Abstract
Background and Aims:
This study was carried out to evaluate the difference in efficacy, safety, and complications of performing brachial plexus nerve blocks by using a nerve locator when compared to ultrasound (US) guidance.
Material and Methods:
A total of 102 patients undergoing upper limb surgery under supraclavicular brachial plexus blocks were randomly divided into two groups, one with US and the other with nerve stimulator (NS). In Group US, “Titan” Portable US Machine, Sonosite, Inc. Kensington, UK with a 9.0 MHz probe was used to visualize the brachial plexus and 40 ml of 0.25% bupivacaine solution was deposited around the brachial plexus in a graded manner. In Group (NS), the needle was inserted 1-1.5 cm above mid-point of clavicle. Once hand or wrist motion was detected at a current intensity of less than 0.4 mA 40 ml of 0.25% bupivacaine was administered. Onset of sensory and motor block of radial, ulnar and median nerves was recorded at 5-min intervals for 30-min. Block execution time, duration of block (time to first analgesic), inadvertent vascular puncture, and neurological complications were taken as the secondary outcome variables.
Results:
About 90% patients in US group and 73.1% in NS group, had successful blocks P = 0.028. The onset of block was faster in the Group US as compared to Group NS and this difference was significant (P 0.007) only in the radial nerve territory. The mean duration of the block was longer in Group US, 286.22 ± 42.339 compared to 204.37 ± 28.54-min in Group NS (P < 0.05). Accidental vascular punctures occurred in 7 patients in the NS group and only 1 patient in the US group.
Conclusion:
Ultrasound guidance for supraclavicular brachial plexus blockade provides a block that is faster in onset, has a better quality and lasts longer when compared with an equal dose delivered by conventional means.
Keywords: Nerve stimulation, supraclavicular blocks, ultrasound guidance
Introduction
Though the invention of the nerve stimulator (NS) provided the advantage of localizing nerves, regional anesthesia still remained a blind procedure. The use of the ultrasonograph (USG) for performance of supraclavicular brachial plexus block was described for The first time in 1978.[1] This heralded a new era in regional anesthesia, wherein successive anesthesiologists established its advantages in their clinical practice.[2] Regional anesthesia procedures no longer were blind and a calculated amount of the drug could be administered at the designated site under real-time observation.
The aim of our study was to analyze the difference in efficacy, safety and complications, while performing supra clavicular brachial plexus nerve blocks by using anatomical landmarks with a nerve locator as compared to ultrasound (US) guidance. The objectives of the study were to study the feasibility and ease of learning supra clavicular brachial plexus blocks using the two methods.
Material and Methods
This prospective, randomized study was conducted on 102 American Society of Anesthesiologists (ASA) Grade I/II patients of either sex from 16 to 60 years of age, admitted for elective upper limb surgery. Informed consent and Institutional Ethics Committee approval was obtained.
A sample size of 50 patients per group was calculated based on a review of literature[3] to show a significant difference between groups, assuming 85% successful blocks in Group USG and 78% successful blocks in Group NS.[4] Keeping a probability of Type 1 error of 0.05 and a probability of Type 2 error of 0.2 as acceptable.
Exclusion criteria were presence of coagulopathy, infection at the injection site, and allergy to local anesthetics, severe pulmonary pathology, and age less than 16 years, mental incapacity precluding informed consent, a body mass index more than 35, or preexisting neuropathy in the operative limb.
A computer generated sequence of numbers was used for randomization and a sealed envelope used for allocation into the two groups.
In both groups, the block was performed by the authors who had an experience of performing 10 successful US-guided brachial plexus blocks. Minimum mandatory monitoring standards were adhered to during the performance of the blocks. Intravenous access was ensured in the arm contralateral to the operative arm. Premedication was administered intravenously (0.03 mg/kg midazolam) to both the groups. In Group US, supraclavicular brachial plexus block was performed under US. In Group NS block, was performed using conventional landmark technique and NS guidance.
The patient was placed supine with the head turned away from the side of block. Following skin preparation the skin 1-1.5 cm above the mid-point of clavicle was infiltrated with injection lignocaine 2% lateral to the pulsations of the sub-clavian artery, if palpable.
In group ultrasound guidance
“Titan” Portable US Machine, Sonosite, Inc. Kensington, UK with a 9.0 MHz probe was used. US gel and a sterile sheath was used for all cases. The image of sub-clavian artery in short axis (cross-sectional view) was obtained. The nerve bundles of brachial plexus appear in groups as 3-4 hypo-echoic (dark) circles anterior and lateral to the sub-clavian artery. A scan prior to needle insertion [Figure 1] shows the exact nerve location, and is thus helpful in defining the desired site, angle and path of needle penetration. A 22 G insulated Teflon coated needle (Stimuplex® D 50 mm, B.Braun, Germany) was then taken and flushed with 10 ml 5% dextrose solution.
Figure 1.

Scout scan of supraclavicular brachial plexus
Once the needle is seen as hyperechoic (bright) line on the screen in close vicinity of the nerves a check withdrawal of the syringe plunger was done. Subsequently, 10 ml of 0.25% bupivacaine solution was injected in a graded manner.
After visually confirming the spread of the drug around the nerve bundle with US, a further 30 ml of the drug was injected. Onset of sensory and motor block of radial, ulnar and median nerves was recorded at 5 min intervals for 30 min.
In group nerve stimulator
Following cleaning, draping and local infiltration, the needle was inserted 1-1.5 cm cephalad to the mid-point of the clavicle. The sub-clavian artery pulsations were palpated to avoid a puncture and the inter-scalene groove palpated to trace the path of the plexus for needle insertion. The block was administered using NS specific, sterile, Teflon-isolated needles (22G insulated needle Stimuplex® D 50 mm B.Braun Germany). A volume of 10 ml syringe filled with 5% dextrose was attached and the needle flushed. The NS was set with pulse duration of 0.15 ms, a current intensity of 1 mA, and a frequency of 2 Hz. Once wrist or hand motion was elicited, the stimulating intensity was progressively reduced to less than 0.4 mA maintaining good twitch. A volume of 40 ml of 0.25% bupivacaine solution was then injected. Onset of the brachial plexus block was recorded in a similar fashion as for Group US. Evaluation of sensory and motor block was performed every 5-min in all nerve territories over a 30-min period.
Block execution time, onset of sensory block, duration of block (time to first analgesic), inadvertent vascular puncture and neurological complications were taken as the secondary outcome variables.
A blinded observer, who was not present during block placement, recorded the onset of sensory and motor blocks in the distribution of the four nerves (the musculo-cutaneous, median, radial, and ulnar terminal nerves) every 5-min. Motor block was evaluated using forearm flexion-extension, thumb and second digit pinch, and thumb and fifth digit pinch.[5] Sensory block was evaluated by comparing the cold sensation elicited by ice in the central sensory region of each nerve with the same stimulus delivered to the contralateral side.
In case of pain prior to surgery, supplementary wrist or elbow blocks were administered. If the patient still experienced pain despite supplementation, general anesthesia was induced, and the block was considered as failed.
These patients were monitored for time to execution of block, that is, the interval between the first needle insertion and its removal at the end of the block.
The time for onset of block that is, the time to loss of cold sensation in the central sensory region of each nerve as mentioned above was measured. Motor and sensory components of the block were assessed as already described. The requirement of supplementary analgesia and general anesthesia was also recorded. The patients were followed-up in the ward for 24 h for the time to requirement of first supplemental analgesia and complications, if any. The time to requirement of supplemental analgesia was taken as the duration of the block.
Statistical analysis
The software Statistical Package for Social Sciences (SPSS) version 17 (IBM, SPSS, Chicago, USA) was used for statistical analysis. All results were expressed as mean ± standard deviation, or as a percentage. Quantitative variables were compared by two sample Student's t-test, and qualitative variables were compared by the Fisher exact test or the Chi-squared test (with Yates correction) where appropriate. P < 0.05 was considered as significant.
Results
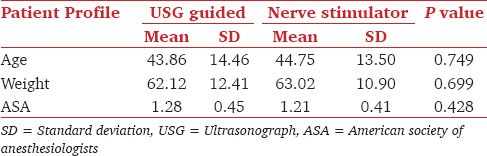
In the present study, 102 patients were randomly assigned to be administered supraclavicular brachial plexus block. There was no significant difference in the demographic characteristics of the two study groups as shown in Table 1. Using independent samples t-test for equality of means, the two groups were comparable in terms of age, ASA status and weight (P > 0.05). There was also no significant difference as regards to gender using the Fischer's exact test (P > 0.773).
Table 1.
Group statistics
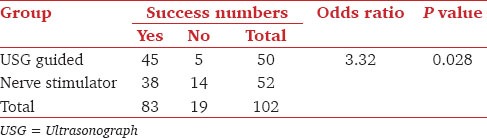
In Group US, 45 out of 50 (90%) patients had developed successful block, compared with 38 of 52 (73.1%) in Group NS including blocks requiring to be supplemented by additional nerve blocks at the wrist (1 patient in the US group and 2 patients in the NS group) as shown in Table 2. This difference was statistically significant at 95% confidence interval odds ratio 3.32 using the Pearson Chi-square test (absolute value 4.816) P = 0.028. General anesthesia was required for the failed blocks in 5 patients of US group and 14 patients of the NS group.
Table 2.
Success of supraclavicular block in study groups
The average time necessary to perform the block (block execution time) was significantly shorter in Group US than in Group NS (8.14 vs. 10.63-min) [Table 3].
Table 3.
BE time within groups
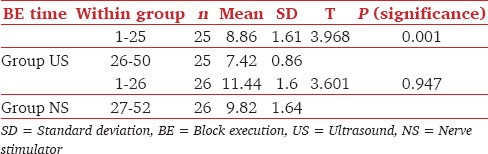
The block execution times in the first and last 25 patients of Group US and first and last 26 patients of Group NS were calculated and compared within the groups [Table 3]. Only Group US had significantly shorter execution times in the second half of patients as compared with the first half (t − 3.9685.8, P − 0.001). In Group NS, there was no significant difference between the two groups (t − 3.601, P − 0.947).
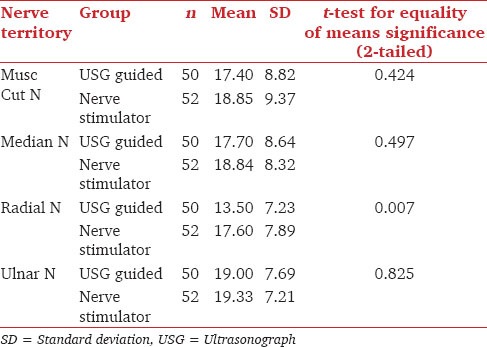
The onset of block ranged from 17.4-min in the musculo-cutaneous N territory to a max of 19.32-min in the ulnar N territory. It was faster in Group US compared to Group NS though the difference was not statistically significant (P > 0.05) except for the radial nerve territory where the difference was significant (P 0.007) as shown in Table 4.
Table 4.
Onset of block in study groups
The mean duration of the block was longer in Group US, 286.22 ± 42.339 compared to 204.37 ± 28.54-min in Group NS, P < 0.05. Duration of block in study groups is shown in Figure 2.
Figure 2.
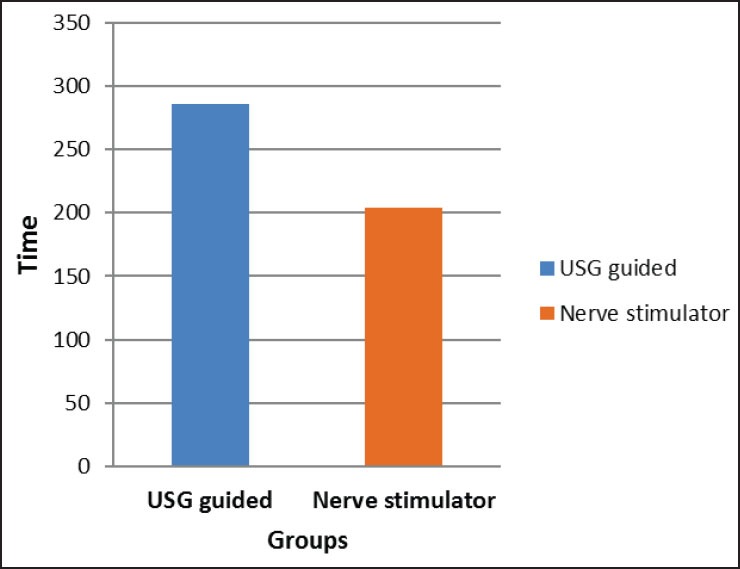
Duration of supraclavicular block in study groups
Seven patients (13.46%) had a vascular puncture in NS group which was confirmed by a flash of blood in the syringe on aspiration. One patient (2%) in Group US had a vascular puncture detected on aspiration prior to injection of the drug and the difference was statistically significant (P < 0.0001). None of the patients in the two groups had any neurological complications.
Discussion
This prospective randomized study demonstrates that US enabled a more accurate delivery of the drug at the site of action (the brachial plexus) under direct vision in real-time. This resulted in a statistically significant number of successful blocks, which were of better quality and intensity.
The success of block with US in the present study was 90%. This compared favorably with the studies published in the past, which achieved 85% success. Moreover, it was confirmed that using the same concentration and volume of bupivacaine solution, both the onset and duration of anesthesia were better in the US group.[5]
The onset of supraclavicular block in our study group ranged from a mean of 13.5-min in the musculo-cutaneous nerve territory to a mean of 19.00 min in the ulnar group which was similar to Kapral et al.[6] who achieved anesthetic conditions in 10-20 min. In the present study, though the onset of block was faster in the US group, statistical significance was attained only in the radial nerve territory and we did not consider the difference clinically significant as a good block ensued in both the groups by approximately 20 min.
The duration of anesthesia was significantly longer in the US group in comparison to the NS group. This could be ascribed to the more precise delivery of drug closer to the brachial plexus. Abrahams et al. have observed that the US group had a combined mean increase in block duration of 25% as compared with NS group,[7] which is similar to our study. In fact in two recent reviews the authors have concluded that there is evidence suggesting a reduction of the volume of local anesthetics required for US-guided upper extremity blockades as compared to nerve stimulation.[8,9]
Though our experience in performance of brachial plexus block was limited, identification of the brachial plexus under US did not pose a problem. This correlates with the views expressed in other similar studies.[5,10,11] In a retrospective analysis of residents trained by two different needle guidance methods the results suggested that US permits higher success rates after fewer blocks, especially for residents with no previous training in nerve stimulation.[12]
A very interesting finding that we noticed in the within group analysis was that the block execution time decreased further in the latter half of US-guided blocks performed as compared to the first half. In contrast, the same was not observed in the NS group. This difference was statistically significant, P = 0.001 for the US group as compared to 0.947 for the NS group [Table 3]. Meaning therefore that there was scope of learning and improving upon US-guided nerve blocks as the operator got more conversant with the technique. While with the NS group since the operators were already conversant with the technique there wasn’t any decrease in the block execution time.
Pneumothorax is a known complication of supraclavicular nerve blocks. The incidence varies from 0.6% to 5%, respectively.[4] There was, however, no clinical evidence of pneumothorax in our study groups. Chest radiographs were not obtained but all the patients were followed-up in the ward. US in the performance of brachial plexus block has been described to be effective in lowering the incidence of pneumothorax.[4,10]
Vascular puncture is another complication of the brachial plexus block. The occurrence of seven vascular punctures in the NS group, while only one in the USG group during check aspiration suggests that US prevents vascular puncture. This is important for the anesthesiologist as intra — vascular injection of local anesthetic solutions can cause neuro and/or cardiac toxicity.[13] The incidence of diaphagramatic palsy is 1%[14] and can be detected clinically by reported respiratory discomfort after the block confirmed on chest radiograph which demonstrates an elevated hemidiaphragm compatible with ipsilateral phrenic nerve block. None of our patients showed this complication. Post operatively the patients weren’t subjected to X-ray chest posterioranterior view for evidence of pneumothorax or diaphragmatic palsy, so minimal pneumothoraces and diaphragmatic palsies could have been missed out.
Despite this limitation this study demonstrates the usefulness of US for the learning and execution of supraclavicular block. US imaging techniques should become an integral part of residency training in anesthesia.
Conclusion
Ultrasound guidance for supra clavicular brachial plexus blockade provides a block that is safer, faster in onset and is more accurate thus lasting longer and of a better quality when compared with an equal dose delivered by conventional means. Moreover, as one starts performing the technique, the execution time decreases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.la Grange P, Foster PA, Pretorius LK. Application of the Doppler ultrasound bloodflow detector in supraclavicular brachial plexus block. Br J Anaesth. 1978;50:965–7. doi: 10.1093/bja/50.9.965. [DOI] [PubMed] [Google Scholar]
- 2.Marhofer P, Willschje H, Greher M, Kapral S. New perspectives in regional anesthesia: The use of ultrasound — Past, present, and future. Can J Anesth. 2005;52(Suppl):R1–6. [Google Scholar]
- 3.Moorthy SS, Schmidt SI, Dierdorf SF, Rosenfeld SH, Anagnostou JM. A supraclavicular lateral paravascular approach for brachial plexus regional anesthesia. Anesth Analg. 1991;72:241–4. doi: 10.1213/00000539-199102000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Chan VW, Perlas A, Rawson R, Odukoya O. Ultrasound-guided supraclavicular brachial plexus block. Anesth Analg. 2003;97:1514–7. doi: 10.1213/01.ANE.0000062519.61520.14. [DOI] [PubMed] [Google Scholar]
- 5.Williams SR, Chouinard P, Arcand G, Harris P, Ruel M, Boudreault D, et al. Ultrasound guidance speeds execution and improves the quality of supraclavicular block. Anesth Analg. 2003;97:1518–23. doi: 10.1213/01.ANE.0000086730.09173.CA. [DOI] [PubMed] [Google Scholar]
- 6.Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994;78:507–13. doi: 10.1213/00000539-199403000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Abrahams MS, Aziz MF, Fu RF, Horn JL. Ultrasound guidance compared with electrical neurostimulation for peripheral nerve block: A systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2009;102:408–17. doi: 10.1093/bja/aen384. [DOI] [PubMed] [Google Scholar]
- 8.Koscielniak-Nielsen ZJ, Dahl JB. Ultrasound-guided peripheral nerve blockade of the upper extremity. Curr Opin Anaesthesiol. 2012;25:253–9. doi: 10.1097/ACO.0b013e32835069c2. [DOI] [PubMed] [Google Scholar]
- 9.Vermeylen K, Engelen S, Sermeus L, Soetens F, Van de Velde M. Supraclavicular brachial plexus blocks: Review and current practice. Acta Anaesthesiol Belg. 2012;63:15–21. [PubMed] [Google Scholar]
- 10.Chan VW, Brull R, McCartney CJ, Xu D, Abbas S, Shannon P. An ultrasonographic and histological study of intraneural injection and electrical stimulation in pigs. Anesth Analg. 2007;104:1281–4. doi: 10.1213/01.ane.0000250915.45247.24. [DOI] [PubMed] [Google Scholar]
- 11.Marhofer P, Chan VW. Ultrasound-guided regional anesthesia: Current concepts and future trends. Anesth Analg. 2007;104:1265–9. doi: 10.1213/01.ane.0000260614.32794.7b. [DOI] [PubMed] [Google Scholar]
- 12.Luyet C, Schüpfer G, Wipfli M, Greif R, Luginbühl M, Eichenberger U. Different learning curves for axillary brachial plexus block: Ultrasound guidance versus nerve stimulation. Anesthesiol Res Pract 2010. 2010:309462. doi: 10.1155/2010/309462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Denson DD, Mazoit JX. Physiology, pharmacology of local anesthetics. In: Raj PP, editor. Clinical Practice of Regional Anesthesia. Churchill Livingstone; 1991. pp. 73–106. [Google Scholar]
- 14.Perlas A, Lobo G, Lo N, Brull R, Chan VW, Karkhanis R. Ultrasound-guided supraclavicular block: Outcome of 510 consecutive cases. Reg Anesth Pain Med. 2009;34:171–6. doi: 10.1097/AAP.0b013e31819a3f81. [DOI] [PubMed] [Google Scholar]


