Abstract
Trauma is a leading cause of death worldwide, and almost 30% of trauma deaths are due to blood loss. A number of concerns have been raised regarding the advisability of the classic principles of aggressive crystalloid resuscitation in traumatic hemorrhagic shock. Some recent studies have shown that early volume restoration in certain types of trauma before definite hemostasis may result in accelerated blood loss, hypothermia, and dilutional coagulopathy. This review discusses the advances and changes in protocols in fluid resuscitation and blood transfusion for treatment of traumatic hemorrhage shock. The concept of low volume fluid resuscitation also known as permissive hypotension avoids the adverse effects of early aggressive resuscitation while maintaining a level of tissue perfusion that although lower than normal, is adequate for short periods. Permissive hypotension is part of the damage control resuscitation strategy, which targets the conditions that exacerbate hemorrhage. The elements of this strategy are permissive hypotension, minimization of crystalloid resuscitation, control of hypothermia, prevention of acidosis, and early use of blood products to minimize coagulopathy.
Keywords: Damage control resuscitation, fluid resuscitation, massive transfusion protocol, permissive hypotension
Introduction
Globally, injuries contribute to around 10% of total deaths and 15% of disability-adjusted life-years.[1] Recent studies suggest that injuries contribute to 13-18% of total deaths in India. Road traffic injuries (RTIs) place a huge burden on the health sector in terms of prehospital care, acute care, and rehabilitation.[1] According to WHO, RTIs are the sixth leading cause of deaths in India with a greater share of hospitalizations, deaths, disabilities and socioeconomic losses in young and middle-age populations. Most of the deaths occur due to poor decision and inappropriate interventions. An estimated 10-20% of these deaths are potentially preventable with better control of bleeding. Early hemorrhage within 6 h after incurring an injury emerged as the biggest cause of preventable deaths. This has led trauma teams to investigate whether the change in practice could help reduce early mortality after severe trauma.[2]
For the past four decades, the standard approach to the trauma victim, who is hypotensive from presumed hemorrhage has been to transfuse large volumes of fluid as early and as rapidly as possible. The goals of this treatment strategy are rapid restoration of intravascular volume and vital signs toward normal and maintenance of vital organ perfusion. High volume IV fluid for hemodynamic instability has been the accepted standard in most prehospital care systems like advanced trauma life support system (ATLS). The most recent laboratory studies and clinical trials evaluating the efficacy of these guidelines however suggest that in the setting of uncontrolled hemorrhage, aggressive fluid resuscitation may be harmful, resulting in increased hemorrhagic volume and subsequently greater mortality.[3]
To devise a strategy for resuscitation certain questions needs to be answered.
What is the risk of hypovolemia in trauma patients?
What is resuscitation injury?
What strategies of fluid resuscitation are available?
Liberal versus restrictive
What are various recommendations from the literature?
We need to understand the pathophysiology of trauma and hemorrhagic shock. It may be defined as a life threatening condition characterized by inadequate delivery of oxygen to vital organs in relation to their metabolic requirements.[4] A systolic blood pressure (SBP) of 90 mmHg is commonly used to define both hypotension and shock; however, oxygen delivery depends on cardiac output rather than blood pressure. Homeostasis with peripheral vasoconstriction acts to preserve blood pressure even as circulatory volume is lost. The relation between cardiac output and blood loss is ill-defined, and the relationship becomes evident only when more than half of circulating volume is lost, or the loss is rapid. Many patients will maintain their pulse and blood pressure even after massive blood loss and tissue hypoxia. This condition is termed as a cryptic shock and is associated with increased mortality.[5]
Resuscitation Injury
Another parameter that needs to be understood is resuscitation injury. In the setting of trauma, capillary permeability increases, leading to a loss of intravascular fluid into the interstitial space. Moreover, acidosis that results from significant trauma impairs cardiac function.[6] Treating these patients with a large volume of crystalloids can lead to cellular swelling and resulting dysfunction.[6] Fluid causes dilutional coagulopathy, clot disruption from increased blood flow, decreased blood viscosity and interstitial edema. There is increased risk of acute respiratory distress syndrome and multi-organ failure. Large volume crystalloid resuscitation causes gastrointestinal and cardiac complications,[5] increased extremity compartment pressures[7] and coagulation disturbances. Abdominal compartment syndrome is clearly proven to be a result of large volume crystalloid resuscitation.[8] Secondary abdominal compartment syndrome occurs in patients without any underlying abdominal injury, has mortality >50% and is clearly linked to over aggressive fluid resuscitation strategies.[8]
Pathophysiology of Hypovolemic Micro-circulation
Hypovolemia and blood loss lead to inadequate perfusion of micro-circulation that result in insufficient oxygen availability to meet the needs of mitochondrial oxidative phosphorylation. Adequate micro-circulation relies on the function of the different components of micro-circulation. Red and white blood cells, endothelial cells and smooth muscle cells have to function in close harmony to ensure adequate micro-circulatory blood flow to transport oxygen to the tissues. The function of these components is affected by hypovolemia. Administration of fluids to correct hypovolemia may modulate micro-circulatory function by various mechanisms. The flow is increased by enhanced filling of the vasculature that generates forcing pressure and promotes micro-circulatory perfusion. Fluids also modify the hemorheology of blood by decreasing the viscosity that additionally promotes blood flow. However, excessive hemodilution can cause shunting of the micro-circulation and impair regional tissue oxygenation. This effect can differ among the different organ systems.[9]
Coagulation and Trauma
Coagulation disorders in trauma have a complex pathophysiology including activation or dysfunction of fibrin generation or both, platelet and endothelium dysfunction, relative inhibition of stable clot formation by anticoagulant and fibrinolytic pathways and either consumption or inhibition of coagulation proteases. Fluid shifts associated with blood loss, crystalloid infusion and transfusion of packed red blood cells (RBC's) contributes to dilutional coagulopathy. Hypothermia and acidosis also contributes to coagulopathy and continued blood loss. Shock following acute blood loss or RBC's appears to be the most important factor in the development of coagulopathy. Hess et al.[10] have suggested in their review six main precipitants of coagulopathy in trauma — tissue trauma, shock, hemodilution, hypothermia, acidemia and inflammation.
The alternate strategy to the early resuscitation is limited resuscitation or hypotensive resuscitation. Two slightly different strategies have been advanced to prevent clot disruption and dilutional coagulopathy. The first is delayed resuscitation, where fluid is withheld until bleeding is definitively controlled. The second is permissive hypotension, where fluid is given, but the resuscitative endpoint is something less than normotension.[11] This approach provides a mechanism for avoiding the detrimental effects associated with early aggressive resuscitation. Permissive hypotension is a term used to describe the use of restricted fluid therapy especially in trauma patients that increases systemic blood pressure without reaching normotension. This implies that maintaining perfusion although decreased from the normal physiological range, is adequate for short periods. The concept does not exclude therapy by means of intravenous fluids; inotropes or vasopressor, the only restriction is to avoid completely normalizing blood pressure in a context where blood loss may be enhanced.[12]
Timings and Goals of Resuscitation from Hemorrhagic Shock
Liberal versus restrictive approach
Advocates of aggressive crystalloid resuscitation suggest that the theoretical benefits of normalizing or even super normalizing blood pressure and oxygen delivery are clear. These benefits include repayment of oxygen debt, clearance of acidosis, and correction of extracellular fluid deficit. However, more recent evidence (primarily in models of uncontrolled hemorrhage) suggests that premature or aggressive resuscitation may lead to dislodging of soft clots and dilutional coagulopathy, which results in increased hemorrhage and mortality.[13]
A recent study reported that overly aggressive fluid treatment accelerated hepatocellular injury while another suggested that slower rates of fluid resuscitation led to improvements in cell mediated immunity.[14] Numerous studies have shown that immediate fluid resuscitation caused increases in the rate, volume, and duration of hemorrhage. Before discussing human data on restrictive resuscitation strategies, it must be noted that all strategies that permit hypotension are absolutely contraindicated in patients with traumatic brain injury (TBI). It has been shown that even a single episode of hypotension causes a doubling of mortality in this patient population.
In the presence of uncontrolled hemorrhage in patients with concurrent TBI, prevention of secondary brain injury from hypotension is crucial as a SBP <90 mmHg is associated with poor outcomes. Infuse small aliquots of fluid (100-200 ml) to maintain SBP above 90 mmHg (Grade I evidence). Concept of permissive hypotension should be carefully considered in the elderly patients and are relatively contraindicated in patients with chronic arterial hypertension, carotid stenosis, angina pectoris and compromised renal function.
Rethinking of aggressive fluid resuscitation followed the publication of famous “Mattox trial” in 1994 by Bickell et al.[15] The investigators performed a prospective, single center trial comparing immediate and delayed fluid resuscitation in 598 adults with penetrating torso injuries. All patients presenting had a prehospital SBP of <90 mmHg. A total 203 of 289 patients (70%) who received delayed fluid resuscitation survived compared with 193 of 309 patients (62%) who received immediate fluid resuscitation (P = 0.4). The number of patients having one or more postsurgical complications was lower in the delayed fluid resuscitation group versus those receiving immediate fluid resuscitation: About 23% versus 30% respectively. Numerous studies before and since this study have failed to demonstrate a survival benefit for aggressive fluid resuscitation before mechanical stabilization of the injury. There is also evidence to suggest that restoring normal or near normal blood pressure using fluid resuscitation before surgery may even worsen survival.
In a study undertaken in 2002 by Dutton et al., 110 patients with hemorrhagic shock were randomized into two groups with target SBP >100 mmHg and target SBP of 70 mmHg. Fluid therapy was targeted to this end point. They used a technique of 250-500 ml boluses to treat hypotensive values. Unfortunately, they found that the blood pressure tended to fluctuate with the boluses, making it hard to accurately maintain the desired value. As a result, for the 110 patients they randomized, the average SBP was 100 mgHg in the restricted protocol and 114 mmHg in the standard cohort (P < 0.001). Survival was equal at 92.7% with four deaths in each group.[16]
Sampalis et al.[17] reviewed the outcome of 217 trauma patients who had received intravenous fluids and compared them with 217 controls who received no-fluids. Correction was made for gender, age, mechanism for injury and injury severity score. Patients who received onsite fluid resuscitation had a higher mortality than the control group, particularly when fluid resuscitation was combined with prolonged prehospital times. They compared prehospital times of <30 min with time >30 min. In one group, the use of onsite IV fluid replacement provides no association with a significant increase in mortality.
In 1986, Blair et al.[18] reported that the incidence of rebleeding was decreased in patients with gastrointestinal hemorrhage for whom early transfusion was withheld (P < 0.01). With a relative paucity of human data, a Cochrane review[19] came to the conclusion that there was no evidence for or against early volume resuscitation in uncontrolled hemorrhage. This study did not prefer one colloid over another and hypertonic crystalloid over isotonic crystalloid.
Cochrane review was done on timing and volume of fluid administration for patients with bleeding to assess the effects of early versus delayed; larger versus smaller volume of fluid administration, in trauma patients with bleeding. In this review, there is no evidence from randomized controlled trials for or against early or larger volume of intravenous fluid administration in uncontrolled hemorrhage. The review concluded that the uncertainty continues regarding best fluid administration strategy in bleeding trauma patients. Further, randomized controlled trials are needed to establish the most effective fluid resuscitation strategy.
A study done by Turner et al.,[20] in 1309 hypotensive trauma patients randomized to receive fluids or no-fluids in the prehospital period revealed 10.4% mortality in early fluid administration group versus 9.8% in delayed/no fluid group. It recommended that rather than concentrating on fluid protocols, ambulance services should avoid unnecessary delays and speed up transfer to definitive care in the hospital.
A study by Anne Morrison et al.[21] showed that hypotensive resuscitation strategy reduces transfusion requirement and severe postoperative coagulopathy in trauma with hemorrhagic shock. It showed that hypotensive resuscitation is a safe strategy in trauma population and hypotensive resuscitation to minimum intraoperative mean arterial pressure (MAP) of 50 mmHg does not increase 30 days mortality as compared to target MAP of 65 mmHg. It reduces the risk of early postoperative mortality of coagulopathy bleeding and does not increase the length of hospital/intensive care unit (ICU) stay.
Emergency Department Evaluation of a Patient in Shock
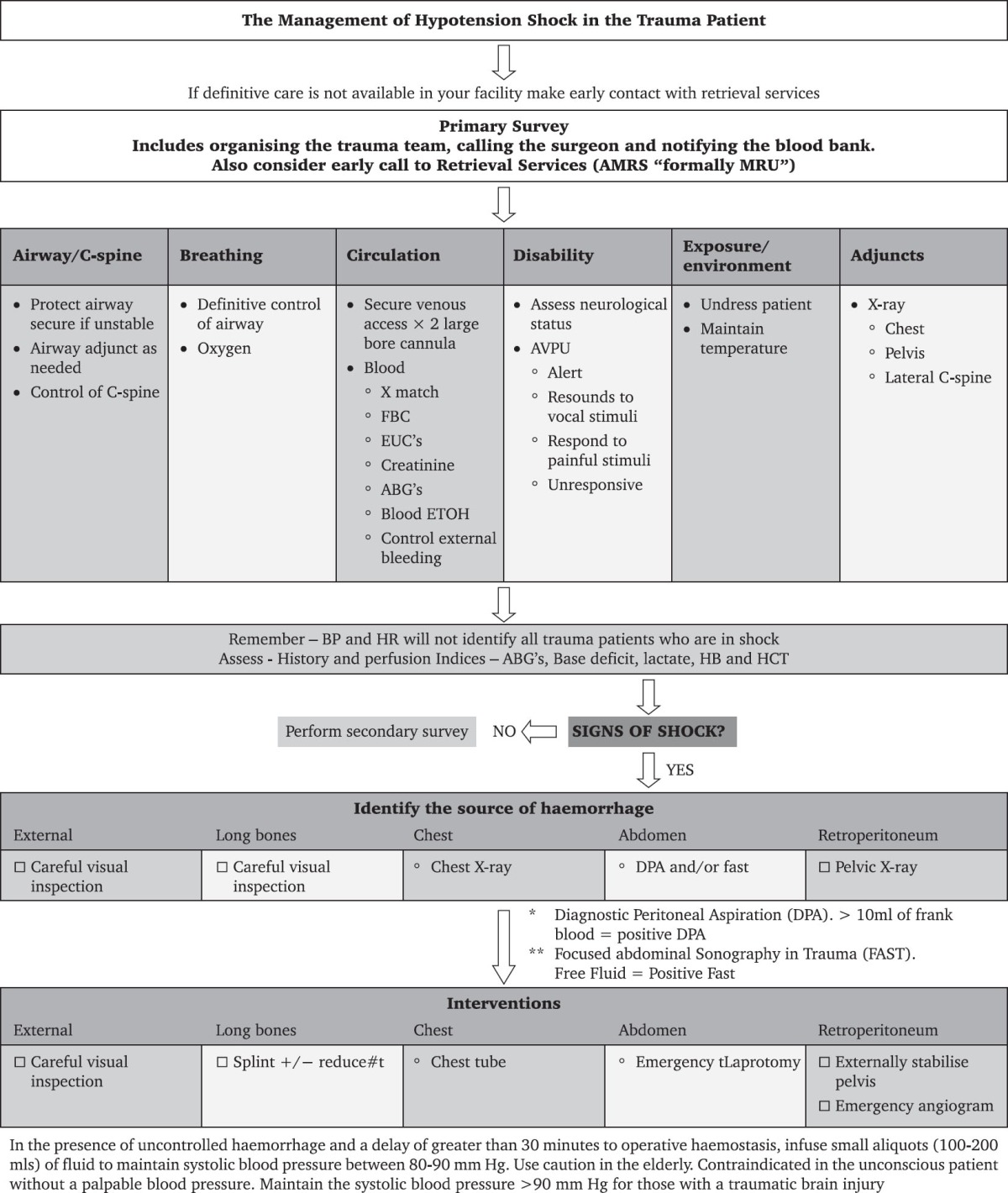
When the trauma patients arrive at triage, they must be rapidly assessed for either being in shock or at risk of shock. Trauma patients should have their airway, breathing and circulation addressed immediately followed by trauma team activation and controlling the source of bleeding and localizing by focused assessment sonography in trauma (FAST)/X-ray chest [Table 1].
Table 1.
Adapted from management of hypovolemic shock in trauma patient; NSW Institute of Trauma and Injury Management; January 2007 SH PN: (T1) 070034
Damage Control Resuscitation[27]
The coagulopathy of trauma is already present in many patients on their arrival to the emergency, and it impacts management. The treatment of coagulopathy in hemorrhagic shock is no longer the responsibility of just the surgeon and the intensivist but initiating the treatment is also within the emergency clinician's purview. This treatment is an essential part of what has come to known as damage control resuscitation (DCR).[22,23,24]
The term “lethal triad” is used to describe the mutually perpetuating combination of acute coagulopathy, hypothermia, and acidosis seen in exsanguinating trauma patients.[25] Hypo-perfusion leads to decreased oxygen delivery, a switch to anaerobic metabolism, lactate production, and metabolic acidosis. Anaerobic metabolism limits endogenous heat production, exacerbating hypothermia caused by exposure and injudicious administration of cold resuscitation fluids and blood. Large, well-conducted retrospective studies have shown that the core temperature of <35°C on admission is an independent predictor of mortality after major trauma.[26]
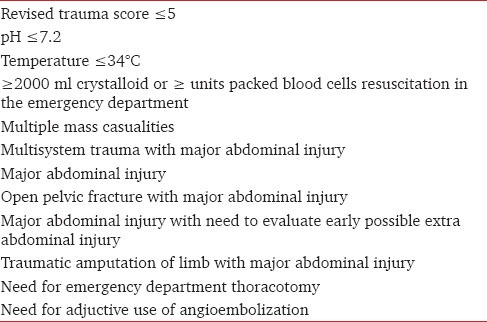
An understanding of the mechanism of coagulopathy, acidosis, and hypothermia “Lethal Triad” forms the basis of DCR. DCR addresses all the three components of the Lethal Triad and integrates the permissive hypotension, hemostatic resuscitation and damage control surgery.[27] Aim is to minimize hypovolemic shock diagnosed by triad of pattern recognition — cold clammy skin, weak or absent radial pulse and abnormal mental status in that acidosis, hypotension and hypothermia need to be addressed too. Acidosis with the base deficit of more than 6 mmol/L is a predominant physiological defect resulting from persistent hypo-perfusion. pH of <7.2 is associated with decreased contractility and cardiac output, vasodilatation, hypotension, bradycardia, dysarrhythmias and decreased blood flow to liver and kidney. Hypothermia is associated with high mortality. If the temperature is <96.50°F hypocoagulability occurs. However, damage control approach is suitable for only selected group of patients. Asensio et al.[27] identified preoperatively characteristics predictive of “exsanguinating syndrome” in which a damage control would be appropriate [Table 2].
Table 2.
Characteristics predictive of “exsanguinating syndrome” and indication of for damage contol from Asensio et al.
Components of Damage Control Resuscitation
Permissive hypotension
The aim is to allow a subnormal blood pressure to minimize hemorrhagic blood loss. For uncontrolled hemorrhage in the absence of TBI, target resuscitation to SBP of 7-90 mmHg, normal mentation and palpable peripheral pulses (level of evidence III). Blood should allow sufficient oxygen delivery to tissues that is ensured by monitoring serum lactate levels and central venous oxygen saturation. There is no study in pediatrics to support its use.
Hemostatic resuscitation
The term denotes the very early use of blood and blood products as primary resuscitation fluids to treat intrinsic acute traumatic coagulopathy and to prevent the development of dilutional coagulopathy. It is initiated within minutes of arrival in the emergency department. First resuscitation is limited to keep blood pressure at 90 mmHg, preventing renewed bleeding from recently clotted vessels. Secondly, intravascular volume restoration is accomplished using thawed plasma a primary resuscitation fluid in at least 1:1 ratio with packed red blood cells (PRBC). Causalities who require continued resuscitation, massive transfusion protocol (MTP) is activated with delivery of 6 units of plasma, 6 units of PRBCs and 10 units of cryoprecipitate. Ruskin et al.[28] showed that deaths from trauma significantly decreased after introduction of MTP.
Massive transfusion however may cause hypocalcemia, hyperkalemia, hypomagnesemia, acid base disturbances, hypothermia, thrombocytopenia, and coagulopathy. Recent studies indicate that packed red cells replacement along with fresh frozen plasma (FFP) and platelet concentrates early in trauma management prevents dilutional effects and markedly improves the coagulopathic bleeding in trauma patients. The aggressive hemostatic resuscitation should be combined with equally aggressive control of bleeding. Tranexamic acid, an antifibrinolytic agent, is to be given to all patients with uncontrolled bleeding who required blood transfusion.[13] As per CRASH-2 trial[29] in 2010 for evaluation of the role of tranexamic acid, 20,000 trauma patients were randomized to receive either tranexamic acid or control. Tranexamic acid significantly reduced the risk of death (odds ratio [OR]: 0.91 [0.85-0.97], P = 0.0035) and death from hemorrhage (OR: 0.85 [90.76-0.96], P < 0.001) without any increase in thromboembolic complication.
Damage control surgery
Damage control surgery is defined as the planned temporary sacrifice of normal anatomy to preserve the vital physiology. This is a concept in which the initial surgery becomes part of the resuscitation process rather than part of the curative process.[30,31] It consists of 3 parts including the initial abbreviated laparotomy, ICU resuscitation and subsequent reoperation for definitive resuscitation [Figure 1].[32] Damage control surgery is a surgical strategy aimed at restoring normal physiology rather than anatomical integrity. Only when the patient has become physiologically stable is the final therapeutic surgery embarked on. This process serves to limit the physiological exposure to an unstable environment, allowing better resuscitation and outcome in the critically ill trauma patients.
Figure 1.
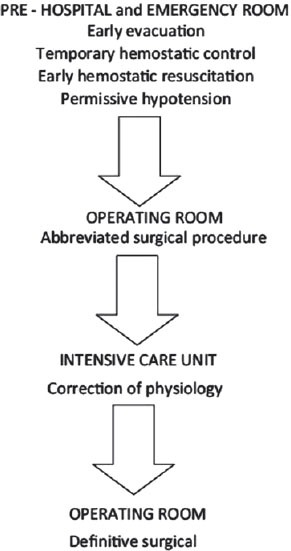
Damage Control Sequence[31]
Multidisciplinary approach to the management of critically injured, updated European guidelines[33] recommends [Figure 2]:
Figure 2.
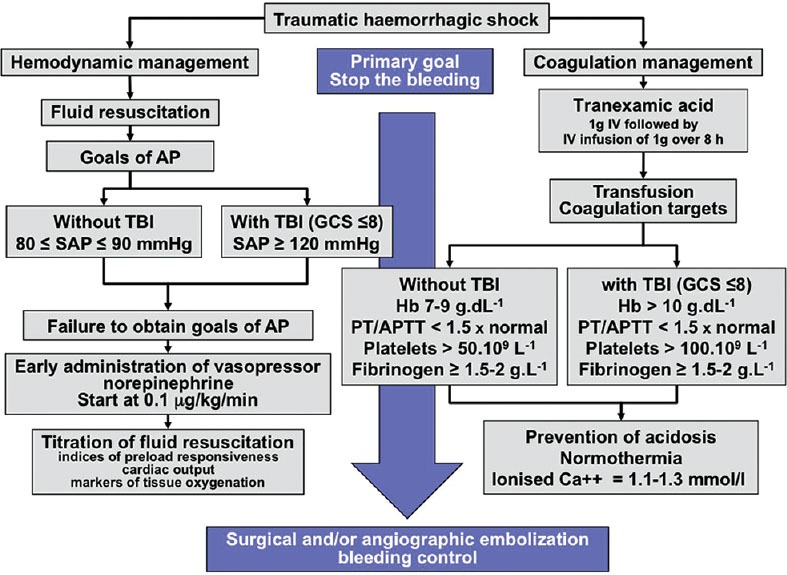
Flow chart of initial management of traumatic hemorrhagic shock. In the acute phase of traumatic hemorrhagic shock, the therapeutic priority is to stop the bleeding. As long as this bleeding is not controlled, the physician must manage fluid resuscitation, vasopressors, and blood transfusion to prevent or treat acute coagulopathy of trauma (AP = Arterial pressure, SAP = Systolic arterial pressure, TBI = Trauma brain injury, Hb = Hemoglobin, PT = Prothrombin time, APTT = Activated partial thromboplastin time)[36]
Time elapsed between injury and operation should be minimized for patients in need of urgent surgical bleeding control (Grade IA).
Patients presenting with hemorrhagic shock and an indentified source of bleeding should undergo an immediate bleeding control procedure unless initial resuscitation measures are successful (Grade IB).
Early imaging (FAST or computed tomography) for detection of free fluid in patients with suspected torso trauma (Grade IB). If FAST is positive, it should be followed by immediate intervention.
A target SBP of 80-100 mmHg until major bleeding is stopped in the initial phase without TBI (Grade IC). Low volume approach is contraindicated in TBI as adequate perfusion pressure is crucial to ensure tissue oxygenation of injured central nervous system.
Target MAP of 65 mmHg or more, in controlled hypotensive resuscitation.
Adjunct tourniquet use to stop life-threatening bleeding from open extremity injuries in the presurgical setting.
Initial normoventilation of trauma patients if there are no signs of imminent cerebral herniation. A low partial pressure of arterial carbon dioxide on admission to the emergency room is associated with a worse outcome in trauma patients with TBI. Hyperventilation and hypocapnia cause intense vasoconstriction with decreased cerebral blood flow and impaired tissue perfusion.
Hemorrhagic shock with identified source of bleeding — initiate immediate bleeding control procedure.
Serum lactate and base deficit measurement to estimate and monitor extent of bleeding and shock (Grade IB). Serum lactate is diagnostic parameter and prognostic marker of hemorrhagic shock. The amount of lactate produced by anaerobic glycolysis is an indirect marker of oxygen debt, tissue hypo-perfusion and the severity of hemorrhagic shock. Base deficit gives indirect estimation of acidosis due to impaired perfusion. Repeated lactate determinations represent a reliable prognostic index for patients with circulatory shock.
DCR should be employed in severely injured patient presenting with deep hemorrhagic shocks, signs of ongoing bleeding and coagulopathy, hypothermia, acidosis, inaccessible major anatomical injury.
Crystalloid should be applied initially for bleeding trauma patients (Grade IB). Hypertonic saline (HTS) to be considered for hemodynamically unstable patients (Grade 2B). Addition of colloid to be considered within the prescribed limits for each solution in hemodynamically unstable patients (Grade 2C).
Early FFP in patients with massive bleeding (Grade IB). Platelets to be administered to maintain the count above 50 × 109/L (Grade IC). However, maintain the count above 100 × 109/L in patients with multiple trauma who are severely bleeding or have traumatic brain trauma (Grade 2C).
Tranexamic acid 10-15 mg/kg followed by infusion of 1-5 mg/kg/h (Grade IB).
Target hemoglobin of 7-9 gm% (Grade IC).
Monitoring of ionized calcium during massive transfusion (Grade IC). Calcium chloride to be administered if ionized calcium levels are low or electrocardiographic changes suggests hypocalcemia (Grade 2C).
Characteristics of Optimal Resuscitation Fluid
As stated by Tremblay et al.[34] that “… the optimal fluid for resuscitation would combine the volume expansion and oxygen carrying capacity of blood, without the need for cross-matching or the risk of disease transmission. In addition, it would restore and maintain the normal composition and distribution of body fluid compartments.” Taking this one step further, the ideal fluid would combine all of those things with positive immunologic and coagulation effects and be durable, portable, and cheap. None of the fluid options currently available comes close to this ideal. Standard trauma resuscitation as defined by the ATLS course includes infusion of ringer lactate solution,[35] which is a racemic mixture containing two stereo-isomers of lactate D-lactate and L-lactate. Normal saline is also frequently used with lactated ringer for resuscitation in hemorrhagic shock, but it has been associated with hyperchloremic acidosis, when given in large volumes.[13]
Hypertonic saline and hypertonic saline dextran solutions (HSD) have also been used as a treatment for raised intra-cranial pressure and early treatment for TBI. Early administration of HSD can lead to improved serum biomarkers of brain injury. But at this time, there is no evidence to suggest that either HTS or HSD provide significant benefit in the early treatment of patients with TBI.[13]
Traditionally there has been no role of colloids in trauma resuscitation due to associated side effects. Gelatins have been associated with anaphylaxis and significant hypernatraemia. They also cause paradoxical hypotension due to release of bradykinin by contaminants.[35] Coagulopathy is a common complication of hemorrhagic shock. Resuscitation associated hemodilution may alter hemostasis by lowering the concentration of clotting proteins. Use of crystalloids has been thought to be without negative effect on coagulation except for that attributable to hemodilution. Crystalloids have no specific adverse effects on renal function except that they may not restore blood volume adequately.[36] However, colloids have adverse effects on renal function. In patients with excessive fluid deficits, glomerular filtration of hyperoncotic colloids (dextrans, 10% hydroxyl ethyl starch [HES], 20% albumin) may cause a hyperviscous urine and stasis of the tubular flow resulting in obstruction of tubular lumen.[36,37] Gelatins have no significant damaging effect on the kidneys.[36,37]
The controversy regarding the use of crystalloids versus colloids for resuscitation has been in debate for last so many years. A recent Cochrane database analysis on crystalloids versus colloids published in 2013 that the resuscitation using colloids compared with crystalloids reduces the risk of death in patients with trauma, burns or following surgery. The use of HES may increase mortality.[38] Cochrane review concluded that since colloid use is not associated with improved survival, and they are considerably more expensive than crystalloids, it is hard to see how their continued use in clinical practice can be justified.[39] Further clinical trials of colloid use need to justify carefully the potential for patient benefit.
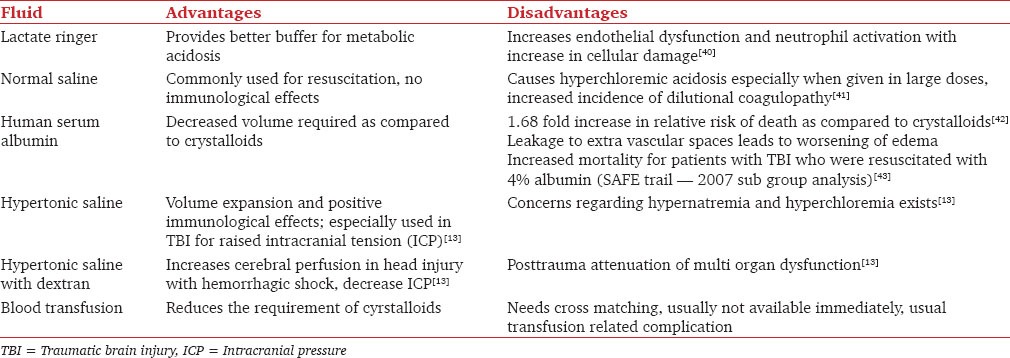
Standard approach to trauma victims has been to infuse large volumes of isotonic crystalloids as early and rapidly as possible. Most efficient solution for use is still under debate. The various options available are summarized in Table 3.
Table 3.
Resuscitation fluids
Conclusion
Debate continues regarding the strategy of fluid management in trauma. Hemorrhagic shock remains a leading cause of morbidity and mortality worldwide. Time-consuming procedures in the field should be avoided, and rapid transport to definitive care should be aimed at. Fluid choice has not been shown to affect the outcome in trauma, however large volume of the crystalloid resuscitation need to be avoided. In the absence of TBI, target SBP of 70-90 mmHg, normal mentation and peripheral pulses in case of uncontrolled hemorrhage should be aimed at. Normotension should be the aim in the presence of TBI. Tranexamic acid should be given to all the patients with penetrating trauma who need transfusion. MTP with fixed ratios should be given. Patients with penetrating trauma for whom definitive care is immediately available may benefit from damage control surgery. While DCR requires further study, the early literature seems to be promising.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gururaj G. Road traffic deaths, injuries and disabilities in India: Current scenario. Natl Med J India. 2008;21:14–20. [PubMed] [Google Scholar]
- 2.Holcomb JB, McMullin NR, Pearse L, Caruso J, Wade CE, Oetjen-Gerdes L, et al. Causes of death in U.S. Special Operations Forces in the global war on terrorism: 2001-2004. Ann Surg. 2007;245:986–91. doi: 10.1097/01.sla.0000259433.03754.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stern SA. Low-volume fluid resuscitation for presumed hemorrhagic shock: helpful or harmful? Curr Opin Crit Care. 2001;7:422–30. doi: 10.1097/00075198-200112000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Strehlow MC. Early identification of shock in critically ill patients. Emerg Med Clin North Am. 2010;28:57–66. doi: 10.1016/j.emc.2009.09.006. vii. [DOI] [PubMed] [Google Scholar]
- 5.Cotton BA, Guy JS, Morris JA, Jr, Abumrad NN. The cellular, metabolic, and systemic consequences of aggressive fluid resuscitation strategies. Shock. 2006;26:115–21. doi: 10.1097/01.shk.0000209564.84822.f2. [DOI] [PubMed] [Google Scholar]
- 6.Lang F, Busch GL, Ritter M, Völkl H, Waldegger S, Gulbins E, et al. Functional significance of cell volume regulatory mechanisms. Physiol Rev. 1998;78:247–306. doi: 10.1152/physrev.1998.78.1.247. [DOI] [PubMed] [Google Scholar]
- 7.Ablove RH, Babikian G, Moy OJ, Stegemann PM. Elevation in compartment pressure following hypovolemic shock and fluid resuscitation: A canine model. Orthopedics. 2006;29:443–5. doi: 10.3928/01477447-20060501-07. [DOI] [PubMed] [Google Scholar]
- 8.Balogh Z, McKinley BA, Cocanour CS, Kozar RA, Valdivia A, Sailors RM, et al. Supranormal trauma resuscitation causes more cases of abdominal compartment syndrome. Arch Surg. 2003;138:637–42. doi: 10.1001/archsurg.138.6.637. [DOI] [PubMed] [Google Scholar]
- 9.Boldt J, Ince C. The impact of fluid therapy on microcirculation and tissue oxygenation in hypovolemic patients: A review. Intensive Care Med. 2010;36:1299–308. doi: 10.1007/s00134-010-1912-7. [DOI] [PubMed] [Google Scholar]
- 10.Hess JR, Brohi K, Dutton RP, Hauser CJ, Holcomb JB, Kluger Y, et al. The coagulopathy of trauma: A review of mechanisms. J Trauma. 2008;65:748–54. doi: 10.1097/TA.0b013e3181877a9c. [DOI] [PubMed] [Google Scholar]
- 11.Revell M, Greaves I, Porter K. Endpoints for fluid resuscitation in hemorrhagic shock. J Trauma. 2003;54:S63–7. doi: 10.1097/01.TA.0000056157.94970.FA. [DOI] [PubMed] [Google Scholar]
- 12.Kreimeier U, Prueckner S, Peter K. Permissive hypotension. Schweiz Med Wochenschr. 2000;130:1516–24. [PubMed] [Google Scholar]
- 13.Cherkas D. Traumatic hemorrhagic shock: Advances in fluid management. Emerg Med Pract. 2011;13:1–19. [PubMed] [Google Scholar]
- 14.Shah KJ, Chiu WC, Scalea TM, Carlson DE. Detrimental effects of rapid fluid resuscitation on hepatocellular function and survival after hemorrhagic shock. Shock. 2002;18:242–7. doi: 10.1097/00024382-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Bickell WH, Wall MJ, Jr, Pepe PE, Martin RR, Ginger VF, Allen MK, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994;331:1105–9. doi: 10.1056/NEJM199410273311701. [DOI] [PubMed] [Google Scholar]
- 16.Dutton RP, Mackenzie CF, Scalea TM. Hypotensive resuscitation during active hemorrhage: Impact on in-hospital mortality. J Trauma. 2002;52:1141–6. doi: 10.1097/00005373-200206000-00020. [DOI] [PubMed] [Google Scholar]
- 17.Sampalis JS, Tamim H, Denis R, Boukas S, Ruest SA, Nikolis A, et al. Ineffectiveness of on-site intravenous lines: Is prehospital time the culprit? J Trauma. 1997;43:608–15. doi: 10.1097/00005373-199710000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Blair SD, Janvrin SB, McCollum CN, Greenhalgh RM. Effect of early blood transfusion on gastrointestinal haemorrhage. Br J Surg. 1986;73:783–5. doi: 10.1002/bjs.1800731007. [DOI] [PubMed] [Google Scholar]
- 19.Kwan I, Bunn F, Roberts I. WHO Pre-Hospital Trauma Care Steering Committee. Timing and volume of fluid administration for patients with bleeding. Cochrane Database Syst Rev. 2003;3:CD002245. doi: 10.1002/14651858.CD002245. [DOI] [PubMed] [Google Scholar]
- 20.Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D. A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma. Health Technol Assess. 2000;4:1–57. [PubMed] [Google Scholar]
- 21.Morrison CA, Carrick MM, Norman MA, Scott BG, Welsh FJ, Tsai P, et al. Hypotensive resuscitation strategy reduces transfusion requirements and severe postoperative coagulopathy in trauma patients with hemorrhagic shock: Preliminary results of a randomized controlled trial. J Trauma. 2011;70:652–63. doi: 10.1097/TA.0b013e31820e77ea. [DOI] [PubMed] [Google Scholar]
- 22.Beekley AC. Damage control resuscitation: A sensible approach to the exsanguinating surgical patient. Crit Care Med. 2008;36:S267–74. doi: 10.1097/CCM.0b013e31817da7dc. [DOI] [PubMed] [Google Scholar]
- 23.Rangarajan K, Subramanian A, Pandey RM. Determinants of mortality in trauma patients following massive blood transfusion. J Emerg Trauma Shock. 2011;4:58–63. doi: 10.4103/0974-2700.76839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hannon T. Trauma blood management: Avoiding the collateral damage of trauma resuscitation protocols. Hematology Am Soc Hematol Educ Program 2010. 2010:463–4. doi: 10.1182/asheducation-2010.1.463. [DOI] [PubMed] [Google Scholar]
- 25.Jansen JO, Thomas R, Loudon MA, Brooks A. Damage control resuscitation for patients with major trauma. BMJ. 2009;338:b1778. doi: 10.1136/bmj.b1778. [DOI] [PubMed] [Google Scholar]
- 26.Martin RS, Kilgo PD, Miller PR, Hoth JJ, Meredith JW, Chang MC. Injury-associated hypothermia: An analysis of the 2004 national trauma data bank. Shock. 2005;24:114–8. doi: 10.1097/01.shk.0000169726.25189.b1. [DOI] [PubMed] [Google Scholar]
- 27.Asensio JA, McDuffie L, Petrone P, Roldan G, Forno W, Gambaro E, et al. Reliable variables in the exsanguinated patient which indicate damage control and predict outcome. Am J Surg. 2001;182:743–51. doi: 10.1016/s0002-9610(01)00809-1. [DOI] [PubMed] [Google Scholar]
- 28.Riskin DJ, Tsai TC, Riskin L, Hernandez-Boussard T, Purtill M, Maggio PM, et al. Massive transfusion protocols: The role of aggressive resuscitation versus product ratio in mortality reduction. J Am Coll Surg. 2009;209:198–205. doi: 10.1016/j.jamcollsurg.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 29.CRASH-2 trial collaborators. Shakur H, Roberts I, Bautista R, Caballero J, Coats T, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): A randomised, placebo-controlled trial. Lancet. 2010;376:23–32. doi: 10.1016/S0140-6736(10)60835-5. [DOI] [PubMed] [Google Scholar]
- 30.Hirshberg A, Sheffer N, Barnea O. Computer simulation of hypothermia during “damage control” laparotomy. World J Surg. 1999;23:960–5. doi: 10.1007/s002689900607. [DOI] [PubMed] [Google Scholar]
- 31.Sagraves SG, Toschlog EA, Rotondo MF. Damage control surgery — The intensivist's role. J Intensive Care Med. 2006;21:5–16. doi: 10.1177/0885066605282790. [DOI] [PubMed] [Google Scholar]
- 32.Hsu JM, Pham TN. Damage control in the injured patient. Int J Crit Illn Inj Sci. 2011;1:66–72. doi: 10.4103/2229-5151.79285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, et al. Management of bleeding following major trauma: An updated European guideline. Crit Care. 2010;14:R52. doi: 10.1186/cc8943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tremblay LN, Rizoli SB, Brenneman FD. Advances in fluid resuscitation of hemorrhagic shock. Can J Surg. 2001;44:172–9. [PMC free article] [PubMed] [Google Scholar]
- 35.Dutta R, Chaturvedi R. Fluid therapy in trauma. MAJFI. 2010;66:312–6. doi: 10.1016/S0377-1237(10)80006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bouglé A, Harrois A, Duranteau J. Resuscitative strategies in traumatic hemorrhagic shock. Ann Intensive Care. 2013;3:1. doi: 10.1186/2110-5820-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boldt J. Volume replacement in the surgical patient — Does the type of solution make a difference? Br J Anaesth. 2000;84:783–93. doi: 10.1093/bja/84.6.783. [DOI] [PubMed] [Google Scholar]
- 38.Boldt J. Fluid choice for resuscitation of the trauma patient: A review of the physiological, pharmacological, and clinical evidence. Can J Anaesth. 2004;51:500–13. doi: 10.1007/BF03018316. [DOI] [PubMed] [Google Scholar]
- 39.Perel P, Roberts I, Ker K. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev. 2013;2:CD000567. doi: 10.1002/14651858.CD000567.pub6. [DOI] [PubMed] [Google Scholar]
- 40.Shires GT, Browder LK, Steljes TP, Williams SJ, Browder TD, Barber AE. The effect of shock resuscitation fluids on apoptosis. Am J Surg. 2005;189:85–91. doi: 10.1016/j.amjsurg.2004.06.040. [DOI] [PubMed] [Google Scholar]
- 41.Alam HB, Sun L, Ruff P, Austin B, Burris D, Rhee P. E- and P-selectin expression depends on the resuscitation fluid used in hemorrhaged rats. J Surg Res. 2000;94:145–52. doi: 10.1006/jsre.2000.6011. [DOI] [PubMed] [Google Scholar]
- 42.Cochrane Injuries Group Albumin Reviewers. Human albumin administration in critically ill patients: Systematic review of randomised controlled trials. BMJ. 1998;317:235–40. doi: 10.1136/bmj.317.7153.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.SAFE Study Investigators, Australian and New Zealand Intensive Care Society Clinical Trials Group, Australian Red Cross Blood Service, George Institute for International Health. Myburgh J, Cooper DJ, et al., editors. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874–84. doi: 10.1056/NEJMoa067514. [DOI] [PubMed] [Google Scholar]


