Abstract
Upper extremity surgery is commonly performed under regional anesthesia. The advent of ultrasonography has made performing upper extremity nerve blocks relatively easy with a high degree of reliability. The proximal approaches to brachial plexus block such as supraclavicular plexus block, infraclavicular plexus block, or the axillary block are favored for the most surgical procedures of distal upper extremity. Ultrasound guidance has however made distal nerve blocks of the upper limb a technically feasible, safe and efficacious option. In recent years, there has thus been a resurgence of distal peripheral nerve blocks to facilitate hand and wrist surgery. In this article, we review the technical aspects of performing the distal blocks of the upper extremity and highlight some of the clinical aspects of their usage.
Keywords: Distal, median, musculocutaneous, peripheral nerve blocks, radial, ulnar, ultrasound
Introduction
Wrist and hand surgery are commonly performed under regional anesthesia.[1,2] The advent of ultrasonography has made performing upper extremity nerve blocks relatively easier and increased their efficacy.[3] More proximal approaches such as supraclavicular plexus block, infraclavicular plexus block, or the axillary block are usually favored for surgical procedures of distal upper extremity.[4,5,6] Ultrasound guidance has however made distal nerve blocks of the upper limb a technically feasible, safe, and efficacious option.[7,8,9] In recent years, there has thus been a resurgence of distal peripheral nerve blocks to facilitate hand and wrist surgery.[10] In this article, we review the technical aspects of performing the distal blocks of the upper extremity and highlight some of the clinical aspects of their usage.
Potential Benefits of Distal Nerve Blocks of Upper Extremity
A more distal approach involving the peripheral nerves of the upper extremity (radial, median, ulnar and musculocutaneous nerves) may offer several benefits. These include the following:
Distal approaches to upper extremity block in general lie away from critical, more central structures such as the pleura, subclavian or axillary artery and the phrenic nerve and thus avoid the risk of inadvertent needle trauma to these structures.
Distal peripheral nerve blocks allow preservation of proximal muscle function of the upper limb. The inability to use the affected limb due to the motor block of proximal and distal musculature has been shown to reduce patient satisfaction.[11] A recent randomized controlled trial comparing ultrasound guided supraclavicular plexus block with distal peripheral nerve blocks for outpatient hand surgery showed better strength preservation and greater patient satisfaction with distal blocks.[12]
In conjunction with a proximal brachial plexus block (infraclavicular), distal nerve blocks of the upper limb have been shown to hasten block onset times and improve block consistency.[10]
Combining a proximal brachial plexus block using a short acting local anesthetic and distal nerve blocks using a longer acting local anesthetic agent may prolong the analgesic component of the block while minimizing proximal muscle dysfunction.[13]
Preservation of motor strength may also allow the patients to move affected digits when instructed to do so during the surgery. This may be vital during certain types of hand surgeries.
Potential Limitations of Distal Nerve Blocks of Upper Extremity
The cutaneous innervation of the upper arm is provided by the musculocutaneous nerve, medial cutaneous nerve of the arm, posterior cutaneous nerve of the arm, and intercostobrachial nerve. Distal nerve blocks will therefore not prevent tourniquet pain in an unsedated patient.
Nerves originating proximally in the axilla such as the medial cutaneous nerve of the forearm and the musculocutaneous nerve (which gives rise to the lateral cutaneous nerve of the forearm) contribute to the cutaneous innervation of the forearm. Thus, distal nerve blocks may not always be sufficient for surgical procedures on the forearm.
A distal approach to nerve block for the upper limb requires blockade of multiple nerves. This, therefore, involves multiple injections that may cause more patient discomfort.
The peripheral nerves can be anisotropic, and scanning for them can be challenging initially. Experimenting with different degrees of probe tilt and scanning positions to find the best view is helpful.
Recommended Applications of Distal Block
Distal blocks of the upper limb may be useful in the following circumstances:
Primary surgical anesthesia: For superficial or minor surgery of the distal upper limb that does not require the use of an arm tourniquet or profound muscle relaxation.
Secondary analgesia: To supplement a general anesthetic or a brachial plexus block performed using short-acting agents. In this instance, increased vigilance is required during block performance due to the reduced ability of the patient to report paresthesia or pain from neural trauma. Strategies to increase safety include the use of both peripheral nerve stimulator (PNS) and ultrasound,[14,15] and injection pressure monitoring.[16,17]
As rescue techniques for incomplete brachial plexus blocks.
Required Equipment and Ergonomics
In general the following are required to perform the blocks:
Appropriate anesthetic equipment and personnel for sedation, monitoring, and oxygenation.
Ultrasound machine with high-frequency linear array transducer (10-15 MHz).
Sterile ultrasound probe cover or Tegaderm™ (3M, St. Paul, MN, USA) dressing.
Sterile ultrasound gel.
Sterile skin preparation (2% chlorhexidine or other appropriate disinfectant).
Local anesthetic for skin infiltration (usually 0.5-1 ml 2% lignocaine). It must be kept in mind that this would increase the number of needle pricks patient receives.
A 22 G, 50 mm short-bevel regional anesthesia block needle.
Sterile gloves.
Local anesthetic: Usually a volume of 3-5 ml suffice for each nerve. The objective is to achieve a circumferential spread of the local anesthetic around the nerve. While using a lower concentration (such as 0.25% bupivacaine) may suffice for analgesia, the duration may also be limited. Using a higher concentration (such as 0.5% bupivacaine) provides an anesthetic block, with a longer duration. Lignocaine may be used when a rapid onset is desired.
Ergonomics: We recommend that the operator stand on the side being blocked, with the ultrasound machine on the opposite side of the patient. This maintains an in-line orientation between the operator, the injection site, and the ultrasound screen.
Specific Distal Nerve Blocks of the Upper Limb
Musculocutaneous nerve (C5, C6, and C7)
Brief anatomy
This nerve is a branch of the lateral cord of the brachial plexus, arising opposite the lower border of the pectoralis major.[18,19] After penetrating the coracobrachialis muscle, the nerve passes obliquely between the biceps brachii and the brachialis innervating all three muscles, and supplying the elbow joint. It then emerges on the lateral side of the arm, pierces the deep fascia lateral to the tendon of the biceps brachii, and continues into the forearm as the lateral cutaneous nerve of the forearm. A schematic diagram is shown in Figure 1.
Figure 1.
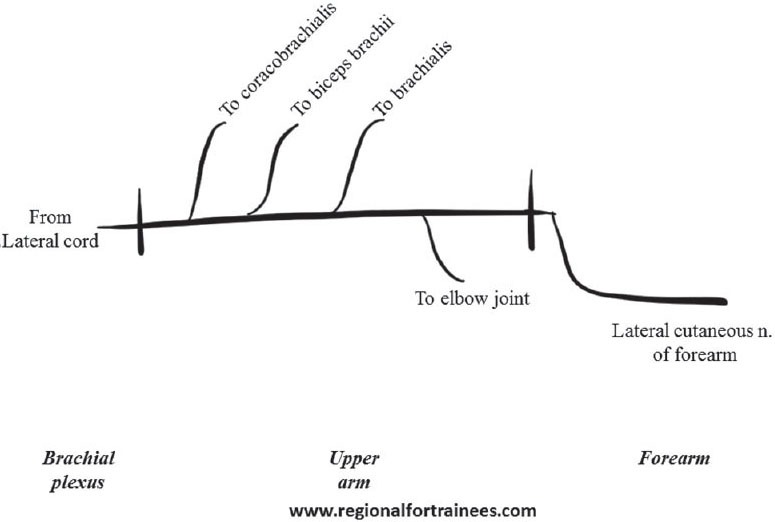
Schematic diagram representing the course of musculocutaneous nerve
Patient position
The patient is positioned supine with the arm being blocked abducted away from the body at a right angle, and extended at the elbow. Alternatively, the abducted arm may be flexed at the elbow [Figure 2].
Figure 2.
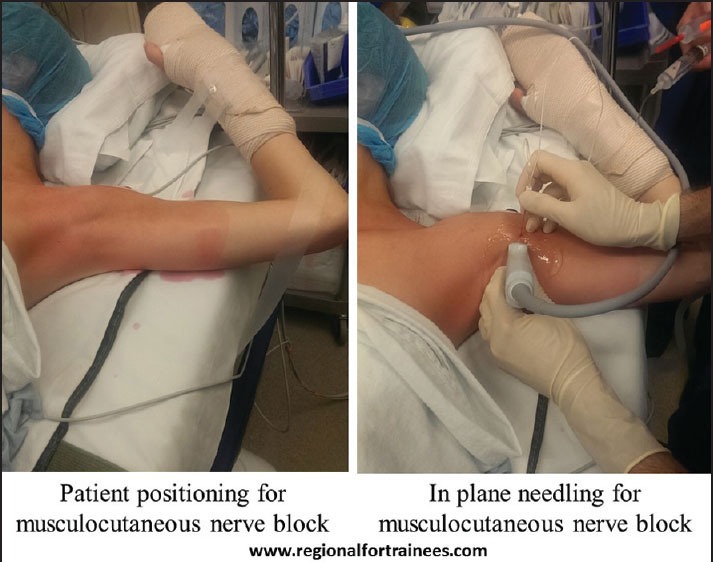
Patient position, scanning technique and in-plane needling for musculocutaneous nerve block
Scanning
A linear transducer is placed at the axilla to identify the axillary artery, above the teres major muscle. The coracobrachialis muscle lateral to the artery, and the biceps brachii further lateral is identified. The musculocutaneous nerve appears as a hyperechoic triangular or oval structure in the fascial plane between coracobrachialis and biceps brachii muscles [Figure 3].
Figure 3.
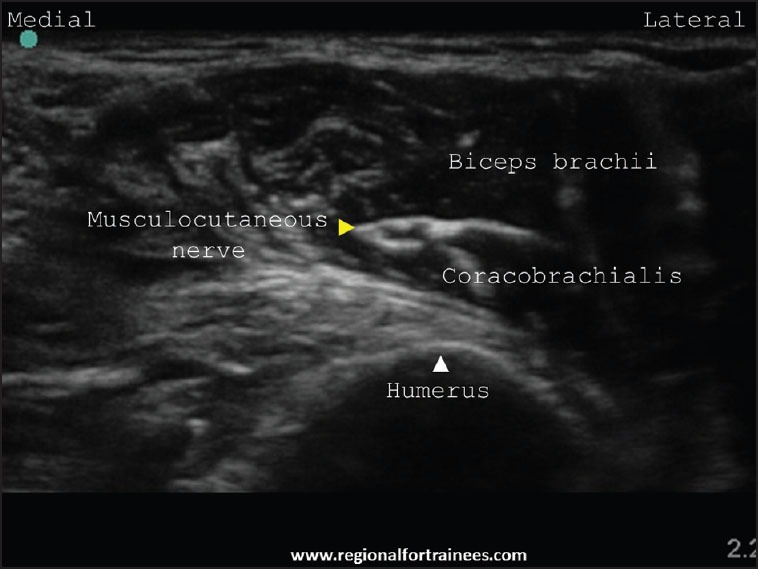
Ultrasound scan of the musculocutaneous nerve
Injection
After raising a skin wheal using local anesthetic, a 22 G, 50 mm short bevel block needle is introduced in-plane in a lateral to medial direction (or out-of-plane depending on operator preference), aiming to enter the fascial plane next to the musculocutaneous nerve. If using a PNS, an evoked motor response constituting elbow flexion is obtained. After negative aspiration, local anesthetic is injected to encircle the nerve. Usually, a volume of 3-5 ml is sufficient for this [Figures 4 and 5].
Figure 4.
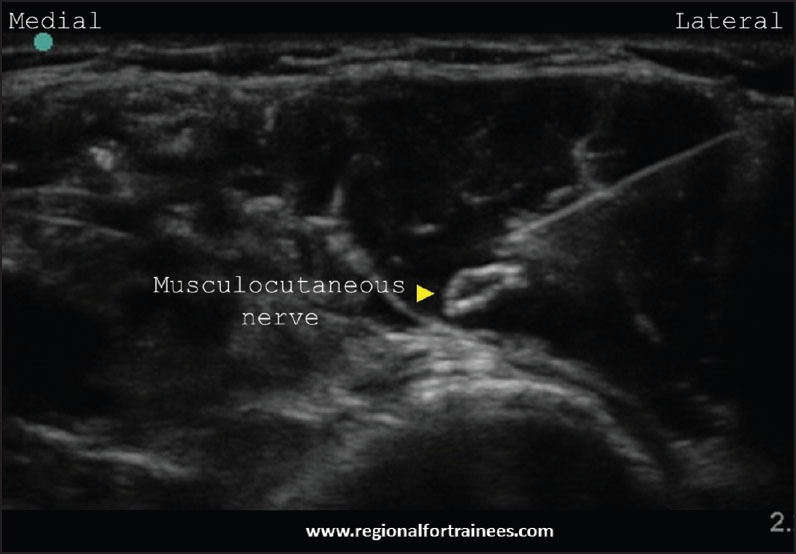
In-plane needling for musculocutaneous nerve
Figure 5.

Musculocutaneous nerve post injection
Radial nerve (C5, C6, C7, C8 and T1)
Brief anatomy
The radial nerve originates from the posterior cord of the brachial plexus (along with the axillary nerve) and enters the posterior compartment of the arm.[18,19,20] It then spirals obliquely over the posterior aspect of the humerus (in the spiral groove) to emerge on the lateral side of the humerus. It then pierces the lateral intermuscular septum to enter the anterior compartment of the arm. Here, it then descends between brachialis and brachioradialis and courses anterior to the lateral epicondyle, where it divides into superficial and deep branches. Figure 6 illustrates a schematic representation of the course and the branches of the radial nerve.
Figure 6.
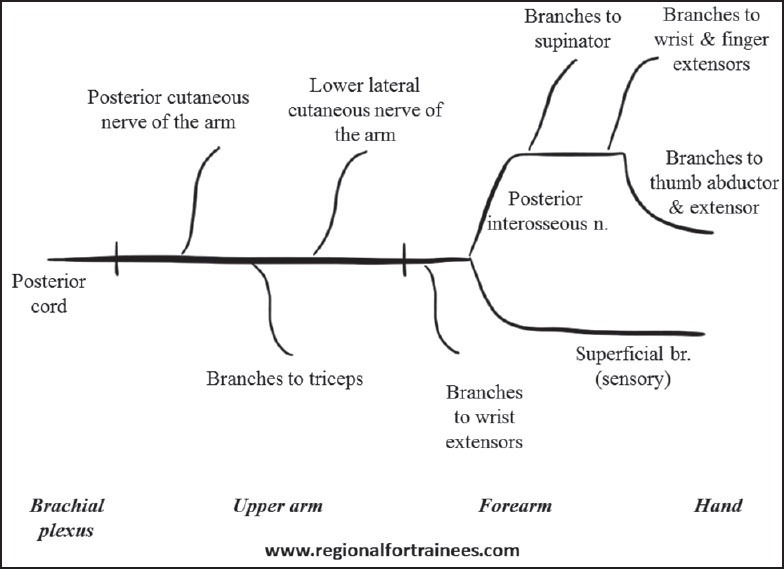
Schematic diagram of the course and branches of the radial nerve
Patient position and scanning technique
The radial nerve may be blocked at the following two positions above the elbow joint:
Just distal to the spiral groove — The arm is the best placed with shoulder adducted and internally rotated, and elbow flexed so that it lies on the chest. This allows the best access to the posterolateral aspect of the humerus [Figure 7]. A linear transducer is placed in the spiral groove to identify the humerus. Upon scanning distally, the radial nerve is usually seen as a triangular hyperechoic structure coming off the humerus [Figure 8a]. Blocking the radial nerve here maximizes the chances of involving both the deep and the superficial branches and is our preferred site of injection.
At the elbow — The patient is positioned supine, with the arm to be blocked kept straight in supination [Figure 7]. At first, the radial nerve is identified as above. On further scanning distally, it flattens out and comes to lie between the biceps and brachioradialis [Figure 8b]. Near the elbow joint, it is seen to branch out into its superficial and deep branches [Figure 8c]. This site may be chosen for simplicity, as the median nerve may also be blocked at the same level by moving the probe medially to identify the latter. However, care must be exercised to choose a point of injection before the bifurcation of the radial nerve to avoid missing one of the branches.
Figure 7.
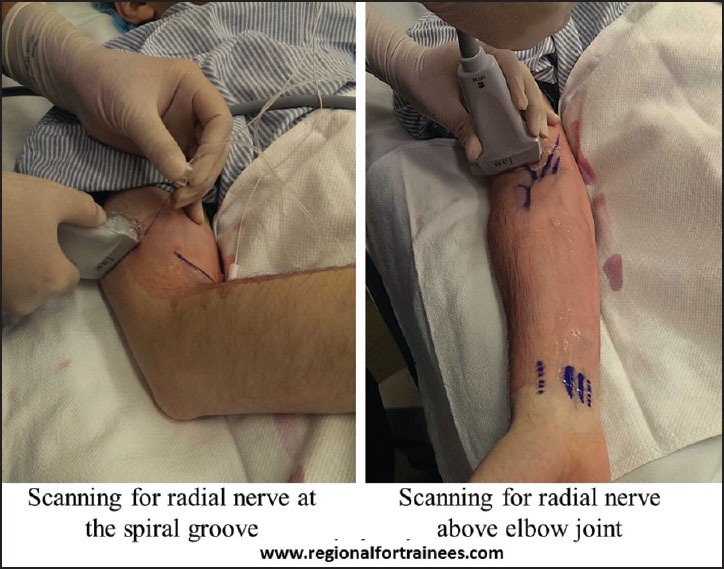
Patient position and scanning technique for radial nerve block
Figure 8a.

Ultrasound scan of the radial nerve at the humeral spiral groove
Figure 8b.
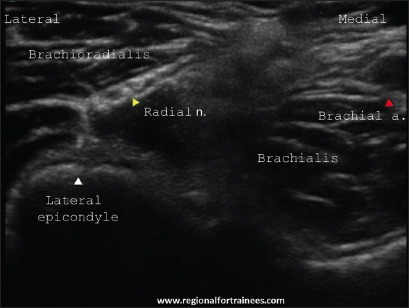
Ultrasound scan of the radial nerve between the biceps and brachioradialis
Figure 8c.
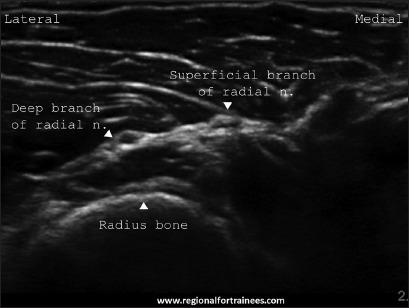
Ultrasound scan of the radial nerve at division into two branches: Superficial and deep
Injection
After raising a skin wheal using local anesthetic, a 22 G, 50 mm short bevel block needle is introduced in-plane (or out-of-plane) aiming to enter the fascial plane next to the radial nerve. If using a PNS, an evoked motor response constituting thumb and finger extension is obtained. An injection of 3-5 ml local anesthetic is made after negative aspiration to encircle the radial nerve [Figures 9, 10a and b]. Injection must not be made too close to the spiral groove to avoid pressure induced nerve damage.
Figure 9.
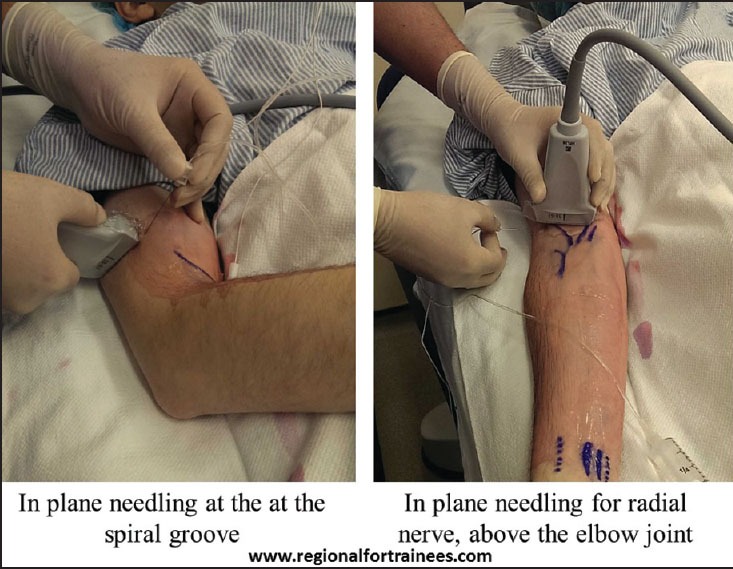
In-plane needling for radial nerve block
Figure 10a.

In-plane needling for radial nerve near spiral groove
Figure 10b.
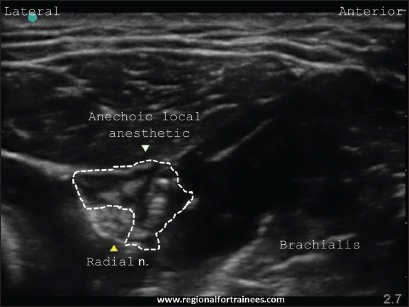
Radial nerve after injection
Ulnar nerve (C8, T1)
Brief anatomy
The ulnar nerve originates from the medial cord of the brachial plexus.[18,19,20] It descends in a subcutaneous plane, initially medial to the brachial artery, to emerge behind the medial epicondyle that seats the nerve. It enters the anterior (flexor) compartment of the forearm between the humeral and ulnar heads, lying under the aponeurosis of flexor carpi ulnaris. In the upper third of the forearm, the nerve is separated from the ulnar artery, but more distally it comes to lie adjacent to the medial side of the artery. This relationship is helpful in identifying the nerve. Figure 11 illustrates a schematic representation of the course and the branches of the ulnar nerve.
Figure 11.
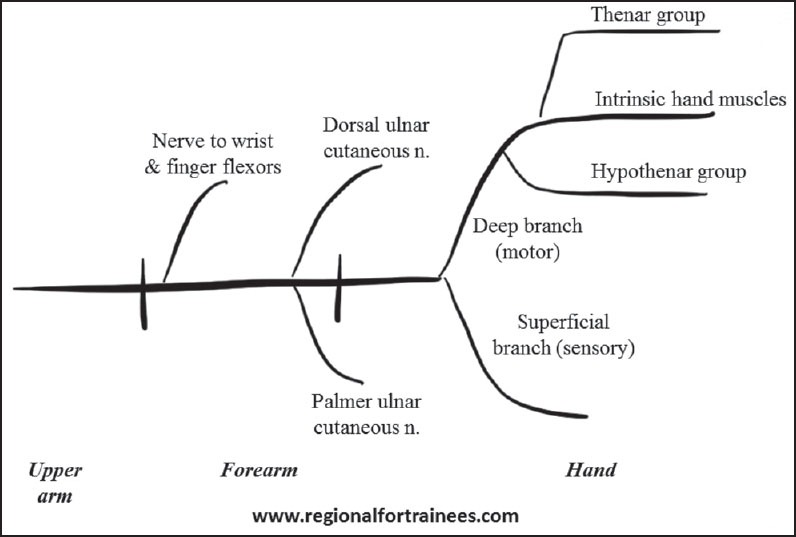
Schematic diagram of the course and branches of the ulnar nerve
Patient position and scanning technique
The ulnar nerve may be blocked at the following two positions:
The mid-humeral level — The patient is positioned supine with the arm being blocked abducted away from the body at a right angle, and extended (or flexed) at the elbow [Figure 12]. A linear transducer is placed in the axilla to identify the axillary artery. The ulnar nerve may be identified medial to it. As the artery is traced distally, the ulnar nerve is visible as a hyperechoic structure superficial and medial to the brachial artery at the mid-humeral level [Figure 13]. Blocking the ulnar nerve here covers the forearm muscles well and is the preferred approach for procedures on the forearm.
At mid-forearm level — The patient is positioned supine, with the arm being blocked kept straight and supinated [Figure 14]. A linear transducer is placed just above the wrist, on its medial aspect to identify the ulnar artery. Upon scanning proximally, the ulnar nerve is usually seen as an oval hyperechoic structure immediately medial to the artery [Figure 15a]. On further proximal scan up to the mid-forearm, the nerve is seen moving further away (medially) from the ulnar artery, to lie between the flexor carpi ulnaris above and flexor digitorum profundus deeper [Figure 15b]. Blocking the ulnar nerve here does not cover the forearm muscles well and is therefore primarily suitable for procedures on the hand.
Figure 12.
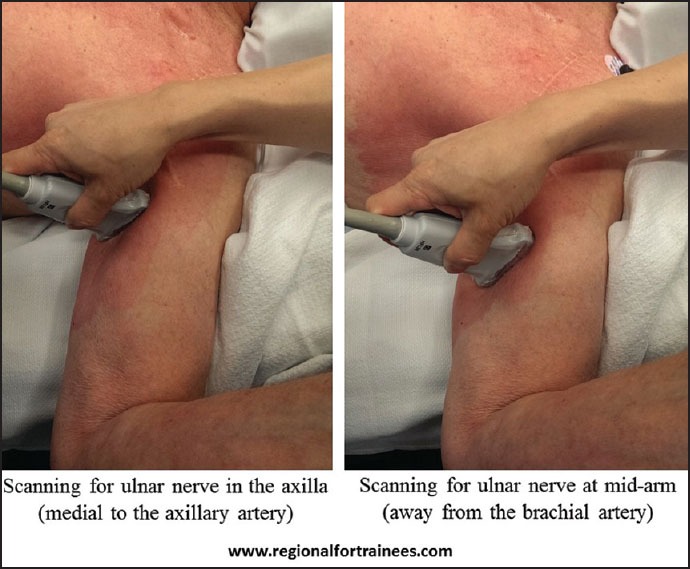
Scanning for the ulnar nerve at mid-humerus
Figure 13.
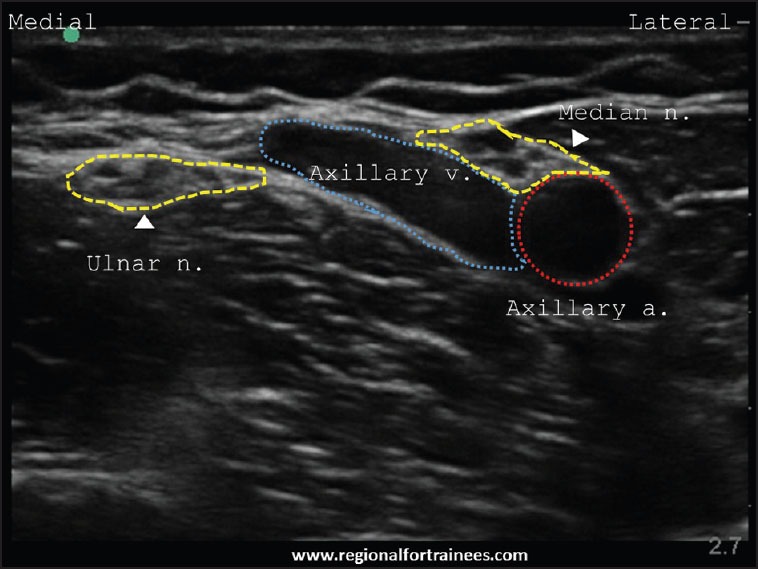
Ultrasound image of ulnar nerve at mid-humerus level. Ulnar nerve is typically seen away from the brachial artery
Figure 14.

Patient position and scanning technique for ulnar nerve block
Figure 15a.
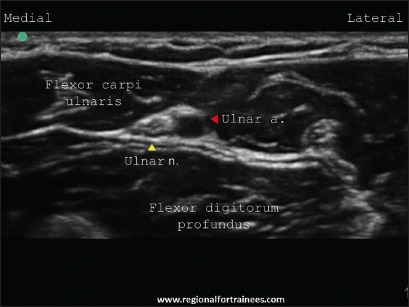
Ultrasound scan of the ulnar nerve next to the ulnar artery (distally)
Figure 15b.
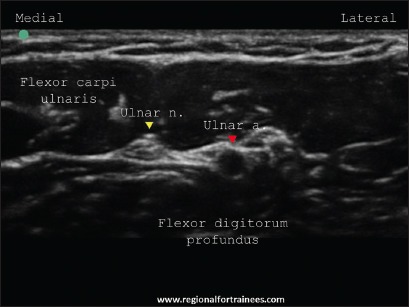
Ultrasound scan of the ulnar nerve away from the ulnar artery (proximally)
Injection
After raising a skin wheal using local anesthetic a 22 G, 50 mm short bevel block needle is introduced in-plane (or out-of-plane) aiming to enter the fascial plane next to the ulnar nerve. If using a PNS, an evoked motor response constituting thumb adduction and ring finger flexion is obtained. An injection of 3-5 ml local anesthetic is made after negative aspiration to cover the nerve circumferentially [Figures 16, 17a and b].
Figure 16.

In-plane needling for ulnar nerve block
Figure 17a.
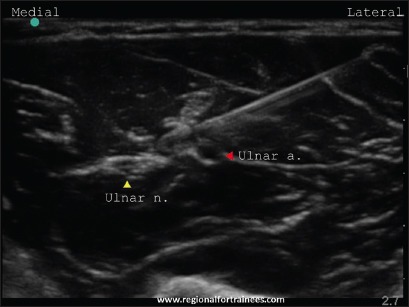
In-plane needling for ulnar nerve at mid-forearm
Figure 17b.
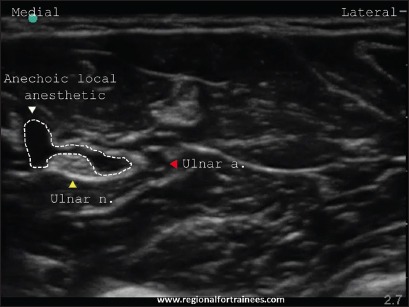
Ulnar nerve at mid-forearm after injection
Median nerve (C5, C6, C7, C8 and T1)
Brief anatomy
The median nerve is formed by the lateral root of median (from the lateral cord) and the medial root of median nerve (from the medial cord) of the brachial plexus.[18,19,20] In the arm, it passes vertically downward lateral to the brachial artery. It crosses brachial artery anteriorly (or rarely posteriorly) to lie medial to it, just above the elbow joint. Here, it lies between biceps brachii and brachialis. In the forearm, passes between the two heads of pronator teres and then travels between flexor digitorum superficialis and flexor digitorum profundus. Figure 18 illustrates a schematic representation of the course and the branches of median nerve.
Figure 18.
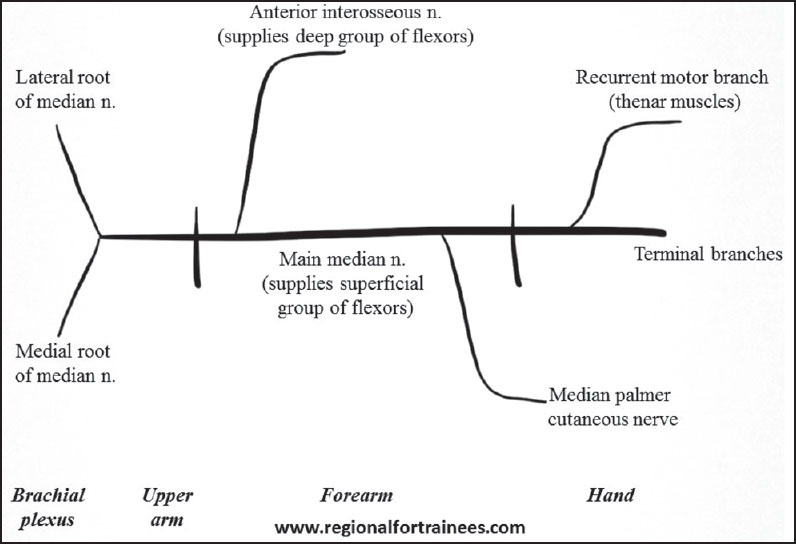
Schematic diagram of the course and branches of the median nerve
Patient position and scanning technique
The median nerve may be blocked at the following positions:
The mid-humeral level — The patient is positioned supine with the arm being blocked abducted away from the body at a right angle, and extended (or flexed) at the elbow [Figure 19]. A linear transducer is placed in the axilla to identify the axillary artery, with median nerve commonly located lateral to it. Upon distal scanning, the median nerve remains adjacent to the artery while the ulnar nerve moves further medially away from the artery [Figure 13]. This injection point allows both median and ulnar nerves to be blocked at the same level.
Above the elbow joint — The patient is positioned supine, with the arm being blocked kept straight and supinated [Figure 20]. A linear transducer is placed over the cubital fossa to identify the brachial artery. The median nerve can be seen as a round to oval hyperechoic structure medial or posterior to the brachial artery [Figure 21a]. The nerve can be blocked here.
At the mid-forearm — The patient is positioned supine, with the arm being blocked kept straight and supinated [Figure 20]. A linear transducer is placed on the ventral aspect of the mid-forearm, where the median nerve is visible in the fascial plane between the flexor digitorum superficialis and flexor digitorum profundus. Another easy way to identify this plane is to identify the ulnar nerve at mid-forearm first (as described above). Upon moving the transducer laterally at this level, the median nerve can be identified in the fascial plane between the flexor digitorum superficialis and flexor digitorum profundus [Figure 21b].
Figure 19.

Scanning for median nerve at the mid-humerus level
Figure 20.
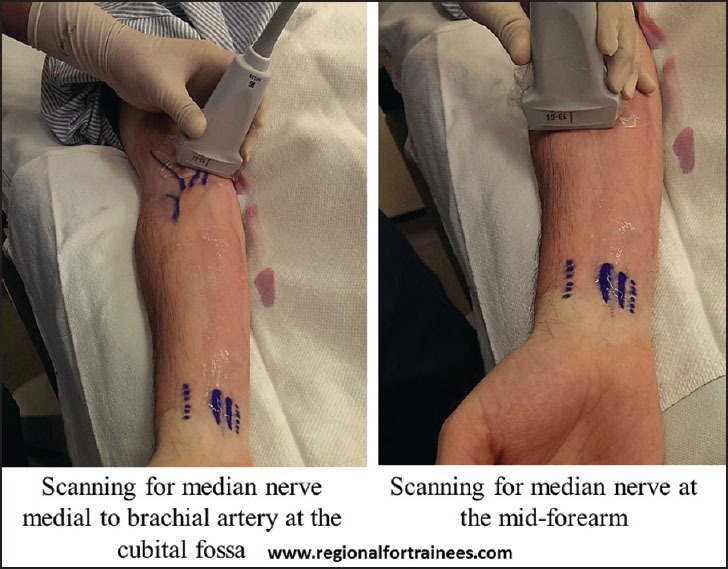
Patient position and scanning technique for median block at the cubital fossa and at the mid-forearm
Figure 21a.
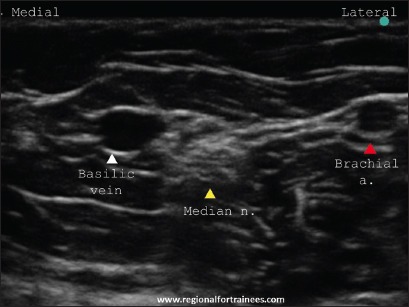
Ultrasound scan of the median nerve at the cubital fossa
Figure 21b.
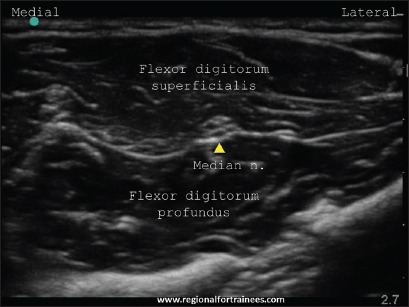
Ultrasound scan of the median nerve at the mid-forearm
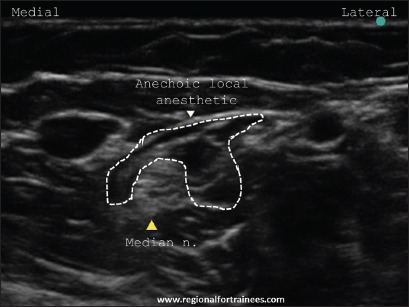
Injection
After raising a skin wheal using local anesthetic, a 22 G, 50 mm short bevel block needle is introduced in-plane (or out-of-plane) and aimed at the fascial plane next to the median nerve. Care is exercised not to puncture the brachial artery, which may be crossed from above or below to access the median nerve [Figures 22a and b]. If using a PNS, an evoked motor response constituting finger flexion is obtained. An injection of 3-5 ml local anesthetic is made after negative aspiration to cover the nerve circumferentially [Figures 23a and b].
Figure 22a.

In-plane needle insertion for median nerve block at the cubital fossa
Figure 22b.
Ultrasound image of the median nerve post injection
Figure 23a.

In-plane needle insertion for median nerve block at mid-forearm
Figure 23b.
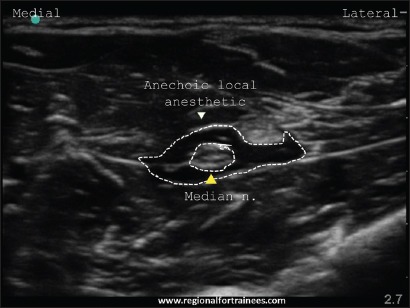
Ultrasound image of the median nerve at mid-forearm postinjection
Medial antebrachial cutaneous nerve or medial cutaneous nerve of the forearm (C8-T1)
Brief anatomy
This nerve is a branch of the medial cord of the brachial plexus, arising medial to the axillary artery. Subsequently it gives a branch that pierces the fascia and supplies the skin over the biceps brachii muscle up to the elbow. The nerve lies medial to the brachial artery at mid-arm level and pierces the brachial fascia along with the basilic vein at the basilic hiatus. It then divides into anterior (volar) and posterior (ulnar) branches supplying the skin over the antero-medial and postero-medial aspect of the forearm respectively.[21,22,23]
Patient position
The patient is positioned supine with arm being blocked abducted away from the body at a right angle, and extended at the elbow. Alternatively, the abducted arm may be flexed at the elbow [Figure 24].
Figure 24.
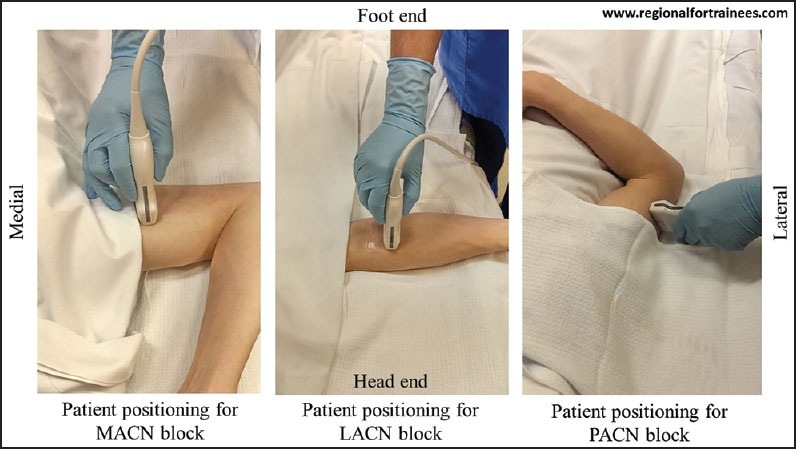
Patient position for medial antebrachial cutaneous nerve, lateral antebrachial cutaneous nerve and posterior antebrachial cutaneous nerve
Scanning
A linear transducer is placed at the mid-arm level (in short axis) to identify the biceps brachii muscle, brachial artery, median nerve (medial to the brachial a.), ulnar nerves (subcutaneous medially) and basilic vein (in the most superficial subcutaneous plane). The medial antebrachial cutaneous nerve (MACN) can be visualized as a hyperechoic oval immediately lateral to the basilic vein [Figure 25a]. Upon a distal scan, it can be seen dividing into its two branches, anterior and posterior [Figure 25b]. While the anterior branch moves laterally, the posterior branch passes under the vein to lie on its ulnar aspect.[24,25]
Figure 25a.
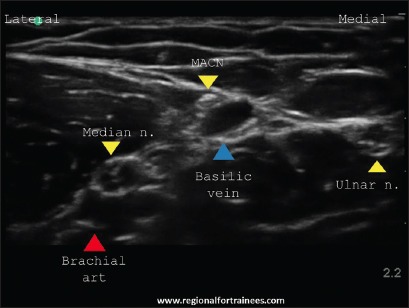
Ultrasound scan of the medial antebrachial cutaneous nerve at the mid-arm level before its division
Figure 25b.
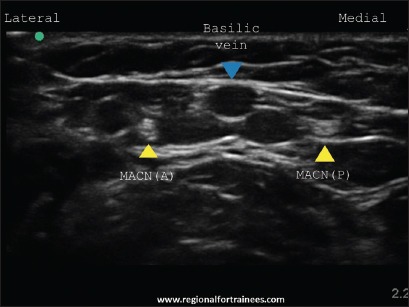
Ultrasound scan of the medial antebrachial cutaneous nerve (MACN) at the mid-arm level after its division (MACN (A) = MACN anterior branch, MACN (P) = MACN posterior branch)
Injection
A 25-27 G hypodermic needle is introduced in-plane in a lateral to medial direction aiming to enter the fascial plane next to the basilic vein. After negative aspiration, 2-3 ml local anesthetic is injected to fill the fascial plane containing the MACN.
Lateral antebrachial cutaneous nerve or lateral cutaneous nerve of the forearm (C5, C6, C7)
Brief anatomy
In the arm, the musculocutaneous nerve pierces the coracobrachialis to descend in the plane between the brachialis and the biceps brachii muscles. After providing motor branches to these muscles, the nerve emerges lateral to the tendon of the biceps brachii muscle at the elbow, pierces the deep fascia distal to the interepicondylar line and continues as the lateral antebrachial cutaneous nerve (LACN). It usually lies medial to the cephalic vein and may divide into anterior (volar) and posterior (ulnar) branches supplying the skin over the antero-lateral and postero-lateral aspect of the forearm respectively.[26,27]
Patient position
The patient is positioned supine with arm being blocked abducted away from the body at a right angle, and extended at the elbow [Figure 24].
Scanning
A linear transducer is placed above the elbow joint (in short axis) to identify the biceps brachii aponeurosis and the biceps tendon [Figure 26a]. The hyperechoic LACN is identified lateral to the tendon, and becomes subcutaneous upon distal scan. Here, it is seen under or medial to the cubital vein [Figure 26b], and is seen dividing into an anterior (volar) and a posterior (ulnar) branch.[28,29]
Figure 26a.

Ultrasound scan of the bicipital aponeurosis above the elbow joint
Figure 26b.
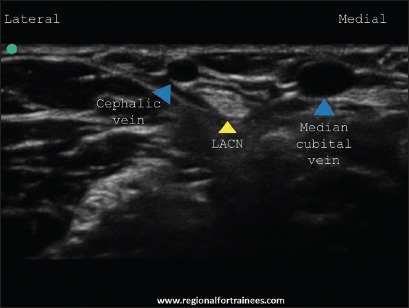
Ultrasound scan of the lateral antebrachial cutaneous nerve just below the elbow joint, where the nerve is located medial to the cephalic vein
Injection
A 25-27 G hypodermic needle is introduced in-plane, in a lateral to medial direction aiming to enter the fascial plane next to the cephalic vein. After negative aspiration, 2-3 ml local anesthetic is injected to fill the fascial plane containing the LACN.
Posterior antebrachial cutaneous nerve or posterior cutaneous nerve of the forearm (C5, C6, C7, C8)
Brief anatomy
After emerging from the spiral groove, the radial nerve pierces the lateral intermuscular septum to enter the anterior compartment of the arm. Along this course, both the inferior lateral cutaneous nerve of the arm and posterior cutaneous nerve of the forearm are given off. Thus, the posterior antebrachial cutaneous nerve (PACN) may be identified at the junction of triceps and brachioradialis in the superficial plane. It divides into an upper branch that supplies the lateral side of lower arm, and a lower branch that supplies the back of the forearm up to the wrist.[18,30]
Patient position
The arm is the best placed with shoulder adducted and internally rotated, and elbow flexed, so that it lies on chest [Figure 24].
Scanning
A linear transducer is placed in the spiral groove (in short axis) to identify the radial nerve [Figure 27a]. Upon distal scanning, small hyperechoic nerve may be seen piercing the triceps to emerge superficially at the junction of the triceps and brachioradialis [Figure 27b]. It divides into an upper and a lower branch [Figure 27c].[28,30]
Figure 27a.
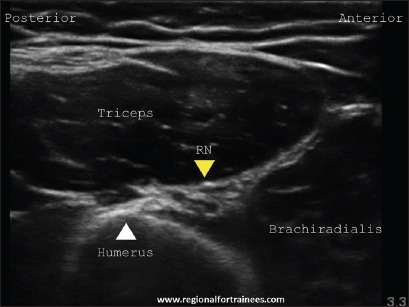
Ultrasound scan of the radial nerve at the spiral groove
Figure 27b.
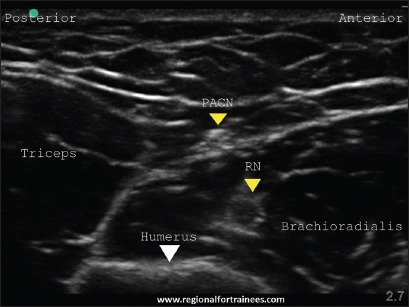
Ultrasound scan of the posterior antebrachial cutaneous nerve just below the spiral groove
Figure 27c.
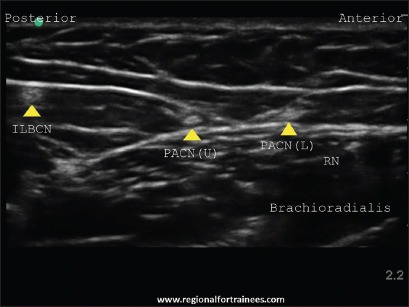
Ultrasound scan of the branches of posterior antebrachial cutaneous nerve (PACN) (PACN (U) = PACN upper branch, PACN (L) = PACN lower branch). Inferior lateral brachial cutaneous nerve (ILBCN) can also be seen
Injection
A 25-27 G hypodermic needle is introduced in-plane, in an anterior to posterior direction aiming to enter the subcutaneous plane containing the nerve. After negative aspiration, 2-3 ml local anesthetic is injected to fill the fascial plane containing the PACN.
Conclusion
The distal peripheral nerve blocks are relatively easy to perform using ultrasound guidance. These blocks are very useful as rescue blocks in the event of an incomplete anesthesia following brachial plexus blocks, or as standalone anesthetic or analgesic techniques. Good anatomical knowledge of their course and branches helps in their identification and selection for appropriate surgical procedures.
Acknowledgments
All images in this manuscript have been taken from www.regionalfortrainees.com (courtesy of www.regionalfortrainees.com).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Maga JM, Cooper L, Gebhard RE. Outpatient regional anesthesia for upper extremity surgery update (2005 to present) distal to shoulder. Int Anesthesiol Clin. 2012;50:47–55. doi: 10.1097/AIA.0b013e31821a00a8. [DOI] [PubMed] [Google Scholar]
- 2.Lin E, Choi J, Hadzic A. Peripheral nerve blocks for outpatient surgery: Evidence-based indications. Curr Opin Anaesthesiol. 2013;26:467–74. doi: 10.1097/ACO.0b013e328362baa4. [DOI] [PubMed] [Google Scholar]
- 3.Tran DQ, Pham K, Dugani S, Finlayson RJ. A prospective, randomized comparison between double-, triple-, and quadruple-injection ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2012;37:248–53. doi: 10.1097/AAP.0b013e31824611bf. [DOI] [PubMed] [Google Scholar]
- 4.Tsui BC, Doyle K, Chu K, Pillay J, Dillane D. Case series: Ultrasound-guided supraclavicular block using a curvilinear probe in 104 day-case hand surgery patients. Can J Anaesth. 2009;56:46–51. doi: 10.1007/s12630-008-9006-5. [DOI] [PubMed] [Google Scholar]
- 5.Chin KJ, Singh M, Velayutham V, Chee V. Infraclavicular brachial plexus block for regional anaesthesia of the lower arm. Anesth Analg. 2010;111:1072. doi: 10.1213/ANE.0b013e3181dbac5d. [DOI] [PubMed] [Google Scholar]
- 6.Handoll HH, Koscielniak-Nielsen ZJ. Single, double or multiple injection techniques for axillary brachial plexus block for hand, wrist or forearm surgery. Cochrane Database Syst Rev. 2006 Jan 25;1:CD003842. doi: 10.1002/14651858.CD003842.pub2. [DOI] [PubMed] [Google Scholar]
- 7.McCartney CJ, Xu D, Constantinescu C, Abbas S, Chan VW. Ultrasound examination of peripheral nerves in the forearm. Reg Anesth Pain Med. 2007;32:434–9. doi: 10.1016/j.rapm.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 8.Foxall GL, Skinner D, Hardman JG, Bedforth NM. Ultrasound anatomy of the radial nerve in the distal upper arm. Reg Anesth Pain Med. 2007;32:217–20. doi: 10.1016/j.rapm.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 9.Kathirgamanathan A, French J, Foxall GL, Hardman JG, Bedforth NM. Delineation of distal ulnar nerve anatomy using ultrasound in volunteers to identify an optimum approach for neural blockade. Eur J Anaesthesiol. 2009;26:43–6. doi: 10.1097/EJA.0b013e328318c5b6. [DOI] [PubMed] [Google Scholar]
- 10.Fredrickson MJ, Ting FS, Chinchanwala S, Boland MR. Concomitant infraclavicular plus distal median, radial, and ulnar nerve blockade accelerates upper extremity anaesthesia and improves block consistency compared with infraclavicular block alone. Br J Anaesth. 2011;107:236–42. doi: 10.1093/bja/aer101. [DOI] [PubMed] [Google Scholar]
- 11.Fredrickson MJ, Price DJ. Analgesic effectiveness of ropivacaine 0.2% vs 0.4% via an ultrasound-guided C5-6 root/superior trunk perineural ambulatory catheter. Br J Anaesth. 2009;103:434–9. doi: 10.1093/bja/aep195. [DOI] [PubMed] [Google Scholar]
- 12.Lam NC, Charles M, Mercer D, Soneru C, Dillow J, Jaime F, et al. A triple-masked, randomized controlled trial comparing ultrasound-guided brachial plexus and distal peripheral nerve block anesthesia for outpatient hand surgery. Anesthesiol Res Pract 2014. 2014 doi: 10.1155/2014/324083. 324083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith BE, Challands JF, Suchak M, Siggins D. Regional anaesthesia for surgery of the forearm and hand. A technique of combined supraclavicular and discrete blocks. Anaesthesia. 1989;44:747–9. doi: 10.1111/j.1365-2044.1989.tb09261.x. [DOI] [PubMed] [Google Scholar]
- 14.Tsui BC, Pillay JJ, Chu KT, Dillane D. Electrical impedance to distinguish intraneural from extraneural needle placement in porcine nerves during direct exposure and ultrasound guidance. Anesthesiology. 2008;109:479–83. doi: 10.1097/ALN.0b013e318182c288. [DOI] [PubMed] [Google Scholar]
- 15.Dillane D, Tsui BC. Is there still a place for the use of nerve stimulation? Paediatr Anaesth. 2012;22:102–8. doi: 10.1111/j.1460-9592.2011.03729.x. [DOI] [PubMed] [Google Scholar]
- 16.Gadsden J, McCally C, Hadzic A. Monitoring during peripheral nerve blockade. Curr Opin Anaesthesiol. 2010;23:656–61. doi: 10.1097/ACO.0b013e32833d4f99. [DOI] [PubMed] [Google Scholar]
- 17.Gadsden JC, Choi JJ, Lin E, Robinson A. Opening injection pressure consistently detects needle-nerve contact during ultrasound-guided interscalene brachial plexus block. Anesthesiology. 2014;120:1246–53. doi: 10.1097/ALN.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 18.Stranding S, editor. 40th ed. London: Churchill Livingstone; 2008. Upper arm. Gray's Anatomy: The Anatomical Basis of Clinical Practice; pp. 823–30. [Google Scholar]
- 19.Stranding S, editor. 40th ed. London: Churchill Livingstone; 2008. Forearm. Gray's Anatomy: The Anatomical Basis of Clinical Practice; pp. 839–56. [Google Scholar]
- 20.Stranding S, editor. 40th ed. London: Churchill Livingstone; 2008. Wrist and hand. Gray's Anatomy: The Anatomical Basis of Clinical Practice; pp. 857–98. [Google Scholar]
- 21.Viscomi CM, Reese J, Rathmell JP. Medial and lateral antebrachial cutaneous nerve blocks: An easily learned regional anesthetic for forearm arteriovenous fistula surgery. Reg Anesth. 1996;21:2–5. [PubMed] [Google Scholar]
- 22.Masear VR, Meyer RD, Pichora DR. Surgical anatomy of the medial antebrachial cutaneous nerve. J Hand Surg Am. 1989;14:267–71. doi: 10.1016/0363-5023(89)90019-1. [DOI] [PubMed] [Google Scholar]
- 23.Thallaj A, Marhofer P, Kettner SC, Al-Majed M, Al-Ahaideb A, Moriggl B. High-resolution ultrasound accurately identifies the medial antebrachial cutaneous nerve at the midarm level: A clinical anatomic study. Reg Anesth Pain Med. 2011;36:499–501. doi: 10.1097/AAP.0b013e318228a359. [DOI] [PubMed] [Google Scholar]
- 24.Moritz T, Prosch H, Pivec CH, Sachs A, Pretterklieber ML, Kriechbaumer L, et al. High-resolution ultrasound visualization of the subcutaneous nerves of the forearm: A feasibility study in anatomic specimens. Muscle Nerve. 2014;49:676–9. doi: 10.1002/mus.24064. [DOI] [PubMed] [Google Scholar]
- 25.Thallaj A. Ultrasound guidance of uncommon nerve blocks. Saudi J Anaesth. 2011;5:392–4. doi: 10.4103/1658-354X.87269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beldner S, Zlotolow DA, Melone CP, Jr, Agnes AM, Jones MH. Anatomy of the lateral antebrachial cutaneous and superficial radial nerves in the forearm: A cadaveric and clinical study. J Hand Surg Am. 2005;30:1226–30. doi: 10.1016/j.jhsa.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 27.Wongkerdsook W, Agthong S, Amarase C, Yotnuengnit P, Huanmanop T, Chentanez V. Anatomy of the lateral antebrachial cutaneous nerve in relation to the lateral epicondyle and cephalic vein. Clin Anat. 2011;24:56–61. doi: 10.1002/ca.21067. [DOI] [PubMed] [Google Scholar]
- 28.Blanco R, Gómez BM, González JM. Ultrasound appearance of the cutaneous nerves of the upper limb: A novel description in pain management. J Pain Relief. 2012;1:e109. [Google Scholar]
- 29.Chiavaras MM, Jacobson JA, Billone L, Lawton JM, Lawton J. Sonography of the lateral antebrachial cutaneous nerve with magnetic resonance imaging and anatomic correlation. J Ultrasound Med. 2014;33:1475–83. doi: 10.7863/ultra.33.8.1475. [DOI] [PubMed] [Google Scholar]
- 30.Egeler C. Cutaneous Nerves of the Arm and Forearm-How Small Can We Go?. Abstracts and Highlight Papers of the 32nd Annual European Society of Regional Anaesthesia and Pain Therapy (ESRA) Congress 2013: Invited Speaker Highlight Papers. 2013:E1–259. doi: 10.1097/AAP.0b013e3182a6a39d. [DOI] [PubMed] [Google Scholar]


