Abstract
[Purpose] The aim of this study was to investigate the effect of a back care pillow (BCP) on pain, lumbar range of motion (LROM) and functional disability of patients with chronic non-specific low back pain (LBP). [Subjects and Methods] Fifty-two subjects who were aged between 20–69 years old, who presented with LBP of more than 3 months duration with a numerical rating scale (NRS) value of at least 4 were randomly assigned to treatment (BCP) and control (CON) groups. Participants in each group received six sessions of the 30 minutes treatment for two weeks. The BCP group was asked to wear the BCP during the daytime during the study period. Pain, lumbar ROM and functional disability were assessed before and after the 2-week treatment, and at the end of a 12-week follow up. [Results] After the 2-week treatment and 12-week follow up, all outcomes had improved in both groups; the BCP group had maintained the decrease in pain intensity and improved lumbar ROM in the extension position after the 12-week follow up, and showed better improvements in all outcomes at 2 weeks and after the 12-week follow up. [Conclusion] BCP combined with physical therapy had better pain, lumbar ROM and functional disability outcomes than physical therapy alone.
Key words: Lower back support, Chronic low back pain, Numerical rating scale
INTRODUCTION
Low back pain (LBP) is the most common problem in the world and is a major cause of disability, and work absenteeism, and has a high cost of treatment. A recent study reported the one year prevalence of LBP is more than 80%, and 10–20% of cases develop into chronic LBP1). A cause of non-specific LBP is tension, soreness and/or stiffness in the lower back region for which it is not easy to identify a specific cause of pain. Several structures in the back, including the joints, discs and connective tissues, may be causes of LBP symptoms2). An abnormal curvature of spine is associated with chronic non-specific LBP symptoms3). Thus, an important way of relieving and preventing LBP symptoms is suggested to be maintenance of the appropriate spine curvature of the lower back4).
There are many potential treatments for LBP. We previously reported that physical therapy including exercise and massage is an effective treatment for the release of muscle stiffness, amelioration of pain, and improvement of physical functions5,6,7). Physical therapy can provide beneficial effects for muscle relaxation and the spinal alignment in LBP. In addition to the treatment of physical therapy, instrument can be provided to support the lumbar spine and to reduce and prevent LBP symptoms, and lumbar support is frequently used to treat patients with LBP8). Appropriate lumbar lordosis decreases disc pressure by changing the distribution of the load between the disc and apophyseal joints and also reduces the tension in the intervertebral ligaments that can cause disc degeneration9, 10). Wearing a lumbar support may increase intra-abdominal pressure that can decrease disc pressure, limit disc compression, and reduce disc pain11). To create a better back supporter, the lumbar spinal curvature of an individual should be considered. A back care pillow (BCP) was designed to support the lumbar spine following the recommendation of a previous study. Measurements of lumbar spinal curvature in the normal population have shown that lumbar spinal curvature differs among age groups and genders12). However, there is lack of evidence to support the effect of a BCP in the treatment of chronic non-specific LBP patients. The aim of this study was to investigate the effects of a BCP on pain, ROM and the functional disability of patients with chronic non-specific LBP.
SUBJECTS AND METHODS
A randomized control trial was conducted with chronic non-specific LBP patients, who were assigned to receive a standard physical therapy treatment plus BCP or only physical therapy treatment. This study was approved by the Ethics Committee for Human Research of Khon Kaen University (Protocol No. HE552347) and it was prospectively registered with the United States Clinical Trials Registry (NCT01911806).
Patients were diagnosed as having chronic nonspecific LBP by medical doctors at the Department of Physical Therapy, Phiboonmungsaharn hospital, Thailand. Each patient was given a personal interview by a research assistant who had one year’s experience in orthopedic physical therapy and a physical examination by a medical doctor. Participants aged between 20–69 years old who presented with LBP for more than three months and had moderate to severe pain on a numerical rating scale (score ≥ 4) were eligible. Participants who had underlying systematic or visceral diseases, specific conditions such as neoplasm, ankylosing spondylitis, previous low back surgery, cauda equina syndrome, nerve root symptoms, or pregnancy were excluded.
The estimated sample size was calculated, based on the result of a pilot study. The standard deviation of the pain score (numeric rating scale: NRS) after treatment of both groups was used to calculate the sample size for a power of 80% at 5% significance and a drop-out rate of 20% was allowed for the estimate on of the final sample size. The required sample size was 26 subjects per group.
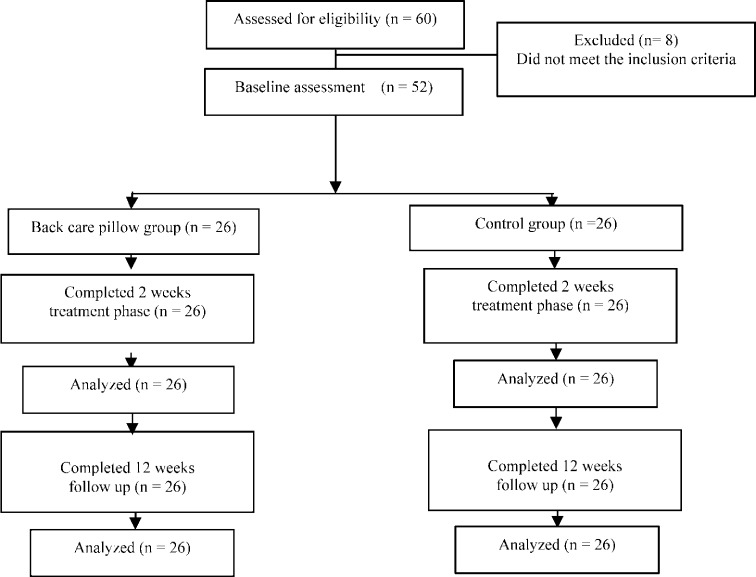
The patients who met the above inclusion criteria were randomly allocated to receive either the treatment with physical therapy alone (control group, CG), or the treatment with physical therapy and BCP (BCP group) using stratified random allocation by age group (group 1 = 20–29 years old, group 2 = 30–39 years old and group 3 = 40–69 years old) with block sizes of 2, 4 and 6. Figure 1 shows the design of the procedural flow and follow-up. A total of fifty-two participants with chronic non-specific LBP were eligible for the study. Details of the demographic data and health status are presented in Table 1. Most of the demographic data were equally balanced between the two groups.
Fig. 1.
Procedural flow and follow-up chart
Table 1. Baseline characteristics of the participants.
| Characteristics | BCP | CON | Total |
|---|---|---|---|
| Number of patients | 26 | 26 | 52 |
| Age (years); Mean±SD | 38.5±11.0 | 39.7±12.2 | 39.1±11.5 |
| 20–29 years; n (%) | 7 (27.0) | 7 (27.0) | 14 (27.0) |
| 30–39 years; n (%) | 7 (27.0) | 7 (27.0) | 14 (27.0) |
| Male 40–69 years; n (%) | 6 (23.0) | 6 (23.0) | 12 (23.0) |
| Female 40–69 years; n (%) | 6 (23.0) | 6 (23.0) | 12 (23.0) |
| Gender; n of female | 11 (42.3) | 13 (50.0) | 24 (46.2) |
| Weight (kg); Mean±SD | 60.0± 10.2 | 62.3±8.1 | 61.1±9.2 |
| Height (cm); Mean±SD | 160.5±7.3 | 164.4±7.8 | 162.4±7.8 |
| BMI; Mean±SD | 23.2±3.0 | 23.0±2.2 | 23.1±2.6 |
BCP: Back care pillow group; CON: Control group; SD: Standard deviation; BMI: Body mass index
Participants in each group received six sessions of 30 minutes treatment for two weeks conducted by the same licensed physical therapist who was blinded to the intervention. They were treated by ultrasound and hot pack.
The participants in the BCP group additionally received a BCP of a specific size for an age group’s standard lumbar spinal curvature determined in a previous study12). Each subject was asked to wear the BCP during the daytime in the treatment period and to continue using it during the 12-week follow up.
All outcomes were measured before and after the 2-week treatment, and at the end of the 12-week follow up.
Pain intensity was measured using a numerical rating scale (NRS). The scale ranged from 0 (no pain) to 10 (severe pain)13). Lumbar range of motion (LROM) was measured using the Modified-Modified Schober test. The examiner put his thumbs on the inferior margin of the posterior superior iliac spine. An ink mark was drawn along the midline of the lumbar spine horizontal to the posterior superior iliac spine (lower landmark). While the examiner held the tape firmly against the skin, he marked a second line 15 cm above the original one (higher landmark). Then, the subject was asked to do an active anterior flexion of the trunk without increasing the pain. The new distance between the lower and higher landmarks was measured. The subject returned to the neutral position. The difference in the initial distance between the skin markings in the neutral position and the measurement in the flexion position was used to indicate the amount of lumbar flexion. After each measurement, the skin marks were removed by rubbing with alcohol to ensure blinding of the next examiner to the landmarks14).
Functional disability was measured using the Thai version of the Roland-Morris Disability Questionnaire (RMDQ). This assesses perceived limitations in 24 activities of daily living, dichotomously. The sum of the score is calculated by summing the ‘yes’ answers. The scale ranges from 0 (no disability) to 24 (severe disability)15).
The data are presented as means and standard deviations (SD). All analyses were performed on the basis of intention-to-treat. One-way repeated measures ANOVA was employed to compare continuous outcome variables between baseline and after the treatment in the intervention group and CG. Analysis of covariance (ANCOVA) was performed to compare differences in outcome measures between the two treatment groups and to estimate the adjusted mean differences and the 95% confidence intervals of each outcome measure in each group. For statistical significance, 80% power and overall two-tailed 5% significance was used.
RESULTS
The baseline characteristics of the participants are shown in Table 1; there were no significant differences between the two groups. The intra-tester reliability of the modified-modified Schober method showed correlation coefficients ranging from 0.99 to 1.00 for the objective measurement of lumbar flexion and extension ROM in healthy volunteers.
After two weeks of treatment and at the 12-week follow up, the pain level and LROM in the BCP group and CG showed significant improvement from the baseline (Table 2). When the results after two weeks of treatment and at the end of the 12-week follow up were compared against the baseline, the pain level and LROM in the extension position showed significant improvements in the BCP group, while the CG did not show any significant differences. There were significant differences in the changes in pain intensity and LROM between the BCP group and CG (Table 3).
Table 2. Outcome measures after 2 weeks of treatment and the follow up of 12 weeks.
| Outcomes | Groups | Baseline | Short-term effectiveness (after 2 weeks of treatment) |
Long-term effectiveness (12 weeks follow-up) |
|---|---|---|---|---|
| NRS (scores) | BCP | 6.8±1.5 | 1.8±1.2* | 1.1±1.2* |
| CON | 6.4±1.5 | 4.1±1.1* | 4.4±1.5* | |
| LROM-flexion (mm) | BCP | 17.5±0.6 | 19.5±0.5* | 20.2±0.5* |
| CON | 17.6±1.1 | 18.3±1.0* | 18.8±1.1* | |
| LROM-extension (mm) | BCP | 14.4±0.3 | 13.1±0.6* | 12.7±0.4* |
| CON | 14.4±0.4 | 14.0±0.4* | 14.0±0.5* | |
| RMDQ (scores) | BCP | 16.2±5.3 | 5.9±3.7* | 2.3±2.7* |
| CON | 14.4±6.3 | 11.7±5.9* | 9.9±5.2* |
BCP: Back care pillow group; CON: Control group; SD: Standard deviation; NRS: Numerical rating scale; LROM: Lumbar range of motion; RMDQ: Roland Morris Disability Questionnaire. Values are presented as mean±SD. * Significantly different (p<0.01) from the baseline.
Table 3. Comparison of the adjusted mean and 95% CI of outcome measures (adjusted for baseline using ANCOVA) at each assessment time.
| Outcomes | Short-term effectiveness (after 2 weeks of treatment) |
Long-term effectiveness (12 weeks follow-up) |
||||
|---|---|---|---|---|---|---|
| BCP | CON | Difference (95% CI) |
BCP | CON | Difference (95% CI) |
|
| NRS (scores) | 1.8 | 4.1* | 2.3 (1.6 to 2.9) | 1.1 | 4.4* | 3.4 (2.6 to 4.1) |
| LROM-flexion (mm) | 19.5 | 18.3* | −1.3 (−1.5 to −1.0) | 20.3 | 18.7* | −1.5 (−1.9 to −1.1) |
| LROM-extension (mm) | 13.1 | 14.0* | 0.9 (0.7 to 1.2) | 12.7 | 14.0* | 1.4 (1.1 to 1.6) |
| RMDQ (scores) | 5.3 | 12.3* | 7.0 (5.3 to 8.7) | 1.8 | 10.3* | 8.5 (6.9 to 10.2) |
BCP: Back care pillow group; CON: Control group; SD: Standard deviation; NRS: Numerical rating scale; LROM: Lumbar range of motion; RMDQ: Roland Morris Disability Questionnaire. * Significant difference between BCP and CON (p<0.001).
There were significant decreases in the RMDQ score at each assessment time in both groups (Table 2). In the comparison of the groups, the BCP group showed more improvement in functional disability than the CG (Table 3).
DISCUSSION
This study demonstrated that BCP plus physical therapy for chronic non-specific LBP decreased pain intensity, improved LROM and functional disability better than standard physical therapy after 2 weeks of treatment and at the end of a 12-week follow up. BCP maintained the decrease in pain intensity and the improvement in LROM in the extension position for 12 weeks after the 2-week treatment.
In the comparison of the BCP group and CG, a clinically significant difference was found between the two groups in pain reduction. A mean difference in the NRS of greater than 2 is generally considered the minimum acceptable when looking for a significant clinical difference between groups16, 17). The clinical findings of the present study are similar to those of Calmels et al.8) who used a lumbar belt for patients with LBP. They found a decrease in pain intensity and RMDQ at 30 and 90 days after treatment in the intervention group. These improvements in RMDQ were clinically important changes in RMDQ16, 17). Other studies have also shown that the pain intensity and the functional status improved in patients with LBP who used a lumbar support for over 12 months; however, there were no significant clinical changes.
The benefits of BCP are possibly explained by mechanisms through which BCP maintain an appropriate lumbar curvature, preserving normal lumbar curve stability, and adaptation of muscle activity to the appropriate lumbar curve. This mechanism may also decrease back muscle spasms8). In addition, the appropriate lordotic curve may decrease intra-disc pressure by changing the distribution of loads between discs18). Decreased pressure on the apophyseal joints may decrease disc degeneration decreasing pain in the apophyseal joints19). The effect on spinal structure may also improve pain intensity; however, the lumbar range of motion provided no evidence to support our hypothesis of decreased pressure on the apophyseal joints.
Limitations of the present study were the small sample size, even though the sample size was calculated based on a pilot study. Further studies will need to investigate different populations, e.g. office workers, for longer periods. Finally, the mechanisms underlying the beneficial effects of BCP also need to be determined.
Acknowledgments
The study was supported by the Faculty of Associated Medical Science, Research Center in Back, Neck, Other Joint Pain and Human Performance (BNOJPH), Khon Kaen University, Khon Kaen, Thailand, and Phiboonmungsaharn Hospital, Thailand. We are grateful for the grant of research funds by the department of Science and Technology, Thailand Research Fund (TRF), and Yonnapa Pah Thai under a project of co-operation with the manufacturing sector sponsored by the research fund TRF-industry. The findings of this study belong to the researchers if the Thailand Research Fund (TRF) and Yonnapa Pah Thai always disagree.
REFERENCES
- 1.Hoy D, Brooks P, Blyth F, et al. : The Epidemiology of low back pain. Best Pract Res Clin Rheumatol, 2010, 24: 769–781. [DOI] [PubMed] [Google Scholar]
- 2.Henschke N, Maher CG, Refshauge KM, et al. : Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ, 2008, 337: a171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diab AA, Moustafa IM: The efficacy of lumbar extension traction for sagittal alignment in mechanical low back pain: a randomized trial. J Back Musculoskeletal Rehabil, 2013, 26: 213–220. [DOI] [PubMed] [Google Scholar]
- 4.Petersen T, Larsen K, Nordsteen J, et al. : The McKenzie method compared with manipulation when used adjunctive to information and advice in low back pain patients presenting with centralization or peripheralization: a randomized controlled trial. Spine, 2011, 36: 1999–2010. [DOI] [PubMed] [Google Scholar]
- 5.Hongsuwan C, Eungpinichpong W, Chatchawan U, et al. : Effects of Thai massage on physical fitness in soccer players. J Phys Ther Sci, 2015, 27: 505–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peungsuwan P, Sermcheep P, Harnmontree P, et al. : The effectiveness of Thai exercise with traditional massage on the pain, walking ability and QOL of older people with knee osteoarthritis: a randomized controlled trial in the community. J Phys Ther Sci, 2014, 26: 139–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Areeudomwong P, Puntumetakul R, Jirarattanaphochai K, et al. : Core stabilization exercise improves pain intensity, functional disability and trunk muscle activity in patients with clinical lumbar instability: a pilot randomized controlled study. J Phys Ther Sci, 2012, 24: 1007–1012. [Google Scholar]
- 8.Calmels P, Queneau P, Hamonet C, et al. : Effectiveness of a lumbar belt in subacute low back pain: an open, multicentric, and randomized clinical study. Spine, 2009, 34: 215–220. [DOI] [PubMed] [Google Scholar]
- 9.Cholewicki J, Shah KR, McGill KC: The effects of a 3-week use of lumbosacral orthoses on proprioception in the lumbar spine. J Orthop Sports Phys Ther, 2006, 36: 225–231. [DOI] [PubMed] [Google Scholar]
- 10.Lim HS, Roh SY, Lee SM: The relationship between pelvic tilt angle and disability associated with low back pain. J Phys Ther Sci, 2013, 25: 65–68. [Google Scholar]
- 11.Zarghooni K, Beyer F, Siewe J, et al. : The orthotic treatment of acute and chronic disease of the cervical and lumbar spine. Dtsch Arztebl Int, 2013, 110: 737–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puntumetakul R, Hiruntrakul P, Premchaisawat W, et al. : The measurement of lumbar spinal curvature in normal Thai population aged 20–69 years using flexible ruler. J Med Tech Phy Ther, 2012, 24: 308–317. [Google Scholar]
- 13.Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP: Validity of four pain intensity rating scales. Pain, 2011, 152: 2399–2404. [DOI] [PubMed] [Google Scholar]
- 14.Rezvani A, Ergin O, Karacan I, et al. : Validity and reliability of the metric measurements in the assessment of lumbar spine motion in patients with ankylosing spondylitis. Spine, 2012, 37: E1189–E1196. [DOI] [PubMed] [Google Scholar]
- 15.Jirarattanaphochai K, Jung S, Sumananont C, et al. : Reliability of the Roland - Morris Disability Questionnaire (Thai version) for the evaluation of low back pain patients. J Med Assoc Thai, 2005, 88: 407–411. [PubMed] [Google Scholar]
- 16.Ostelo RW, Deyo RA, Stratford P, et al. : Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine, 2008, 33: 90–94. [DOI] [PubMed] [Google Scholar]
- 17.Maughan EF, Lewis JS: Outcome measures in chronic low back pain. Eur Spine J, 2010, 19: 1484–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adams MA, May S, Freeman BJ, et al. : Effects of backward bending on lumbar intervertebral discs. Relevance to physical therapy treatments for low back pain. Spine, 2000, 25: 431–437, discussion 438. [DOI] [PubMed] [Google Scholar]
- 19.Cholewicki J, Juluru K, Radebold A, et al. : Lumbar spine stability can be augmented with an abdominal belt and/or increased intra-abdominal pressure. Eur Spine J, 1999, 8: 388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]