnostic and therapeutic procedures at the bedside, and may be called upon in an emergency to perform life-saving interventions such as establishing a surgical airway. The prioritization of life-saving surgical interventions that is a central concept in trauma care, as well as the systematic approach to identifying and assessing critically ill patients that is fundamental to critical care, are aligned closely with the safe execution of duties expected of first-year trainees.
Trauma education was an early adopter of simulation methodologies, with national curricula (such as ATLS®) that incorporate simulated patient encounters as part of an introduction to a systematic, team-based approach to the trauma patient. Simulation has also taken root in critical care and other related specialties that train providers to respond as teams to patient needs and perform tasks such as resuscitation in line with the latest evidence-based protocols in various care environments. High-fidelity manikin-based simulations in particular are conducive to trauma and critical care training, as they can recreate rapid simultaneous changes in multiple physiologic parameters as are seen in these environments8.
Simulation is also useful for the cultivation of non-technical skills such as communication. While residents communicate with patients and families daily, they are rarely the ones to break bad news in difficult end of life situations. Residents may also be limited in opportunities to observe experienced providers communicate in such situations. Poor quality of end-of-life discussions is a frequent cause of patient/family complaints, and junior providers often feel inadequately prepared for these conversations due to lack of training11. In a questionnaire asking participating residents to rate each session, “Explaining Brain Death” was one of the highest rated sessions, with an average rating of 4.8/5, along with qualitative feedback indicating it was perceived as a positive learning experience. We suggest that teaching hospitals reach out to their regional organ procurement organization for their expertise in developing this specific set of communication skills, as well as experience in putting them to practice professionally.
Caveats and Limitations
Metrics of resident performance by faculty are notably and admittedly absent. We observed a significant increase in residents’ perception of their own performance, which reflects a high degree of satisfaction with their educational experience. However, in terms of sophistication as a training program, assessment of learner satisfaction is at the lowest level in the well-established Kirkpatrick framework, and objective measures of performance are required to establish a more robust curriculum12. A variety of tools exist for the direct observation and assessment of the clinical skills of trainees13. Global rating scales and checklists with some validity evidence exist to quantify team-based crisis management skills14, but there is an inherent difficulty in assessing and tracking changes in an individual resident's level of competence when performing as part of a team. This measurement is further confounded when a faculty instructor is present to prompt the resident team to perform critical tasks.
In a previous research study of a half-day simulation-based training course for advanced practitioners at our institution, three dedicated expert assessors scored all pre- and post-training encounters using assessment tools adapted for each specific scenario which demonstrated improvements in domains such as confidence, teamwork, decision making, and situational awareness8. From the perspective of a residency program, allocation of attending faculty time (valued internally at $200 per hour) for resident assessment must be done judiciously. Given the severe demand on resident and faculty time, as well as the broad range of topics to be covered, formative sessions were prioritized over repetition of identical sessions purely for the purpose of summative evaluation of each individual resident. Instead, participating residents took part in the simulated encounters as teams, with faculty present in the room providing prompting and commentary on the evolving clinical situation.
Important next steps will be to identify an acceptable method to regularly conduct evaluations of resident performance during these simulated clinical encounters, or to pursue methods for team-based assessments. The same measurement tools would then need to be implemented in the clinical realm to seek translational effects of training into actual outcomes. A balance will need to be struck between time spent on teaching and time spent on assessment, in order to make maximal use of a limited number of teaching hours while still maintaining curricular accountability and research output.
Conclusion
We successfully implemented an integrated trauma and surgical critical care simulation curriculum for general surgery residents. Our implementation begins to address contemporary societal expectations regarding residency education, while balancing the stringent clinical service demands on residents. The three-day module template was implemented for other topics in surgery, and the structure should be broadly adaptable to other surgical or medical specialties. We invite programs seeking a practical implementation of simulation-based education within their residencies to consider our modular curriculum design.
One of the keys to the success launch of this curriculum was the structure and oversight provided by the simulation program director and a full-time simulation fellow. Administrative arrangements were made in advance for the scheduling of faculty and residents to participate, and coverage of residents’ clinical duties. The presence of an education fellow minimized burden on faculty such that teaching was turnkey - standardized teaching materials such as slide decks were available for all didactic sessions, as well as having all necessary teaching materials and equipment such as simulators set up and ready for use at the simulation center.
Objective assessment of competence and validation remain ongoing challenges to our curriculum, and simulation education in general. Ultimately we were unable to provide a framework for ongoing objective assessment and validation of the curriculum beyond resident confidence and subjective feedback. Despite these limitations, we were able to deliver a practical, tailored simulation-based training intervention that helped residents feel better prepared to be effective members of the trauma and surgical critical care services at our institution.
Figure 1.
The three-day module schedule consists of a combination of didactic, hands-on, and simulation sessions. Sessions can be split to run concurrently, accommodating residents in smaller groups.
Acknowledgements
The authors wish to acknowledge the staff at the Penn Medicine Clinical Simulation Center for their continuing support of this curriculum. We thank Dr. Jennifer Snow for volunteering her time and expertise for the hands-on sessions, and Dr. Daniel Holena for coordinating the faculty schedule for the division of Traumatology, Surgical Critical Care, and Emergency Surgery. Special thanks to the Division of Surgery Education and the Surgery Residents’ Council chairs for making it possible to integrate this educational initiative as part of the general surgery residency program, as well as all the residents who participated.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contribution
KWM wrote the manuscript, and contributed to the study planning and all subsequent phases.
NM and JLP contributed to the study planning as well as critical review.
JB contributed to the study planning and statistical analysis.
RA conceived the study concept and contributed to all subsequent phases of the study including critical review.
Disclosures
Kiyoyuki Miyasaka was funded by NIH CTSA grant No. 5 KL2 TR 139-8.
Rajesh Aggarwal is a consultant for Applied Medical.
References
- 1.Berkenstadt H, Ben-Menachem E, Simon D, Ziv A. Training in Trauma Management: The Role of Simulaion-Based Medical Education. Anesthesiology Clin. 2013;31:167–177. doi: 10.1016/j.anclin.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 2.American Board of Surgery [November 4, 2014];ABS to Require ACLS, ATLS and FLS for General Surgery Certification. http://www.absurgery.org/default.jsp?news_newreqs Updated August 15, 2008.
- 3.Society of Critical Care Medicine [September 18, 2014];Fundamental Critical Care Support Course (FCCS) web site. http://www.learnicu.org/Fundamentals/Pages/FCCS.aspx.
- 4.Editorial Simulation in trauma education: Beyond ATLS. Injury, Int J. Care Injured. 2014;45:817–818. doi: 10.1016/j.injury.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education [November 4, 2014];Common Program Requirements. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/CPRs2013.pdf.
- 6.American College of Surgeons Committee on Trauma . Advanced Trauma Life Support® Student Course Manual. Ninth Edition. American College of Surgeons; Chicago, IL: 2012. [Google Scholar]
- 7.SCORE General Surgery Resident Curriculum Portal. ( http://www.surgicalcore.org)
- 8.Pascual JL, Holena DN, Vella MA, Palmieri J, Sicoutris C, Selvan B, Fox AD, Sarani B, Sims C, Williams NN, Schwab CW. Short simulation training improves objective skills in established advanced practitioners managing emergencies on the ward and surgical intensive care unit. J Trauma. 2011;71:330–338. doi: 10.1097/TA.0b013e31821f4721. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan AM, Lakoma MD, Block SD. The status of medical education in end-of-life care: a national report. J Gen Intern Med. 2003 Sep;18(9):685–95. doi: 10.1046/j.1525-1497.2003.21215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. [November 4, 2014];Gift of Life Donor Program. http://www.donors1.org.
- 11.Clayton JM, Butow PN, Waters A, Laidsaar-Powell RC, O'Brien A, Boyle F, Back AL, Arnold RM, Tulsky JA, Tattersall MH. Evaluation of a novel individualized communication-skills training intervention to improve doctors’ confidence and skills in end-of-life communication. Palliat Med. 2013;27(3):236–243. doi: 10.1177/0269216312449683. [DOI] [PubMed] [Google Scholar]
- 12.Doumouras AG, Keshet I, Nathens AB, Ahmed N, Hicks CM. A crisis of faith? A review of simulation in teaching team-based, crisis management skills to surgical trainees. J Surg Educ. May-Jun. 2012;69(3):274–81. doi: 10.1016/j.jsurg.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Kogan JR, Holmboe ES, Hauer KE. Tools for direct observation and assessment of clinical skills of medical trainees: a systematic review. JAMA. 2009;302(12):1316–26. doi: 10.1001/jama.2009.1365. [DOI] [PubMed] [Google Scholar]
- 14.Kim J, Neilipovitz D, Cardinal P, Chiu M. A comparison of global rating scale and checklist scores in the validation of an evaluation tool to assess performance in the resuscitation of critically ill patients during simulated emergencies. Simul Healthc. 2009 Spring;4(1):6–16. doi: 10.1097/SIH.0b013e3181880472. [DOI] [PubMed] [Google Scholar]