Abstract
Purpose
Hypoxemia during one-lung ventilation (OLV) remains a serious problem, particularly in the supine position. We investigated the effects of alveolar recruitment (AR) and positive end-expiratory pressure (PEEP) on oxygenation during OLV in the supine position.
Materials and Methods
Ninety-nine patients were randomly allocated to one of the following three groups: a control group (ventilation with a tidal volume of 8 mL/kg), a PEEP group (the same ventilatory pattern with a PEEP of 8 cm H2O), or an AR group (an AR maneuver immediately before OLV followed by a PEEP of 8 cm H2O). The tidal volume was reduced to 6 mL/kg during OLV in all groups. Blood gas analyses, respiratory variables, and hemodynamic variables were recorded 15 min into TLV (TLVbaseline), 15 and 30 min after OLV (OLV15 and OLV30), and 10 min after re-establishing TLV (TLVend).
Results
Ultimately, 92 patients were analyzed. In the AR group, the arterial oxygen tension was higher at TLVend, and the physiologic dead space was lower at OLV15 and TLVend than in the control group. The mean airway pressure and dynamic lung compliance were higher in the PEEP and AR groups than in the control group at OLV15, OLV30, and TLVend. No significant differences in hemodynamic variables were found among the three groups throughout the study period.
Conclusion
Recruitment of both lungs with subsequent PEEP before OLV improved arterial oxygenation and ventilatory efficiency during video-assisted thoracic surgery requiring OLV in the supine position.
Keywords: Alveolar recruitment, one-lung ventilation, positive end-expiratory pressure, supine position
INTRODUCTION
Video-assisted thoracic surgery (VATS) in the supine position for lesions of the anterior mediastinum has become popular, and this procedure requires one-lung ventilation (OLV).1,2,3 Surgical positions considerably influence the deterioration speed and nadir value of arterial oxygen tension (PaO2) after the start of OLV.4,5 In contrast to the lateral decubitus position, preferential redistribution of pulmonary perfusion to the ventilated lung by gravity is absent during OLV in the supine position, resulting in the more frequent development of dangerous hypoxemia.4,6
Hypoxemia during OLV develops mainly due to the involvement of the intrapulmonary shunt (Qs/Qt) with blood flow through the capillaries of the non-ventilated lung and anesthesia-induced atelectasis in the ventilated lung, leading to a mismatch of the ratio of ventilation to perfusion (V/Q).7,8,9 Alveolar recruitment (AR) is an effective ventilatory maneuver that reverts alveolar collapse by increasing the transpulmonary pressure. Positive end-expiratory pressure (PEEP) during OLV, by aiding AR and restoring functional residual capacity, has been proposed to minimize atelectasis in the ventilated lung and thus improve oxygenation.10,11,12,13,14,15 On the other hand, the application of PEEP alone may paradoxically increase pulmonary vascular resistance and the shift of blood flow to the non-ventilated lung, leading to an increase in Qs/Qt and impairment of oxygenation.15,16,17 Therefore, considering that only slight gravity-dependent pulmonary shift takes place in the supine position, PEEP per se likely demonstrates both positive and negative effects on Qs/Qt and V/Q matching. However, the effects of the AR maneuver and PEEP on oxygenation during OLV in the supine position have not been evaluated. We tested whether the AR maneuver with subsequent PEEP and PEEP alone could improve oxygenation during OLV in the supine position in patients undergoing VATS in a prospective and randomized trial. As secondary endpoints, the effects of the proposed treatment on Qs/Qt and physiologic dead space were also evaluated.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board (ref: 4-2011-0301) and registered at http://clinicaltrials.gov (NCT 01652612). After written informed consent was obtained from all patients, 99 patients of ages 20-70 years with America Society of Anesthesiologists physical status class II or III who were scheduled for VATS in the supine position were enrolled in this study. Exclusion criteria included an expected duration of OLV <30 min, uncompensated cardiac disease, chronic obstructive or restrictive pulmonary disease (preoperative forced expiratory volume in 1 second and forced vital capacity below 60% of the predicted value), and obesity (body mass index >30 kg/m2). Patients were randomly allocated to one of three groups using a computerized randomization table one day before surgery by an independent anesthesiology nurse who was not involved in this study (control group: n=33; PEEP group: n=33; AR group: n=33).
Patients were monitored by electrocardiography and pulse oximetry, as well as by monitoring for nasopharyngeal temperature, invasive arterial pressure, and central venous pressure. Anesthesia was induced with propofol (1.5 mg/kg), remifentanil (0.5-1.0 µg/kg), and rocuronium (0.3-0.9 mg/kg) while monitoring for train-of-four stimulation. Anesthesia was maintained with sevoflurane (1.0-2.0 vol%) and remifentanil (0.1-0.3 µg/kg/min). The trachea was intubated using a left-sided double-lumen tube (Broncho-Cath®; Mallinckrodt Medical Inc., Athlone, Ireland); the correct position was confirmed using a fiberoptic bronchoscope after intubation and supine surgical positioning. A 7-Fr central venous catheter (Arrow International, Reading, PA, USA) was inserted via the right internal jugular vein. The insertion length of the central venous catheter was calculated using a height-based formula in order to place its tip near the right atrium,18 which was confirmed by portable chest X-ray.
The lungs were initially ventilated using a constant-flow, volume-controlled ventilation mode (Zeus ventilator; Dräger Medical, Lübeck, Germany) with a tidal volume (VT) of 8 mL/kg predicted body weight, an inspiratory:expiratory (I:E) ratio of 1:2, an inspiratory pause of 10%, and a respiratory rate of 12 bpm in 100% oxygen without PEEP. After all patients were placed in the supine surgical position with pillows under each hemithorax allowing some degree of tilting (≤10°), the ventilator was switched to the pressure-controlled mode, adjusting the peak inspiratory pressure to obtain the same VT as during the volume-controlled mode. In the PEEP group, a PEEP of 8 cm H2O was applied. In the AR group, the AR maneuver was performed: the peak inspiratory pressure and PEEP were sequentially increased from 30/10 to 35/15 cm H2O in steps of five breaths and then to 40/20 cm H2O for ten breaths with an I:E ratio of 1:1. And then, the ventilator was set back to the baseline setting in the pressure-controlled mode at a PEEP of 8 cm H2O.10,12 OLV was initiated at the moment of skin incision, and the tube lumen of the non-ventilated lung was opened to room air. During OLV, VT was reduced to 6 mL/kg, and the respiratory rate was adjusted to maintain an end-tidal CO2 tension (ETCO2) of 35-40 mm Hg.
During surgery, intrathoracic CO2 insufflation was accomplished at a set pressure of 8-10 mm Hg and was automatically controlled by a CO2 insufflator. During OLV, if SpO2 declined to <90%, surgery was temporarily interrupted to resume intermittent two-lung ventilation (TLV) until SpO2 recovered to >95%. After the OLV period, both lungs were re-expanded by hand bagging in all patients.
Arterial and central venous blood gas analyses, respiratory variables, and hemodynamic variables were recorded at the following points: 15 min into TLV (TLVbaseline), 15 and 30 min after OLV (OLV15 and OLV30), and 10 min after the re-establishment of TLV (TLVend). Respiratory variables included the peak airway pressure (Ppeak), mean airway pressure (Pmean), and dynamic lung compliance, which was calculated as VT/(Ppeak-PEEP). Physiologic (dead space to tidal volume ratio, VD/VT) was calculated according to the Hardman and Aitkenhead19 equation: VD/VT=1.14×(PaCO2-E'CO2)/PaCO2-0.005. The shunt fraction (Qs/Qt) was determined using the formula: Qs/Qt=(CcO2-CaO2)/(CcO2-CvO2), assuming that mixed venous O2 partial pressure was equal to central venous O2 partial pressure. Arterial and central venous blood samples were measured using an automated blood gas analyzer (Stat Profile ® CCX; Nova Biomedical, MA, USA). Hemodynamic measurements included the heart rate, mean arterial pressure, and central venous pressure.
Statistical analyses were performed using SPSS 18.0 (SPSS Inc., Chicago, IL, USA). Data are presented as mean±standard deviation, or numbers as appropriate. Based on the results of a previous study evaluating the effect of the AR strategy in the lateral decubitus position,11 we estimated that a sample of 31 patients per treatment group would be sufficient for detecting a 76-mm Hg mean difference of PaO2 between any two groups with a power of 0.8, a type I error of 0.05, and a standard deviation of 108 mm Hg. Factoring in a drop-out rate of 5%, we calculated that 33 patients would be required for each group. To assess for normality, the Kolmogorov-Smirnov (K-S) test was performed on the data set. Normally-distributed data were analyzed with a one-way analysis of variance for continuous variables. If there was a significant difference among the groups, a post hoc analysis using Bonferroni's test was performed. In cases where the K-S test demonstrated that data did not follow a normal distribution, comparisons between treatments were performed using the Kruskal-Wallis test, and Bonferroni correction was used for multiple comparisons. Categorical data were analyzed with a χ2 test. A p value less than 0.05 was considered to be statistically significant.
RESULTS
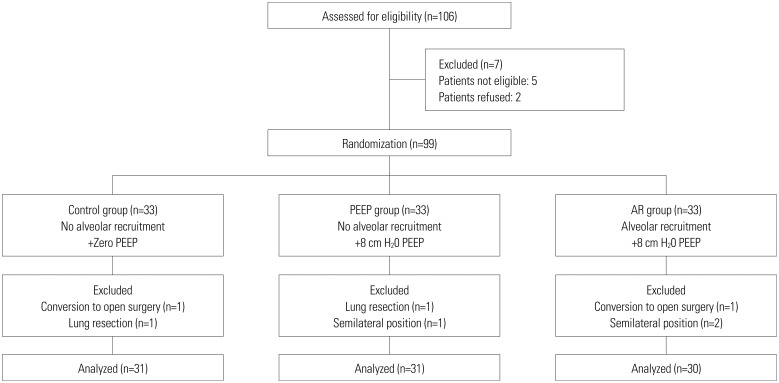
One hundred six patients were assessed for eligibility; 99 of these patients consented to participate in the study and were randomly assigned to groups. Of the enrolled patients, seven patients were excluded from the study due to changes in the surgical plan during surgery; therefore, 92 patients completed the study (Fig. 1). Patients' characteristics and clinical data were similar among the groups (Table 1). None of the patients demonstrated dangerous hypoxemia (SpO2<90%) for a 30-min OLV period regardless of the side of surgical approach.
Fig. 1. The consort flow diagram. PEEP, positive end-expiratory pressure.
Table 1. Demographic and Operative Data.
| Control group (n=31) | PEEP group (n=31) | AR group (n=30) | |
|---|---|---|---|
| Age (yr) | 44±14 | 49±14 | 46±14 |
| Male/female | 9/22 | 6/25 | 13/17 |
| Body mass index (kg/m2) | 23.3±3.0 | 22.7±2.5 | 23.0±3.3 |
| Hypertension | 1 | 4 | 1 |
| Diabetes | 3 | 2 | 0 |
| FVC (%) | 97±13 | 91±18 | 91±16 |
| FEV1 (%) | 106±14 | 97±17 | 99±17 |
| FEV1/FVC (%) | 83±5 | 80±8 | 84±7 |
| DLCO (%) | 111±19 | 105±16 | 107±21 |
| Hemoglobin (g/dL) | 12.2±1.1 | 12.0±0.9 | 12.3±1.1 |
| Duration of anesthesia (min) | 126±43 | 139±62 | 143±38 |
| Duration of surgery (min) | 82±42 | 83±48 | 95±37 |
| Duration of one-lung ventilation (min) | 67±39 | 60±33 | 74±29 |
| Operation side (R/L) | 5/26 | 4/27 | 8/22 |
| Operative diagnosis | |||
| Myasthenia gravis with/without thymoma | 7/6 | 6/8 | 7/7 |
| Thymic cyst/tumors | 4/10 | 11/6 | 2/11 |
| Bronchial cyst | 3 | 0 | 3 |
| Intrathoracic chest wall lipoma | 1 | 0 | 0 |
FEV1, forced expiratory volume in 1 second; FVC, functional vital capacity; DLCO, diffusion capacity of lung for carbon monoxide; PEEP, positive end-expiratory pressure; AR, alveolar recruitment.
Values are number of patients or mean±SD.
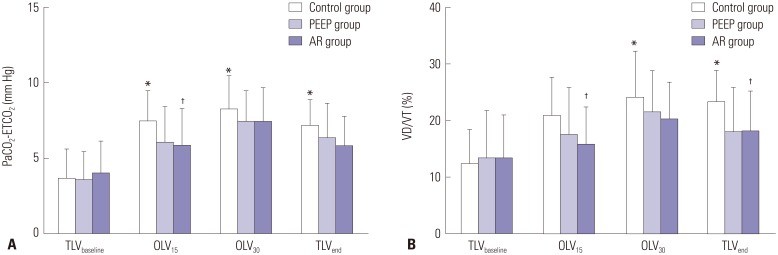
The arterial and central venous blood gas data are shown in Table 2. PaO2 was higher at TLVend (p=0.027) in the AR group than in the control group. The PaCO2-ETCO2 difference at OLV15 (p=0.043) and the estimated VD/VT at OLV15 and TLVend (p<0.05) decreased more in the AR group than in the control group (Fig. 2). When compared with TLVbaseline, PaO2 decreased while PaCO2 increased during OLV in all groups (p<0.01). At TLVend, PaO2 did not return to baseline values only in the control group. Compared with TLVbaseline, the estimated VD/VT increased at OLV30 and TLVend (p<0.05), and the PaCO2-ETCO2 difference increased during OLV and at TLVend (p<0.01) in the control group. Qs/Qt increased at OLV30 compared with TLVbaseline in all groups (p<0.05).
Table 2. Blood Gas Analysis Data.
| Group | TLVbaseline | OLV15 | OLV30 | TLVend |
|---|---|---|---|---|
| PaO2 (mm Hg) | ||||
| Control | 419.3±70.5 | 284.5±67.3* | 255.8±83.6* | 351.6±60.7* |
| PEEP | 392.0±70.8 | 258.1±69.7* | 240.5±68.4* | 398.4±73.4 |
| AR | 414.9±69.0 | 276.5±62.3* | 258.2±84.6* | 402.2±80.0† |
| PcvO2 (mm Hg) | ||||
| Control | 51.2±17.7 | 49.4±13.1 | 55.4±15.8 | 52.6±19.0 |
| PEEP | 48.8±16.2 | 45.8±10.1 | 48.6±11.0 | 49.7±12.3 |
| AR | 47.4±7.8 | 49.2±6.8 | 49.6±8.4 | 51.3±13.1 |
| PaCO2 (mm Hg) | ||||
| Control | 31.1±4.4 | 40.0±4.6* | 39.2±5.7* | 34.6±4.9* |
| PEEP | 30.7±3.4 | 39.2±5.3* | 39.6±6.0* | 37.1±7.0* |
| AR | 32.8±5.0 | 41.0±7.5* | 41.4±6.2* | 36.0±5.7* |
| Qs/Qt (%) | ||||
| Control | 16.7±7.7 | 23.3±8.6 | 29.0±12.2* | 22.9±11.4 |
| PEEP | 18.0±4.5 | 21.9±6.6 | 25.1±7.5* | 18.1±7.7 |
| AR | 16.3±4.6 | 21.1±8.2 | 25.9±10.2* | 17.1±6.4 |
PaO2, arterial oxygen tension; PcvO2, central venous oxygen tension; PaCO2, arterial carbon dioxide tension; Qs/Qt, intrapulmonary shunt fraction; TLVbaseline, 15 min into TLV; OLV15 and OLV30, 15 min and 30 min after OLV; TLVend, 10 min after TLV was re-initiated; PEEP, positive end-expiratory pressure; AR, alveolar recruitment.
Values are mean±SD.
*p<0.05 vs. TLVbaseline in each group, †p<0.05 vs. control group.
Fig. 2. Changes in the PaCO2-ETCO2 difference (A) and estimated VD/VT (B). PaCO2-ETCO2, arterial to end-tidal carbon dioxide tension difference; estimated VD/VT, physiologic dead space. *p<0.05 vs. TLVbaseline in each group, †p<0.05 vs. control group.
Lung mechanics and hemodynamic data are presented in Table 3 and 4. During OLV and at TLVend, Pmean (p<0.01) and dynamic lung compliance (p<0.01) were higher in the PEEP and AR groups than in the control group. At TLVend, Ppeak was higher in the PEEP and AR groups than in the control group (p<0.01). Compared with TLVbaseline, Ppeak, and Pmean increased during OLV and at TLVend (p<0.01) in all groups, whereas dynamic lung compliance decreased during OLV in all groups yet only in the control group at TLVend (p<0.01). No significant differences were found among the groups in terms of hemodynamic variables throughout the study period. Compared with TLVbaseline, central venous pressure increased during OLV in all groups (p<0.01), and the mean arterial pressure decreased at TLVend in the control and AR groups (p<0.05).
Table 3. Lung Mechanics.
| Group | TLVbaseline | OLV15 | OLV30 | TLVend |
|---|---|---|---|---|
| Tidal volume (mL) | ||||
| Control | 494±88 | 424±98* | 413±81* | 505±82 |
| PEEP | 477±73 | 376±76* | 379±76* | 498±113 |
| AR | 513±104 | 404±104* | 403±109* | 491±97 |
| Ppeak (cm H2O) | ||||
| Control | 12.3±2.8 | 19.6±4.5* | 20.8±5.7* | 15.0±4.0* |
| PEEP | 12.8±2.0 | 22.1±3.0* | 23.0±3.2* | 18.1±2.6*† |
| AR | 12.8±2.3 | 21.9±5.0* | 23.1±5.3* | 18.6±3.2*† |
| Pmean (cm H2O) | ||||
| Control | 6.0±2.2 | 8.4±2.4* | 8.6±2.2* | 7.1±2.5* |
| PEEP | 6.0±1.6 | 12.4±2.0*† | 12.1±2.0*† | 10.6±2.0*† |
| AR | 5.6±1.8 | 12.8±1.7*† | 13.1±1.8*† | 11.1±2.3*† |
| Cdyn (mL/cm H2O) | ||||
| Control | 41.3±4.9 | 21.8±4.8* | 20.3±5.0* | 34.6±7.5* |
| PEEP | 42.1±11.7 | 27.4±5.6*† | 26.8±6.5*† | 45.4±7.9† |
| AR | 41.2±6.2 | 30.9±8.7*† | 29.1±8.2*† | 41.8±10.0† |
Ppeak, peak airway pressure; Pmean, mean airway pressure; Cdyn, dynamic lung compliance; TLVbaseline, 15 min into TLV; OLV15 and OLV30, 15 min and 30 min after OLV; TLVend, 10 min after TLV was re-initiated; PEEP, positive end-expiratory pressure; AR, alveolar recruitment.
Values are mean±SD.
*p<0.05 vs. TLVbaseline in each group, †p<0.05 vs. control group.
Table 4. Hemodynamic Changes.
| Group | TLVbaseline | OLV15 | OLV30 | TLVend |
|---|---|---|---|---|
| Heart rate (beats/min) | ||||
| Control | 67±14 | 71±14 | 69±10 | 69±12 |
| PEEP | 67±15 | 70±13 | 68±12 | 69±11 |
| AR | 68±13 | 70±12 | 72±9 | 68±10 |
| MAP (mm Hg) | ||||
| Control | 83±13 | 90±12 | 86±11 | 79±11* |
| PEEP | 89±18 | 90±13 | 87±11 | 81±14 |
| AR | 89±13 | 91±15 | 88±11 | 79±10* |
| CVP (mm Hg) | ||||
| Control | 10±4 | 16±3* | 16±4* | 11±3 |
| PEEP | 10±3 | 17±4* | 16±4* | 11±4 |
| AR | 10±3 | 17±3* | 18±4* | 12±3 |
MAP, mean arterial pressure; CVP, central venous pressure; TLVbaseline, 15 min into TLV; OLV15 and OLV30, 15 min and 30 min after OLV; TLVend, 10 min after TLV was re-initiated; PEEP, positive end-expiratory pressure; AR, alveolar recruitment.
Values are mean±SD.
*p<0.05 vs. TLVbaseline in each group.
DISCUSSION
This study investigated the effects of AR with subsequent PEEP and PEEP alone on oxygenation during OLV in the supine position. We observed that bilateral lung recruitment before the start of OLV not only improved the efficiency of ventilation but also increased arterial oxygenation with no significant change of Qs/Qt. Although dynamic lung compliance improved in both treatment groups, PEEP without recruitment did not lead to improved oxygenation.
The range of applications of VATS in treating mediastinal cysts and tumors has extended due to the evolution of surgical techniques; consequently, various patient positions require OLV.1,2,20 Minimally invasive techniques offer the advantages of improved cosmesis, less surgical stress, shorter hospital durations, and efficacy equivalent to conventional open surgery.3,21 However, hypoxemia related to one-lung anesthesia occurs with an incidence of approximately 5-10%, affecting postoperative outcomes such as cognitive dysfunction, renal failure, and pulmonary hypertension.22,23 Compared with the lateral decubitus position, semilateral and supine surgical positions during OLV are associated with less gravity-induced redistribution of pulmonary perfusion to the ventilated lung, leading to higher Qs/Qt and more hypoxemia.4,6 Additionally, anesthesia-induced atelectasis contributes to shunting in the ventilated lung regardless of the patient position.8,9 In this study, two preventative ventilatory strategies in relation to atelectasis demonstrated increased dynamic lung compliance throughout the study period; however, only AR with subsequent PEEP resulted in improved efficiency of ventilation and oxygenation by reducing the physiologic dead space.
Dead space is the portion of ventilation that does not participate in gas exchange, indicating the degree of ventilatory efficiency.24 OLV increases dead space and the PaCO2-ETCO2 difference, thereby requiring a greater minute ventilation to maintain the same level of PaCO2.25 Our results are consistent with previous findings that AR improved the efficiency of alveolar ventilation during OLV, resulting in a lower PaCO2-ETCO2 difference and a reduced alveolar component of dead space, which is directly related to atelectasis and Qs/Qt.10,11,12 In previous studies regarding AR, protocols were designed to apply a PEEP of 5-8 cm H2O in both treated and control patients undergoing thoracic surgery in the lateral position.10,11 Although the application of PEEP has been known to be beneficial to the atelectatic areas, it did not improve efficiency of ventilation without a preemptive recruitment maneuver.10,11,12,13,14,15 Additionally, PEEP applied to the ventilated lung may cause a shift of pulmonary blood flow to the non-ventilated lung and thus increase Qs/Qt, especially in the supine position, in which there is a similar influence of gravitational force on both lungs.6,15,16,17 However, during OLV in the supine position in this study, Qs/Qt did not differ among the two treatments groups and the control group. Increased intrathoracic pressure caused by CO2 insufflation in the non-ventilated lung could be one possible explanation of similar Qs/Qt, as such pressure diverts pulmonary perfusion to the ventilated lung. Another explanation may be that the pressure-controlled mode during OLV might be associated with lower airway pressure and less compression of perialveolar vessels.26
Contrary to our expectations, OLV in the supine position was well tolerated, and SpO2 remained >90% during a 30 minstudy period of OLV in all patients, whether they received treatment or not. Two previous studies evaluating oxygenation during OLV in the supine position have reported different incidences of hypoxemia.4,6 In one previous trial, hypoxemia (SpO2<90%) developed within 30 min of OLV in 82% of patients with normal preoperative pulmonary function undergoing micro-coagulation therapy for hepatic tumors.4 In the other trial, although none of the patients developed hypoxemia, significantly lower PaO2 values were observed in the supine position than in the lateral position during a 15 min-study period of OLV before the start of surgery.6 However, there were several differences between those studies and our study. First, the previous studies involved relatively small numbers of patients. Second, compared with a previous trial,4 minimally invasive techniques performed in this study may contribute better oxygenation by decreasing both pain and surgical stress responses, which influence the development of hypoxemia.27,28 Third, intrathoracic CO2 insufflation into the non-ventilated lung to facilitate exposure of the surgical field may contribute in shifting pulmonary perfusion to the ventilated lung.
The current study has several limitations. First, as this is the first study to compare the effects of the AR maneuver and PEEP during OLV in the supine position, we excluded patients with obesity or underlying pulmonary disease in order to avoid confounding factors. However, hypoxemia was observed in one patient of the control group using both side approaches in the second OLV episode. Therefore, the potential benefits of this ventilatory strategy could be more pronounced in patients with poor pulmonary function. Second, we included patients who underwent VATS using a bilateral approach, which may influence final PaO2 values after re-establishment of TLV. However, no difference was noted in the operative data among groups. Third, we calculated Qs/Qt based on right atrium blood samples instead of pulmonary arterial blood samples.
In summary, recruitment of both lungs with subsequent PEEP improved arterial oxygenation and ventilatory efficiency in patients undergoing VATS in the supine position. This strategy may reduce the risk of hypoxemia; however, it needs to be investigated further in high-risk patients.
ACKNOWLEDGEMENTS
This study was supported by a faculty research grant of Yonsei University College of Medicine (grant 6-2012-0032).
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Darlong LM. Video-assisted thoracic surgery for superior posterior mediastinal neurogenic tumour in the supine position. J Minim Access Surg. 2009;5:49–51. doi: 10.4103/0972-9941.55110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nesher N, Pevni D, Aviram G, Kramer A, Mohr R, Uretzky G, et al. Video-assisted thymectomy with contralateral surveillance camera: a means to minimize the risk of contralateral phrenic nerve injury. Innovations (Phila) 2012;7:266–269. doi: 10.1097/IMI.0b013e3182742a53. [DOI] [PubMed] [Google Scholar]
- 3.Jurado J, Javidfar J, Newmark A, Lavelle M, Bacchetta M, Gorenstein L, et al. Minimally invasive thymectomy and open thymectomy: outcome analysis of 263 patients. Ann Thorac Surg. 2012;94:974–981. doi: 10.1016/j.athoracsur.2012.04.097. [DOI] [PubMed] [Google Scholar]
- 4.Watanabe S, Noguchi E, Yamada S, Hamada N, Kano T. Sequential changes of arterial oxygen tension in the supine position during one-lung ventilation. Anesth Analg. 2000;90:28–34. doi: 10.1097/00000539-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Nyrén S, Radell P, Lindahl SG, Mure M, Petersson J, Larsson SA, et al. Lung ventilation and perfusion in prone and supine postures with reference to anesthetized and mechanically ventilated healthy volunteers. Anesthesiology. 2010;112:682–687. doi: 10.1097/ALN.0b013e3181cf40c8. [DOI] [PubMed] [Google Scholar]
- 6.Bardoczky GI, Szegedi LL, d'Hollander AA, Moures JM, de Francquen P, Yernault JC. Two-lung and one-lung ventilation in patients with chronic obstructive pulmonary disease: the effects of position and F(IO)2. Anesth Analg. 2000;90:35–41. doi: 10.1097/00000539-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Hedenstierna G, Tenling A. The lung during and after thoracic anaesthesia. Curr Opin Anaesthesiol. 2005;18:23–28. doi: 10.1097/00001503-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Hedenstierna G, Tokics L, Strandberg A, Lundquist H, Brismar B. Correlation of gas exchange impairment to development of atelectasis during anaesthesia and muscle paralysis. Acta Anaesthesiol Scand. 1986;30:183–191. doi: 10.1111/j.1399-6576.1986.tb02393.x. [DOI] [PubMed] [Google Scholar]
- 9.Strandberg A, Tokics L, Brismar B, Lundquist H, Hedenstierna G. Atelectasis during anaesthesia and in the postoperative period. Acta Anaesthesiol Scand. 1986;30:154–158. doi: 10.1111/j.1399-6576.1986.tb02387.x. [DOI] [PubMed] [Google Scholar]
- 10.Unzueta C, Tusman G, Suarez-Sipmann F, Böhm S, Moral V. Alveolar recruitment improves ventilation during thoracic surgery: a randomized controlled trial. Br J Anaesth. 2012;108:517–524. doi: 10.1093/bja/aer415. [DOI] [PubMed] [Google Scholar]
- 11.Park SH, Jeon YT, Hwang JW, Do SH, Kim JH, Park HP. A preemptive alveolar recruitment strategy before one-lung ventilation improves arterial oxygenation in patients undergoing thoracic surgery: a prospective randomised study. Eur J Anaesthesiol. 2011;28:298–302. [PubMed] [Google Scholar]
- 12.Tusman G, Böhm SH, Sipmann FS, Maisch S. Lung recruitment improves the efficiency of ventilation and gas exchange during one-lung ventilation anesthesia. Anesth Analg. 2004;98:1604–1609. doi: 10.1213/01.ANE.0000068484.67655.1A. [DOI] [PubMed] [Google Scholar]
- 13.Tusman G, Böhm SH, Melkun F, Staltari D, Quinzio C, Nador C, et al. Alveolar recruitment strategy increases arterial oxygenation during one-lung ventilation. Ann Thorac Surg. 2002;73:1204–1209. doi: 10.1016/s0003-4975(01)03624-4. [DOI] [PubMed] [Google Scholar]
- 14.Valenza F, Ronzoni G, Perrone L, Valsecchi M, Sibilla S, Nosotti M, et al. Positive end-expiratory pressure applied to the dependent lung during one-lung ventilation improves oxygenation and respiratory mechanics in patients with high FEV1. Eur J Anaesthesiol. 2004;21:938–943. doi: 10.1017/s0265021504000316. [DOI] [PubMed] [Google Scholar]
- 15.Hoftman N, Canales C, Leduc M, Mahajan A. Positive end expiratory pressure during one-lung ventilation: selecting ideal patients and ventilator settings with the aim of improving arterial oxygenation. Ann Card Anaesth. 2011;14:183–187. doi: 10.4103/0971-9784.83991. [DOI] [PubMed] [Google Scholar]
- 16.Inomata S, Nishikawa T, Saito S, Kihara S. "Best" PEEP during one-lung ventilation. Br J Anaesth. 1997;78:754–756. doi: 10.1093/bja/78.6.754. [DOI] [PubMed] [Google Scholar]
- 17.Rozé H, Lafargue M, Perez P, Tafer N, Batoz H, Germain C, et al. Reducing tidal volume and increasing positive end-expiratory pressure with constant plateau pressure during one-lung ventilation: effect on oxygenation. Br J Anaesth. 2012;108:1022–1027. doi: 10.1093/bja/aes090. [DOI] [PubMed] [Google Scholar]
- 18.Czepizak CA, O'Callaghan JM, Venus B. Evaluation of formulas for optimal positioning of central venous catheters. Chest. 1995;107:1662–1664. doi: 10.1378/chest.107.6.1662. [DOI] [PubMed] [Google Scholar]
- 19.Hardman JG, Aitkenhead AR. Estimating alveolar dead space from the arterial to end-tidal CO(2) gradient: a modeling analysis. Anesth Analg. 2003;97:1846–1851. doi: 10.1213/01.ANE.0000090316.46604.89. [DOI] [PubMed] [Google Scholar]
- 20.De Giacomo T, Diso D, Anile M, Venuta F, Rolla M, Ricella C, et al. Thoracoscopic resection of mediastinal bronchogenic cysts in adults. Eur J Cardiothorac Surg. 2009;36:357–359. doi: 10.1016/j.ejcts.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 21.Meyer DM, Herbert MA, Sobhani NC, Tavakolian P, Duncan A, Bruns M, et al. Comparative clinical outcomes of thymectomy for myasthenia gravis performed by extended transsternal and minimally invasive approaches. Ann Thorac Surg. 2009;87:385–390. doi: 10.1016/j.athoracsur.2008.11.040. [DOI] [PubMed] [Google Scholar]
- 22.Karzai W, Schwarzkopf K. Hypoxemia during one-lung ventilation: prediction, prevention, and treatment. Anesthesiology. 2009;110:1402–1411. doi: 10.1097/ALN.0b013e31819fb15d. [DOI] [PubMed] [Google Scholar]
- 23.Tang L, Kazan R, Taddei R, Zaouter C, Cyr S, Hemmerling TM. Reduced cerebral oxygen saturation during thoracic surgery predicts early postoperative cognitive dysfunction. Br J Anaesth. 2012;108:623–629. doi: 10.1093/bja/aer501. [DOI] [PubMed] [Google Scholar]
- 24.Hedenstierna G, Sandhagen B. Assessing dead space. A meaningful variable? Minerva Anestesiol. 2006;72:521–528. [PubMed] [Google Scholar]
- 25.Fletcher R. The arterial-end-tidal CO2 difference during cardiothoracic surgery. J Cardiothorac Anesth. 1990;4:105–117. doi: 10.1016/0888-6296(90)90457-q. [DOI] [PubMed] [Google Scholar]
- 26.Sentürk NM, Dilek A, Camci E, Sentürk E, Orhan M, Tugğrul M, et al. Effects of positive end-expiratory pressure on ventilatory and oxygenation parameters during pressure-controlled one-lung ventilation. J Cardiothorac Vasc Anesth. 2005;19:71–75. doi: 10.1053/j.jvca.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 27.Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001;87:62–72. doi: 10.1093/bja/87.1.62. [DOI] [PubMed] [Google Scholar]
- 28.Youssef SJ, Louie BE, Farivar AS, Blitz M, Aye RW, Vallières E. Comparison of open and minimally invasive thymectomies at a single institution. Am J Surg. 2010;199:589–593. doi: 10.1016/j.amjsurg.2010.01.001. [DOI] [PubMed] [Google Scholar]