Abstract
Purpose of this Study :
To review the characteristics, concomitant injuries and mortality in children with polytrauma and associated pelvic fractures treated in a Level-I Trauma Centre.
Materials and Methods :
Between December 2003 and November 2013, 49 children with an Injury Severity Score (ISS) of 16 or greater and a pelvic fracture met the inclusion criteria and were evaluated. The mortality, transfusion requirements and length of intensive care unit stay were correlated with the ISS, Abbreviated Injury Scale, concomitant limb and spine fractures, and type of pelvic ring injury (AO/OTA classification).
Results :
The mean ISS at presentation was 31.4 (range 16 to 57). 19 (38.7%) patients sustained a Type A, 27 (55.1%) a Type B and 3 (6.2%) a Type C injury. Head and face trauma was present in 33 (67.3%) cases. Blood transfusion during the resuscitation process was necessitated in six (12.2%) patients. Thirty-eight (77.5%) patients were managed non-operatively for their pelvic injuries. The mean duration of hospital stay was 23.9 days (range 1 to 146 days). In this cohort of polytrauma paediatric patients there were five (10.2%) mortalities (all suffered an associated head trauma ) within 30 days from the initial injury.
Conclusion:
Severe head injury and a high ISS are significantly associated with mortality in children with pelvic fractures. These patients have a high incidence of concomitant spine and chest injuries Hemorrhage due to pelvic injuries is rare. Severe head injuries predict a longer ICU stay in this population.
Keywords: Children, mortality, pelvic fracture, polytrauma
INTRODUCTION
Trauma is the leading cause of death in children [1-3]. The incidence of pelvic fractures in the pediatric population has been estimated at 2.7% [4]. Motor Vehicle Collisions followed by falls have been reported as the two most common causes of pelvic ring injuries in children [5]. The average Injury Severity Score (ISS) of a child with pelvic ring injury has been reported to be ≥16 [6-11].
There is a range of reported rates of mortality associated with pelvic ring injuries in the pediatric population. In a large epidemiological study Galano et al. [3] reported a mortality rate of 0.55% for children with pelvic fractures. On the other hand, Ismail et al. [12] stated a mortality rate of 5% in this population. The above values refer to the overall mortality rates and not mortality associated with multiply injured patients. Nevertheless there are several reports in the contemporary orthopaedic trauma literature underlining the fact that mortality is not due to fatal haemorrhage but rather is usually associated with a concomitant severe head injury [6, 13]. High overall ISS and the type of pelvic fracture have also been associated with increased mortality [6].
The objective of this study was to review and report on the characteristics, concomitant injuries and associated early mortality of the polytrauma children (ISS≥16) with pelvic ring injury that were treated in a Level-I Trauma Centre within a 10-year period.
PATIENTS AND METHODS
We performed a retrospective review of the prospectively populated national Trauma Audit and Research Network (TARN) database in a Level-I Trauma Centre. Between December 2003 and November 2013 the data of all polytrauma patients that suffered a pelvic fracture were reviewed. Patient identification and data collection was therefore conducted retrospectively from a prospectively populated database. The query “pelvic fracture” was used to identify the patients. The results were then validated by comparing them with the local hospital database. Inclusion criteria were patients less than 16 years of age, presented with ISS > 16 and a pelvic ring injury. Exclusion criteria were adult patients (age>16 years), non-polytrauma patients (ISS<16) and patients without a pelvic ring injury and incomplete files.
Patient demographics including age, sex and mechanism of injury were collected. Admission data including ISS, Abbreviated Injury Scale (AIS) of all anatomic areas, type of pelvic injury according to AO/OTA [14] classification, concomitant injuries, length of hospital stay, length of Intensive Care Unit (ICU) stay, blood transfusion requirements, type and number of surgical procedures, and mortality within the first 30 days from the injury were recorded. Two fellowship-trained orthopaedic trauma surgeons reviewed patients’ notes. Any discrepancies were resolved by consensus.
The mortality, transfusion requirements, length of hospital and intensive care unit length stay were correlated with the ISS, AIS, concomitant limb and spine fractures, and type of pelvic injury. Univariate assessment involved using the Fisher exact test for categorical data and the independent t-test to compare means of continuous variables. Statistical significance was assumed when a p value was calculated to be less than 0.05.
RESULTS
Out of 56 patients, 49 (25 males) patients with a mean age of 10.9 years (range 0.7 – 16.9 years) met the inclusion criteria and formed the basis of this study. Table 1 provides details of each case and Table 2 summarises patient and injury demographics. The vast majority i.e. 44 out of 49 (89.7%) patients were injured as a result of a motor vehicle collision. The mean ISS at presentation was 31.4 (range 16 to 57). Of the 49 pelvic fractures, 19 (38.7%) were classified as Type A, 27 (55.1%) as Type B and 3 (6.2%) as Type C. All patients had a plain radiograph of the pelvis as a baseline investigation. A CT scan was subsequently performed in all patients. This was the standardised approach to all polytrauma patients in our institution for the time period that these patients were initially assessed. Two patients sustained a concomitant minimally displaced acetabular fracture.
Table 1.
Demographics: patients, injuries and treatment.
| Patient Number | Gender | Age | AIS Head and C-spine | AIS Face | AIS Chest and T-spine | AIS Abdomen and L-spine | AIS Limbs and pelvis | AIS External/ burns | ISS | Limb Fracture | Spine Fracture | Pelvic OTA Classification | Acetabular Fracture | Injury Mechanism | Number of Theatre Visits | Pelvic Fixation | Outcome 30 Days | Inpatient Stay | Critical Care Stay | Blood Units Transfused |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 11.7 | 4 | 0 | 4 | 0 | 2 | 0 | 36 | No | No | B | 0 |
Vehicle incident/ collision |
1 | Dead | 1 | 1 | 0 | |
| 2 | M | 11.3 | 5 | 0 | 3 | 0 | 2 | 0 | 38 | No | No | A | 0 | Vehicle incident/ collision |
1 | Dead | 1 | 0 | 0 | |
| 3 | F | 1.8 | 5 | 2 | 0 | 2 | 4 | 1 | 45 | No | No | B | 0 |
Vehicle incident/ collision |
1 | Dead | 1 | 1 | 1 | |
| 4 | F | 13.2 | 5 | 0 | 3 | 4 | 2 | 0 | 50 | No | No | B | 0 | Vehicle incident/ collision |
1 | Dead | 1 | 1 | 0 | |
| 5 | F | 15.7 | 5 | 2 | 4 | 4 | 4 | 0 | 57 | Yes | No | B | 0 |
Vehicle incident/ collision |
0 | Dead | 1 | 1 | 9 | |
| 6 | F | 8.4 | 3 | 0 | 0 | 0 | 3 | 0 | 18 | No | No | A | 0 | Vehicle incident/ collision |
0 | Alive | 5 | 1 | 0 | |
| 7 | M | 2.8 | 3 | 0 | 0 | 0 | 3 | 0 | 18 | No | No | B | 0 |
Vehicle incident/ collision |
0 | Alive | 6 | 2 | 0 | |
| 8 | M | 8.3 | 0 | 0 | 3 | 0 | 3 | 1 | 19 | No | No | B | 0 | Vehicle incident/ collision |
0 | Alive | 3 | 0 | 0 | |
| 9 | F | 15.3 | 0 | 0 | 0 | 0 | 4 | 0 | 16 | Yes | No | B | 0 |
Fall more than 2m |
1 |
EXFIX and then ORIF (PS plating and iliac wing plating) |
Alive | 11 | 0 | 0 |
| 10 | F | 16.9 | 0 | 0 | 0 | 0 | 4 | 0 | 16 | No | No | B | 0 | Vehicle incident/ collision |
1 | EXFIX,SI | Alive | 10 | 3 | 0 |
| 11 | M | 2.8 | 0 | 0 | 0 | 0 | 4 | 0 | 16 | No | No | B | 0 |
Vehicle incident/ collision |
1 | EXFIX | Alive | 7 | 2 | 0 |
| 12 | M | 8.7 | 0 | 0 | 0 | 0 | 4 | 0 | 16 | No | No | B | 0 | Vehicle incident/ collision |
0 | Alive | 4 | 0 | 0 | |
| 13 | F | 13.9 | 0 | 0 | 0 | 0 | 4 | 1 | 17 | No | No | C | 1 |
Vehicle incident/ collision |
2 | ORIF | Alive | 23 | 0 | 0 |
| 14 | M | 12.1 | 0 | 0 | 0 | 0 | 4 | 1 | 17 | No | No | B | 0 | Vehicle incident/ collision |
0 | Alive | 3 | 0 | 0 | |
| 15 | M | 13.3 | 0 | 0 | 3 | 0 | 3 | 1 | 19 | Yes | No | A | 0 |
Vehicle incident/ collision |
2 | Alive | 11 | 1 | 0 | |
| 16 | M | 7.8 | 0 | 0 | 3 | 0 | 3 | 1 | 19 | No | No | A | 0 | Vehicle incident/ collision |
0 | Alive | 4 | 2 | 0 | |
| 17 | M | 16.5 | 0 | 0 | 0 | 2 | 4 | 1 | 21 | No | No | B | 0 |
Vehicle incident/ collision |
1 | EXFIX, SI | Alive | 14 | 0 | 0 |
| 18 | M | 16.1 | 4 | 0 | 0 | 0 | 2 | 1 | 21 | No | No | B | 0 | Vehicle incident/ collision |
1 | Alive | 14 | 7 | 0 | |
| 19 | F | 13.9 | 0 | 2 | 3 | 2 | 3 | 1 | 22 | No | No | B | 0 |
Vehicle incident/ collision |
0 | Alive | 6 | 1 | 0 | |
| 20 | M | 3.3 | 2 | 0 | 3 | 0 | 3 | 1 | 22 | Yes | No | A | 0 | Vehicle incident/ collision |
1 | Alive | 10 | 2 | 2 | |
| 21 | M | 7.5 | 2 | 0 | 3 | 0 | 3 | 1 | 22 | Yes | No | A | 0 |
Vehicle incident/ collision |
3 | Alive | 7 | 1 | 0 | |
| 22 | M | 16.9 | 3 | 2 | 3 | 0 | 2 | 1 | 22 | No | No | A | 1 | Vehicle incident/ collision |
1 | Alive | 9 | 2 | 0 | |
| 23 | F | 9.8 | 4 | 2 | 0 | 0 | 2 | 1 | 24 | Yes | No | A | 0 |
Vehicle incident/ collision |
2 | Alive | 34 | 5 | 0 | |
| 24 | M | 5.1 | 0 | 0 | 4 | 2 | 2 | 0 | 24 | No | No | A | 0 | Vehicle incident/ collision |
0 | Alive | 7 | 2 | 0 | |
| 25 | M | 15.3 | 0 | 0 | 0 | 0 | 5 | 0 | 25 | No | No | C | 0 | Crush | 1 | ORIF iliac wing | Alive | 10 | 0 | 0 |
| 26 | F | 16.6 | 0 | 0 | 3 | 0 | 4 | 1 | 26 | No | No | B | 0 | Vehicle incident/ collision |
1 | EXFIX | Alive | 8 | 0 | 0 |
| 27 | F | 15.8 | 4 | 2 | 0 | 0 | 3 | 1 | 29 | Yes | No | B | 0 |
Vehicle incident/ collision |
2 | EXFIX, SI | Alive | 51 | 13 | 0 |
| 28 | F | 10.6 | 5 | 0 | 0 | 0 | 2 | 0 | 29 | No | No | A | 0 | Vehicle incident/ collision |
2 | Alive | 146 | 146 | 0 | |
| 29 | F | 14.4 | 4 | 0 | 3 | 0 | 2 | 1 | 29 | No | No | A | 0 |
Vehicle incident/ collision |
0 | Alive | 12 | 2 | 0 | |
| 30 | F | 11.5 | 3 | 0 | 4 | 0 | 2 | 1 | 29 | No | No | A | 0 | Vehicle incident/ collision |
0 | Alive | 18 | 2 | 0 | |
| 31 | M | 11.7 | 0 | 0 | 4 | 2 | 3 | 0 | 29 | Yes | Yes | A | 0 |
Vehicle incident/ collision |
3 | Alive | 12 | 1 | 0 | |
| 32 | F | 3.5 | 0 | 0 | 0 | 4 | 4 | 0 | 32 | No | No | B | 0 | Vehicle incident/ collision |
8 | EXFIX | Alive | 65 | 18 | 1 |
| 33 | M | 16.6 | 4 | 0 | 0 | 0 | 4 | 1 | 33 | No | No | B | 0 |
Vehicle incident/ collision |
0 | Alive | 3 | 0 | 0 | |
| 34 | F | 8.8 | 4 | 2 | 3 | 3 | 2 | 1 | 34 | Yes | No | B | 0 |
Vehicle incident/ collision |
1 | Alive | 14 | 0 | 0 | |
| 35 | F | 3 | 4 | 0 | 3 | 3 | 2 | 0 | 34 | No | No | B | 0 | Fall more than 2m |
0 | Alive | 3 | 3 | 0 | |
| 36 | M | 5.6 | 3 | 0 | 3 | 4 | 3 | 1 | 34 | Yes | Yes | B | 0 |
Vehicle incident/ collision |
4 | Alive | 36 | 0 | 0 | |
| 37 | M | 13.3 | 4 | 0 | 3 | 2 | 3 | 1 | 34 | Yes | No | A | 0 | Vehicle incident/ collision |
0 | Alive | 1 | 2 | 0 | |
| 38 | F | 12.5 | 4 | 2 | 4 | 0 | 2 | 1 | 36 | No | No | A | 0 |
Vehicle incident/ collision |
3 | Alive | 40 | 13 | 1 | |
| 39 | F | 16.3 | 0 | 0 | 4 | 3 | 4 | 1 | 41 | Yes | Yes | A | 0 | Fall more than 2m |
1 | Alive | 57 | 5 | 0 | |
| 40 | F | 0.7 | 4 | 0 | 3 | 4 | 2 | 1 | 41 | No | No | B | 0 |
Vehicle incident/ collision |
0 | Alive | 7 | 2 | 0 | |
| 41 | M | 16.6 | 3 | 0 | 3 | 4 | 4 | 1 | 41 | No | Yes | A | 0 | Vehicle incident/ collision |
1 | Alive | 15 | 1 | 0 | |
| 42 | M | 12.5 | 4 | 0 | 3 | 3 | 4 | 0 | 41 | No | No | B | 0 |
Vehicle incident/ collision |
1 | Alive | 33 | 28 | 0 | |
| 43 | F | 14.3 | 5 | 0 | 0 | 0 | 4 | 1 | 42 | Yes | Yes | B | 0 | Vehicle incident/ collision |
1 | EXFIX | Alive | 93 | 12 | 0 |
| 44 | M | 3.5 | 5 | 2 | 3 | 0 | 3 | 1 | 43 | No | Yes | B | 0 |
Vehicle incident/ collision |
0 | Alive | 110 | 59 | 0 | |
| 45 | F | 16 | 4 | 0 | 3 | 2 | 5 | 0 | 50 | Yes | No | C | 0 | Vehicle incident/ collision |
2 | ORIF (iliac wing plating and RP screw) |
Alive | 53 | 2 | 1 |
| 46 | M | 14 | 5 | 3 | 4 | 0 | 3 | 1 | 50 | Yes | No | B | 0 |
Vehicle incident/ collision |
1 | Alive | 22 | 2 | 0 | |
| 47 | M | 12.9 | 4 | 0 | 5 | 3 | 2 | 0 | 50 | No | No | A | 0 | Vehicle incident/ collision |
1 | Alive | 52 | 7 | 0 | |
| 48 | F | 11.9 | 5 | 2 | 0 | 0 | 5 | 1 | 54 | Yes | No | B | 0 |
Vehicle incident/ collision |
0 | Alive | 70 | 24 | 0 | |
| 49 | M | 3.2 | 3 | 0 | 4 | 5 | 4 | 1 | 57 | Yes | Yes | A | 0 | Crush | 2 | Alive | 48 | 17 | 0 |
ISS - Injury Severity Score, AIS - Abbreviated Injury Scale, EXFIX – pelvic external fixation, ORIF – open reduction and internal fixation, SI – iliosacral screw, PS – pubic symphysis, RP – retrograde pubic.
Table 2.
Patient and injury demographics.
| Number | |
|---|---|
| Gender | 25 males, 24 females |
| Mean Age (years) | 10.9 (0.7-16.9) |
| Mechanism of Injury | 44 Moving Vehicle Accidents 3 Falls from Height 2 Crush Injuries |
| Pelvic injuries | 19A, 27B, 3C |
| Acetabular fractures | 2 |
| Mean ISS | 31.4 (16-57) |
Associated injuries were very common (Table 3). Head and face trauma was encountered in 33 (67.3%) cases whilst chest and thoracic spine injuries were evident in 30 (61.2%) cases. Urogenital injuries were present in three (6.1%) cases. Seventeen (34.7%) patients presented with a limb fracture (Table 4). The commonest fractures were femoral and tibial (7 cases each, 14.2%).
Table 3.
Concomitant injuries.
| Number | |
|---|---|
| Head/Face | 33 |
| Chest/Thoracic Spine | 30 |
| Abdomen/Lumbar Spine | 19 |
| Limb fracture | 17 (see Table 4) |
| Urological | 3 (3 urethral lacerations and one bladder laceration) |
| Cord Neurology | 4 |
Table 4.
Fractures by site and their management.
| Number | Operative Fixation | |
|---|---|---|
| Clavicle | 4 | |
| Humerus | 3 | 1 K-wiring, 1 ORIF |
| Radius/Ulna | 2 | 1 K-wiring |
| Femur | 7 | 4 ORIF, 1 nail, 1 external fixation then ORIF |
| Tibia/Fibula | 7 | 2 nail, 3 ORIF, 2 circular fixator |
| Foot | 1 | |
| Spine | 7 |
Blood transfusion during the immediate resuscitation process was required in six (12.2%) patients. These patients needed a mean of 2.5 units of blood (range 1-9). None of them required embolization to control haemorrhage. Two of these patients sustained a Type A injury, three sustained Type B injuries and one sustained Type a C injury. The mean ISS of the patients requiring a transfusion was 40.3 whilst patients not requiring transfusion had a mean ISS of 29.8 (p=0.025). Specific types of pelvic injuries or other concomitant injuries were not significantly associated with a requirement for transfusion (p>0.05). The six patients that required a blood transfusion had a mean admission serum haemoglobin level of 8.7g/dL and a mean packed cell volume (PCV) of 0.26 on admission. These levels had increased to a mean serum haemoglobin level of 10.8g/dL and a PCV of 0.32 on discharge.
Thirty-eight (77.5%) patients were managed non-operatively for their pelvic injuries (Table 5). Of the eleven (22.5%) patients that were managed operatively eight had suffered a Type B and three a Type C injury respectively. Four patients with a type B injury had an external fixation applied as a definitive mode of surgical stabilisation. The external fixation was maintained for three weeks in all of these patients. One patient with a Type B injury was provisionally stabilised with an external fixator that was subsequently removed and definitive stabilised with internal fixation. Three patients with Type C injuries were managed with open reduction and internal fixation. The characteristics of the patients were similar in both groups (operative and no-operative), (Table 6).
Table 5.
Operative treatment (excluding patients that died).
| Number | Age 0-10 Years | Age 10-14 Years | Age 14-17 Years | |
|---|---|---|---|---|
| External fixation | 4B | 2B | 0 | 2B |
| External fixation then Internal fixation | 1B | 0 | 0 | 1B |
| External fixation and internal fixation | 3B | 0 | 0 | 3B |
| Internal fixation | 3C | 0 | 1C | 2C |
| Non-operative | 38 | 15 | 12 | 6 |
| Mean time to first operation from ED presentation (hours) | 42.4 (3-137) | 32.9 (3-62) | 7.5 (7.5) | 49.1 (3-137) |
| Mean number Of theatre visits | 1.1 (0-8) | 4.5 (1-8) | 2 (2) | 1.3 (1-2) |
| Mean length of inpatient stay (days) | 27.1 (3-146) | 21.8 (3-110) | 33.6 (1-146) | 25.7 (3-57) |
| Mean length of critical care stay (days) | 8.9 (0-146) | 6.8 (0-59) | 17.5 (1-146) | 3.4 (0-13) |
Table 6.
Operative vs non-operative fixation of pelvic injuries (excluding patients that died).
| Operative Management |
Non-Operative Management | p-Value | |
|---|---|---|---|
| Number | 11 | 33 | |
| Mean Age (Years) | 13.3 | 10.1 | 0.031 |
| Mean ISS | 26.1 | 30.9 | 0.511 |
| Mean AIS head | 1.2 | 2.7 | 0.067 |
| Mean AIS chest | 0.5 | 2.5 | 0.012 |
| Mean AIS abdomen | 0.7 | 1.2 | 0.503 |
| Limb fracture | 4 | 12 | 1.000 |
| Spine fracture | 1 | 6 | 0.659 |
| Transfusion | 2 | 2 | 0.257 |
| Mean inpatient stay | 31.4 | 24.9 | 0.709 |
| Mean ICU stay | 4.5 | 10.3 | 0.456 |
| Pelvic Fracture | <0.001 | ||
| A | 0 | 18 | |
| B | 8 | 15 | |
| C | 3 | 0 |
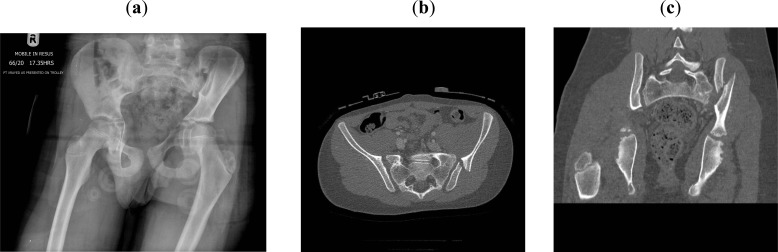
An example of a 10-year-old patient with a Type C injury (equivalent to Lateral Type II according to Young and Burgess classification [15]) is shown in Figs. (1-3).
Fig. (1).
Preoperative Anteroposterior pelvic radiograph (a), axial (b) and coronal (c) CT scans demonstrating a type C injury of the left hemipelvis, equivalent to Lateral Compression type II injury (crescent fracture) in a 10-year-old boy.
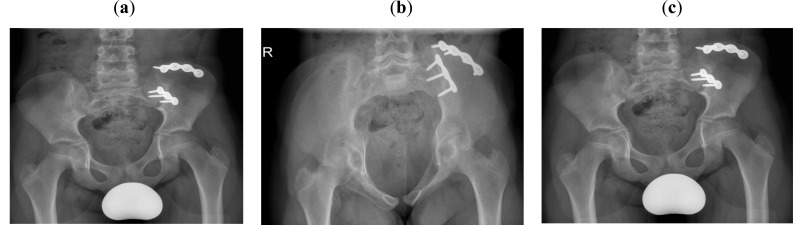
Fig. (3).
Anteroposterior (a), inlet (b) and outlet (c) radiographs of the same patient at four months postoperatively.
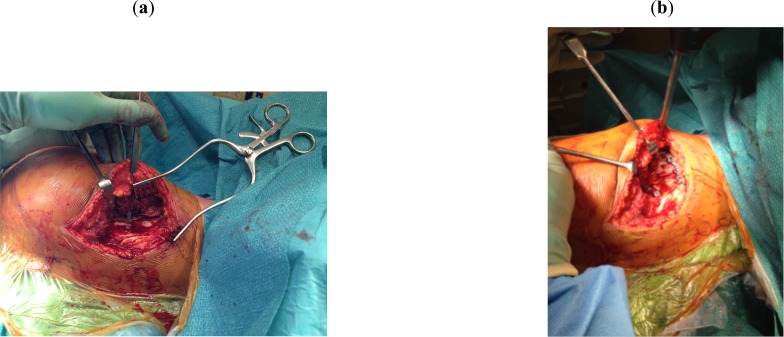
The patient was taken to theatre on the second day after his admission. Following standard preparation and general anesthesia he was placed lateral on a flat radiolucent table. An 8 cm curvilinear incision was made 1 cm lateral to the Posterior Superior Iliac Spine. The gluteal musculature was detached from the external surface of the iliac wing after the release of the inferior extension of the gluteus maximus from the lumbodorsal fascia. The outer surface of the ilium was exposed to visualise the fracture line. Reduction was achieved using clamps. The fracture was stabilised using two 3.5 mm reconstruction plates.
The mean duration of hospital stay was 27.1 days (range 3 to 146 days). Excluding the patients who died, the patients who had an operation stayed in the hospital for a mean of 34.3 days (range 7 to 93 days) and in ICU for a mean of 4.5 days (range 0 to 12 days). The patients who were managed non-operatively for their pelvic injuries hospitalised for 24.9 days (1-146 days) and stayed in ICU for 10.3 days (0-146 days).
In this cohort of polytrauma paediatric patients there were five (10.2%) mortalities within 30 days from the initial trauma. All of these deaths occurred within 24 hours from the initial traumatic event. The non-survivors had a significantly higher mean ISS of 45.2 compared to a mean ISS of 29.5 of the survivors (p=0.007). These patients also had a severe head injury with a mean AIS (head) of 4.8 compared to mean AIS (head) of 2.3 of the patients who survived (p=0.008). The type of the fracture and the other concomitant injuries were not significantly associated with increased mortality (Table 7).
Table 7.
Predictors of mortality.
| Dead | Alive | p-Value | |
|---|---|---|---|
| Number | 5 | 44 | |
| Mean Age (Years) | 10.7 | 10.9 | 0.939 |
| Gender | 4F 1M | 20F 24M | 0.190 |
| Mean ISS | 45.2 | 29.5 | 0.007 |
| Mean AIS head | 4.8 | 2.3 | 0.008 |
| Mean AIS chest | 2.8 | 2.0 | 0.314 |
| Mean AIS abdomen | 2.0 | 1.1 | 0.237 |
| Limb Fracture | 1 | 16 | 0.646 |
| Spine Fracture | 0 | 7 | 1.000 |
| Transfused? | 2 | 4 | 0.107 |
| Pelvic Fracture | 0.479 | ||
| A | 1 | 18 | |
| B | 4 | 23 | |
| C | 0 | 3 |
All mortalities were within 24 hours of presentation due to head injury.
The length of ICU stay was found be associated to head injury as well. Excluding patients that died within the first 24 hours, patients who required an ICU stay of longer than 24 hours were more likely to have an associated head injury (p=0.021), (Table 8).
Table 8.
Predictors of ICU stay (excluding patients that died).
| ICU Stay > 24 hours | ICU Stay < 24 hours | p-Value | |
|---|---|---|---|
| Number | 27 | 17 | |
| Mean Age (Years) | 10.1 | 12.3 | 0.394 |
| Mean ISS | 33.3 | 23.5 | 0.092 |
| Mean AIS head | 3.1 | 1.1 | 0.021 |
| Mean AIS chest | 2.2 | 1.6 | 0.372 |
| Mean AIS abdomen | 1.1 | 1.0 | 0.968 |
| Limb fracture | 6 | 10 | 1.000 |
| Spine fracture | 4 | 3 | 1.000 |
| Transfusion | 3 | 3 | 0.662 |
| Pelvic Fracture | 0.347 | ||
| A | 13 | 5 | |
| B | 13 | 10 | |
| C | 1 | 2 |
Of note is the fact that the characteristics of this cohort remained unchanged when age was taken into account (patients younger and older than 10 year), (Table 9).
Table 9.
Analysis by age (excluding patients that died).
| Age<10 Years | Age>10 Years | p-Value | |
|---|---|---|---|
| Number | 17 | 27 | |
| Mean ISS | 27.8 | 31.1 | 0.469 |
| Mean AIS head | 2.4 | 2.7 | 0.683 |
| Mean AIS chest | 2.3 | 1.9 | 0.517 |
| Mean AIS abdomen | 1.5 | 1.0 | 0.242 |
| Limb fracture? | 6 | 10 | 1.000 |
| Spine fracture? | 3 | 4 | 1.000 |
| Transfusion | 2 | 2 | 0.634 |
| Mean inpatient stay | 21.7 | 29.5 | 0.438 |
| Mean ICU stay | 6.8 | 10.1 | 0.655 |
| Operative fixation of pelvis? | 2 | 9 | 0.159 |
| Pelvic Fracture | 0.347 | ||
| A | 7 | 11 | |
| B | 10 | 13 | |
| C | 0 | 3 |
DISCUSSION
Pelvic ring fractures in children is an indicator of potential injuries to other body areas (16). Despite this general consensus, there are few studies in the current orthopaedic trauma literature reporting on the characteristics, management and mortality associated with these injuries in the setting of polytrauma. Most of the published studies report and analyse the pediatric pelvic trauma irrespective of the ISS [6]. To the best of our knowledge our series is the only one in the contemporary literature that analyses the pelvic injury in the context of the severely multiply injured patient.
The analysis of this cohort reveals that the majority of pelvic injuries in polytrauma patients are rotationally and vertically unstable i.e. type B (55.1%) and C (6.2%) injuries. Blasier et al.(17) reported a 70% incidence of type A and 30% incidence of type B and C injuries whilst Grisoni et al. [13] stated an incidence of 83.3% type A and 16.7% of type B and C injuries. The aforementioned studies though analysed data from children with pelvic fractures irrespective of their ISS scores. Our study underscores the fact that multiply injured patients suffer more complex pelvic injuries.
The head/neck and spine injuries were the most prevalent concomitant injuries encountered in 67.3% and 61.2% respectively. In a recent review of the literature Gannslen et al. [6] reported overall incidences of 38.8% and 3.2% for head and spine injuries respectively. The involvement of the upper trunk is thought to be higher in the setting of more severe pelvic injuries (18). Of note is the fact that severe chest trauma was prevalent in this series encountered in 30 cases. Other series [2] have reported that the chest is less frequently affected but our study underlines that fact that in polytrauma children the incidence of chest injury is higher. Nevertheless chest injury in our series did not affect the length of ICU stay.
In the present cohort of patients the only significant independent predictors of mortality in polytrauma children with pelvic fractures were a high ISS and the presence of severe head injury. ISS has been previously associated with increased mortality in polytrauma children [19, 20]. The overall mortality of paediatric patients with pelvic ring injury has been estimated to an average of 6.4% (range 0 - 25%) [21]. In contrast to the most common cause of mortality in the adult polytrauma population which is mainly catastrophic uncontrollable haemorrhage, our study confirms that haemorrhage is not directly related to acute death in polytrauma children. Ismail et al. [12] reported that children do not die from uncontrollable pelvic haemorrhage but that catastrophic bleeding is associated with visceral organ injury. Grisoni et al. [13] as well concluded that pelvic haemorrhage is less common in children compared to that encountered in adult trauma and that it is more easily controllable. As has been previously underlined by other scholars the mortality in the multiply injured paediatric population is directly linked to the severity of the concomitant head injury [5] and high ISS [22]. The high incidence of head trauma in children has been attributed to the mechanism of injury of pelvic ring in children which is lateral crush, usually by a car [5, 23]. In our series all deaths occurred within 24 of the traumatic event in patients with head injury. Severe head injury also predicted a longer stay in ICU.
Although severity of the injury (high ISS) had been associated to the complexity of the pelvic ring injury in previous studies [5], in our study mortality was not associated with the type of the pelvic injury. This has also been shown by Subasi et al. [24]. Other authors though have associated increased mortality to the type [25] and complexity [4] of pelvic trauma. On the other hand the mortality was indeed associated with high ISS - a finding that was anticipated and confirmed the previous literature reports.
In this cohort the three patients that sustained a Type C injury were treated operatively whilst all of the 19 patients that suffered a type A injury were managed non-operatively. None of the patients who died within 24 hours from presentation had surgery to the pelvic brim. Of the non-survivors one had a Type A fracture and 4 had a Type B injury.
Of the 23 survivors with Type B injury, 8 were managed operatively and 11 non-operatively for their pelvic injuries. From the operatively treated Type B group, two patients were toddlers (patient No 11: 2.8 years old, and patient No 32: 3.5 years old). Both of these patients sustained a Type B1 (equivalent to “open –book” injury according to Young-Burgess classification) with pubic symphysis diastasis more that 2.5 cm and were managed with an external fixator. The rest of the patients with Type B injuries (6 patients) were adolescents (age >14 years). One of these patients (patient No 9) sustained a Type B2-3 injury (equivalent to LC-II injury according to Young-Burgess classification) and was managed with temporary external fixation that was later converted to open reduction and internal fixation of the iliac wing. Three of the patients (patients No 10, 17, 27) on the operative group had suffered an unstable Type B2 injury (equivalent to LC-I) and were managed with a distraction external fixator and a sacroiliac screw. The remaining two patients (Patients No 26 and 43) sustained a type B1 injury and were managed only with an external fixator because of the compromised perisymphyseal soft tissue condition.
Only two patients (patients No 18 and 33) from the non-operatively type B injuries were adolescents. The patients of this group had either a Type B1 (open book) injury with pubic symphysis diastasis of less than 2.5 cm or a stable Type B2 (Lateral compression type I) injury and were consequently managed non-operatively.
The indications for operative management of pelvic ring injuries in this cohort were mainly the severe displacement and the facilitation of more effective rehabilitation and nursing care. The prevention of deformity after severe displacement is the main indication for operative management of pelvic injuries [21, 26-28]. For type B2 injuries (lateral compression Type 1) that were unstable a surgical fixation was performed to facilitate rehabilitation and nursing and also to reduce the pain management requirements [29]. Patients older than 14 years can be managed with the usual techniques and implants used for stabilisation in adult patients [21] and that was the case in our series. Six out of eight patients that underwent surgical fixation of their pelvic fractures were older that 14 years and were managed using reduction and fixation techniques similar to that used in adults. The remaining two patients had suffered a Type B1 (open book) injury and were treated with an application of an anterior superior (iliac crest) internal fixation. No fixation of the pubic symphysis was undertaken although we appreciate that celclage osteosynthesis with transosseous suturing is recommended by some authors [30].
This study has several limitations including its retrospective nature and the relatively small number of patients. It is worth noting though that most of the published studies report on similar size patient cohorts. Nevertheless the data analysed were collected from a prospectively collected database. An additional limitation of the present study is the lack of documentation of long-term and patient-recorded outcomes. However, our intention was to analyse the characteristics and early mortality associated to these injuries and underline the special considerations pertaining to their early management. To the best of our knowledge this is the only study in contemporary orthopaedic trauma literature that reports on a substantial number of polytraumatised children with pelvic fractures and its major advantage lies in the above fact.
CONCLUSION
This study depicts the fact that polytrauma children with pelvic injuries have different causes of mortality compared to adults. The severe head injury is the major contributing factor. A high ISS also predicts an increased mortality in this population. Hemorrhage from pelvic injuries is rarely catastrophic and can be managed following local protocols. The severity of the pelvic injury is not associated with early mortality. The length of ICU stay, which is an important medical, social and health economical parameter was found to be associated to the head trauma sustained. The treating physician should also be aware of the high incidence of concomitant spine and chest injuries in the polytrauma children with pelvic fractures.
Fig. (2).
Intraoperative photographs showing the fracture of the left iliac wing before (a) and after (b) the application of the two reconstruction plates. The patient’s head is on the right. The circles on the bottom of the screen represent the PSIS and the lateral transverse process of L5. Note the curvilinear incision for the approach to the iliac wing.
ACKNOWLEDGEMENTS
Declared none.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Letts M., Davidson D., Lapner P. Multiple trauma in children: predicting outcome and long-term results. Can. J. Surg. 2002;45(2):126–131. [PMC free article] [PubMed] [Google Scholar]
- 2.Snyder C.L., Jain V.N., Saltzman D.A., Strate R.G., Perry J.F., Jr, Leonard A.S. Blunt trauma in adults and children: a comparative analysis. J. Trauma. 1990;30(10):1239–1245. doi: 10.1097/00005373-199010000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Galano G.J., Vitale M.A., Kessler M.W., Hyman J.E., Vitale M.G. The most frequent traumatic orthopaedic injuries from a national pediatric inpatient population. J. Pediatr. Orthop. 2005;25(1):39–44. doi: 10.1097/00004694-200501000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Hauschild O., Strohm P.C., Culemann U., Pohlemann T., Suedkamp N.P., Koestler W., Schmal H. Mortality in patients with pelvic fractures: results from the German pelvic injury register. J. Trauma. 2008;64(2):449–455. doi: 10.1097/TA.0b013e31815982b1. [DOI] [PubMed] [Google Scholar]
- 5.Leonard M., Ibrahim M., Mckenna P., Boran S., McCormack D. Paediatric pelvic ring fractures and associated injuries. Injury. 2011;42(10):1027–1030. doi: 10.1016/j.injury.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Gänsslen A., Hildebrand F., Heidari N., Weinberg A.M. Pelvic ring injuries in children. Part I: Epidemiology and primary evaluation. A review of the literature. Acta Chir. Orthop. Traumatol. Cech. 2012;79(6):493–498. [PubMed] [Google Scholar]
- 7.Chia J.P., Holland A.J., Little D., Cass D.T. Pelvic fractures and associated injuries in children. J. Trauma. 2004;56(1):83–88. doi: 10.1097/01.TA.0000084518.09928.CA. [DOI] [PubMed] [Google Scholar]
- 8.Nabaweesi R., Arnold M.A., Chang D.C., Rossberg M.I., Ziegfeld S., Sawaya D.E., Bathurst M.A., Colombani P., Abdullah F. Prehospital predictors of risk for pelvic fractures in pediatric trauma patients. Pediatr. Surg. Int. 2008;24(9):1053–1056. doi: 10.1007/s00383-008-2195-8. [DOI] [PubMed] [Google Scholar]
- 9.Rieger H., Brug E. Fractures of the pelvis in children. Clin. Orthop. Relat. Res. 1997;(336):226–239. doi: 10.1097/00003086-199703000-00031. [DOI] [PubMed] [Google Scholar]
- 10.Silber J.S., Flynn J.M., Koffler K.M., Dormans J.P., Drummond D.S. Analysis of the cause, classification, and associated injuries of 166 consecutive pediatric pelvic fractures. J. Pediatr. Orthop. 2001;21(4):446–450. doi: 10.1097/01241398-200107000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Torode I., Zieg D. Pelvic fractures in children. J. Pediatr. Orthop. 1985;5(1):76–84. doi: 10.1097/01241398-198501000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Ismail N., Bellemare J.F., Mollitt D.L., DiScala C., Koeppel B., Tepas J.J., III Death from pelvic fracture: children are different. J. Pediatr. Surg. 1996;31(1):82–85. doi: 10.1016/S0022-3468(96)90324-3. [DOI] [PubMed] [Google Scholar]
- 13.Grisoni N., Connor S., Marsh E., Thompson G.H., Cooperman D.R., Blakemore L.C. Pelvic fractures in a pediatric level I trauma center. J. Orthop. Trauma. 2002;16(7):458–463. doi: 10.1097/00005131-200208000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Marsh J.L., Slongo T.F., Agel J., Broderick J.S., Creevey W., DeCoster T.A., Prokuski L., Sirkin M.S., Ziran B., Henley B., Audigé L. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J. Orthop. Trauma. 2007;21(10) Suppl.:S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 15.Young J.W., Burgess A.R., Brumback R.J., Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. 1986;160(2):445–451. doi: 10.1148/radiology.160.2.3726125. [DOI] [PubMed] [Google Scholar]
- 16.Spiguel L., Glynn L., Liu D., Statter M. Pediatric pelvic fractures: a marker for injury severity. Am. Surg. 2006;72(6):481–484. [PubMed] [Google Scholar]
- 17.Blasier R.D., McAtee J., White R., Mitchell D.T. Disruption of the pelvic ring in pediatric patients. Clin. Orthop. Relat. Res. 2000;(376):87–95. doi: 10.1097/00003086-200007000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Meyer-Junghänel L., Gänsslen A., Pohlemann T., Tscherne H. [Treatment outcome after complex pelvic trauma in children]. Unfallchirurg. 1997;100(3):225–233. doi: 10.1007/s001130050115. [DOI] [PubMed] [Google Scholar]
- 19.Wesson D.E., Spence L.J., Williams J.I., Armstrong P.F. Injury scoring systems in children. Can. J. Surg. 1987;30(6):398–400. [PubMed] [Google Scholar]
- 20.Eichelberger M.R., Bowman L.M., Sacco W.J., Mangubat E.A., Lowenstein A.D., Gotschall C.S. Trauma score versus revised trauma score in TRISS to predict outcome in children with blunt trauma. Ann. Emerg. Med. 1989;18(9):939–942. doi: 10.1016/S0196-0644(89)80457-3. [DOI] [PubMed] [Google Scholar]
- 21.Gänsslen A., Hildebrand F., Heidari N., Weinberg A.M. Pelvic ring injuries in children. Part II: Treatment and results. A review of the literature. Acta Chir. Orthop. Traumatol. Cech. 2013;80(4):241–249. [PubMed] [Google Scholar]
- 22.Vitale M.G., Kessler M.W., Choe J.C., Hwang M.W., Tolo V.T., Skaggs D.L. Pelvic fractures in children: an exploration of practice patterns and patient outcomes. J. Pediatr. Orthop. 2005;25(5):581–587. doi: 10.1097/01.bpo.0000175112.91122.41. [DOI] [PubMed] [Google Scholar]
- 23.Garvin K.L., McCarthy R.E., Barnes C.L., Dodge B.M. Pediatric pelvic ring fractures. J. Pediatr. Orthop. 1990;10(5):577–582. doi: 10.1097/01241398-199009000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Subasi M., Arslan H., Necmioglu S., Onen A., Ozen S., Kaya M. Long-term outcomes of conservatively treated paediatric pelvic fractures. Injury. 2004;35(8):771–781. doi: 10.1016/j.injury.2003.09.037. [DOI] [PubMed] [Google Scholar]
- 25.Smith W., Shurnas P., Morgan S., Agudelo J., Luszko G., Knox E.C., Georgopoulos G. Clinical outcomes of unstable pelvic fractures in skeletally immature patients. J. Bone Joint Surg. Am. 2005;87(11):2423–2431. doi: 10.2106/JBJS.C.01244v. [DOI] [PubMed] [Google Scholar]
- 26.Bryan W.J., Tullos H.S. Pediatric pelvic fractures: review of 52 patients. J. Trauma. 1979;19(11):799–805. doi: 10.1097/00005373-197911000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Keshishyan R.A., Rozinov V.M., Malakhov O.A., Kuznetsov L.E., Strunin E.G., Chogovadze G.A., Tsukanov V.E. Pelvic polyfractures in children. Radiographic diagnosis and treatment. Clin. Orthop. Relat. Res. 1995;(320):28–33. [PubMed] [Google Scholar]
- 28.Schwarz N., Posch E., Mayr J., Fischmeister F.M., Schwarz A.F., Ohner T. Long-term results of unstable pelvic ring fractures in children. Injury. 1998;29(6):431–433. doi: 10.1016/S0020-1383(98)00074-6. [DOI] [PubMed] [Google Scholar]
- 29.Tosounidis T., Kanakaris N., Nikolaou V., Tan B., Giannoudis P.V. Assessment of Lateral Compression type 1 pelvic ring injuries by intraoperative manipulation: which fracture pattern is unstable? Int. Orthop. 2012;36(12):2553–2558. doi: 10.1007/s00264-012-1685-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gänsslen A., Hildebrand F., Heidari N., Weinberg A.M. Acetabular fractures in children: a review of the literature. Acta Chir. Orthop. Traumatol. Cech. 2013;80(1):10–14. [PubMed] [Google Scholar]