Abstract
Background
Older adults often experience impaired mobility, lower extremity muscle weakness, and increased fall risk. Furthermore, when older adults perform tasks that require control of submaximal force, impairments in their ability to maintain steady and accurate force output has been reported. Such problems may be related to deteriorating levels of mobility, particularly in older adults who have fallen.
Purpose
The purpose of this study was to determine whether an association exists between muscle force steadiness (MFS) or muscle force accuracy (MFA) of the knee extensors and mobility in older adults who have fallen.
Methods
Twenty older adults (x̄ = 77.5 ± 7yrs, 5 males and 15 females) with 2 or more co-morbid conditions and who experienced a fall in the past year underwent assessment of maximal voluntary isometric contraction (MVIC) of the knee extensors. A submaximal target force of 50% of their MVIC was used to determine concentric (CON) and eccentric (ECC) steadiness (the fluctuations in force production) and accuracy (the average distance of the mean force from the target force) measures. Mobility was indicated by the 6 minute walk test (6MWT), the timed up and go (TUG), stair ascent (StA), and stair descent (StD) tests. Correlation analysis was used to assess the relation between measures of muscle force control and mobility.
Results
The correlations between MFS and mobility were not significant (p>0.05) for either contraction type. However, MFA during ECC contractions only, were correlated significantly with all measures of mobility: 6MWT (r=−0.48, p=0.03), TUG (r=0.68, p=0.01), StA (r=0.60, p=0.01), StD (r=0.75, p<0.01).
Conclusion
The identification of the relationship between ECC MFA and mobility in older adults who have fallen is novel. While the correlations are not causal, these relationships suggest inaccurate force output during ECC contractions of the knee extensors is linked to impaired mobility.
Keywords: Aging, concentric, eccentric, mobility, steadiness
INTRODUCTION
Older adults often experience muscle dysfunction and mobility challenges that place them at an increased risk for falling.1–5 Further, the ability of older adults to perform mobility tasks such as walking, stair negotiation, or rising from a chair may require increased effort compared with young adults and could result in an accident.6 Specifically, a fall can occur when negotiating stairs, with more incidents occurring during stair descent.7 In addition to maximal force production, submaximal muscle function has also been suggested as a potential contributor to fall risk.8 It is not clear, however, if the ability to control submaximal force is directly linked to performance on mobility tasks in older adults who have fallen.
The force produced during a muscle contraction fluctuates around an average value.3,9–12 The amplitude of force fluctuations can provide information about the ability of the nervous system to regulate force output. The force fluctuations during submaximal muscle contractions, or variability in motor output, is increased for older compared with young adults and is often characterized as muscle force steadiness (MFS).9,13–16 Further, increased force variability may adversely impact movement precision depending on the type of muscle contraction or age of the individual.3,9,17–20
In addition to MFS, muscle force accuracy (MFA), which measures the ability of an individual to achieve a target force for a period of time, has also been utilized to assess the control of submaximal force output.15 Although data on MFA are limited and less frequently reported compared with MFS, MFA has been found to be impaired in older adults during relatively slow contractions and rapid, discrete contractions.15,20–22 It is not known whether MFA is associated with decreased mobility in older adults who have fallen. It may seem intuitive that increased variability in motor output, characterized as MFS and MFA, may be associated with decreased mobility in older adults who have fallen. However, to our knowledge no evidence has been reported in this older adult population.
The purpose of this single group correlational study was to determine the association between concentric and eccentric submaximal motor control of the knee extensors and the performance of mobility tasks in older adults who had fallen. We postulated a link between mobility and MFS and MFA during concentric (CON) and eccentric (ECC) knee extensor contractions.
METHODS
Twenty older adults volunteered to participate in a 1 day experimental session lasting approximately 2.5h. The participants (see Table 1) included adults ≥65 years of age who experienced at least 1 fall in the past year, were able to ambulate within the community with or without an assistive device and were managing 2 or more co-morbid medical conditions. A fall was defined as having experienced an event resulting in an unexpected contact or resting position with the ground or floor for medically unexplained reasons. Exclusion criteria included progressive neurologic disorders, cancer treatment, chronic heart failure or unstable medical conditions. Participants were recruited from the Salt Lake City community. Participants provided signed confirmation of their informed consent. The Institutional Review Board at the University of Utah approved the procedures used in this study.
Table 1.
Participant characteristics of older impaired adults who had fallen
| Participant Characteristics |
Mean ± SD |
|---|---|
| Age (y) | 77.5 ± 7 |
| Height (cm) | 166.4 ± 9 |
| Weight (kg) | 69.5 ± 16 |
| BMI (Kg/M2) | 25.14 ± 6 |
| MVIC (N) | 272 ± 68 |
| Number of Falls | 1.35 ± 0.67 |
| Co-Morbidities | 4.21 ± 2.62 |
Abbreviations: (y) = Years, (cm) = Centimeters, (kg) = Kilograms, BMI = Body Mass Index, (Kg/M2) = Kilogram/meter2 ratio, MVIC = Maximal Voluntary Isometric Contraction
Knee Extension Maximal Muscle Torque Measurements
Participants performed maximal voluntary isometric contractions (MVIC) of the knee extensor muscles at a joint angle of 45 degrees of knee flexion on a KinCom dynamometer (KinCom 500H, Chattecx Corp; Harrison, TN). The center of the knee joint was aligned with the axis of the dynamometer, the mid-thigh was secured with a strap, and the distal lower leg was secured to the lever arm with a velcro strap. Prior to testing, participants performed 3 warm up submaximal contractions, 1 at 50% and 2 at 75% of their perceived maximal effort. Following a rest period of 1 to 3 minutes, participants performed 3 maximal isometric contractions by pushing as forcefully as possible for 3 seconds with strong verbal encouragement. One minute of rest was given between each trial. The maximal peak torque of the 3 trials, with a difference no greater than 5% between trials, was used as the MVIC. A 4th trial was performed if the aforementioned criteria were not met. Following MVIC testing and prior to measuring MFS, participants were given 10 minutes of rest.
Muscle Force Steadiness and Muscle Force Accuracy
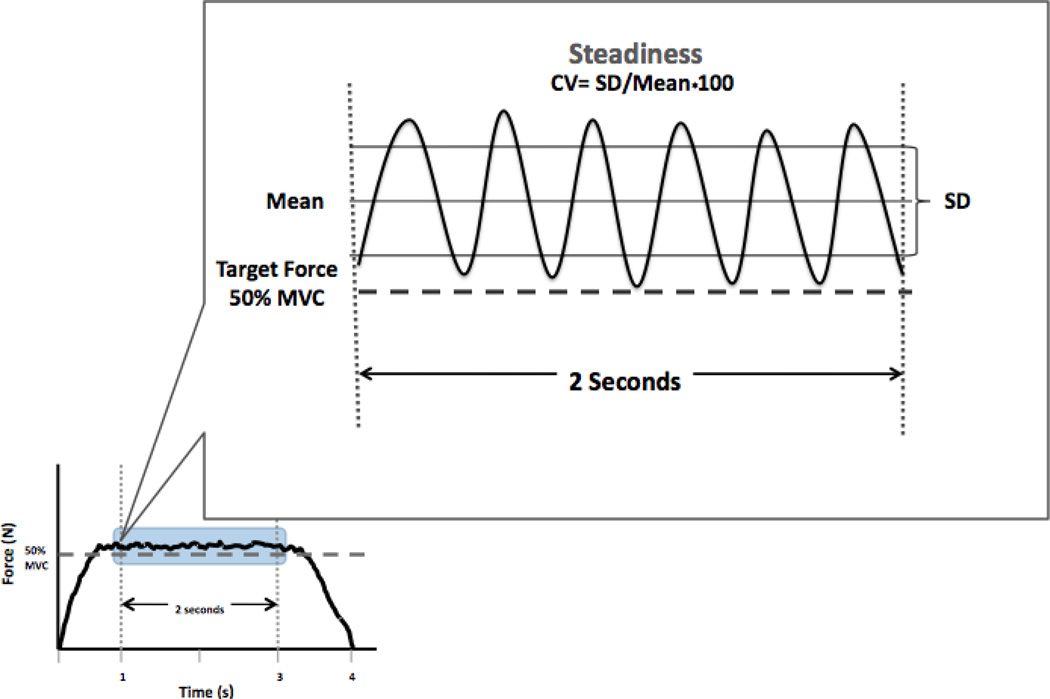
MFS was measured by having the participants perform submaximal CON and ECC contractions of the knee extensors while attempting to match a target force line of 50% of their MVIC. Using a KinCom dynamometer (KinCom 500H, Chattecx Corp; Harrison, TN) set at a speed of 15 deg•sec−1, data were collected between 75-15 degrees of knee extension. The monitor was positioned approximately 1 meter in front of the subject. Participants were instructed to perform a smooth, steady contraction while attempting to match the target force line. Participants initially performed 2 familiarization trials followed by a series of test trial sequences (TTS), with each series containing 3 trials per TTS for a total of 30 trials. Each trial lasted 8 seconds in duration, the first 4 seconds consisting of a CON contraction immediately followed by a 4 second ECC contraction of the knee extensor muscles. Participants were given a 1 minute rest period between each test trial and a 3 to 5 minute rest period between each series of 3 trials. The first 6 TTS (a total of 18 trials) were not included in the data analysis as they were considered practice trials to ensure that participants understood the task, and to avoid the potential contribution of early motor learning effects reported by others.15,23 MFS and MFA measures were collected on the weaker leg, as determined by the MVIC force. MFS was characterized by the coefficient of variation (CV= standard deviation (SD)/mean•100), an accepted method for quantifying normalized force variability.3,24 MFA was defined as the difference between the average force produced and the submaximal target force (Figure 1).
Figure 1. Example of muscle force steadiness and muscle force accuracy measures.
The force trace represents a muscle force steadiness (MFS) trial over a four second time interval recorded during a muscle contraction (either concentric or eccentric). Muscle force accuracy (MFA) was also recorded as the force output relative to a target force set as 50% of the subject’s maximal voluntary isometric contraction (MVIC). The middle 2 second interval (enlarged) was used to calculate MFS expressed as CV of force, and MFA.
Mobility Testing
Standardized tests of mobility were used including the 6 minute walk test (6MWT), the timed up and go test (TUG), and the stair test (stair ascent = StA and stair descent = StD). These tests have been reported to be reliable (ICC range 0.90–0.96) in older adults.5,25–28
Six Minute Walk Test
The 6MWT test measures the total distance an individual can walk in 6 minutes and assesses their walking ability, a functional component of activities of daily living.29 Participants were instructed to walk as far as they possibly could in 6 minutes around a rectangular course 89.45 meters (m) in length and the total distance walked was recorded for data analysis. The 6MWT has been shown to have a high test re-test reliability.27
Timed Up and Go Test
The TUG test has been used to measure mobility and been shown to be related to increased fall risks in older adults.5,30 Participants started in a seated position with their backs against the backrest of a chair (43 cm seat height). They were instructed to rise from the chair as quickly and safely as they could, walk a distance of 3 meters, turn around a cone, and walk back to the chair and to sit back down. Timing commenced once movement occurred and ceased when participants returned to the starting position with their backs against the backrest of the chair.30 Participants were given 1 practice trial, followed by 3 test trials, with at least a 1 minute rest period between trials. The mean of 3 trials was used for data analysis.
Stair Test
The StA and StD tests were administered by having participants positioned at the base of a well-lit 10-step (17.15 cm steps) staircase with handrails. Under close supervision, participants were instructed to safely ascend and descend the stairs as quickly as possible. Timing commenced once movement occurred and stopped when both feet reached the top or bottom step.31 Participants were given 1 to 3 minutes rest between trials. The mean of 3 trials were used for data analysis. The validity of these test measures have been reported previously.28
Data Processing
The torque signal from the dynamometer was analog-to-digital converted at 1000 samples/s (DAQ-National Instruments) and low-pass filtered (20th order Butterworth) at 100 Hz. The middle 2 seconds from each 4 second force trace was used to measure MFS to avoid the ramping up and down of force production. After linear detrending of the middle 2s, mean torque, SD of torque, and CV of torque were calculated using Matlab software (Mathworks, Inc.; Natlick, MA, Matlab 2009).32 MFS test trials where the mean torque produced was within ± 20% of the target force were included as part of the data analysis. MFA was expressed as a percentage of the target force (%TF). The mean force produced was divided by the target force and multiplied by 100 ([mean force* target force−1]*100). A value of 100%TF signified a mean force equal to the target force. Values for MFA %TF above or below 100% indicated overshoot or undershoot of the mean force relative to the target force.
Statistical Analysis
In order to determine whether an association was present between MFS, MFA, and mobility tasks, Pearson product moment correlation coefficients were utilized to evaluate the bivariate relationships. The statistical significance level was set at p<0.05. Data analysis was performed using SPSS version 20 (IBM SPSS Inc, Armonk, NY).
RESULTS
All twenty participants completed the study. Demographic characteristics expressed as group means and standard deviation (SD) for age, height, weight, BMI, MVIC, number of falls and number of co-morbidites were included in Table 1. There was a greater proportion of females (n=15) compared to males (n=5). Participants appeared to be typical of older community dwelling adults for age, gender, height and weight as observed by others.33–35 Group means and 95% confidence interval of the mobility test measures for the 6MWT, TUG, StA and StD were included in Table 2.
Table 2.
Group means and 95% CI for mobility scores of older impaired adults who had fallen
| Mobility Test | Mean ± 95% CI |
|---|---|
| Six Minute Walk Test (M) | 482 [436,528] |
| Timed Up and Go (s) | 7.78 [7.03,8.54] |
| Stair Ascent (s) | 6.10 [5.52,6.67] |
| Stair Descent (s) | 6.09 [5.30,6.88] |
Abbreviations: (M) = Meters, (s) = Seconds
Muscle Force Steadiness and Mobility Tests
No significant correlations were detected for CON MFS and mobility tasks for the 6MWT (r=−0.22, p=0.93), TUG (r=−0.13, p=0.96), StA (r−0.14, p=0.55), and StD (r=0.02, p=0.93). Likewise, ECC MFS was not significantly correlated with mobility tasks consisting of the 6MWT (r=−0.39, p=0.09), TUG (r=0.42, p=0.07), StA (r=0.27, p=0.24), and StD (r=0.30, p=0.20).
Muscle Force Accuracy and Mobility Tests
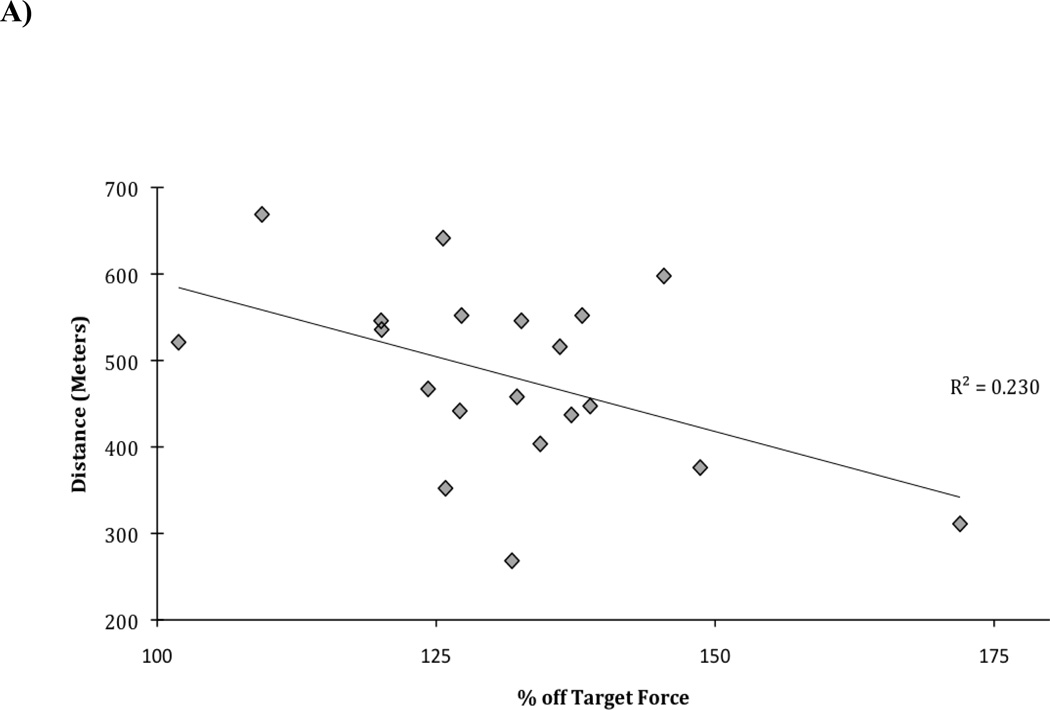
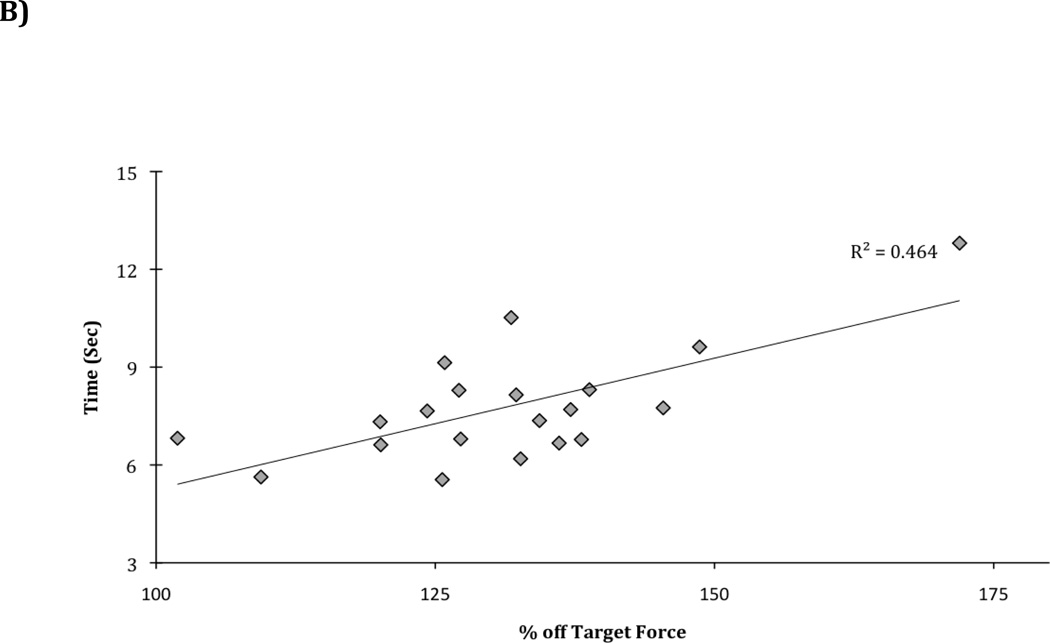
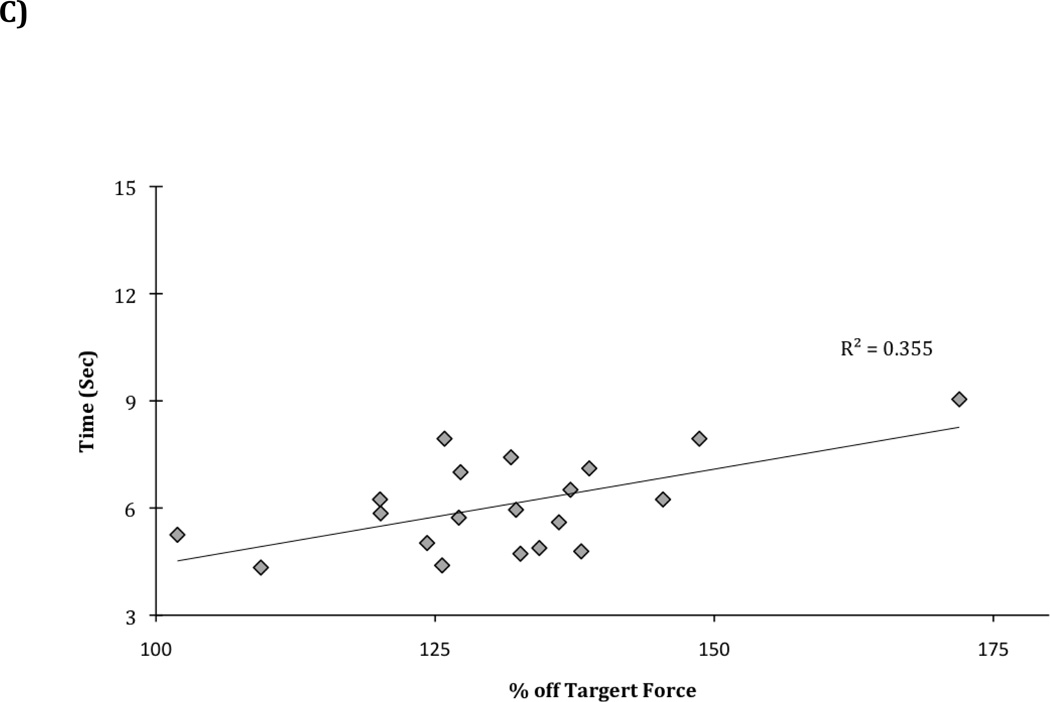
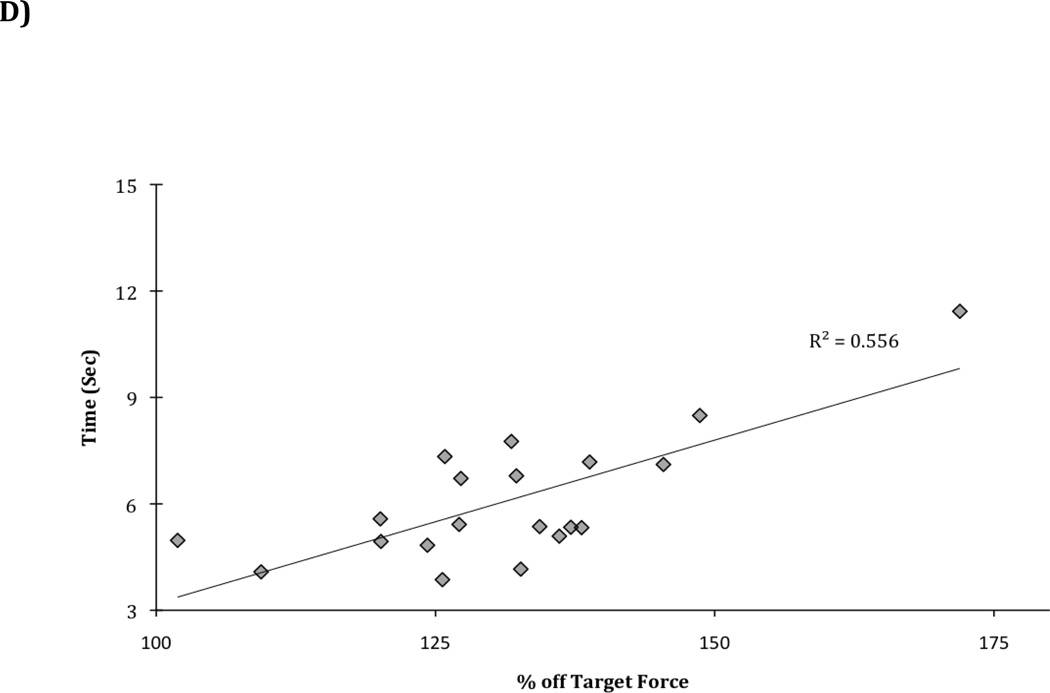
Although CON MFA was not correlated with mobility tasks for the 6MWT (r=−0.10, p=0.67), TUG (r=0.23, p=0.33), StA (r=0.17, p=0.47), and StD (r=0.38, p=0.10), there were moderate to good correlations for ECC MFA and the 6MWT (r=−0.48, p<0.05), TUG (r=0.68, p<0.01), StA (r=0.60, p<0.01), and StD (r=0.75, p<0.01) (Figure 2).
Figure 2. A–D Scatterplots, correlations between eccentric muscle force accuracy and mobility tests.
The scatterplots represent moderate to strong relationships between eccentric muscle force accuracy (MFA) (expressed as the percentage of target force) and mobility test scores: A) Eccentric muscle force accuracy and 6 minute walk r = −0.48, P<0.05; B) Eccentric muscle force accuracy and timed up and go test r = 0.68, P<0.01; C) Eccentric muscle force accuracy and stair ascent r = 0.60, P<0.01; D) Eccentric muscle force accuracy and stair descent r = 0.75, p<0.01.
DISCUSSION
The purpose of this study was to determine if the steadiness and accuracy of submaximal knee extensor force was correlated with performance on mobility tasks in older adults who had fallen. Interestingly, only force accuracy during ECC contractions was correlated with performance on mobility tasks. Force accuracy during ECC explained between ~23–56% of the variance in the performance of the mobility tasks. However, no significant associations were found between force steadiness measures during either CON or ECC contractions and mobility performance. Additionally, no significant correlations were detected between force accuracy during CON contractions and mobility performance. These findings are novel and unique in that: 1) this is the first report to document knee extensor force accuracy as a feature of submaximal muscle function linked to mobility tasks; 2) this is the first study to show that this relationship is specific to submaximal ECC contractions; and 3) these relationships may point to an important feature of muscle impairment in older adults who have fallen.
Previously reported evidence regarding MFA and mobility tasks is very limited. Only Seynnes et al. reported that submaximal isometric MFS was associated with chair rise time, yet no associations were detected between MFA and mobility tasks.36 And though Hortobagyi et al. did not correlate motor control measures (MFS & MFA) with functional tasks they reported that older adults demonstrated overshooting of the target force by 2 times the amount during CON and 3 times the amount during ECC contractions of the knee extensor muscles compared to young adults.15 Moreover, Carville et al. did not correlate steadiness measures with mobility, but rather reported that at-risk older adults who had fallen exhibited greater variability in motor output during eccentric but not concentric contractions of the knee extensors compared with older non-fallers.8 Collectively, the reported evidence of associations between knee extensor steadiness and accuracy (MFS and MFA) and mobility tasks is very limited and varies between contraction types.
Interestingly, others have compared steadiness and accuracy in older adults with performance tasks including general limb movement trajectories or motor tasks that require movement precision as performed by muscles of the hand.16,17 The general reported findings were that older adults demonstrated greater variability when performing ECC submaximal muscle contractions, particularly at low target force levels 9,15,19,37 when compared to young adults.3,18,20,24,38 Further, it is the relationships between task performance, movement precision, and force steadiness that may present additional challenges for older adults who have fallen.11,36,39
Possible Mechanisms
The plausible mechanisms that may explain associations between ECC force accuracy and mobility include: 1) unique characteristics or variations in the descending command during ECC compared with CON or isometric contractions; and 2) ability to modulate pre-synaptic inhibition of Ia afferents during ECC contractions.
Reviews by Enoka40, Duchateau and Enoka41, and Duchateau and Baudry42 have suggested how the motor output or descending command may vary when performing ECC compared to CON contractions. In general, when a CON contraction is performed, the torque produced by the muscle force produced is slightly greater than the torque produced by the applied load in order for the muscle to produce a shortening contraction. However, during an ECC contraction, the applied load torque is greater than the muscle force torque and the muscle performs a lengthening contraction.40,41 The muscle activation levels during submaximal ECC contractions may differ from that of CON contractions and the specific modulation of the activation signal to the targeted muscle may vary.9,43 For example, during an ECC contraction, reported evidence suggests that in addition to derecruitment of active motor units, the discharge rate also tends to decline.44 Accordingly, the overall activation level of a muscle is less during ECC contraction compared to CON.40 Further, changes in the neuromuscular system due to aging include reductions in the number of motor neurons and muscle fibers, motor unit remodeling via collateral sprouting from adjacent motor neurons, and increased size of existing motor units.45,46 Collectively, these age related changes to the motor unit can affect the activation and discharge rate of the motor units, thereby contributing to the variability in the force output.3,9,14
An additional mechanism that may play a contributory role to the increased variability in motor output is pre-synaptic inhibition of Ia afferents. Input from Ia afferents to the active motor neuron pool can be inhibited due to the depolarization of primary afferent fibers by interneurons and consequently affect the activation of the motor units to the targeted muscle.47,48 Further, depending on the task that is to be performed, whether position control or force control, older adults demonstrate a decreased ability to regulate presynaptic inhibition compared with young adults. For example, Baudry and Enoka47 reported that the ability of older adults to regulate presynaptic Ia afferent inhibition was reduced when individuals were tasked to control hand position while supporting a mass (position control) compared with exerting the same force against a rigid constraint (force control).
The clinical relevance of the reported findings in this study are such that MFA may be an additional factor to consider when exploring force control in older adults, particularly in those who have fallen, as this may impede or reduce their ability when performing mobility tasks. Since resistance exercise training can improve MFS in older adults.10,13,15,17,49 further investigation is warranted on the effects of such training on MFA measures, particularly during ECC contractions.
Limitations
This study included a relatively small number of individuals and multiple bivariate correlations. The results should be interpreted in light of the concept that statistical associations between ECC MFA and mobility tasks do not equate to causation. For example, discretion should be used with interpreting these particular outcomes to design interventions for improving force control in older adults who have fallen. However, these findings are novel and are at least suggestive that inaccurate submaximal force output during lengthening contractions may contribute to impaired mobility in older adults at risk for falling.
CONCLUSION
Overall, there were moderate to good correlations between the ability to produce accurate force during eccentric contractions and performance on mobility tasks in older adults who fall. These findings are novel and suggest that a decreased ability to regulate eccentric forces may contribute to impaired mobility in older adults who are at risk for falling or have fallen. Further investigations should determine if training-related improvements in force accuracy during lengthening contractions result in improved mobility in older adults at risk for falls.
Acknowledgments
However, author Paul C. LaStayo received NIH funding in-part: NIA R01AG031255-S1.
Footnotes
The aforementioned author’s declare that there were no conflicts of interests in conjunction with this study.
Some of the content of this paper was submitted as an abstract for platform presentation, research section, Combined Section Meeting, American Physical Therapy Association 2013, San Diego, CA. The abstract entitled, “Muscle force steadiness, force accuracy, and mobility function in older adults who have fallen: are they linked?” was accepted and presented in the Marilyn Gossman Scholars Graduate Student Research Seminar, January 2013.
Contributor Information
Kaiwi Chung-Hoon, Email: kaiwi.chunghoon@hsc.utah.edu.
Brian L. Tracy, Email: brian.tracy@colostate.edu.
Leland E. Dibble, Email: lee.dibble@hsc.utah.edu.
Robin L. Marcus, Email: robin.marcus@hsc.utah.edu.
Paul Burgess, Email: p.r.burgess@utah.edu.
Paul C. LaStayo, Email: paul.lastayo@health.utah.edu.
REFERENCES
- 1.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 2.Delbaere K, Bourgois J, Witvrouw EE, Willems TM, Cambier DC. Age-related changes in concentric and eccentric muscle strength in the lower and upper extremity: A cross-sectional study. Isokinetics and Exercise Science. 2003;11(3):145–151. [Google Scholar]
- 3.Galganski ME, Fuglevand AJ, Enoka RM. Reduced control of motor output in a human hand muscle of elderly subjects during submaximal contractions. J Neurophysiol. 1993;69(6):2108–2115. doi: 10.1152/jn.1993.69.6.2108. [DOI] [PubMed] [Google Scholar]
- 4.Schiffman JM, Luchies CW, Richards LG, Zebas CJ. The effects of age and feedback on isometric knee extensor force control abilities. Clin Biomech. 2002;17(6):486–493. doi: 10.1016/s0268-0033(02)00041-4. [DOI] [PubMed] [Google Scholar]
- 5.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903. [PubMed] [Google Scholar]
- 6.Hortobagyi T, Mizelle C, Beam S, DeVita P. Old adults perform activities of daily living near their maximal capabilities. J Gerontol A Biol Sci Med Sci. 2003;58(5):M453–M460. doi: 10.1093/gerona/58.5.m453. [DOI] [PubMed] [Google Scholar]
- 7.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 8.Carville SF, Perry MC, Rutherford OM, Smith IC, Newham DJ. Steadiness of quadriceps contractions in young and older adults with and without a history of falling. Eur J Appl Physiol. 2007;100(5):527–533. doi: 10.1007/s00421-006-0245-2. [DOI] [PubMed] [Google Scholar]
- 9.Enoka RM, Christou EA, Hunter SK, et al. Mechanisms that contribute to differences in motor performance between young and old adults. J Electromyogr Kinesiol. 2003;13(1):1–12. doi: 10.1016/s1050-6411(02)00084-6. [DOI] [PubMed] [Google Scholar]
- 10.Tracy BL, Byrnes WC, Enoka RM. Strength training reduces force fluctuations during anisometric contractions of the quadriceps femoris muscles in old adults. J Appl Physiol. 2004;96(4):1530–1540. doi: 10.1152/japplphysiol.00861.2003. [DOI] [PubMed] [Google Scholar]
- 11.Christou EA, Carlton LG. Age and contraction type influence motor output variability in rapid discrete tasks. J Appl Physiol. 2002;93(2):489–498. doi: 10.1152/japplphysiol.00335.2001. [DOI] [PubMed] [Google Scholar]
- 12.Krishnan C, Allen EJ, Williams GN. Effect of knee position on quadriceps muscle force steadiness and activation strategies. Muscle Nerve. 2011;43(4):563–573. doi: 10.1002/mus.21981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laidlaw DH, Kornatz KW, Keen DA, Suzuki S, Enoka RM. Strength training improves the steadiness of slow lengthening contractions performed by old adults. J Appl Physiol. 1999;87(5):1786–1795. doi: 10.1152/jappl.1999.87.5.1786. [DOI] [PubMed] [Google Scholar]
- 14.Christou EA. Aging and variability of voluntary contractions. Exerc Sport Sci Rev. 2011;39(2):77–84. doi: 10.1097/JES.0b013e31820b85ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hortobagyi T, Tunnel D, Moody J, Beam S, DeVita P. Low- or high-intensity strength training partially restores impaired quadriceps force accuracy and steadiness in aged adults. J Gerontol A Biol Sci Med Sci. 2001;56(1):B38–B47. doi: 10.1093/gerona/56.1.b38. [DOI] [PubMed] [Google Scholar]
- 16.Marmon AR, Pascoe MA, Schwartz RS, Enoka RM. Associations among strength, steadiness, and hand function across the adult life span. Med Sci Sports Exerc. 2011;43(4):560–567. doi: 10.1249/MSS.0b013e3181f3f3ab. [DOI] [PubMed] [Google Scholar]
- 17.Kornatz KW, Christou EA, Enoka RM. Practice reduces motor unit discharge variability in a hand muscle and improves manual dexterity in old adults. J Appl Physiol. 2005;98(6):2072–2080. doi: 10.1152/japplphysiol.01149.2004. [DOI] [PubMed] [Google Scholar]
- 18.Burnett RA, Laidlaw DH, Enoka RM. Coactivation of the antagonist muscle does not covary with steadiness in old adults. J Appl Physiol. 2000;89(1):61–71. doi: 10.1152/jappl.2000.89.1.61. [DOI] [PubMed] [Google Scholar]
- 19.Laidlaw DH, Bilodeau M, Enoka RM. Steadiness is reduced and motor unit discharge is more variable in old adults. Muscle Nerve. 2000;23(4):600–612. doi: 10.1002/(sici)1097-4598(200004)23:4<600::aid-mus20>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 20.Christou EA, Shinohara M, Enoka RM. Fluctuations in acceleration during voluntary contractions lead to greater impairment of movement accuracy in old adults. J Appl Physiol. 2003;95(1):373–384. doi: 10.1152/japplphysiol.00060.2003. [DOI] [PubMed] [Google Scholar]
- 21.Hortobagyi T, Garry J, Holbert D, Devita P. Aberrations in the control of quadriceps muscle force in patients with knee osteoarthritis. Arthritis Rheum. 2004;51(4):562–569. doi: 10.1002/art.20545. [DOI] [PubMed] [Google Scholar]
- 22.Christou EA, Poston B, Enoka JA, Enoka RM. Different neural adjustments improve endpoint accuracy with practice in young and old adults. J Neurophysiol. 2007;97(5):3340–3350. doi: 10.1152/jn.01138.2006. [DOI] [PubMed] [Google Scholar]
- 23.Sorensen TJ, Langberg H, Aaboe J, Bandholm T, Bliddal H, Henriksen M. The association between submaximal quadriceps force steadiness and the knee adduction moment during walking in patients with knee osteoarthritis. J Orthop Sports Phys Ther. 2011;41(8):592–599. doi: 10.2519/jospt.2011.3481. [DOI] [PubMed] [Google Scholar]
- 24.Tracy BL, Enoka RM. Older adults are less steady during submaximal isometric contractions with the knee extensor muscles. J Appl Physiol. 2002;92(3):1004–1012. doi: 10.1152/japplphysiol.00954.2001. [DOI] [PubMed] [Google Scholar]
- 25.Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82(2):128–137. doi: 10.1093/ptj/82.2.128. [DOI] [PubMed] [Google Scholar]
- 26.Crosbie J, Naylor JM, Harmer AR. Six minute walk distance or stair negotiation? Choice of activity assessment following total knee replacement. Physiother Res Int. 2010;15(1):35–41. doi: 10.1002/pri.453. [DOI] [PubMed] [Google Scholar]
- 27.Kervio G, Carre F, Ville NS. Reliability and intensity of the six-minute walk test in healthy elderly subjects. Med Sci Sports Exerc. 2003;35(1):169–174. doi: 10.1097/00005768-200301000-00025. [DOI] [PubMed] [Google Scholar]
- 28.Ploutz-Snyder LL, Manini T, Ploutz-Snyder RJ, Wolf DA. Functionally relevant thresholds of quadriceps femoris strength. J Gerontol A Biol Sci Med Sci. 2002;57(4):B144–B152. doi: 10.1093/gerona/57.4.b144. [DOI] [PubMed] [Google Scholar]
- 29.Enright PL. The six-minute walk test. Respir Care. 2003;48(8):783–785. [PubMed] [Google Scholar]
- 30.Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 31.LaStayo PC, Marcus RL, Dibble LE, Smith SB, Beck SL. Eccentric exercise versus usual-care with older cancer survivors: The impact on muscle and mobility--an exploratory pilot study. BMC Geriatr. 2011;11:5. doi: 10.1186/1471-2318-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith JW, Marcus RL, Peters CL, Pelt CE, Tracy BL, LaStayo PC. Muscle force steadiness in older adults before and after total knee arthroplasty. J Arthroplasty. 2014;29(6):1143–1148. doi: 10.1016/j.arth.2013.11.023. [DOI] [PubMed] [Google Scholar]
- 33.Wu TY, Chie WC, Yang RS, et al. Factors associated with falls among community-dwelling older people in Taiwan. Ann Acad Med Singapore. 2013;42(7):320–327. [PubMed] [Google Scholar]
- 34.Shumway-Cook A, Silver IF, LeMier M, York S, Cummings P, Koepsell TD. Effectiveness of a community-based multifactorial intervention on falls and fall risk factors in community-living older adults: a randomized, controlled trial. J Gerontol A Biol Sci Med Sci. 2007;62(12):1420–1427. doi: 10.1093/gerona/62.12.1420. [DOI] [PubMed] [Google Scholar]
- 35.Sjosten NM, Salonoja M, Piirtola M, et al. A multifactorial fall prevention programme in the community-dwelling aged: predictors of adherence. Eur J Public Health. 2007;17(5):464–470. doi: 10.1093/eurpub/ckl272. [DOI] [PubMed] [Google Scholar]
- 36.Seynnes O, Hue OA, Garrandes F, et al. Force steadiness in the lower extremities as an independent predictor of functional performance in older women. J Aging Phys Act. 2005;13(4):395–408. doi: 10.1123/japa.13.4.395. [DOI] [PubMed] [Google Scholar]
- 37.Tracy BL, Maluf KS, Stephenson JL, Hunter SK, Enoka RM. Variability of motor unit discharge and force fluctuations across a range of muscle forces in older adults. Muscle Nerve. 2005;32(4):533–540. doi: 10.1002/mus.20392. [DOI] [PubMed] [Google Scholar]
- 38.Graves AE, Kornatz KW, Enoka RM. Older adults use a unique strategy to lift inertial loads with the elbow flexor muscles. J Neurophysiol. 2000;83(4):2030–2039. doi: 10.1152/jn.2000.83.4.2030. [DOI] [PubMed] [Google Scholar]
- 39.Hortobagyi T, DeVita P. Altered movement strategy increases lower extremity stiffness during stepping down in the aged. J Gerontol A Biol Sci Med Sci. 1999;54(2):B63–B70. doi: 10.1093/gerona/54.2.b63. [DOI] [PubMed] [Google Scholar]
- 40.Enoka RM. Eccentric contractions require unique activation strategies by the nervous system. J Appl Physiol. 1996;81(6):2339–2346. doi: 10.1152/jappl.1996.81.6.2339. [DOI] [PubMed] [Google Scholar]
- 41.Duchateau J, Enoka RM. Neural control of shortening and lengthening contractions: influence of task constraints. J Physiol. 2008;586(24):5853–5864. doi: 10.1113/jphysiol.2008.160747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duchateau J, Baudry S. Insights into the neural control of eccentric contractions. Journal of Applied Physiology. 2013;113(7):1895–1904. doi: 10.1152/japplphysiol.00002.2013. [DOI] [PubMed] [Google Scholar]
- 43.Mottram CJ, Christou EA, Meyer FG, Enoka RM. Frequency modulation of motor unit discharge has task-dependent effects on fluctuations in motor output. J Neurophysiol. 2005;94(4):2878–2887. doi: 10.1152/jn.00390.2005. [DOI] [PubMed] [Google Scholar]
- 44.Nardone A, Romano C, Schieppati M. Selective recruitment of high-threshold human motor units during voluntary isotonic lengthening of active muscles. J Physiol. 1989;409:451–471. doi: 10.1113/jphysiol.1989.sp017507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vandervoort AA. Aging of the human neuromuscular system. Muscle Nerve. 2002;25(1):17–25. doi: 10.1002/mus.1215. [DOI] [PubMed] [Google Scholar]
- 46.Roos MR, Rice CL, Vandervoort AA. Age-related changes in motor unit function. Muscle Nerve. 1997;20(6):679–690. doi: 10.1002/(sici)1097-4598(199706)20:6<679::aid-mus4>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 47.Baudry S, Maerz AH, Enoka RM. Presynaptic modulation of Ia afferents in young and old adults when performing force and position control. J Neurophysiol. 2009;103(2):623–631. doi: 10.1152/jn.00839.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baudry S, Maerz AH, Gould JR, Enoka RM. Task- and time-dependent modulation of Ia presynaptic inhibition during fatiguing contractions performed by humans. J Neurophysiol. 2010;106(1):265–273. doi: 10.1152/jn.00954.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Doherty TJ. Invited review: Aging and sarcopenia. J Appl Physiol. 2003;95(4):1717–1727. doi: 10.1152/japplphysiol.00347.2003. [DOI] [PubMed] [Google Scholar]