Abstract
Effective transitions to home care have been identified as among the factors leading to reducing hospital readmissions within 30 days of discharge and improvements on various other quality measures. Innovative applications of published evidence-based models and best practices designed to improve care transitions have been implemented in various settings across the country in an effort to enhance quality performance. For this article, The Joint Commission collected a series of case examples to examine how evidence-based innovations in care transitions are reducing readmissions and improving other quality outcomes. The organizations providing the case examples were interviewed and asked to provide performance data demonstrating quality improvement, as well as information about their care processes and data-gathering techniques. Their innovative approaches are reducing hospital readmissions; improving patient safety, satisfaction, and engagement; and contributing to other positive outcomes.
Introduction
Figure.

No caption available.
Over the past several years, many evidence-based transitions of care models developed to improve patient outcomes have been published in the literature. These models include:
Care Transitions Program (Coleman et al., 2006),
Transitional Care Model (TCM; Naylor & Sochalski, 2010),
State Action on Avoidable Rehospitalizations (also known as STAAR; Sevin et al., 2013),
Better Outcomes for Older Adults Through Safe Transitions (BOOST; Project BOOST, 2010),
The Bridge Model (Illinois Transitional Care Consortium, 2010),
Guided Care (Johns Hopkins, 2012),
Geriatric Resources for Assessment and Care of Elders (also known as GRACE; Counsell et al., 2006), and
Project RED (Boston University Medical Center, 2003).
These innovative models have drawn considerable interest as hospitals work to reduce 30-day readmissions and avoid Medicare penalties. In 2012, the all-cause 30-day hospital readmission rate among Medicare fee-for-service beneficiaries was 18.5% (Centers for Medicare & Medicaid Services, 2013). The 30-day readmission rate for patients with chronic conditions such as heart failure, chronic obstructive pulmonary disorder (COPD), pneumonia, and diabetes is a few percentage points higher (Agency for Healthcare Research and Quality [AHRQ], 2012). AHRQ (2010) has documented the higher readmission rates and costs associated with patients having multiple comorbidities, as well. These data have caused healthcare organizations to focus their attention on high-risk patients in efforts to reduce readmissions and unnecessary costs. Hospitals also understand that new payment models will require the ability to achieve population health goals by successfully transitioning patients and managing them outside the walls of an inpatient facility.
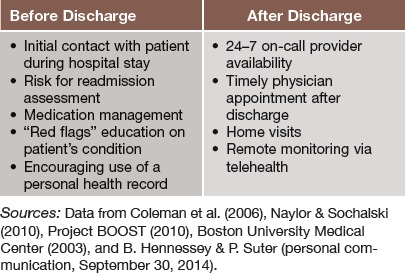
Organizations specializing in home care are adopting quality measures to demonstrate the value home care contributes to improved outcomes—particularly lower readmission rates of patients with conditions associated with a high rate of readmissions, such as heart failure, COPD, pneumonia, and diabetes. Home healthcare agencies (HHAs)—including one or more of those featured in this paper—are also improving quality performance on measures such as emergency department visits, patient satisfaction, caregiver competence, and patient compliance. The published research on care transitions to home recommends a set of interventions introduced before or after discharge. Table 1 outlines these interventions.
Table 1.
Recommended Interventions Before and After Discharge
Background and Methods
The Joint Commission has a particular interest in improving care transitions, thereby enhancing quality and safety performance and evidence-based health outcomes relating to readmissions and, more specifically, to accountability measures of performance related to heart attack, heart failure, pneumonia, surgical care, childhood asthma, inpatient psychiatric services, immunizations, perinatal care, and care of patients with venous thromboembolism and stroke. To contribute to the important conversation about care transitions, The Joint Commission engaged professionals within the home care community associated with recent initiatives to improve outcomes to provide insight on current practices in care transitions. They were asked to describe the key process steps in their transitions programs and to provide an overview of their quality measures and performance data.
The five healthcare organizations contributing information for this article were chosen because of their reputations in the home care community. The examples reflect an emphasis on real-time innovation rather than research. All of the featured organizations are working to respond quickly to cost pressures and patient needs through innovative approaches to transitions of care. They plan, implement, and revise according to what works and what does not work. This article aims to show that outstanding outcomes can be achieved through evidence-based innovation and to encourage all healthcare organizations to pursue quality improvement efforts in this area. Five examples of organizations that have developed innovations in transitions of care, along with the results they have achieved, follow.
Sutter Care at Home: Patient Engagement and Self-Management With a Focus on Health Literacy
Sutter Care at Home conducted an extensive review of the literature to compare various transitional care models. This review guided the development of the Integrated Care Management (ICM) Transitions of Care Program. The program identifies patients at high risk for hospital readmission according to the Institute for Healthcare Improvement's patient risk categories. High-risk patients are identified as those admitted twice or more in the last year, and patients/family caregivers who are unable to teach back or who demonstrate low confidence in self-care at home (Sevin et al., 2013).
The ICM program focuses on patient engagement through the provision of self-management support and health-literate care. The team begins in-hospital bedside visits after the patient chooses Sutter Care at Home. The team asks each patient to identify his or her personal concerns at the time of care transition to permit individualized transition care planning (B. Hennessey & P. Suter, personal communication, September 30, 2014). Citing a study that found nearly 9 of 10 adults have difficulty using routinely available health information (Kutner et al., 2006), the Sutter team uses a health-literacy universal-precautions approach by providing a jargon-free medications list and “stoplight” action plans. Written in plain language and supported by the teach-back process, the “stoplight” plans help the patient understand signs/symptoms associated with his or her particular medical condition by organizing the symptoms by green (under control, no need for action), yellow (take action today), and red (take action now). For example, for weight control, no change in weight is green, an increase of 3 lb overnight or 5 lb in a week is yellow, and an increase in 5 lb overnight is red.
The Sutter team has ensured the consistent use of SBAR communication—situation, background, assessment, recommendation—by placing SBAR prompts in Sutter Care at Home's electronic medical record's transitions summary note. After discharge, patients receive a visit from a home care nurse within 24 hours. The nurse reinforces stoplight instructions, reconciles medications, and reviews the patient's identified concerns. High-risk patients receive a total of nine “touch points” (in-person, telehealth, or telephone contacts) within the first 2 weeks of care. Patients readmitted within 30 days are reviewed at a case conference to determine what could have prevented the readmission.
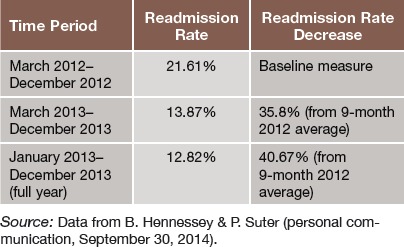
Sutter collected readmission outcomes data before the transitions program's introduction and measures postintervention data monthly, using a pre–post time design (Table 2). The data come directly from claims data across the system. Sutter Medical Center at Santa Rosa began implementation of the program in March 2012, with the entire protocol rolled out by December 2012. Two other HHAs replicated Sutter's program. White County Medical Center in Arkansas reported a 47% readmissions decline, and First Health in North Carolina achieved a 38% decline (B. Hennessey & P. Suter, personal communication, September 30, 2014).
Table 2.
Readmission Rates, Sutter Medical Center at Santa Rosa
Virtua Home Care: The Use of Transitional Care Nurses and a Multidisciplinary Approach
Virtua Home Care developed its Transitions of Care Program by adapting the TCM developed at the University of Pennsylvania. Key components are the use of transitional care nurses (TCNs) and a multidisciplinary team to provide intensive follow-up care. Virtua's program provides services to patients with heart failure, COPD, pneumonia, and/or diabetes who are enrolled in fee-for-service Medicare and are eligible to receive the home healthcare benefit. The program's goal was to reduce readmissions among this population while remaining cost-neutral (Berry et al., 2011; Su et al., 2011).
The TCN follows the patient from hospital to home and provides interventions to reduce readmissions and optimize the patient's health status. The multidisciplinary team includes physicians, social workers, discharge planners, pharmacists, and others; their focus is to provide coordinated and ongoing clinical care while working to encourage the active engagement of the patient and caregivers in care management (Naylor et al., 2004).
Virtua prepared field nurses with experience in cardiopulmonary nursing and home care to be the TCNs. The preparation focused on the TCNs learning the standards of practice for each of the chronic diseases and the principles of health coaching. The TCNs have regular patient case conferences with Virtua's home care medical director, who is a board-certified geriatrician. Recommendations from the medical director have helped the TCNs to develop effective care plans for the patients. During case conferences, the TCN gains support and input from the multidisciplinary team to set realistic patient goals, help patients recognize the need for self-management, and coach patients in navigating the healthcare system (Berry et al., 2011; Su et al., 2011).
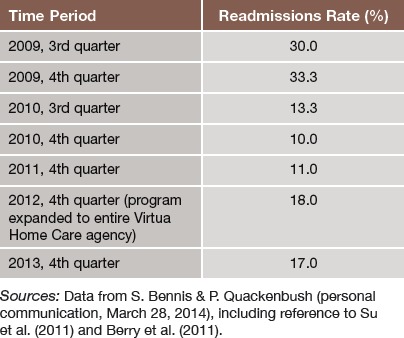
Virtua uses a dashboard to measure all-cause readmissions for patients with the four chronic illness diagnoses and achieved a gradual decline in the 30-day readmissions rates for patients participating in the Transitions of Care Program. Table 3 illustrates readmissions results from the start of the program in 2009 to the fourth quarter of 2013. In keeping with the agency's goal of keeping the program budget neutral, no new budgeted positions were added to implement the program (S. Bennis & P. Quackenbush, personal communication, March 28, 2014).
Table 3.
Readmissions Rates, Virtua Home Care Transitions of Care Program
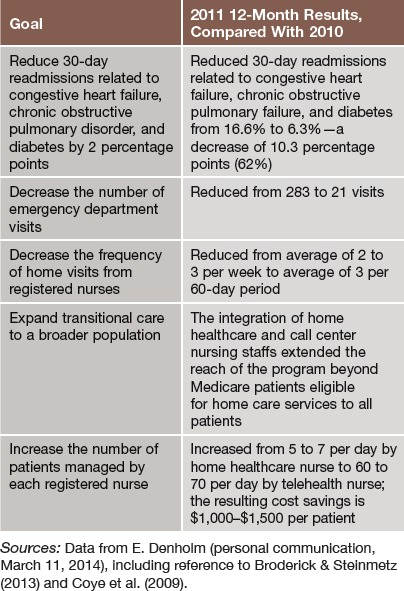
Centura Health at Home: Using Telehealth for an Entire Patient Population
Centura Health at Home's telehealth program integrated previously separate home healthcare and clinical call center nurses. The goals were to reduce 30-day readmissions related to heart failure, COPD, and diabetes by 2 percentage points; decrease the number of emergency department visits; decrease the frequency of home visits from registered nurses (RNs); expand transitional care to a broader population; and increase the number of patients managed by each RN (Broderick & Steinmetz, 2013; E. Denholm, personal communication, March 11, 2014).
For patients covered by Medicare's home healthcare benefit, the RNs monitor vital signs, weight, and behavioral health data via remote technology located in patient homes while providing care coordination, advice, and assistance via telephone. Patients use devices, such as scales, blood pressure cuffs, pulse oximeters, and thermometers, to measure their vital signs and transmit the data via phone line at least once daily, and more if the condition requires it. RNs can call patients if there are significant changes in vital signs or health status and involve a physician if necessary. Primary care physicians write up “as needed” orders that nurses can modify, allowing the monitoring nurses to react to trending data within a specified set of parameters. Patients can see the vital sign data, and having this information suggests when patients should talk to a nurse and helps patients to reduce anxiety, according to Centura patient satisfaction and self-management measurement data. Patients can contact the clinical call center with questions 24-7. Centura discharges patients from the remote monitoring program when they no longer meet home care criteria (Broderick & Steinmetz, 2013; E. Denholm, personal communication, March 11, 2014).
Centura does not monitor patients who do not qualify for the Medicare home healthcare benefit via the remote technology. For these patients, RNs make weekly phone calls usually for 3 weeks to review medication lists and care plans, compare medications to discharge orders, and provide teach-back education to further patients' understanding of their conditions and lifestyle behaviors. During these calls, RNs identify potential medical issues and help to arrange follow-up interventions as needed. Centura discharges patients in the calls-only intervention when the three weekly calls are complete or when the patient self-discharges (Broderick & Steinmetz, 2013; E. Denholm, personal communication, March 11, 2014). Table 4 outlines Centura's quality results.
Table 4.
Quality Performance, Centura Health at Home
Pediatric Home Service: Comprehensive Care for Young Patients With Medical Complexities
Pediatric Home Service (PHS) provides home care to young patients with medical complexities. Under the direction of an on-staff medical director, PHS provides services including respiratory therapy, infusion nursing and pharmacy, home care nursing provided by an RN or LPN, specialized nutrition, and clinical social work services. PHS also provides education and training for nurses, patients, and family caregivers. Clinical support is available 24/7 (PHS Management Staff, conference call and e-mail communication, March 25, 2014).
PHS's home care delivery model includes:
Home care coordination throughout the discharge process.
A clinician assigned to each patient. This clinician (usually a RN or respiratory therapist) coordinates the care plan. If the patient requires medical equipment in the home, this clinician visits the home prior to hospital discharge to plan equipment locations and assure safety.
Clinical educators and technical support staff who train parents and other caregivers to care for children and use equipment safely and effectively. They translate manufacturers' instructions into user-friendly language and images for parents and caregivers.
Ongoing follow-up visits by the assigned clinician or other PHS staff, ensuring patient safety through continuous education and reeducation when necessary.
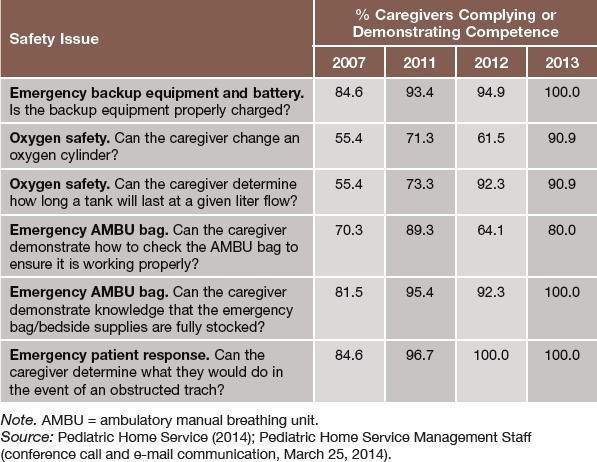
In 2006, PHS conducted a survey to assess in-home caregiver emergency preparedness. The survey included assessments of caregivers' essential skills and knowledge relating to equipment, oxygen safety and use, emergency resuscitation bag function and use, and emergency response procedures. Although caregivers were found to be skilled in routine daily care, there was a demonstrated need for additional education and training, particularly in oxygen use and safety. As a result, PHS developed the Stop, Take Inventory, Assess, Review (STAR) Kit—education materials and tools designed to enhance patient safety in the home. The kit includes informational DVDs, safety checklists and reminders, troubleshooting guides, equipment tags, and an emergency action plan. PHS gave the STAR Kit free to PHS families, home care providers, and referring physicians. The kit also became part of PHS's education program. A follow-up survey in 2007 demonstrated marked improvement, but PHS believed even more could be done. After elements of the program were adjusted, survey results in 2011 indicated even greater improvement. In 2013, PHS achieved improvement across the board (PHS Management Staff, personal communication, March 25, 2014). See Table 5.
Table 5.
Results of Stop, Take Inventory, Assess, Review (STAR) Kit to Improve Patient Safety in the Home
PHS's care process has also contributed to good outcomes on other measures:
Infection control. In the third quarter of 2013, PHS documented a central line–associated bloodstream infection (CLABSI) rate of only 0.41 per 1,000 catheter-days, despite PHS patients being very ill and having complex catheter treatments. A national study of pediatric CLABSI rates within HHAs associated with children's hematology/oncology centers found a mean CLABSI rate of 0.54 per 1,000 catheter-days (Rinke et al., 2013).
Accuracy. To assure that its patients receive accurate supplies, PHS tracks shipping data and has achieved consistently over 98% accuracy between January 2011 and December 2013.
Patient satisfaction. An average of 98.5% of PHS families indicated they were “satisfied or very satisfied” with the overall quality of care and services in 2012. The satisfaction improved to 100% in 2013. New patients are surveyed within the first month of receiving care, and ongoing patients yearly.
Responsiveness. Between 2 and 3 minutes is the average length of time it takes for a PHS on-call clinician to respond to a phone call, according to data gathered between October 2012 and September 2013 (Pediatric Home Service, 2014; PHS Management Staff, Personal Communication, March 25, 2014).
Cleveland Clinic Infusion Pharmacy at Home: Keeping Patient Satisfaction High
Cleveland Clinic Infusion Pharmacy at Home provides medications, nutritional support, infusion pumps and supplies, and infusion equipment education to home healthcare patients diagnosed with a variety of conditions in an eight-state service area. Working in most cases with the Cleveland Clinic's on-site Medicare-certified HHA, the infusion pharmacy team starts educating the patient about infusion therapy during the inpatient stay and reinforces the education while the patient is at home through on-call services and home visits. Educational materials include step-by-step instructions with pictures and places to write notes. Subject matter includes how to manage and administer medications and how to operate infusion equipment. Staff members educate patients about issues such as dehydration, weight gain, and water retention, using teach-back methods to foster understanding and competence (Cleveland Clinic, 2014; E. Hendrickson, personal communication, February 26, 2014). The infusion therapy team also shares information about the patient with the HHA via the Cleveland Clinic's electronic health record. If the patient prefers to work with another agency, the team keeps in touch with that agency via telephone and other means. The key is constant follow-up.
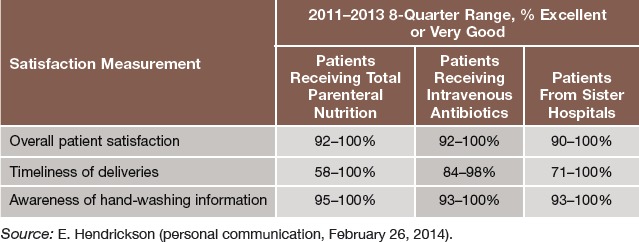
The pharmacy works as part of a Cleveland Clinic multidisciplinary team providing parenteral antibiotic therapy. The team reduced 30-day readmissions of patients receiving this therapy via peripherally inserted central catheter (PICC) lines inserted through the arm from 20.67% (January 2013) to 13.76% (December 2013). For patients with central lines inserted through the chest, who are generally higher risk than patients with PICC lines, readmissions were reduced from 39.9% to 16.6%. The pharmacy also tracks overall patient satisfaction, timeliness satisfaction, and awareness of hand-washing information among these groups of patients: Cleveland Clinic patients receiving total parenteral nutrition (TPN), Cleveland Clinic patients receiving community outpatient parenteral antibiotic therapy, and patients from sister hospitals receiving either TPN or antibiotics. Creating awareness of good hand hygiene techniques among patients transitioning from hospital to home care helps to optimize health outcomes by reducing the risk of infusion catheter-associated infections and complications (Cleveland Clinic, 2014; E. Hendrickson, personal communication, February 26, 2014). See Table 6.
Table 6.
Infusion Pharmacy Patient Satisfaction
Conclusion
Healthcare providers featured in this article demonstrate that effective care transitions to home leading to improved outcomes just don't happen; they are the result of rigorous planning and implementation of evidence-based interventions. Effective transitions occur when referring and discharging providers demonstrate accountability for safeguarding the patient's welfare beyond the time that the patient is in their direct care. They assume responsibility to assess the patient's needs and meaningfully participate in the planning to assure that their risks are mitigated and their needs met by the next direct care provider.
Healthcare providers are moving urgently to create better transitions and outcomes; for this reason, the emphasis is on rapid cycle innovation rather than research. Fortunately, a solid base of research has been created for providers to innovate upon, and effective innovations will optimize health outcomes while having a positive impact on financial results.
Future of Home Health
Figure.

No caption available.
The Alliance for Home Health Quality and Innovation has announced the Future of Home Health Project. It is a research-based strategic planning for the future of home healthcare. They want to hear your ideas. Visit the future of Home Health website at: http://ahhqi.org/home-health/future-project and send your ideas tofutureofhh@ahhqi.org
REFERENCES
- Agency for Healthcare Research and Quality. (2010). Statistical Brief #8:. Healthcare Cost and Utilization Project (HCUP). Retrieved from http://www.hcup-us.ahrq.gov/reports/statbriefs/sb89.jsp [PubMed]
- Agency for Healthcare Research and Quality. (2012). Hospital readmission rates higher for chronic conditions. Retrieved from http://archive.ahrq.gov/news/newsroom/news-and-numbers/030712.html
- Berry D., Costanzo D. M., Elliott B., Miller A., Miller J. L., Quackenbush P., Su Y. P. (2011). Preventing avoidable hospitalizations. Home Healthcare Nurse, 29(9), 540–549. [DOI] [PubMed] [Google Scholar]
- Boston University Medical Center. (2003). Project RED. Retrieved from http://www.bu.edu/fammed/projectred/
- Broderick A., Steinmetz V. (2013). Centura Health at Home: Home telehealth as the standard of care. Commonwealth Fund. Retrieved from http://www.commonwealthfund.org/publications/case-studies/2013/jan/telehealth-centura [Google Scholar]
- Centers for Medicare & Medicaid Services. (2013). New data shows Affordable Care Act reforms are leading to lower hospital readmission rates for Medicare beneficiaries. Retrieved from http://blog.cms.gov/2013/12/06/new-data-shows-affordable-care-act-reforms-are-leading-to-lower-hospital-readmission-rates-for-medicare-beneficiaries/
- Cleveland Clinic. (2014). Infusion pharmacy at home. Retrieved from http://my.clevelandclinic.org/connected-care/services/home-infusion-pharmacy.aspx
- Coleman E. A., Parry C., Chalmers S., Min S. J. (2006). The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine, 166(17), 1822–1828. [DOI] [PubMed] [Google Scholar]
- Counsell S. R., Callahan C. M., Buttar A. B., Clark D. O., Frank K. I. (2006). Geriatric Resources for Assessment and Care of Elders (GRACE): A new model of primary care for low-income seniors. Journal of the American Geriatrics Society, 54(7), 1136–1141. [DOI] [PubMed] [Google Scholar]
- Coye M. J., Haselkorn A., DeMello S. (2009). Remote patient management: Technology-enabled innovation and evolving business models for chronic disease care. Health Affairs, 28(1), 126–135. [DOI] [PubMed] [Google Scholar]
- Illinois Transitional Care Consortium. (2010). The Bridge Model. Retrieved from http://www.transitionalcare.org/the-bridge-model
- Johns Hopkins. (2012). Guided Care. Retrieved from http://www.guidedcare.org
- Kutner M., Greenberg E., Jin Y., Paulsen C. (2006). The Health Literacy of America's Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006-483). Washington, DC: National Center for Education Statistics. [Google Scholar]
- Naylor M. D., Brooten D. A., Campbell R. L., Maislin G., McCauley K. M., Schwartz J. S. (2004). Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatrics Society, 52(5), 675–684. [DOI] [PubMed] [Google Scholar]
- Naylor M. D., Sochalski J. A. (2010). Scaling up: Bringing the transitional care model into the mainstream. Commonwealth Fund, 103, 1–12. [PubMed] [Google Scholar]
- Pediatric Home Service. (2014). PHS in-home healthcare statistics. Retrieved from http://www.pediatrichomeservice.com/about-us-outcome.php
- Project BOOST—: Better Outcomes for Older Adults through Safe Transitions. (2010). Implementation guide to improve care transitions. Retrieved from http://www.hospitalmedicine.org/BOOST/
- Rinke M. L., Bundy D. G., Milstone A. M., Deuber K., Chen A. R., Colantuoni E., Miller M. R. (2013). Bringing central line-associated bloodstream infection prevention home: CLABSI definitions and prevention policies in home health care agencies. Joint Commission Journal on Quality and Patient Safety, 39(8), 361–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevin C., Evdokimoff M., Sobolewski S., Taylor J., Rutherford P., Coleman E. A. (2013). How-to Guide: Improving Transitions From the Hospital to Home Health Care to Reduce Avoidable Rehospitalizations. Cambridge, MA: Institute for Healthcare Improvement; Retrieved from http://www.ihi.org/resources/Pages/Tools/HowtoGuideImprovingTransitionsfromHospitaltoHomeHealthCareReduceAvoidableHospitalizations.aspx [Google Scholar]
- Su Y., Miller A., Miller J., Kamin L., Loganathan S., Bennis S., ..., Flannery K. (2011). Improving care transitions and reducing acute care hospitalizations: New Jersey Care Transitions Project home health experience. Remington Report, May/June 2011, 8–13. [Google Scholar]


