Abstract
[Purpose] This study aimed to investigate the perceived discomfort and trunk muscle activity in three different 1-hour sitting postures. [Subjects] A repeated-measures design study was conducted on 10 healthy subjects. [Methods] Each subject sat for an hour in three sitting postures (i.e., upright, slumped, and forward leaning sitting postures). Subjects rated perceived body discomfort using Borg’s CR-10 scale at the beginning and after 1 hour sitting. The electromyographic activity of the trunk muscle activity was recorded during the 1-hour period of sitting. [Results] The forward leaning sitting posture led to higher Borg scores in the low back than those in the upright (p = 0.002) and slumped sitting postures (p < 0.001). The forward leaning posture was significantly associated with increased iliocostalis lumborum pars thoracis (ICL) and superficial lumbar multifidus (MF) muscle activity compared with the upright and slumped sitting postures. The upright sitting posture was significantly associated with increased internal oblique (IO)/transversus abdominis (TrA) and ICL muscle activity compared with the slumped sitting posture. [Conclusion] The sitting posture with the highest low back discomfort after prolonged sitting was the forward leaning posture. Sitting in an upright posture is recommended because it increases IO/TrA muscle activation and induces only relatively moderate ICL and MF muscle activation.
Key words: Pain, Sitting posture, Electromyography
INTRODUCTION
Low back pain (LBP) is a significant health problem with a 1 year prevalence rate of between 41–64%1, 2), and approximately 60–80% of individuals report experiencing LBP once in their lifetime1, 3). A significant portion of individuals will develop chronic LBP4, 5). As a result, LBP creates a socioeconomic burden on society. Its total socioeconomic burden in the US in 2006 exceeded $100 billion6), and in the Netherlands, it exceeded 3.5 billion euro in 20077).
Evidence suggests that signs of perceived body discomfort, such as tension, fatigue, soreness, or tremors, are predictors of LBP8). Many individuals experience these musculoskeletal discomforts particularly at the buttock and low back regions during prolonged sitting9). Increased discomfort from prolonged sitting has been attributed to increased muscle fatigue10), decreased intervertebral disc nutrition11), and reduced blood flow in muscles12). Occupational groups exposed to poor postures while sitting have a considerably increased risk of experiencing LBP (OR=9.0, 95% CI 4.9–16.4)13). To date, no studies have investigated the effect of different sitting postures on perceived body discomfort.
Pain is generally viewed as a long-term effect of an imbalance between work-related physical factors and physical capacity, whereas perceived discomfort indicates a short-term effect8). Hodges and Moseley (2003) proposed that LBP can affect motor control by changing the excitability in the motor pathway, influencing the sensory system, and reducing muscle activity. The altered motor control patterns have been shown to recruit trunk muscles that compromise the stability of the lumbar spine14). Thus, perceived discomfort of muscles may reflect early signs of altered muscle activity, but it has received limited attention.
The aim of this study was to quantify perceived body discomfort and trunk muscle activities (i.e., rectus abdominis [RA], internal oblique/transversus abdominis [IO/TrA], iliocostalis lumborum pars thoracis [ICL], and superficial lumbar multifidus muscle [MF]) experienced during three sitting postures held for an hour (i.e., upright, slumped, and forward leaning sitting postures).
SUBJECTS AND METHODS
A pilot study was conducted, and the electromyography (EMG) values of the MF and IO/TrA, which are the core stabilizers of the lumbar spine, were used to calculate sample size. As a result, 10 healthy office workers were recruited for the study, which employed a repeated-measures design. Based on the sample size (n = 10), a power analysis revealed that the study had sufficient power (80%) to detect a “moderate to large” effect (f = 0.454–1.973). The inclusion criteria for the study were at least one year of experience in their current work positions and sitting at least two hours per working day. The exclusion criteria were neck and back pain in the preceding 12 months, current or past history of known spinal disorders, signs of neurological deficit (i.e., muscle weakness or loss/disturbance of sensation), osteoarthritis, rheumatoid arthritis, gout, kidney diseases, open wound or contusion at the buttocks or posterior thigh region, hemorrhoids, and pregnancy. Those with a body mass index <18.5 or >23 kg/m2 or skin fold thickness in the abdominal and suprailiac area >20 mm (to reduce EMG artifacts due to interposed adipose tissue between the surface electrode and the target muscles) were also excluded15). All subjects were provided information about the study and signed a consent form. The study was approved by the Chulalongkorn University Human Ethics Committee.
The Borg CR-10 scale, a measuring tool for postural discomfort, was used to determine each subject’s level of discomfort during prolonged sitting. The Borg CR-10 scale and a body chart from a standardized Nordic questionnaire were presented in such a way that the subjects could indicate which parts of their body experienced discomfort (i.e., the neck, shoulder, upper back, low back, hip/thigh, and knee) and how much discomfort was felt (on a scale of 0–10; 0 being no discomfort and 10 being extreme discomfort)16).
The EMG signals of trunk muscles, including the RA, IO/TrA, ICL, and MF, were recorded using two Ag/AgCl disposable surface electrodes with a distance between them of 20 mm (3 M Health Care, London, ON, Canada) and an electrical contact surface area of 1 cm2. Prior to electrode placement, the skin was prepared to reduce skin impedance below 5 kΩ by cleaning with an alcohol swab. Electrodes were placed parallel to the following muscles on both sides as recommended by the European Recommendations for Surface Electromyography (SENIAM): RA, 1 cm above the umbilicus and 2 cm lateral to midline; IO/TrA, 1 cm medial to the anterior superior iliac spine; ICL, midway between the midline and lateral aspect of the participant’s body at the level of L1 spinous process; and MF, 2 cm from the spinous process at the L5 level17,18,19). The reference electrode was placed over the right iliac crest. All electrodes were anchored securely by double-sided tape to avoid excessive movement of the leads, which remained in place throughout the session.
The EMG signal was recorded by a TeleMyo 2400T G2 (Noraxon U.S.A., Inc., Scottsdale, AZ, USA). The EMG signal was sampled at 1,500 Hz, band-pass filtered between 20–450 Hz, amplified (analogue differential amplifier, common mode rejection ratio 100 dB, total gain 500), and stored in a personal computer for later analysis.
The EMG signals were collected, stored, displayed, processed, and analyzed by MyoResearch XP software version 1.08. The raw EMG signal was first visually checked for electrocardiac artifacts. It was processed for ECG reduction, band-pass filtered at 20 to 450 Hz using a fourth-order zero-lag Butterworth filter, full-wave rectified, and then smoothed within 50 ms to determine the RMS.
Two minutes of every 10 minutes of normalized EMG data from the 60-minute sitting period (i.e., the first 2 minutes, 9th–11th minutes, 19th–21st minutes, 29th–31st minutes, 39th–41st minutes, 49th-51st minutes, and 59th–61st minutes) were retrieved for analysis.
EMG data were normalized to the maximal voluntary isometric contraction (MVIC) values obtained for each muscle, resulting in EMG data expressed as a percent of maximum voluntary isometric contraction (%MVIC). For the right and left RA, the subjects were positioned supine on a couch with the legs straight and strapped to the couch with a belt. The investigator (standing at the head end of the couch) applied resistance to the shoulders of the subjects while they performed a resisted curl up with maximal manual isometric resistance applied in a symmetrical manner20). For the right IO/TrA, a resisted crossed curl up was performed by the subjects with the left shoulder moving toward the right and maximal manual isometric resistance applied to the left shoulder by the investigator (standing on the right side). For the left IO/TrA, the same procedure was repeated on the opposite side. For the ICL and MF, the subject were positioned prone, with the legs straight and strapped to the couch with a belt. They were instructed to lift their head, shoulders, and elbows just off the examination table with their hands on their neck. Symmetrical maximal manual resistance was provided to the scapular region by the investigator (standing at the head of the subject)19).
Three MVIC trials of 5 seconds duration each21) with a 3 minute rest period between trials to avoid the cumulative effect of fatigue were performed22). The MVIC of each muscle was averaged over the three trials.
An experiment was conducted in which outcomes were repeatedly measured in subjects who sat in different sitting positions for a period of 1 hour. Three common sitting postures were investigated in the present study, including upright, slumped, and forward leaning sitting postures23). The measurement outcomes were perceived body discomfort and trunk muscle activity.
At the beginning, the subjects were instructed to complete the Borg CR-10 scale. Following the application of surface electrodes, they sat unsupported on a stool with their hips and knees at 90 degrees flexion, their feet positioned shoulder width apart, and their arms relaxed at the sides of their body. The stool was built to accommodate a person with a height of 180 cm so that he/she would sit with their hips and knees at 90 degrees flexion. Those of height below 180 cm sat on the stool with foam pads placed underneath their feet so that their hips and knees were at 90 degrees flexion. The subjects were asked to sit for an hour watching a movie, during which time the EMG signals of the RA, IO/TrA, ICL, and MF were collected. During the 1 hour of sitting, the subjects were instructed to avoid talking and to maintain the assigned sitting posture as much as possible with subtle movements allowed if they felt too much discomfort. After completion of the 1-hour sitting period, the subjects were asked to complete the Borg CR-10 scale again.
Each subject sat in the three sitting postures (i.e., upright, slumped, and forward leaning sitting postures) on 3 separate days with a 1-day interval between measurements. The sequence of sitting postures was randomized. The upright sitting posture consisted of sitting with anterior rotation of the pelvis, the thoracolumbar spine extended, and the shoulder blades slightly retracted24). The slumped sitting posture consisted of sitting with posterior rotation of the pelvis and the thoracolumbar spine relaxed while the subjects looked straight ahead24). The forward leaning sitting posture consisted of sitting with anterior rotation of the pelvis and the thoracolumbar spine extended while bending forward more than 10 degrees25). In the forward leaning sitting posture, the subjects were asked to cross their arms to prevent use of them to support body weight.
To control the alignment of sitting postures during the experiment, an adjustable vertical alignment stick was developed and attached to the right side of a regular stool (size 30 × 45 × 45 cm). In the upright sitting posture (Fig. 1B), the adjustable vertical stick was set at 90 degrees. In the forward leaning sitting posture, the adjustable vertical stick was set at 10 degrees forward from the vertical line (Fig. 1C). In the slumped sitting posture (Fig. 1A), the adjustable vertical stick was not used. Two infrared sensors (Distance Measuring Sensor Unit, GP2Y0A21YK0F, Sharp Corporation, Osaka, Japan) were inserted into the adjustable vertical alignment stick at the T1 and T10-level26). An auditory feedback signal from the sensors sounded if the subjects deviated from the selected sitting posture, reminding them to return to the proper sitting posture.
Fig. 1.
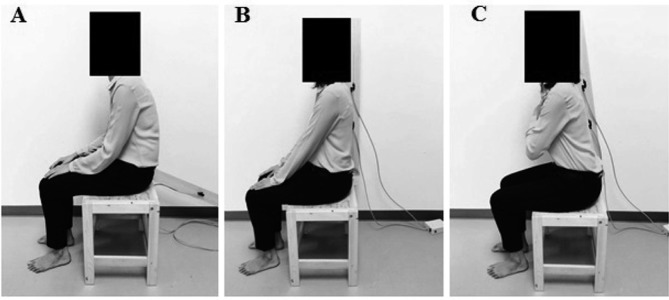
(A) Slump sitting, (B) Upright sitting, (C) Forward leaning sitting
Kolmogorov-Smirnov’s test was performed to check the distribution of the data. The paired-sample t-test was used to compare the Borg scores before and after an hour of sitting in each sitting posture. Also, the Borg scores after an hour of sitting were compared among the three sitting postures using one-way analysis of covariance (ANCOVA), with the Borg scores at the beginning as the covariate. The Bonferroni procedure was performed to determine whether two selected means were significantly different from each other.
Two-way analysis of variance (ANOVA) for repeated measures was employed to determine the effects of sitting posture, time, and sitting posture x time interaction on the EMG activity of trunk muscles. When a significant interaction between sitting posture and time was detected, the effects of sitting posture and time were examined separately using one-way ANOVA. The Tukey post hoc comparison was used to determine whether two selected means of the EMG activity of trunk muscles were significantly different from each other for the EMG activity of trunk muscles. All statistical analyses were performed using the SPSS statistics software, version V17.0 (SPSS Inc, Chicago, IL, USA).
RESULTS
The demographic characteristics of the participants are presented in Table 1. The Borg scores at the neck, upper back, low back and both hip/thighs after 1 hour of sitting were significantly greater than those at the beginning (Table 2). There was no significant difference in the Borg scores after 1 hour of sitting among the three sitting postures in all body regions (p > 0.05), except for the low back (F2,26 = 23.208, p < 0.001). The Borg score in the forward leaning sitting posture was significantly greater than those in the upright (p = 0.002) and slumped sitting postures (p < 0.001). There was a significant difference in Borg scores between upright sitting posture and slumped sitting posture (p = 0.021).
Table 1. Characteristics of study population (n = 10).
| Characteristics | Mean (SD) |
|---|---|
| Age (years) | 26.3 (1.6) |
| Gender (female) | 7 |
| Height (cm) | 164.2 (7.3) |
| Weight (kg) | 56.1 (7.5) |
| Body mass index (kg/m2) | 20.7 (1.4) |
| Skin fold thickness (mm) | |
| Abdominal area | 15.7 (3.0) |
| Suprailiac area | 7.4 (3.3) |
Table 2. The Borg scores at the beginning and after 1 hour of sitting in nine body regions.
| Body region | Mean Borg scores | |||||
|---|---|---|---|---|---|---|
| Upright sitting | Slumped sitting | Forward leaning sitting | ||||
| Before | After | Before | After | Before | After | |
| Neck | 0.050 | 1.250* | 0.400 | 2.500* | 0.150 | 0.900* |
| Rt. shoulder | 0.200 | 0.900 | 0.300 | 0.750 | 0.000 | 0.550 |
| Lt. shoulder | 0.000 | 0.500 | 0.000 | 0.500 | 0.000 | 0.500 |
| Upper back | 0.500 | 0.950* | 0.200 | 0.950* | 0.000 | 2.500* |
| Low back | 0.200 | 2.300* | 0.300 | 0.750 | 0.300 | 4.400* |
| Rt. hip/thigh | 0.000 | 0.800* | 0.000 | 0.150 | 0.000 | 0.900* |
| Lt. hip/thigh | 0.000 | 0.700* | 0.000 | 0.150 | 0.000 | 0.800* |
| Rt. knee | 0.000 | 0.300 | 0.000 | 0.000 | 0.000 | 0.000 |
| Lt. knee | 0.000 | 0.300 | 0.000 | 0.000 | 0.000 | 0.000 |
*p value < 0.05
Paired t-tests revealed no significant difference between sides for the EMG data, and therefore, the left and right side data were averaged. Two-way mixed ANOVA indicated no significant effect of sitting posture (F2,27=0.482, p=0.623), time (F6,162=0.159, p=0.987), and sitting posture × time interaction (F12,162=0.886, p=0.563) on RA EMG activity. There was a significant effect of sitting posture on IO/TrA (F2,27=4.013, p=0.030), ICL (F2,27=23.879, p<0.001), and MF (F2,27=31.647, p<0.001) EMG activity. No significant effects of time and sitting posture × time interaction were found on IO/TrA (F12,162=1.210, p=0.280), ICL (F12,162=0.510, p=0.906), and MF (F12,162=0.542, p=0.884) EMG activities.
The Tukey post hoc comparison revealed that IO/TrA EMG activity in the upright sitting posture was significantly greater than that in the slumped sitting posture (p = 0.048). The EMG activities of the ICL for the three sitting postures were significantly different from each other (p = 0.001–0.008). The EMG activity of the MF in the forward leaning sitting posture was significantly greater than those in the upright and slumped sitting postures (p ≤ 0.001).
DISCUSSION
The results of this study revealed that 1 hour of sitting in upright, slumped, or forward leaning sitting postures led to increased discomfort at the neck, upper back, low back, and hip/thighs. Different sitting postures influenced discomfort after 1 hour of sitting only in the low back. The sitting posture with the highest low back discomfort after 1 hour of sitting was the forward leaning posture, followed by the upright and slumped sitting postures, respectively. The forward leaning sitting posture was associated with increased ICL and MF muscle activity compared with the upright and slumped sitting postures. The upright sitting posture was associated with increased IO/TrA and ICL muscle activity compared with the slumped sitting posture. We found no effect of 1 hour of sitting, regardless of sitting posture, on trunk muscle activity.
The results of the present study are in line with the findings of previous studies showing that perceived body discomfort increased significantly during prolonged sitting9). Vergara and Page27) reported that discomfort occurred mainly in the neck and low back. Perceived musculoskeletal discomfort is a predictor of LBP among healthy subjects8). Thus, our findings lend further support to the notion that prolonged sitting may lead to the development of LBP.
Prolonged sitting in the forward leaning posture significantly increased discomfort in the low back compared with sitting in the upright and slumped postures. In the forward leaning sitting posture, the pelvis tilts forward, and the center of gravity is in front of the ischial tuberosities. Forward rotation of the pelvis or forward bending of the trunk during sitting significantly increases back muscle activity28, 29). In the current study, ICL and MF muscle activities were significantly greater in the forward leaning sitting posture than the upright and slumped sitting postures. Prolonged activation of muscle may lead to localized muscle tension, muscle strains, muscle fatigue, and other soft-tissue damage. Paraspinal muscle fatigue reduces the muscular support to the spine, causing impairment of motor co-ordination and control as well as increased mechanical stress on ligaments and intervertebral discs12, 30). In addition, the load on the vertebral body increases approximately 48% at 15-degree trunk flexion31). Vergara and Page27) reported that forward rotation of the pelvis and increased lumbar lordosis were associated with LBP. Thus, it is hypothesized that sitting in the forward leaning posture for a long period of time may lead to the development of LBP.
Our finding that the upright sitting posture is associated with increased IO/TrA and ICL muscle activity compared with the slumped sitting posture concurs with a study by O’Sullivan et al24). Internal oblique muscle activation is generally accepted to represent the activation of the TrA in all tasks32). Evidence suggests that the main dynamic stabilizer of the lower back and pelvis is the TrA33). Contraction of the TrA was found to be significantly delayed in patients with low back pain34). Core stability exercises have a strong theoretical basis in the treatment and prevention of LBP, as evidenced by their widespread clinical use35). Thus, the upright sitting posture with increased activation of the TrA would be an appropriate posture for a long period of time spent sitting.
A reduction in the EMG activity of trunk muscles in slumped sitting has been reported consistently in the literature36, 37). When postural muscle activity decreases, the lumbopelvic region becomes dependent on its passive structures to maintain the position against gravity at end-range spine flexion38). This phenomenon plausibly makes the spine susceptible to injury.
Although there is still a lack of international consensus over the ideal sitting posture, the findings of the current study suggest that a person should avoid sitting in a forward leaning posture for a prolonged time because it induces high perceived discomfort and back muscle activity, which may lead to the development of LBP. The slumped sitting posture is the most comfortable sitting posture for the low back after 1 hour of sitting. However, the slumped sitting posture reduces muscle activation of the trunk, which may adversely cause overloading of ligaments and intervertebral discs, leading to the development of LBP. The upright sitting posture seems to be a healthy sitting posture for the low back because it leads to activation of the local spinal stabilizing muscles, i.e., the TrA, and causes only moderate discomfort after prolonged sitting.
There are a number of methodological limitations that are noteworthy. First, the sample size was relatively small (n=10), increasing the likelihood of a type II error, although calculation of the statistical power based on 10 subjects indicated that the study had an 80% probability of detecting moderate to large effects. Second, the sitting postures tested in this study were controlled. Variations in how a person sits may exist and affect perceived body discomfort and trunk muscle activity. For example, in this study, subjects were asked to cross their arms to prevent use of them to support body weight while sitting in the forward leaning sitting posture. Further research on the effect of arm support on perceived body discomfort and trunk muscle activity is recommended. Lastly, the present study only investigated perceived body discomfort and trunk muscle activity in young healthy subjects. The change in perceived body discomfort and trunk muscle activity during various sitting postures for a prolonged time in individuals with LBP may not correspond to that of an asymptomatic population. Thus, extrapolation of these results to people with LBP should be made with caution. Further research is required to examine the effect of prolonged sitting posture on perceived body discomfort and trunk muscle activity in patients with LBP.
In conclusion, the current study examined perceived body discomfort and trunk muscle activity in different prolonged (1 hour) sitting postures, i.e., upright, slumped, and forward leaning sitting postures. The results showed that the highest low back discomfort after 1 hour of sitting occurred with the forward leaning posture, followed by the upright and slumped sitting postures. The forward leaning sitting posture was associated with increased ICL and MF muscle activity, and the upright sitting posture was associated with increased IO/TrA and ICL muscle activity. The findings from this study suggest that the upright sitting posture may be an appropriate sitting posture to prevent the development of LBP in individuals who usually spend a long period of time sitting.
REFERENCES
- 1.Manchikanti L: Epidemiology of low back pain. Pain Physician, 2000, 3: 167–192. [PubMed] [Google Scholar]
- 2.Barrero LH, Hsu YH, Terwedow H, et al. : Prevalence and physical determinants of low back pain in a rural Chinese population. Spine, 2006, 31: 2728–2734. [DOI] [PubMed] [Google Scholar]
- 3.Ihlebaek C, Hansson TH, Laerum E, et al. : Prevalence of low back pain and sickness absence: a “borderline” study in Norway and Sweden. Scand J Public Health, 2006, 34: 555–558. [DOI] [PubMed] [Google Scholar]
- 4.Henschke N, Maher CG, Refshauge KM, et al. : Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ, 2008, 337: a171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costa LC, Maher CG, McAuley JH, et al. : Prognosis for patients with chronic low back pain: inception cohort study. BMJ, 2009, 339: b3829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katz JN: Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am, 2006, 88: 21–24. [DOI] [PubMed] [Google Scholar]
- 7.Lambeek LC, van Tulder MW, Swinkels IC, et al. : The trend in total cost of back pain in The Netherlands in the period 2002 to 2007. Spine, 2011, 36: 1050–1058. [DOI] [PubMed] [Google Scholar]
- 8.Hamberg-van Reenen HH, van der Beek AJ, Blatter BM, et al. : Does musculoskeletal discomfort at work predict future musculoskeletal pain? Ergonomics, 2008, 51: 637–648. [DOI] [PubMed] [Google Scholar]
- 9.Søndergaard KH, Olesen CG, Søndergaard EK, et al. : The variability and complexity of sitting postural control are associated with discomfort. J Biomech, 2010, 43: 1997–2001. [DOI] [PubMed] [Google Scholar]
- 10.Hosea TM, Simon SR, Delatizky J, et al. : Myoelectric analysis of the paraspinal musculature in relation to automobile driving. Spine, 1986, 11: 928–936. [DOI] [PubMed] [Google Scholar]
- 11.Maroudas A, Stockwell RA, Nachemson A, et al. : Factors involved in the nutrition of the human lumbar intervertebral disc: cellularity and diffusion of glucose in vitro. J Anat, 1975, 120: 113–130. [PMC free article] [PubMed] [Google Scholar]
- 12.McGill SM, Hughson RL, Parks K: Lumbar erector spinae oxygenation during prolonged contractions: implications for prolonged work. Ergonomics, 2000, 43: 486–493. [DOI] [PubMed] [Google Scholar]
- 13.Lis AM, Black KM, Korn H, et al. : Association between sitting and occupational LBP. Eur Spine J, 2007, 16: 283–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hodges PW, Moseley GL: Pain and motor control of the lumbopelvic region: effect and possible mechanisms. J Electromyogr Kinesiol, 2003, 13: 361–370. [DOI] [PubMed] [Google Scholar]
- 15.Anuurad E, Shiwaku K, Nogi A, et al. : The new BMI criteria for Asians by the regional office for the western pacific region of WHO are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J Occup Health, 2003, 45: 335–343. [DOI] [PubMed] [Google Scholar]
- 16.Borg G: Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health, 1990, 16: 55–58. [DOI] [PubMed] [Google Scholar]
- 17.De Foa JL, Forrest W, Biedermann HJ: Muscle fibre direction of longissimus, iliocostalis and multifidus: landmark-derived reference lines. J Anat, 1989, 163: 243–247. [PMC free article] [PubMed] [Google Scholar]
- 18.Hermens HJ, Freriks B, Merletti R, et al. : European recommendations for surface electromyography. Roessingh Research and Development, Enschede 1999. [Google Scholar]
- 19.Danneels LA, Cagnie BJ, Cools AM, et al. : Intra-operator and inter-operator reliability of surface electromyography in the clinical evaluation of back muscles. Man Ther, 2001, 6: 145–153. [DOI] [PubMed] [Google Scholar]
- 20.Dankaerts W, O’Sullivan P, Burnett A, et al. : Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine, 2006, 31: 698–704. [DOI] [PubMed] [Google Scholar]
- 21.Jang EM, Kim MH, Oh JS: Effects of a bridging exercise with hip adduction on the EMG activities of the abdominal and hip extensor muscles in females. J Phys Ther Sci, 2013, 25: 1147–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McLean L, Chislett M, Keith M, et al. : The effect of head position, electrode site, movement and smoothing window in the determination of a reliable maximum voluntary activation of the upper trapezius muscle. J Electromyogr Kinesiol, 2003, 13: 169–180. [DOI] [PubMed] [Google Scholar]
- 23.Harrison DD, Harrison SO, Croft AC, et al. : Sitting biomechanics part I: review of the literature. J Manipulative Physiol Ther, 1999, 22: 594–609. [DOI] [PubMed] [Google Scholar]
- 24.O’Sullivan PB, Dankaerts W, Burnett AF, et al. : Effect of different upright sitting postures on spinal-pelvic curvature and trunk muscle activation in a pain-free population. Spine, 2006, 31: E707–E712. [DOI] [PubMed] [Google Scholar]
- 25.Nachemson A: The effect of forward leaning on lumbar intradiscal pressure. Acta Orthop Scand, 1965, 35: 314–328. [DOI] [PubMed] [Google Scholar]
- 26.Claus AP, Hides JA, Moseley GL, et al. : Is ‘ideal’ sitting posture real? Measurement of spinal curves in four sitting postures. Man Ther, 2009, 14: 404–408. [DOI] [PubMed] [Google Scholar]
- 27.Vergara M, Page A: Relationship between comfort and back posture and mobility in sitting-posture. Appl Ergon, 2002, 33: 1–8. [DOI] [PubMed] [Google Scholar]
- 28.Mastalerz A, Palczewska I: The influence of trunk inclination on muscle activity during sitting on forward inclined seats. Acta of bioengineering and biomechanics / Wroclaw University of Technology, 2010, 12: 19–24. [PubMed] [Google Scholar]
- 29.Mork PJ, Westgaard RH: Back posture and low back muscle activity in female computer workers: a field study. Clin Biomech (Bristol, Avon), 2009, 24: 169–175. [DOI] [PubMed] [Google Scholar]
- 30.Wilke H, Neef P, Hinz B, et al. : Intradiscal pressure together with anthropometric data—a data set for the validation of models. Clin Biomech (Bristol, Avon), 2001, 16: S111–S126. [DOI] [PubMed] [Google Scholar]
- 31.Rohlmann A, Zander T, Graichen F, et al. : Measured loads on a vertebral body replacement during sitting. Spine J, 2011, 11: 870–875. [DOI] [PubMed] [Google Scholar]
- 32.McGill S, Juker D, Kropf P: Appropriately placed surface EMG electrodes reflect deep muscle activity (psoas, quadratus lumborum, abdominal wall) in the lumbar spine. J Biomech, 1996, 29: 1503–1507. [DOI] [PubMed] [Google Scholar]
- 33.Lee JS, Kim TH, Kim DY, et al. : Effects of selective exercise for the deep abdominal muscles and lumbar stabilization exercise on the thickness of the transversus abdominis and postural maintenance. J Phys Ther Sci, 2015, 27: 367–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hodges PW: Is there a role for transversus abdominis in lumbo-pelvic stability? Man Ther, 1999, 4: 74–86. [DOI] [PubMed] [Google Scholar]
- 35.Cho HY, Kim EH, Kim J: Effects of the CORE exercise program on pain and active range of motion in patients with chronic low back pain. J Phys Ther Sci, 2014, 26: 1237–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Callaghan JP, Dunk NM: Examination of the flexion relaxation phenomenon in erector spinae muscles during short duration slumped sitting. Clin Biomech (Bristol, Avon), 2002, 17: 353–360. [DOI] [PubMed] [Google Scholar]
- 37.Miura T, Sakuraba K: Influence of different spinal alignments in sitting on trunk muscle activity. J Phys Ther Sci, 2013, 25: 483–487. [Google Scholar]
- 38.O’Sullivan PB, Grahamslaw KM, Kendell M, et al. : The effect of different standing and sitting postures on trunk muscle activity in a pain-free population. Spine, 2002, 27: 1238–1244. [DOI] [PubMed] [Google Scholar]


