Abstract
[Purpose] This study evaluated a specific rehabilitation protocol using a half squat after total knee reconstruction with distal femur megaprosthesis and tibial allograft-prosthesis composite. [Subject and Methods] Squat execution was recorded by a three-dimensional system before and after a specific rehabilitation program on a 28-year-old patient. Squat duration, body center of mass trajectory, and vertical range of motion were determined. Step width and joint angles and symmetry (hip flexion, extension, and rotation, knee flexion, and ankle dorsal and plantar flexion) were estimated. Knee and hip joint symmetry was computed using a bilateral cyclogram technique. [Results] After rehabilitation, the squat duration was longer (75%), step width was similar, and vertical displacement was higher. Hip flexion increased by over 20%, and ankle dorsiflexion diminished by 14%. The knee had the highest symmetry gain (4.1–3.4%). Angle-angle plot subtended areas decreased from 108° to 40°2 (hip) and from 204° to 85°2 (knee), showing improvement in movement symmetry. [Conclusion] We concluded that the squat is an effective multifactorial exercise to estimate rehabilitation outcomes after megaprosthesis, also considering that compressive and shear forces are minimal up to 60–70° of knee flexion.
Key words: Knee prosthesis, Half-squat, Knee ROM
INTRODUCTION
The squat is one of the most common exercises in strengthening and conditioning protocols1), and it is a closed kinetic chain exercise commonly performed in rehabilitation settings2). In particular, the half-squat (70–100°) and semi-squat (40°) are recommended for knee rehabilitation2).
The number of muscles involved1, 3), the shear force implicated2), the low load near the proximal third of the femur shaft4) (which is very compliant in total joint replacement), and the similarity to a wide range of daily-living tasks1, 4) make the squat a very useful exercise in rehabilitation programs. Moreover, the compressive forces involved during the squat cycle (in particular between 40% and 60%4)) are an important factor in knee stabilization, minimizing the reciprocal translation between the femur and the tibia2). Although the squat is a common exercise, rehabilitation outcomes are often evaluated through force testing procedures or gait analysis.
This report aims to evaluate a specific rehabilitation protocol after osteosarcoma resection and megaprosthesis implantation using half-squat exercises. Due to the large bone and muscle mass implicated in joint replacement surgery, physicians could benefit from an understanding of the usefulness of half-squat exercises since they are easy to perform and can be utilized alongside traditional gait analysis.
SUBJECT AND METHODS
One 28-year-old man was voluntarily recruited after total knee resection and reconstruction with a distal femur megaprosthesis and tibial allograft-prosthesis composite. He was diagnosed with a synovial sarcoma (monophasic fibrous, right knee). During surgery, 6.1 cm of the distal femur and 6.4 cm of the proximal tibia were removed. After one month, a surgical wound revision was made. Chemotherapy followed the surgical treatment.
Five months later, he underwent a new surgical reconstruction in order to accommodate the extensor mechanism after a patellar tendon rupture. Surgical intervention again became necessary 3 and 5 years later because of a mechanical failure; megaprosthesis revisions were made to replace polyethylene components and to revise the extensor mechanism. A knee brace in extension was worn for 30 days and subsequently an unlocked brace for another 4 weeks. Then he began walking with full weightbearing as tolerated.
The first evaluation took place one month after the final surgery before beginning rehabilitation. He reported a high score on the Functional Independence Measure (119/126); thigh muscle circumferences were 51 cm (right), and 55 cm (left). Passive knee flexion was reduced at 100°, while passive extension was increased (about 10°). Knee extension strength was 3/5 as measured by the British Medical Research Council scale. Sensation was intact. During standing, a right-sided genu recurvatum was evident.
After an explanation of all procedures, written informed consent was obtained from the participant. The Local Ethical Committee and the medical staff of the hospital approved all phases of this study. The same operator (a physiotherapy expert in conditioning and training) asked the patient to perform five half squat repetitions. No indication about the squat depth was given, and the upper limbs were allowed to hang freely3). To avoid visual feedback that could alter movement spontaneity, no mirror was present in the room. The operator provided cues during all trials to keep the heels in contact with the floor5) in order to avoid compensatory movements at the knees, hips, and spine and to guarantee power generation and stabilization in the foot bones1). The operator also specified a posture as close as possible to an upright position at all times to maintain the spine in a neutral alignment1). Moreover, to reduce spinal compression, the patient was asked to perform an anti-flexion movement before starting the action and to hold his breath1). After 40 sessions (90 minutes each) of the rehabilitation program outlined below, the subject re-performed the squat trials. Following is a brief description of the therapy (gym and hydrotherapy).
The exercises performed during the gym sessions were: quadriceps, hamstring, and gluteus isometric contractions (5 s hold); quadriceps and hamstring co-contractions with the knee at 0, 30, and 90 degrees of flexion; passive, active-assisted, and active hip-knee-ankle joint mobilization; knee flexion (without external load, closed eyes), stopping the movement at 15, 30, 60, and 90 degrees; sit to stand; frontal and lateral step up and down; and squat exercises at a self-chosen depth.
The standing trial consisted of: one-legged standing, standing with eyes open and closed on a firm surface/foam cushion; and gait training on flat surfaces and on stairs. Stair training began with a single step up (height 15 cm), and after strength improvements increased to four steps up and down with a handrail.
Hydrokinesitherapy (water level of 1.20 m) included: posture correction exercises (requested to practice standing for 2 minutes); walking forward, backward, and sideways; half-squat; single leg balance; proprioception exercises keeping a board under the foot; and skipping exercises.
The patient was able to progress from 10 to 30–40 repetitions of each exercise. Fatigue or pain was the criteria to stop any performance. Exercise repetition and series were progressed depending on the patient’s level of perceived exertion.
During squat execution, kinematic data were sampled at 120 Hz with a motion analysis system (SMART, BTS, Italy). Nine infrared cameras positioned around a working volume of 4.2 × 2.6 × 2.4 m3 recorded the three-dimensional (3D) coordinates of 25 passive 1-cm reflective markers placed on the patient’s forehead, seventh cervical vertebra, sacrum, right and left tragi, acromia, olecranon, ulna styloid processes, anterior superior iliac spines, greater trochanters, femoral lateral and medial epicondyles, tibial apophyses, lateral malleoli, heels, and first metatarsal heads. The duration of each squat was recorded. Subsequently, squat cycles were normalized to a 100-samples time sequence. Events were located by visually inspecting the 3D coordinates of the sacrum marker. The cycle started and ended when the sacrum displacement between consecutive frames was higher or lower than 0.5 cm in at least one direction.
Body center of mass (COM) trajectory was estimated with the segmental centroid method validated by Mapelli et al6). In particular, the COM vertical range of motion (ROM) was obtained.
Step width was computed by measuring the transverse plane distance between the centroid of the markers of each foot.
Joint angles (hip flexion, extension, and rotation, knee flexion, and ankle dorsal/plantar flexion) were estimated by computing the relative rotation matrix between the anatomical frames attached to each body segment. The ZYʹXʺ Euler convention was adopted. Joint ROMs were obtained. Anterior displacement (AD) was computed as the maximum angle on the sagittal plane between the Y-axis and the vector connecting lateral malleolus and the greater trochanter.7) High AD values meant that the subject was leaning forward, while an AD of 0° indicated that the trochanter marker was vertically aligned with the malleolus.
Parameters extracted from the squat cycles were presented as mean±standard deviation (SD) and the percentage change between measurements. To assess the relative asymmetry of each parameter, the Symmetry Angle (SA) parameter was computed as8):
 |
Xleft and Xright are the corresponding left and right parameters. An SA value of 0% indicates perfect symmetry, while 100% indicates that the two values are equal and opposite in magnitude. Finally, to account for the asymmetry of joint kinematics throughout the entire cycle, the bilateral cyclogram technique was adopted.9) The area within the angle-angle plot would be null in a perfectly symmetric coupling.
RESULTS
The squat duration was considerably longer (75%) after rehabilitation. Step width was almost the same, while in the second measurement the COM vertical displacement was 30% higher (Table 1). After rehabilitation, the most evident changes in joint ROMs were hip flexion, augmented more than 20%, and ankle dorsiflexion, which diminished by 14%. The knee had the highest gain in ROM symmetry (SA reduced from 4.1% to 3.4%). AD was slightly greater on both sides after rehabilitation, with an increase in SA of about 9%.
Table 1. Mean ± SD of selected biomechanical parameters of the five squat exercises. Pre- and post-intervention results are provided.
| Pre | Post | Percent change (%) | |
|---|---|---|---|
| Exercise execution | |||
| Squat duration (s) | 3.60±0.54 | 6.30±0.59 | 74.9 |
| COM vertical ROM (m) | 0.224±0.022 | 0.288±0.019 | 29.2 |
| Postural arrangement | |||
| Step width (m) | 0.283±0.002 | 0.289±0.002 | 1.8 |
| Right anterior displacement (degrees) | 2.5±0.5 | 3.9±0.4 | 56.8 |
| Left anterior displacement (degrees) | 3.2±0.2 | 3.8±0.1 | 17.4 |
| Symmetry angle (%) | −7.9 | 1.2 | 9.1 |
| Joint ROM | |||
| Right hip flexion (degrees) | 57.4±3.9 | 69.7±1.7 | 21.4 |
| Left hip flexion (degrees) | 54.1±7.9 | 65.3±1.2 | 20.6 |
| Symmetry angle (%) | 1.9 | 2.1 | 0.2 |
| Right knee flexion (degrees) | 74.9±0.2 | 72.4±0.7 | −3.4 |
| Left knee flexion (degrees) | 65.9±3.1 | 65.1±2.2 | −1.3 |
| Symmetry angle (%) | 4.1 | 3.4 | −0.7 |
| Right ankle flexion (degrees) | 23.8±2.5 | 20.6±1.4 | −13.7 |
| Left ankle flexion (degrees) | 26.5±3.0 | 22.8±0.7 | −14.1 |
| Symmetry angle (%) | −3.4 | −3.3 | 0.1 |
Percent change was computed as [(post value-pre value)/pre value]*100.
Hip and knee flexion angles are shown in the left panels of Fig. 1: a good alignment of lower limbs can be observed at movement inversion (50% of the cycle, at the plateau between the descent and ascent phase). On the affected side, the hip was more externally rotated after rehabilitation, up to 10° in the lowest COM position. The angle-angle plot subtended area (Fig. 1, right panels) decreased from 108 to 40 squared degrees (hip) and from 204 to 85 squared degrees (knee), showing a great improvement in the symmetry of movement (visible as the joint angular overlap in the descent and ascent phases).
Fig. 1.
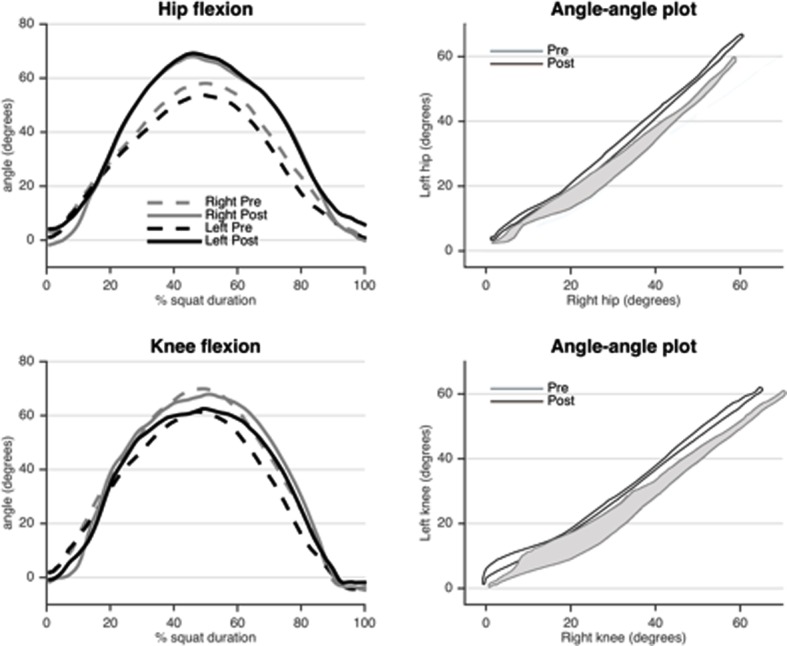
Average hip (top panels) and knee (bottom panels) flexion kinematics during the squat exercises on both sides and measurements. The right panels illustrate the angle-angle plot of each measurement as an indicator of movement symmetry. The area within the cyclogram in the hip joint reduced (top right) from 108 (pre) to 40 (post) squared degrees and in the knee joint (bottom right) from 204 (pre) to 85 (post) squared degrees.
DISCUSSION
Megaprosthesis surgery is highly invasive but allows patients to achieve full independence with an appropriate rehabilitation program. A major issue for these patients is to gain the best outcome in terms of daily activity and work experience. At present, only few researchers have provided protocols, tests, or scales to evaluate recovery. Since gaining acceptable gait capability is by far the primary outcome sought by physicians and therapists, rehabilitation programs are often focused on walking exercises. Our aim, however, was to verify if another closed chain exercise, like the half squat, could be a valid test of rehabilitation progress and if it could be used during routine rehabilitation exercises.
The patient executed the squat exercises well; although the COM vertical ROM increased by 29%, the AD on each side remained low (increase <2°), proving that the load was kept close to the support base; therefore, movement was controlled by lower limb action rather than by trunk movement. Without verbal or visual feedback, the subject freely reached about 70° of knee flexion. This level corresponds to half-squatting1, 2), where the anterior shear and compressive forces are at a minimum, the posterior shear forces are not yet implicated, and the tendofemoral stress is reduced2). Squat duration was longer after rehabilitation. As it can be seen in Fig. 1 (bottom left panel), knee flexion exhibited a plateau at movement inversion, indicating a better load management. These data are even more interesting considering the augmented COM vertical displacement and that the support base was kept almost equal. The knee flexion and angle-angle plots also revealed good motor control at the knee joint level with symmetry between sides and between the phases of movement.
Hip flexion ROM increased on both sides after rehabilitation, up to normal values10). Furthermore, we noticed good symmetry between the right and left limbs, denoted by a 60% reduction in the angle-angle plot subtended area. However, the peak value was reached before 50% of the squat cycle. For this reason, the hip pattern may need slight correction, considering that the maximum flexion should be around 55% of the cycle9). Hip external rotation increased after rehabilitation. Although this may appear positive, it could indicate a massive activation of the hip musculature that took the place of the quadriceps for anti-gravity actions. Ankle dorsiflexion was more symmetrical after rehabilitation, indicating similar displacements on both sides. This is crucial, since the ankle complex significantly contributes to general body support.
In the current study, objective body motion measurements were obtained without any invasive intervention. This is crucial for patients who have undergone chemotherapy and substantial bone resections. In particular, the squat exercise analysis, which has rarely been conducted in this physiotherapy context, allowed us to gain an interesting insight about force and motor control recovery in a young patient with knee megaprosthesis. Results highlighted that the half-squat could be a reliable exercise in rehabilitation procedures, involving both lower limb and spine musculature2) and motor control.
Force improvements in the quadriceps, hamstrings and glutei1, 2) were independently observed together with increased vertical displacement and longer movement inversion duration. A good movement pattern of hip and knee flexion was reached, since both joint ROMs became similar10), while the general arrangement of the foot and ankle complex was improved; better load management was gained without any support base variation. Furthermore, better motor control could be hypothesized by observing the AD as an indicator of body weight management. We may conclude that the squat is an effective multifactorial exercise for estimating rehabilitation outcomes after megaprosthesis, also considering that the compressive and shear forces are minimal up to 60°–70° of knee flexion2).
REFERENCES
- 1.Schoenfeld BJ: Squatting kinematics and kinetics and their application to exercise performance. J Strength Cond Res, 2010, 24: 3497–3506. [DOI] [PubMed] [Google Scholar]
- 2.Escamilla RF: Knee biomechanics of the dynamic squat exercise. Med Sci Sports Exerc, 2001, 33: 127–141. [DOI] [PubMed] [Google Scholar]
- 3.Dionisio VC, Almeida GL, Duarte M, et al. : Kinematic, kinetic and EMG patterns during downward squatting. J Electromyogr Kinesiol, 2008, 18: 134–143. [DOI] [PubMed] [Google Scholar]
- 4.D’Angeli V, Belvedere C, Ortolani M, et al. : Load along the femur shaft during activities of daily living. J Biomech, 2013, 46: 2002–2010. [DOI] [PubMed] [Google Scholar]
- 5.Kasuyama T, Sakamoto M, Nakazawa R: Ankle joint dorsiflexion measurement using the deep squatting posture. J Phys Ther Sci, 2009, 21: 195–199. [Google Scholar]
- 6.Mapelli A, Zago M, Fusini L, et al. : Validation of a protocol for the estimation of three-dimensional body center of mass kinematics in sport. Gait Posture, 2014, 39: 460–465. [DOI] [PubMed] [Google Scholar]
- 7.Neumann DA: Kinesiology of the Musculoskeletal System, 2nd ed. London: Mosby, 2002. [Google Scholar]
- 8.Zifchock RA, Davis I, Higginson J, et al. : The symmetry angle: a novel, robust method of quantifying asymmetry. Gait Posture, 2008, 27: 622–627. [DOI] [PubMed] [Google Scholar]
- 9.Goswami A: Kinematic quantification of gait symmetry based on bilateral cyclograms. US Pat, 2009, 7, 503, 900. [Google Scholar]
- 10.Butler RJ, Plisky PJ, Southers C, et al. : Biomechanical analysis of the different classifications of the functional movement screen deep squat test. Sports Biomech, 2010, 9: 270–279. [DOI] [PubMed] [Google Scholar]


