Abstract
Hematemesis is a rare manifestation of a ruptured bronchial artery aneurysm (BAA) in the mediastinum. It is difficult to diagnose a ruptured BAA presenting as hematemesis, because it can be confused with other diseases, such as Boerhaave’s syndrome, variceal disease, or a perforated ulcer. In this report, we describe a case of BAA resulting in hematemesis and mediastinal hemorrhage.
Keywords: Mediastinum, Bronchial arteries, Aneurysm, Hematemesis, Esophagus
CASE REPORT
A 55-year-old man presented at our emergency department with sudden-onset sharp chest pain that had started two hours previously. He also complained of progressive swelling and bruising on his neck, and the development of dysphagia and dyspnea over the previous two hours.
He had a history of admission with spontaneous hemothorax seven years previously, and at that time, despite several work-ups for hemothorax, its origin was not found. He was discharged after blood evacuation by closed thoracostomy. Other than this incident, he had hypertension but no history of gastrointestinal or bleeding disorders.
Upon arrival at the emergency department, he appeared pale, but his vital signs were stable. Extensive neck swelling was observed, as well as bruising on the neck and upper chest. During the examination, he suddenly vomited bright red blood with food material three times, and approximately a quarter-cup of blood was generated on each occasion. His dyspnea worsened and oxygen saturation fell abruptly. Endotracheal intubation was performed and a nasogastric tube was inserted. Fresh blood was evacuated and melena was visible in the rectum. His initial hemoglobin level was 12.6 g/dL. Other laboratory tests, including cardiac markers and his coagulation profile, were within their normal ranges. An electrocardiogram showed sinus rhythm.
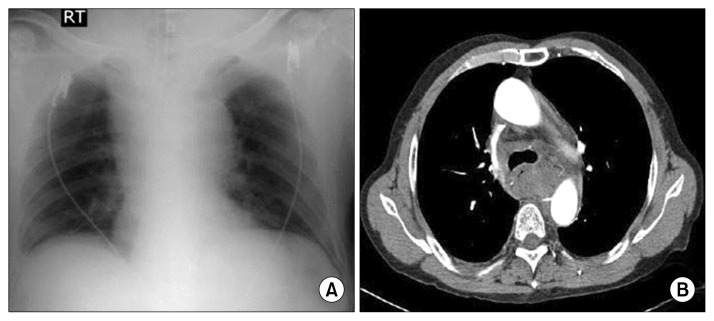
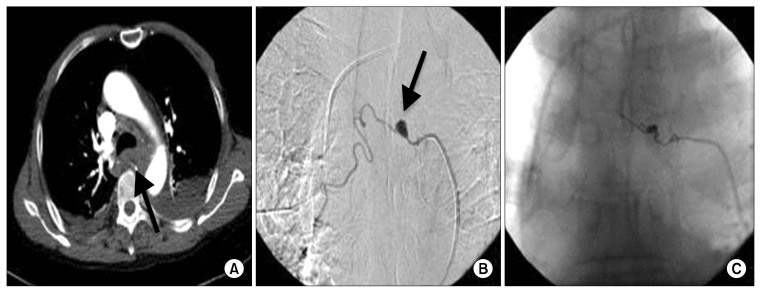
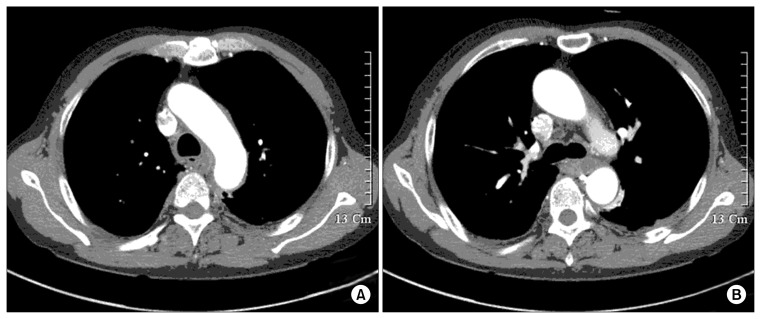
An initial chest X-ray (Fig. 1A) showed right superior mediastinal widening. Emergency thoracic computed tomography (CT) angiography (Fig. 1B) revealed extensive non-enhancing soft tissue lesions in the posterior mediastinum and neck, which were suspected to be hematomas. Emergency gastroscopy showed many blood clots but no definite focus of gastrointestinal bleeding, such as an ulcer, mass, or perforation. Instead, gastroscopy showed extrinsic esophageal compression. Since the patient was hemodynamically stable, conservative management was adopted in the intensive care unit. Followup CT on the third day post-admission showed a focal aneurysm in the right bronchointercostal trunk (Fig. 2A). Subsequent selective bronchial arteriography revealed a 1-cm aneurysm in the right bronchial artery (Fig. 2B). No leakage of contrast medium from the aneurysm was observed by CT or arteriography. Since the aneurysm was considered to be the cause of the hematemesis and mediastinal hemorrhage, we decided to perform embolization to prevent recurrence. The right bronchial artery was subsequently embolized with four microcoils (VortX-18; Boston Scientific Co., Marlborough, MA, USA) and 33% glue (Fig. 2C), and repeat CT showed that the mediastinal hematoma had nearly disappeared (Fig. 3). Follow-up gastroscopy revealed no specific findings other than gastritis. The patient was discharged without complications. Over the course of one year of follow-up, he remained well, with no signs of recurrence.
Fig. 1.
(A) Chest X-ray revealing right superior mediastinal widening. (B) Chest computed tomography imaging showing soft tissue lesions in the posterior mediastinum.
Fig. 2.
(A) A follow-up chest computed tomography image showing a focal aneurysm in the right bronchointercostal trunk. Selective bronchial arteriography (B) before (arrow) and (C) after transcatheter arterial embolization with coil and glue.
Fig. 3.
(A, B) Repeat computed tomography performed six days after the embolization, showing that the mediastinal hematoma had quickly disappeared.
DISCUSSION
Acute spontaneous mediastinal hemorrhage is rare but life-threatening condition [1]. Spontaneous mediastinal hemorrhage can develop as a result of trauma, aortic dissection, the Valsalva maneuver, or iatrogenic procedures [2]. The rupture of a bronchial artery aneurysm (BAA) is also known to result in mediastinal hemorrhage. When a BAA ruptures into the mediastinum, most patients present with chest pain, hemothorax, or hemomediastinum [3]. Rarely, a BAA may rupture into the esophagus, resulting in hematemesis [4]. Furthermore, if hematemesis is a prominent symptom of BAA rupture, it can be confused with Boerhaave’s syndrome, variceal disease, or a perforated ulcer. To the best of our knowledge, only three cases of BAA presenting with hematemesis have been reported in the literature [4–6]. In one case, a pinhole connection between the aneurysm and esophagus was found during an endoscopic examination [6], but in the present case, no evidence of communication was found between the aneurysm and the esophagus.
We first suspected that the mediastinal hemorrhage and hematemesis were caused by the perforation of an esophageal ulcer, but repeated gastroscopy showed a normal esophagus. No evidence of any gastrointestinal disease was revealed by gastroscopy and CT. The only abnormal finding was the finding of a BAA without evidence of extravasation three days after the onset of symptoms. After ruling out the possibility of mediastinal hematoma, the BAA was the only remaining possible source of the mediastinal hemorrhage. Since the BAA was regarded as the source of the mediastinal hemorrhage and hematemesis, it was embolized to avoid recurrence.
The treatment of a ruptured BAA depends on the patient’s hemodynamic status and the presence of cardiorespiratory compromise. If the patient is hemodynamically stable, endovascular embolization is considered to be the first-line management strategy, and surgery should only be considered when embolization is contraindicated, as in patients allergic to contrast medium or when a medullary artery is involved [1].
In patients presenting at an emergency department with hematemesis and mediastinal hemorrhage, the possibility of a ruptured BAA should be investigated.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Mizuguchi S, Inoue K, Kida A, et al. Ruptured bronchial artery aneurysm associated with bronchiectasis: a case report. Ann Thorac Cardiovasc Surg. 2009;15:115–8. [PubMed] [Google Scholar]
- 2.Gomelsky A, Barry MJ, Wagner RB. Spontaneous mediastinal hemorrhage: a case report with a review of the literature. Md Med J. 1997;46:83–7. [PubMed] [Google Scholar]
- 3.Seo YH, Kwak JY. Spontaneous hemomediastinum and hemothorax caused by a ruptured bronchial artery aneurysm. Korean J Thorac Cardiovasc Surg. 2011;44:314–7. doi: 10.5090/kjtcs.2011.44.4.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tringali S, Tiffet O, Berger JL, Cuilleret J. Bronchial artery aneurysm disguised as a leiomyoma of the esophagus. Ann Thorac Surg. 2002;73:632–3. doi: 10.1016/S0003-4975(01)03121-6. [DOI] [PubMed] [Google Scholar]
- 5.Shaer AH, Bashist B. Computed tomography of bronchial artery aneurysm with erosion into the esophagus. J Comput Assist Tomogr. 1989;13:1069–71. doi: 10.1097/00004728-198911000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Fukunaga A, Okushiba S, Ohno K, et al. Mediastinal bronchial artery aneurysm with hematemesis. Dis Esophagus. 2003;16:328–31. doi: 10.1111/j.1442-2050.2003.00360.x. [DOI] [PubMed] [Google Scholar]