Abstract
Objective
The objectives were to identify and predict patterns of weight control behavior in 15 year old (yo) girls and to examine weight control group differences in energy intake.
Method
Subjects included 166 girls assessed every 2 years (ys) from age 5 to 15. Latent class analysis was used to identify patterns of weight control behaviors. Antecedent variables (e.g. inhibitory control at 7ys), and concurrent variables (e.g. BMI and dietary intake at 15ys) were included as predictors. Assessments were a combination of survey, interview, and laboratory measures.
Results
LCA identified four classes of weight control behaviors, Non-dieters (26%), and three dieting groups: Lifestyle (16%), Dieters (43%), and Extreme Dieters (17%). Levels of restraint, weight concerns, and dieting frequency increased across groups, from Non-dieters to Extreme Dieters. BMI at 5ys and inhibitory control at 7ys predicted weight control group at 15ys; e.g. with every one-point decrease in inhibitory control, girls were twice as likely to be Extreme Dieters than Non-dieters. Girls in the Extreme Dieters group were mostly classified as under-reporters, and had the lowest self-reported intake, but ate significantly more in the laboratory.
Discussion
Among 15yo girls, “dieting” includes a range of both healthy and unhealthy behaviors. Risk factors for membership in a weight control groups are present as early as 5ys. Patterns of intake in the laboratory support the view that lower reported energy intake by Extreme Dieters is likely due under-reporting as an intent to decrease intake, not actual decreased intake.
Dieting to lose or maintain weight is prevalent among both normal weight and overweight adolescents; estimates indicate that roughly two-thirds of adolescent girls report trying to lose weight 1. Research has shown that self-reported dieting is often not successful, leading to greater long-term weight gain 2, and may increase the development of subclinical disordered eating and clinical eating disorders 3. Multiple individual and psychosocial factors have been found to impact dieting behavior in childhood and adolescence. These factors include peer and media influence 4, parent influences such as the modeling of dieting behavior 5 and direct encouragement to diet6, and individual characteristics including elevated weight status 7 and depression 8. Additionally, while research has shown that weight concerns and dietary restraint are already present during middle childhood 11, it is unclear how these early characteristics influence later dieting behavior during adolescence.
However, while dieting is often assessed as a singular behavior, dieting is a multidimensional construct and can be thought of as the use of weight control behavior(s). In fact, a wide range of weight control behaviors can be included in self-reports of dieting. French and colleagues 9 established a comprehensive list of weight control behaviors, which includes both healthy (e.g. increased fruits and vegetables, increased exercise), and unhealthy (e.g. use of appetite suppressants, skipping meals) weight control behaviors. However, this information is lost when the data are collapsed into a dichotomous item. By collapsing the data into a dichotomous measure you lose variability, thereby obscuring or masking associations of different combinations of weight control behaviors with potential predictors or consequences. Given that that dieting is implicated as a causal factor for a number of disorders (e.g. obesity and weight gain, eating disorders) 2,3, it is necessary to explore etiological factors that link dieting to these disorders. Therefore, it is necessary to distinguish between weight control behaviors that are consistent with healthy weight management (e.g. increase fruits and vegetables) and might be necessary in our obesogenic environment from those that may constitute subclinical disordered eating (e.g. use of unhealthy weight control behaviors such as laxative, diuretics, and appetite suppressants) in order to determine which types of dieters might be at risk.
By definition, dieting is intended to influence dietary intake; however, associations between reported dieting and dietary intake are mixed, in part due to the inconsistent classification of dieting. For example, results of research assessing whether self-reported dieters had different patterns of intake than self-reported non-dieters indicate that dieters consume less nutrient-dense food 10, and have lower overall diet quality 11. In contrast, in another study where the researchers classified self-reported dieters into either moderate (use of a method other than vomiting or use of diet pills) or extreme dieters (use of vomiting or diet pills) 12, moderate dieters reported consuming more servings of fruits and vegetables and fewer servings of high fat foods than either non-dieters or extreme dieters. Taken together, this suggests that more work is needed to explore the influence of dieting on dietary intake, and warrants the examination of differences in dietary intake by patterns of weight control behavior.
Using girls’ responses to French’s list of weight control behaviors as items in Latent class analysis (LCA) provides the opportunity to identify distinct groups of patterns of weight control behaviors that may differ in terms of the number and types of behaviors involved. These groups may also differ in the predictors of group membership and in both self-reported and weighed dietary intake. Taken together, this will help provide researchers with insight into what behaviors adolescent girls are using to help control their weight, and what the consequences of those behaviors might be. While this technique has not yet been used with adolescent weight control behaviors, it has been used to examine patterns and predictors of specific weight control behaviors in adult women 13,14 using the French Weight Control Scale 9. The present study has 3 aims: 1) to use LCA to identify distinct patterns of weight control behaviors among 15 year old (yo) girls; 2) to explore weight control group differences in antecedent (e.g. BMI at 5 years [ys], inhibitory control at 7ys) and concurrent (e.g. BMI at 15ys, dietary restraint at 15ys) variables; and 3) to examine latent class group differences in self-reported dietary intake from 3 24hr multiple-pass dietary recalls, including the extent of under reporting, and weighed intake at standard lunch meal and in the eating in absence of hunger protocol (EAH), obtained in a laboratory setting.
METHODS
Participants
Participants at study entry included 197 non-Hispanic, white families living in Central Pennsylvania recruited as part of a longitudinal cohort study of the health and development of young girls with one of the primary aims to obtain descriptive data on what girls are doing when they report dieting. Eligibility criteria for girls’ participation at recruitment included living with the biological mother and father, the absence of severe food allergies or chronic medical problems affecting food intake, and the absence of dietary restrictions involving animal products. The sample was not recruited based on weight status. Parents and their 5yo daughter (mean age: 5.4 ± 0.4ys) were recruited for participation into the study using flyers and newspaper advertisements. In addition, families with age-eligible female children within a five-county radius received mailings and follow-up phone calls (Metromail Inc.). Additional details on the study population can be found elsewhere 6,8,15,16. Families were assessed at age 5, (N=192) study entry baseline, and then assessed every 2ys at daughter ages 7 (N=192), 9 (N=183), 11 (N=177), 13 (N=168), and 15 (N=167). Attrition was primarily due to family relocation outside of the area. One girl had missing weight control behavior data at 15ys, and thus the final sample had 166 girls and their families.
At study entry, the mean family income was $35,000-$50,000. Parents were well educated; mothers’ mean level of education was 14.5 ± 2.3ys (range: 12-20ys), and fathers’ mean level of education was 14.7 ± 2.5ys (range: 12-20ys). When the girls were 5yo, the mean BMI [wt(kg)/ht(m)2) was 26.4 ± 6.1 for mothers and 28.1 ± 4.4 for fathers. Only mothers were measured for height and weight at daughter age 15, and their mean BMI had increased to 28.4 ± 6.5. The Pennsylvania State University Institutional Review Board approved all study procedures, and parents provided consent for their family’s participation before the study began.
Measures
Antecedent predictors were included at the first time point of measurement in the study (BMI, body satisfaction, and self-competence at age 5, inhibitory control at age 7, fear of fat of at age 9). Pubertal status was assessed at age 11, as the median age of the onset of breast development is 10yo 17, and thus this was the first time point of measurement with variability. All concurrent predictors (BMI, body fat percentage, restraint, disinhibition, weight concerns, dieting risk, self-esteem, depression, binge eating, dieting frequency) and concurrent dietary intake variables (self-reported, lunch, EAH) were assessed at age 15. Cronbach’s alpha was used to assess internal consistency for all subscales with more than 2 items.
Weight control behaviors for LCA (age 15)
Dieting behavior was examined at age 15 as specific weight control behaviors, assessed by responses to the question, “Have you ever done any of the follow things to lose weight or to keep from gaining weight?” In the current study, 20 weight control behaviors from the comprehensive list developed by French et al. 9 were selected as potential items to be used in the LCA. Behaviors were coded as healthy or unhealthy using French’s classification of the behaviors 9. In order to reduce sparseness in the observed data contingency table, which is particularly important with a sample of this small size, similar items (e.g. eliminate snacking and eliminate sweets and junk) were combined if their correlation was high (~0.70). Thus, the following items were combined into superordinate factors: i) eliminating snacking, sweets, and junk food; ii) reducing the amount of food consumed and calories eaten. Due to the low prevalence (14%) of using at least one unhealthy behavior in the current sample, the unhealthy behaviors (use of laxatives/enemas, diuretics, diet pills, or appetite suppressants, smoking cigarettes, or vomiting) were also combined into a superordinate factor. Response options for each behavior were: never, rarely, sometimes, often, and always. Dichotomous indicators of each weight control behavior were created for use in LCA models for this study: coded two (yes) if they engaged in healthy behaviors “sometimes” or more often and in unhealthy behaviors “rarely” or more often. To compare responses between use of weight control behaviors and reports of dieting, girls were also asked, “Have you ever dieted?”
Anthropometric measurement predictors
Height and weight were measured in triplicate when girls were 5yo and 15yo and were used to compute BMI scores at each time point. BMI percentiles were calculated using the 2000 CDC Growth Charts; overweight was defined as a BMI > 85th percentile on the basis of a standardized reference criteria 18. Pubertal status via breast development was measured at age 11 through visual inspection by a nurse who was trained by Dr. Herman-Giddens using the published training manual 19. Ratings were obtained for each breast on a scale of 1-5 (1=no development, 5= mature) using the Tanner rating system 20, and averaged together to create a mean pubertal status score.
Psychological well-being predictors
Children’s perceived self-competence was measured at age 5 using The Pictorial Scale of Perceived Competence and Social Acceptance for Young Children for 4-5 year olds 21. General competence is the mean of cognitive competence and physical competence. Self-esteem was measured at age 15 using a 10-item scale developed by Rosenberg 22 and modified by O’Brien 23 designed to measure global self-esteem. Depression was measured at age 15 using the Center for Epidemiological Studies Depression Scale (CED-D) developed by Radloff 24. It is a 20-item self-report questionnaire. Good internal consistency was observed (α ≥ 0.78) for all psychological well-being predictors.
Temperament predictor
Girls’ inhibitory control was assessed at age 7 by using the parent version of the Children's Behavior Questionnaire’s Inhibitory Control subscale 25. Inhibitory control is defined as the ability to restrain a dominant response and instead perform a subdominant response. Good internal consistency was observed for inhibitory control (α = 0.74).
Eating and weight-related characteristics
Children’s body satisfaction at age 5 was measured using an amended Body Satisfaction Scale 26. The Body Satisfaction Scale originally consisted of a list of 16 body parts, half involving the head and the other half involving the body. The amended version contains an additional 10 items concerning various body parts and reduced the response set to: “too little,” “too big,” “just right.” Fear of fat in children was assessed at age 9 using the personal fear of fat scale (5 items) on the Fear of Becoming Fat 27. Dietary restraint and disinhibition were measured at age 15 using the original Dutch Eating Behavior Questionnaire (DEBQ) 28. For this study, overall total disinhibition, defined as the sum of external and emotional disinhibition, was used as the measure of disinhibition. Weight concerns at age 15 were measured using the Weight Concerns scale 29. Dieting risk at age 15 was assessed using the dieting subscale on the Eating Attitudes Test (EAT-26), the summarized version of the EAT-40 30. A higher dieting risk score indicates increased dieting behaviors and practices, concern about weight, and food avoidance. Binge eating at age 15 was assessed using the Binge Eating Scale 31, designed to assess the behavioral aspects of binge eating episodes as well as the feelings and thoughts associated with this behavior. Good internal consistency was observed for all eating and weight-related characteristics (all α ≥ 0.74). Dieting frequency was assessed at age 15 by a one-item measure, “During the past year, how often did you diet (by diet, we mean changing the way you eat to control your weight)?” Response options were: never, less than once a month, 1 to 3 a month, 2 to 6 times per week, and every day.
Dietary intake
All dietary intake data was collected when girls were 15yo. Girls’ self-reported intakes were measured using three 3 24-hr recalls, 2 weekdays and 1 weekend day, randomly selected over a 2-wk period. Interviews were conducted by trained staff using computer-assisted Nutrition Data System for research (NDS-R, Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN). Nutrient data were averaged across three days to obtain an estimate of energy and nutrient intakes and are based on food only. Physiologically plausible reports of energy intake were determined by comparing reported energy intake with predicted energy requirements using procedures outlined by Huang et al. 32. A detailed description of this procedure is described elsewhere 32. Briefly, sex- and age-specific standard deviation (SD) cutoffs were created for reported energy intake as a percent of predicted energy requirement 33. A girl was considered a plausible reporter if reported energy intake as a percent of predicted energy requirements was within the ±1 SD cutoff (at 15ys). Those with values exceeding the upper bounds were categorized as “over-reporters,” and those with values below the lower cutoff value were categorized as “under-reporters.”
Weighed intake was measured in the laboratory for both a standardized lunch and the Eating in the Absence of Hunger (EAH) protocol. For lunch, each girl was given a 12 inch (580 kcal) Subway sandwich (choice of turkey, ham, or cheese), a Subway mustard packet, a Subway mayonnaise packet (35 kcal), a 12 oz. can of Minute Maid Lemonade (150 kcal), a Rice Krispies Treat (90 kcal), and 1.5 oz. (160 kcal) bag of Synder’s of Hanover pretzels, for a total of 1,015 kcal. The EAH protocol was developed to measure children’s snack food consumption in the presence of palatable foods while in the absence of hunger 34. Approximately 70 min after lunch, each girl was given a preload of a Dannon Frusion yogurt smoothie (260 kcal). Approximately 20 min following the preload, girls were presented with generous portions of 5 snack foods: 75g (375 kcal) of Frito Lay Nacho Cheese Doritos, 84g (480 kcal) of Pringles potato chips, 112g (520 kcal) of Nabisco Nutter Butter Sandwich Cookies, 96g (495 kcal) of Keebler Fudge Shoppe Stripe Cookies, and 65g (365 kcal) of Hershey’s Milk Chocolate Nuggets, and were asked to rate their preference and liking of each food. Each girl was offered a total of 2,235 kcal.
Statistical analyses
All data analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC). Descriptive statistics were computed for all predictor and all dietary variables. Chi-square was used to examine differences in weight status and plausibility of reporting by weight control group. Statistical significance was defined as p ≤ 0.05.
Latent class analysis (LCA) is a person-centered measurement method used to identify an underlying latent grouping variable that is not observed but can be inferred from a set of measured indicators, individual weight control behaviors assessed at age 15 in this case. A detailed description of this procedure is described elsewhere 35. Parameters estimated in LCA include class membership probabilities, defined as the proportion of a population expected to belong to each latent class and sum to one, and item-response probabilities, defined as the probability of endorsing each item given class membership 35. Probabilities of items close to one indicate that the item is characteristic of membership in that latent class and that those in that latent class are likely to have tried it as a weight control behavior. Probabilities of items close to zero indicate that individuals in that latent class are not likely to have tried the behavior. In order to reduce sparseness in the observed data contingency table, which is particularly important with a sample of this small size, similar items (e.g. eliminate snacking and eliminate sweets and junk) were combined if their correlation was high (~0.70). Thus, the following items were combined into superordinate factors: i) eliminating snacking, sweets, and junk food; ii) reducing the amount of food consumed and calories eaten. Due to the low prevalence (14%) of using at least one unhealthy behavior in the current sample, the unhealthy behaviors (use of laxatives/enemas, diuretics, diet pills, or appetite suppressants, smoking cigarettes, or vomiting) were combined into a superordinate factor. Items that did not discriminate among groups (e.g. eat a low carbohydrate diet, join diet centers, join weight loss groups) were not included in the final models. Thus, from the original set of 20 weight control behaviors, a final set of 9 weight control behaviors was selected for use in the latent class models.
The final latent class model was identified by comparing latent class models with one to five latent classes to select the model with the optimal fit and best model interpretation using criterion specified by Lanza et al, which are the Akaike’s Information Criterion (AIC), Bayesian Information Criterion (BIC), entropy, and the G2 fit statistic. 35 After the best model was identified, the next step was to explore differences between the weight control groups on a number of individual concurrent (e.g. BMI at 15ys) and antecedent (e.g. BMI at 5ys) characteristics. This was first done directly in the LCA model to help maximize power. Each variable was included separately, one at a time, in the latent class model to examine the estimation of odds ratios that describe the increase in odds of membership in a particular latent class relative to a reference class corresponding to a one-unit change in the variable. In order to aid with the interpretability of the data, differences among weight control behavior groups on individual variables were also tested using ANOVA with Tukey’s honestly significant difference post hoc tests. In order to examine this outside the LCA model, each girl was assigned to the latent weight control group corresponding to her maximum posterior probability of membership using the classify-analyze approach described by Bray et al. 36. Self-reported intake and lunch intake data were adjusted for girls’ estimated energy requirement (EER) to account for differences in energy needs based on height and weight.
Results
Identification of the latent class model
The fit statistics for one to five class models are shown in Table 1. The BIC indicated that the two class solution was the best-fitting model; however, the AIC indicated that the four-class solution was the best-fitting model. Next, we evaluated the entropy of the two to four class models. Both the two and four class models yielded entropies exceeding the recommended .85, however, the three class model did not and thus was no longer considered. Lastly, we evaluated the interpretability of the two and four class models. The two-class solution collapsed all of the dieters into one group, whereas the four class model separated the dieters into three dieting classes that upon investigation were meaningful, qualitatively distinct groups. In addition, the four class model yielded average posterior probabilities of 0.98, 0.88, 0.93, and 0.91, all together indicating that the four-class model provided a good fit to the data.
Table 1.
Fit statistics for latent class models with one to five classes
| AIC1 | BIC2 | Entropy | G2 fit statistic |
Degrees of freedom |
|
|---|---|---|---|---|---|
| 1 class | 660 | 688 | 1.00 | 642 | 502 |
| 2 classes | 245 | 304 | 0.93 | 207 | 492 |
| 3 classes | 219 | 309 | 0.83 | 161 | 482 |
| 4 classes | 204 | 325 | 0.86 | 126 | 472 |
| 5 classes | 212 | 365 | 0.82 | 114 | 462 |
AIC = Akaike’s Information Criterion
BIC = Bayesian Information Criterion
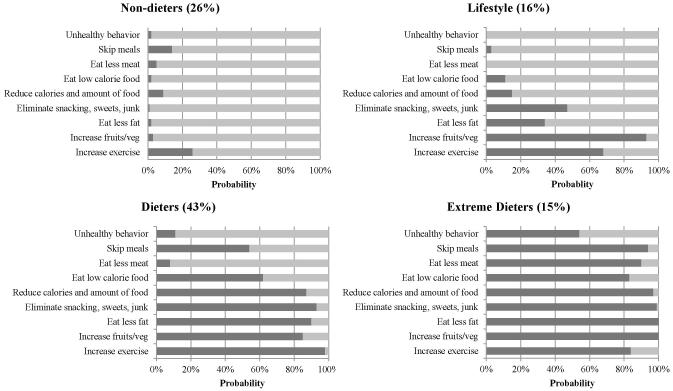
Four class model of weight control behaviors
As shown in Table 2, twenty-six percent of the sample was predicted to belong in latent class 1. This group was named the “Non-dieters” group as it is characterized by a low probability of endorsing all of the 9 weight control behaviors. Three “dieting” weight control groups were identified, and varied in the number and type of weight control behaviors they endorsed. Sixteen percent of the sample was predicted to belong to latent class 2, and is named the “Lifestyle” group since it is characterized by a high probability of reporting increasing exercise and eating more fruits and vegetables for weight control, both health-promoting lifestyle changes. Forty-three percent of the sample was predicted to belong to latent class 3, named the “Dieters” group since it is characterized by a high probability of reporting increasing exercise, increasing fruits and vegetables, eating less fat, eliminate snacks, sweets, and junk, reducing calories and amount of food, and eating low calorie food, behaviors that are all consistent with dieting. Fifteen percent of the sample was predicted to belong to latent class 4. This group is named the “Extreme Dieters” group, and is characterized by a high probability of having used all 9 weight control strategies, including over 50% of the class expected to report using at least one unhealthy weight control behavior. Of the girls in the Extreme Dieters group, 12 girls (48%) did not report using any unhealthy weight control behaviors, 7 girls (28%) reported using 1 unhealthy weight control behavior, 4 girls (16%) reported using 2 unhealthy weight control behaviors, and 2 girls (8%) reported using 4 unhealthy weight control behaviors. Figure 1 depicts the item-response probabilities for each of the weight control groups.
Table 2.
Probability of girls reporting using each weight-control behavior given latent class membership
| Latent class |
||||
|---|---|---|---|---|
| Non-dieters (26%) |
Lifestyle (16%) |
Dieters (43%) |
Extreme Dieters (15%) |
|
| Weight control behavior | ||||
| Increase exercise (72%)1 | 0.26 | 0.69 | 0.98 | 0.84 |
| Eat more fruits and vegetables (67%) | 0.03 | 0.94 | 0.85 | 1.00 |
| Eat less fat (60%) | 0.02 | 0.34 | 0.90 | 1.00 |
| Eliminate snacking, sweets, and junk (63%) | 0.01 | 0.47 | 0.93 | 0.99 |
| Reduce calories and amount of food (57%) | 0.09 | 0.15 | 0.87 | 0.97 |
| Eat low calorie food (42%) | 0.02 | 0.11 | 0.62 | 0.83 |
| Eat less meat (19%) | 0.05 | 0.00 | 0.08 | 0.90 |
| Skip meals (42%) | 0.12 | 0.03 | 0.54 | 0.94 |
| Unhealthy behavior (14%) | 0.02 | 0.00 | 0.11 | 0.54 |
Unhealthy behavior refers to use of laxatives/enemas, diuretics, diet pills, or appetite suppressants, smoking cigarettes, or vomiting
Percent of total sample reporting use of each weight control behavior
Figure 1.
Probability of reporting each weight-control behavior, conditional on membership in weight control group (N=166)
For comparison, 21% of the Non-dieters responded “yes” to having ever dieted. Of the Lifestyle group, 65% responded “yes” to having ever dieted. Of the Dieters, 86% responded “yes” to having ever dieted. Of the Extreme Dieters, 95% responded “yes” to having ever dieted.
Antecedent characteristics predicting latent class membership
As shown in Table 3, BMI at 5ys, fear of fat at 9ys and pubertal development at 11ys were all significant predictors of weight control behavior group membership at age 15, and inhibitory control at 7ys was a marginally significant predictor of group membership at age 15. To provide additional information to help with interpretation of the weight control groups, mean values for the antecedent predictor variables are shown by weight control group in Table 4.
Table 3.
Odds ratios for individual effects of antecedent predictors of membership in the 3 dieting groups relative to the Non-dieters group
| P value | Lifestyle (16%) |
Dieters (43%) |
Extreme Dieters (15%) |
|
|---|---|---|---|---|
|
|
||||
| BMI (5ys) | *** | 1.05 (0.81, 1.36) |
1.12 (0.92, 1.37) |
1.51
(1.20, 1.90) |
| Self-competence (5ys)1 | NS | 0.89 (0.54, 1.47) |
1.09 (0.73, 1.63) |
0.71 (0.45, 1.12) |
| Body satisfaction (5ys)2 | NS | 1.24 (0.36, 4.23) |
0.86 (0.37, 2.01) |
0.47 (0.17, 1.30) |
| Inhibitory control (7ys)3 | * | 1.21 (0.67, 2.21) |
1.19 (0.76, 1.86) |
0.53
(0.31, 0.91) |
| Fear of fat (9ys)4 | *** | 1.57 (0.60, 4.08) |
3.60
(1.72, 7.52) |
4.66
(2.10, 10.35) |
| Pubertal status (11ys)5 | ** | 1.81 (0.82, 3.98) |
2.12 (0.99, 3.85) |
3.26
(1.49, 7.13) |
Non-dieters group was used as reference class. Predictors entered in separate logit models. Reference latent class has odds of ratio 1.0. Increase in log-odds of membership in latent class relative to membership in reference class corresponding to one-unit change in predictor.
P < 0.10,
P < 0.05,
P < 0.01,
****P < .0001
Meausred using The Pictorial Scale of Perceived Competence and Social Acceptance for Young Children
Measured using an amended Body Satisfaction Scale
Measured using mothers’ reports on CBQ
Measured using Fear of Fat Scale
Measured using tanner staging of breast development
Table 4.
Descriptive characteristics for antecedent covariates for the weight control behavior groups
| Latent Class | ||||
|---|---|---|---|---|
|
| ||||
| Non-dieters (26%) |
Lifestyle (16%) |
Dieters (43%) |
Extreme Dieters (15%) |
|
|
|
||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| BMI percentile (5ys)1 | 55.2 (24.3)a | 56.4 (22.1)a | 58.5 (29.4)a | 74.3 (22.6)b |
| Self-competence (5ys)2 | 7.0 (0.7)ab | 6.9 (1.0)ab | 7.1 (0.7)a | 6.7 (1.3)b |
| Body satisfaction (5ys)3 | 2.7 (0.5)a | 2.7 (0.3)a | 2.6 (0.5)a | 2.5 (0.4)a |
| Inhibitory control (7ys)4 | 5.0 (0.9)a | 5.2 (0.6)a | 5.1 (0.7)a | 4.6 (0.8)b |
| Fear of fat (9ys)5 | 1.3 (0.5)a | 1.4 (0.5)a | 1.8 (0.7)b | 2.0 (1.0)b |
| Pubertal status (11ys)6 | 1.9 (0.6)a | 2.3 (0.8)b | 2.3 (0.8)b | 2.6 (0.8)b |
Means sharing the same superscript are not significantly different from each other (P<0.05).
While BMI was included as a covariate, data are shown here as BMI percentiles to aid in interpretation.
Meausred using The Pictorial Scale of Perceived Competence and Social Acceptance for Young Children; range 1(low) to 8(high)
Measured using an amended Body Satisfaction Scale; range 1(low) to 3(high)
Measured using mothers’ reports on CBQ; range 1(low) to 7 (high)
Measured using Fear of Fat Scale; range 1(low) to 4(high)
Measured using tanner staging of breast development at 11y; range 1(low) to 5(high)
Girls in the Extreme Dieters group had higher BMI percentiles at 5ys and lower levels of inhibitory control at 7ys than girls in the other three groups, and had higher fear of fat at 9ys than girls in the Lifestyle or Non-dieters groups. With every one-point decrease in inhibitory control, girls were twice as likely to be in the Extreme Dieters group than to be in the Non-dieters group, and girls in the Extreme Dieters group had significantly lower inhibitory control at 7ys than girls in the other three groups. Similarly, with every one-point increase in BMI at 5ys, girls were 1.5 times more likely to be in the Extreme Dieters group than to be in the Non-dieters group, and girls in the Extreme Dieters group had significantly higher BMIs at 5ys than girls in the other three groups. The proportion of girls classified as normal weight vs. overweight at 5yo differed by group membership (p < .05). At 5ys, 12% of Non-dieters were overweight or obese, 8 % of the girls in the Lifestyle group were overweight or obese, 20 % of Dieters were overweight or obese, and 38 % of Extreme Dieters were overweight or obese.
Concurrent characteristics predicting latent class membership
As shown in Table 5, all concurrent covariates, measured at 15ys, were significant predictors of weight control group membership. Percent body fat, restraint, weight concerns, self-esteem, depression, binge eating, and dieting frequency independently predicted membership in all three dieting groups (Lifestyle, Dieters, Extreme Dieters) relative to the Non-dieters group. Using percent body fat as an example, with every one-point unit increase in percent body fat, girls were 1.09 times more likely to be in the Lifestyle group, 1.12 times more likely to be in the Dieters group, and 1.24 times more likely to be in the Extreme Dieters group than to be in the Non-dieters.
Table 5.
Odds ratios for individual effects of concurrent (age 15) predictors on membership in the 3 dieting groups relative to the Non-dieters group
| P value | Lifestyle (16%) |
Dieters (43%) |
Extreme Dieters (15%) |
|
|---|---|---|---|---|
|
|
||||
| BMI | **** | 0.97 (.86, 1.10) |
1.09
(1.01, 1.18) |
1.27
(1.14, 1.39) |
| Body fat %1 | **** |
1.09
(1.01, 1.17) |
1.12
(1.06, 1.19) |
1.24
(1.14, 1.34) |
| Restraint2 | **** |
4.53
(1.47, 13.95) |
27.22
(9.39, 78.88) |
129.87
(35.41, 476.28) |
| Disinhibition3 | **** | 0.67 (0.30, 1.50) |
2.41
(1.37, 4.26) |
4.59
(2.35, 8.97) |
| Weight concerns4 | **** |
6.37
(1.89, 21.44) |
23.55
(6.85, 80.88) |
156.91
(34.61, 711.28) |
| Dieting risk5 | **** | 1.05 (0.62, 1.79) |
1.68
(1.17, 2.40) |
2.73
(1.84, 4.06) |
| Self-esteem6 | **** | 0.89 (0.77, 1.01) |
0.79
(0.70, 0.88) |
0.68
(0.59, 0.78) |
| Depression7 | **** |
1.08
(1.01, 1.16) |
1.13
(1.06, 1.20) |
1.21
(1.13, 1.30) |
| Binge eating8 | **** | 1.09 (0.97, 1.21) |
1.18
(1.08, 1.29) |
1.36
(1.23, 1.51) |
| Dieting frequency9 | **** |
5.00
(1.45, 17.26) |
8.62
(2.68, 27.72) |
12.64
(3.78, 42.40) |
Non-dieters as reference class. Reference latent class has odds of ratio 1.0. Predictors entered in separate logit models. *P < 0.10, **P < 0.05, ***P < 0.01,
P < .0001
Body fat percentage was measured using Dual-energy X-Ray absorptiometry (DXA).
Measured using the restraint subscale from the DEBQ
Measured using the disinhibition subscale from the DEBQ)
Measured using the Weight Concerns Scale
Measured using the Dieting subscale on the EAT
Measured using the Rosenberg Self-Esteem Scale
Measured using the CES-D
Measured using the Binge Eating Scale
Dieting frequency is self-reported, measured as the frequency of dieting during the past year.
To provide additional information to aid in interpretation of the weight control groups, mean values for the concurrent predictor variables are shown by weight control group in Table 5. Levels of restraint, weight concerns, and self-reported dieting frequency increased on an ordinal scale across groups, from Non-dieters to Extreme Dieters. As shown in Table 6, girls in the Extreme Dieters group had significantly higher values for all of the measured covariates (with the exception of self-esteem, which was significantly lower) than girls in the other 3 groups; girls in the Dieters group had higher values than girls in Lifestyle or Non-dieters on disinhibition, depression, dieting risk, and had lower self-esteem.
Table 6.
Descriptive characteristics and concurrent (age 15) covariates for the weight control behavior groups
| Latent Class | ||||
|---|---|---|---|---|
|
| ||||
| Non-dieters (26%) |
Lifestyle (16%) |
Dieters (43%) |
Extreme Dieters (15%) |
|
|
|
||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| BMI percentile1 | 55.5 (28.2)a | 52.1 (21.9)a | 63.1 (22.4)b | 81.2 (17.9)c |
| Body fat %2 | 24.6 (6.0)a | 26.9 (5.0)ab | 28.4 (5.0)b | 32.5 (6.2)c |
| Restraint3 | 1.3 (0.4)a | 1.7 (0.5)b | 2.6 (0.6)c | 3.4 (0.7)d |
| Disinhibition4 | 2.1 (0.6)a | 1.9 (0.5)a | 2.5 (0.6)b | 2.8 (0.7)c |
| Weight concerns5 | 0.4 (0.5)a | 1.0 (0.4)b | 1.5 (0.7)c | 2.5 (0.7)d |
| Dieting risk6 | 0.3 (0.8)a | 0.2 (0.7)a | 1.3 (1.8)b | 6.1 (3.9)c |
| Self-esteem7 | 36.8 (3.5)c | 34.9 (3.5)c | 32.2 (4.9)b | 26.8 (6.0)a |
| Depression8 | 6.5 (5.9)a | 9.8 (6.5)a | 14.1 (8.1)b | 22.2 (12.9)c |
| Binge eating9 | 4.4 (3.8)a | 6.3 (4.4)ab | 8.3 (5.4)b | 18.8 (8.9)c |
| Dieting frequency10 | 1.1 (0.3)a | 1.6 (1.1)b | 2.1 (1.1)c | 2.6 (1.2)d |
Means sharing the same superscript are not significantly different from each other (P<0.05).
While BMI was included as a covariate, data are shown here as BMI percentiles to aid in interpretation.
Body fat percentage was measured using Dual-energy X-Ray absorptiometry (DXA).
Measured using the restraint subscale from the DEBQ; range 1(low) to 5(high)
Measured using the disinhibition subscale from the DEBQ; range 1(low) to 5(high)
Measured using the Weight Concerns Scale; range 0(low) to 5(high)
Measured using the Dieting subscale on the EAT; range 0(low) to 27(high)
Measured using the Rosenberg Self-Esteem Scale; range 10(low) to 40 (high)
Measured using the CES-D; range 0 (low) to 60 (high)
Measured using the Binge Eating Scale; range 0(low) to 46 (high)
Dieting frequency is self-reported, measured as the frequency of dieting from never (1) to everyday (5) during the past year.
The proportion of girls classified as normal weight vs. overweight/obese at age 15 differed by group membership (p < .001); 17% of Non-dieters were overweight/obese, 8 % of the girls in the Lifestyle group were overweight/obese, 16 % of Dieters were overweight/obese, and 56 % of Extreme Dieters were overweight/obese.
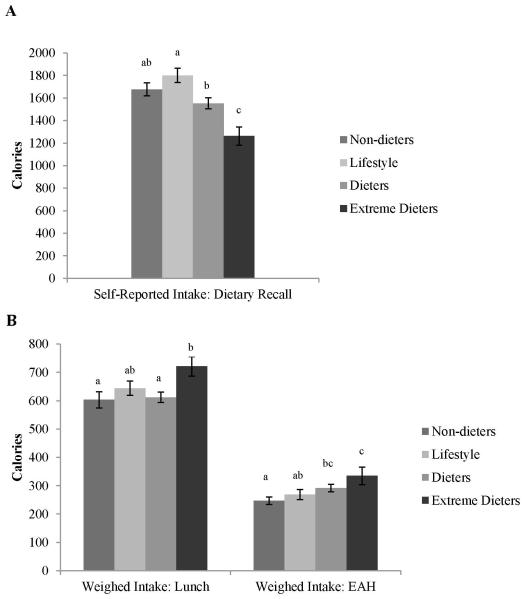
Concurrent weight control group differences in dietary intake
Mean self-reported intake is shown by weight control group in Figure 2a. Self-reported intake based on 3 24hr recalls differed by weight control group (p < 0.0001). Girls in the Extreme group reported that they consumed significantly fewer calories than girls in the other weight control groups (p < .05); these girls reported an average of 1263±405 calories per day, compared to 1668±395, 1789±325, and 1553±401 calories by girls in the Non-dieters, Lifestyle, and Dieters groups, respectively. The plausibility of reporting of self-reported intake also differed by group membership (p < .05). In the Non-dieters group, 60% were identified as under-reporters, 38% as plausible reporters, and 2% as over-reporters. In the Lifestyle group, 58% were identified as under-reporters, 38% as plausible reporters, and 4% as over-reporters. In the Dieters group, 75% were identified as under-reporters, 22% as plausible reporters, and 3% as over-reporters. In the Extreme Dieters group, 96% were identified as under-reporters and 4% as plausible reporters.
Figure 2.
Self-reported and weighed dietary intakes are shown by weight control group. Self-reported intake (A) based on 3 24h multiple-pass dietary recalls. Percent underreporting differed by group (61% for Non-dieters, 58% for Lifestyle, 75% for Dieters, and 96% for Extreme Dieters). Weighed intake (B) was measured at lunch and the Eating in Absence of Hunger (EAH) paradigm. 1,015 kcal were offered at the lunch, and 2,235 kcal were offered during EAH. Data are shown as means plus standard error. Means sharing the same superscript are not significantly different from each other (P<0.05).
In contrast, as shown in Figure 2b, the weighed intake data obtained at the standardized lunch consumed in the laboratory revealed a very different pattern of findings. Overall, the groups differed in their lunch intake (p < 0.01); girls in the Non-dieters, Lifestyle, Dieters, and Extreme Dieters groups consumed 603±186, 661±148, 606±140, and 721±171 calories, respectively. Girls in the Extreme Dieters group consumed significantly more calories than girls in the Non-dieters and Dieters groups (p < .05). A similar pattern emerged in the EAH protocol (p < 0.05); girls in the Non-dieters, Lifestyle, Dieters, and Extreme Dieters groups consumed 247±86, 269±86, 291±109, and 335±164 calories, respectively. Girls in the Extreme Dieters group consumed more calories in EAH than girls in Non-dieters or Lifestyle groups (p <0.05), and marginally significantly more than girls in the Dieters (p <. 10). When total weighed intake in the laboratory was examined as a combination of lunch and EAH, girls in the Extreme Dieters group consumed significantly more (1049 ± 306) calories than girls in the other three groups (850 ± 230, 909 ± 179 and 908 ± 211 for girls in the Non-dieters, Lifestyle, and Dieters, respectively).
DISCUSSION
These findings underscore the view that dieting is not a singular behavior; but is an umbrella term for a wide range of both healthy and unhealthy weight control behaviors. The results revealed four groups using distinct patterns of weight control behaviors in the current sample of adolescent girls: Non-dieters, and three groups of self-reported dieters, Lifestyle, Dieters, and Extreme Dieters. The dieting groups increased in the number and severity of reported weight control behaviors from Lifestyle to Extreme Dieters. These groups were also qualitatively different on a number of psychosocial and weight characteristics, with levels of dietary restraint, weight concerns, and self-reported dieting frequency increasing across groups, from non-dieters to Extreme Dieters. Results from the current study expand on the literature using LCA to identify patterns of weight control behaviors in women 13,14 to a sample of adolescent females. These findings are similar to those obtained with the women, with appropriate differences noted due to the discrepancy in developmental stage, such as the absence of use of decreased alcohol as a weight control behavior. Risk factors for membership in the Extreme Dieters group were noted as early as 5ys; with every one-point decrease in inhibitory control, girls were twice as likely to be in the Extreme Dieters group than to be in the Non-dieters group, and with every one-point increase in BMI, girls were 1.5 times more likely to be in the Extreme Dieters group than to be in the Non-dieters group. Girls in the Extreme Dieters group were more likely to be under-reporters, and had lowest self-reported intake, but ate significantly more in the laboratory.
Predictors of dieting group membership were apparent as early as age 5. This is consistent with previous work indicating that early overweight status is a risk factor for later weight concerns and eating pathology. It was shown in prior work in this sample that the girls who were overweight at 5ys had higher levels of disinhibited eating, dietary restraint, weight concern, body dissatisfaction 15, and dieting at 9ys 7, which puts them at risk for continued overweight and dieting attempts, as seen in the current study. The current findings add to the literature that weight status at 5ys also predicts an increased frequency of self-reported dieting and use of unhealthy weight control behaviors at 15ys. Thus early weight management may help prevent later weight gain, which may help decrease early attempts at dieting and later use of unhealthy weight control behaviors. While inhibitory control increases from middle childhood to adolescence 37, rank-order differences in inhibitory control are relatively stable over time 38. Inhibitory control is an important factor in dieting success 39 and in early weight gain 40. Thus, it is possible that initial attempts to control weight might not be successful for girls with low inhibitory control and thus they turn to the more unhealthy weight control behaviors in their later attempts. While the results from the current study indicate this as a possibility, future work is needed to confirm this finding. Given that risk factors for later membership in the Extreme Dieters group were present as early as 5yo, these findings suggest that there is a need to start prevention interventions in the areas of self-regulation and weight management early, in childhood, to prevent the later use of unhealthy weight control behaviors.
All of the concurrent descriptive variables were significant predictors of group membership, with self-reported dieting frequency, restraint, and weight concerns increasing on an ordinal scale across groups, from non-dieters to Extreme Dieters. The relationship between weight concerns and group membership is consistent with past findings that weight concerns are one of the strongest correlates of dieting and weight control practices among adolescents and adults 29,41. The current study adds that greater weight concerns are related to the use of an increased number of and more unhealthy weight control behaviors. The increase in percent overweight and body fat at age 15 across the groups is consistent with previous research that adolescents who are overweight and obese are more likely to diet 6 and use unhealthy weight control behaviors 41. Girls in the Extreme Dieters group have the lowest inhibitory control and greatest disinhibition, which may make it harder for these girls to sustain both healthy and unhealthy weight control behaviors, and may lead to loss of control and subsequent weight gain 42. Taken together, this suggests that for those who would likely benefit from weight reduction or maintenance, physicians and other health professionals should emphasize the importance of using health-promoting weight control behaviors (e.g. increasing physical activity and fruit and vegetable consumption and decreasing consumption of high energy-dense food) as part of a lifestyle change without emphasizing it as dieting. It is necessary that health care providers not only provide adolescents with the knowledge of why this is important, but also with the skills and support to help successfully implement these behaviors.
Psychological well-being, examined in the current study as both decreased self-esteem and increased depression, decreased on an ordinal scale across the three dieting groups, from Lifestyle to Extreme Dieters. This is consistent with previous findings that both self-esteem 43 and depression 8 are associated with dieting, disordered eating and the use of unhealthy weight control behaviors 44 in children and adolescents, and suggests that successful weight control interventions might include treatment for depression and components aimed at increasing self-esteem, which may help mitigate the use of unhealthy weight control behaviors. Dieting and disordered eating persist and increase 45 into young adulthood, suggesting that the girls in the study who are using unhealthy weight control behaviors at age 15 will continue to do so. This is a problem because the use of unhealthy weight control behaviors increases the risk for disordered eating and clinical eating disorders 3, could inhibit proper growth and development 46, and many of the unhealthy weight control behaviors, such as smoking, increase health risks in other domains 47.
Examining associations between dieting and measures of food intake such as self-reported intake and the EAH protocol provides an opportunity to look at possible consequences of dieting on food intake. In the current study, weight control group differences for self-reported intake and weighed intake measures show strikingly different patterns. Previous associations between reported dieting and nutrient intake have been mixed, likely due to differences in dietary assessment (e.g., food frequency questionnaires vs. dietary recall) and inconsistent categorization (e.g., yes/no dieting vs. specific weight control behaviors) of dieting and weight control behaviors10,11. A comparison of self-reported intake from dietary recalls across groups shows that girls in the Extreme Dieters group are, based on their self-reports, consuming the fewest calories, which is consistent with their greatest frequency of dieting attempts. However, weighed intake in the laboratory indicates that girls in the Extreme Dieters group are actually eating significantly more, even after adjusting for potential differences in energy requirements. Taken together, this suggests that the group differences in self-reported intake may reflect differences in the extent to which girls are underreporting, which is reflected in differences of plausible reporters, and might not accurately reflect differences in actual intake.
Extreme Dieters had the highest average BMI percentile, the greatest levels of restraint, and most were classified as under-reporters. This is consistent with previous research, given that increased weight status is one of the strongest predictors of underreporting in children 16, and research indicates that those high in restraint are more likely to underreport their intake 48. Dietary restraint reflects a cognitive desire and intent to restrict intake 49. Thus, particularly in those who are overweight and high in restraint, self-reported intake might reflect intended, but not actual, intake. Girls in the Extreme Dieters group might have a greater tendency to underreport their intake given their higher levels of restraint and increased weight status, but have greater reactivity and actually consume the most calories when presented with food, as shown in the current study. While the current findings need to be replicated in another sample with both self-reported and weighed intake, these findings support the recent expert report by the Energy Balance Measurement Working Group 50 that self-reported intake can be inaccurate and does not necessarily portray actual patterns of intake. Thus, results from studies relying on self-reported intake in dieters or those high in dietary restraint and/or reactivity need to be interpreted with caution, as this data might reflect intended intake and not actual intake. Future studies should include both self-reported and weighed intake to gain insight into multiple aspects of eating behavior in this population.
The current study is not without limitations. The current sample was homogenous – white adolescent females from middle-class families, and thus the results may not generalize to other populations. Additionally, much of the data, including the use of specific weight control practices, is self-reported data, which might have resulted in reporting and social desirability bias. However, this is a limitation of the field as a whole, and future research should focus on developing tools that assess aspects of weight control behavior that do not rely on self-report. Another limitation is that due to the exploratory nature of this paper, weight control behavior was assessed at only one time point. Future work should assess weight control behavior at repeated time points to capture the dynamic nature of weight control behavior. While one limitation of LCA is that it can create artificial subtypes in a data set, this study used LCA in an exploratory manner to tease apart and describe multiple naturalistic patterns of health-promoting weight control behaviors.
In conclusion, findings from the current study advance our understanding of what weight control behaviors adolescent girls use when they diet. The current study found that there were three patterns of self-reported dieting in 15yo girls, increasing in the number of reported weight control behaviors used and distinct in antecedent and concurrent descriptive characteristics, the majority of which increased pursuant to the dieting groups. Early weight status and inhibitory control were identified as early risk factors for membership in the Extreme Dieters group at age 15. Analysis of the dietary data supports the theory that under-reporting in those high in restraint reflects intended restriction, not actual restricted intake 49. These findings underscore the view that adolescent dieting is an umbrella term representing a wide range of both healthy and unhealthy weight control behaviors. Thus, it is necessary to not just assess dieting, as there are significant discrepancies around this term, but also any weight control behaviors used. Given that dieting is implicated as a causal factor for a number of disorders (e.g. obesity, eating disorders 2,3), in order to identify etiological factors it is necessary to distinguish between patterns of weight control behaviors. Future work should focus on using this information to help target interventions for girls who have early risk factors for membership in the Extreme Dieters group to help reduce the later use of unhealthy weight control behaviors. Given the observed relationship between the use of unhealthy weight control behaviors and aspects of health (e.g. lower psychological well-being), health professionals should start screening for the use of unhealthy weight control behaviors. Including this as a regular screening in well-child visits could help identify girls who might be at an elevated risk of developing a later eating disorder.
ACKNOWLEDGEMENTS
This research was supported by NIH HD32973 (L. Birch) and USDA National Institute for Food and Agriculture Grant # 2011-67001-301 Program A2121 - Childhood Obesity Prevention: Transdisciplinary Graduate Education and Training in Nutrition and Family Sciences (K. Balantekin). We thank Stephanie T. Lanza of the Methodology Center at The Pennsylvania State University for her consultation on latent class analysis.
References
- 1.Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, et al. Youth risk behavior surveillance-United States, 2011. MMWR Surveill Summ. 2012;61:1–162. [PubMed] [Google Scholar]
- 2.Field AE, Austin SB, Taylor CB, Malspeis S, Rosner B, Rockett HR, et al. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics. 2003;112:900–906. doi: 10.1542/peds.112.4.900. [DOI] [PubMed] [Google Scholar]
- 3.Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, Eisenberg M. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: How do dieters fare 5 years later? J Am Diet Assoc. 2006;106:559–568. doi: 10.1016/j.jada.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Levine MP, Smolak L, Hayden H. The relation of sociocultural factors to eating attitudes and behaviors among middle school girls. J Early Adolesc. 1994;14:471–490. [Google Scholar]
- 5.Pike KM, Rodin J. Mothers, daughters, and disordered eating. J of Abnorm Psychol. 1991;100:198–204. doi: 10.1037//0021-843x.100.2.198. [DOI] [PubMed] [Google Scholar]
- 6.Balantekin KN, Savage JS, Marini ME, Birch LL. Parental encouragement of dieting promotes daughters’ early dieting. Appetite. 2014;80:190–196. doi: 10.1016/j.appet.2014.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davison KK, Markey CN, Birch LL. A longitudinal examination of patterns in girls' weight concerns and body dissatisfaction from ages 5 to 9 years. Int J Eat Disorder. 2003;33:320–332. doi: 10.1002/eat.10142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sinton MM, Birch LL. Weight status and psychosocial factors predict the emergence of dieting in preadolescent girls. Int J Eat Disorder. 2005;38:346–354. doi: 10.1002/eat.20176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.French SA, Perry CL, Leon GR, Fulkerson JA. Dieting behaviors and weight change history in female adolescents. Health Psychol. 1995;14:548–555. doi: 10.1037//0278-6133.14.6.548. [DOI] [PubMed] [Google Scholar]
- 10.Nowak M. The weight-conscious adolescent: Body image, food intake, and weight-related behavior. J Ad Health. 1998;23:389–398. doi: 10.1016/s1054-139x(97)00263-2. [DOI] [PubMed] [Google Scholar]
- 11.Woodruff SJ, Hanning RM, Lambraki I, Storey KE, McCargar L. Healthy Eating Index-C is compromised among adolescents with body weight concerns, weight loss dieting, and meal skipping. Body Image. 2008;5:404–408. doi: 10.1016/j.bodyim.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 12.Story M, Neumark-Sztainer D, Sherwood N, Stang J, Murray D. Dieting status and its relationship to eating and physical activity behaviors in a representative sample of US adolescents. J Am Diet Assoc. 1998;98:1127. doi: 10.1016/S0002-8223(98)00261-2. [DOI] [PubMed] [Google Scholar]
- 13.Lanza ST, Savage JS, Birch LL. Identification and Prediction of Latent Classes of Weight-loss Strategies Among Women. Obesity. 2010;18:833–840. doi: 10.1038/oby.2009.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Savage JS, Birch LL. Patterns of Weight Control Strategies Predict Differences in Women's 4-Year Weight Gain. Obesity. 2010;18:513–520. doi: 10.1038/oby.2009.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shunk JA, Birch LL. Girls at risk for overweight at age 5 are at risk for dietary restraint, disinhibited overeating, weight concerns, and greater weight gain from 5 to 9 years. J Am Diet Assoc. 2004;104:1120–1126. doi: 10.1016/j.jada.2004.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savage JS, Mitchell DC, Smiciklas-Wright H, Symons Downs D, Birch LL. Plausible reports of energy intake may predict body mass index in pre-adolescent girls. J Am Diet Assoc. 2008;108:131–135. doi: 10.1016/j.jada.2007.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parent A-S, Teilmann G, Juul A, Skakkebaek NE, Toppari J, Bourguignon J-P. The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocr rev. 2003;24:668–693. doi: 10.1210/er.2002-0019. [DOI] [PubMed] [Google Scholar]
- 18.Kuczmarksi RJ, Ogden CL, Grummer-Strawn LM, Flegalm KM, Guo SS, Wei R. CDC growth charts for the United States: methods and development (Vol. Series Report 11, No. 246) National Center of Health Statistics; Hyattsville, MD: 2000. [PubMed] [Google Scholar]
- 19.Herman-Giddens ME, Bourdony CJ. Assessment of Sexual Maturity Stages in Girls. American Academy of Pediatrics. 2005 [Google Scholar]
- 20.Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harter S, Pike R. The pictorial scale of perceived competence and social acceptance for young-children. Child Dev. 1984;55:1969–1982. [PubMed] [Google Scholar]
- 22.Rosenberg M. Society and the adolescent self-image. Psychiatr Q. 1965;39:751–751. [Google Scholar]
- 23.O'brien EJ. Global self-esteem scales - unidimensional or multidimensional. Psychol Rep. 1985;57:383–389. [Google Scholar]
- 24.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 25.Rothbart MK, Ahadi SA, Hershey KL, Fisher P. Investigations of temperament at three to seven years: The children's behavior questionnaire. Child Dev. 2001;72:1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- 26.Slade PD, Dewey ME, Newton T, Brodie D, Kiemle G. Development and preliminary validation of the Body Satisfaction Scale (BSS) Psychol Health. 1990;4:213–220. [Google Scholar]
- 27.Shapiro S, Newcomb M, Burns Loeb T. Fear of fat, disregulated-restrained eating, and body-esteem: prevalence and gender differences among eight-to ten-year-old children. J Clin Child Psychol. 1997;26:358–365. doi: 10.1207/s15374424jccp2604_4. [DOI] [PubMed] [Google Scholar]
- 28.Van Strien T, Frijters JER, Bergers GPA, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disorder. 1986;5:295–315. [Google Scholar]
- 29.Killen JD, Taylor CB, Hayward C, Wilson DM, Haydel KF, Hammer LD, et al. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls - a 3-year prospective analysis. Int J Eat Disorder. 1994;16:227–238. doi: 10.1002/1098-108x(199411)16:3<227::aid-eat2260160303>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 30.Garner DM, Garfinkel PE. Eating attitudes test - index of the symptoms of anorexia-nervosa. Psychol Med. 1979;9:273–279. doi: 10.1017/s0033291700030762. [DOI] [PubMed] [Google Scholar]
- 31.Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7:47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 32.Huang TTK, Roberts SB, Howarth NC, McCrory MA. Effect of screening out implausible energy intake reports on relationships between diet and BMI. Obes Res. 2005;13:1205–1217. doi: 10.1038/oby.2005.143. [DOI] [PubMed] [Google Scholar]
- 33.Goldberg G, Black A, Jebb S, Cole T, Murgatroyd P, Coward W, et al. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr. 1991;45:569–581. [PubMed] [Google Scholar]
- 34.Fisher JO, Birch LL. Restricting access to palatable foods affects children's behavioral response, food selection, and intake. Am J Clin Nutr. 1999;69:1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- 35.Lanza ST, Collins LM, Lemmon DR, Schafer JL. PROC LCA: A SAS procedure for latent class analysis. Struct Equ Modeling. 2007;14:671–694. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bray BC, Lanza ST, Tan X. Eliminating bias in classify-analyze approaches for latent class analysis. Struct Equ Modeling. 2015;22:1–11. doi: 10.1080/10705511.2014.935265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barkley RA. Attention-deficit Hyperactivity Disorder and the Nature of Self-control. Guilford Press; 1997. [Google Scholar]
- 38.Kochanska G, Murray K, Jacques TY, Koenig AL, Vandegeest KA. Inhibitory control in young children and its role in emerging internalization. Child Devel. 1996;67:490–507. [PubMed] [Google Scholar]
- 39.Nederkoorn C, Houben K, Hofmann W, Roefs A, Jansen A. Control yourself or just eat what you like? Weight gain over a year is predicted by an interactive effect of response inhibition and implicit preference for snack foods. Health Psychol. 2010;29:389. doi: 10.1037/a0019921. [DOI] [PubMed] [Google Scholar]
- 40.Anzman SL, Birch LL. Low Inhibitory Control and Restrictive Feeding Practices Predict Weight Outcomes. Journal Pediatr. 2009;155:651–656. doi: 10.1016/j.jpeds.2009.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Neumark-Sztainer D, Story M, Hannan PJ, Perry CL, Irving LM. Weight-related concerns and behaviors among overweight and nonoverweight adolescents - Implications for preventing weight-related disorders. Arch Pediatr Adolesc Med. 2002;156:171–178. doi: 10.1001/archpedi.156.2.171. [DOI] [PubMed] [Google Scholar]
- 42.Field AE, Byers T, Hunter DJ, Laird NM, Manson JE, Williamson DF, et al. Weight cycling, weight gain, and risk of hypertension in women. Am J Epidemiol. 1999;150:573–579. doi: 10.1093/oxfordjournals.aje.a010055. [DOI] [PubMed] [Google Scholar]
- 43.Joiner GW, Kashubeck S. Acculturation, body image, self-esteem, and eating-disorder symptomatology in adolescent Mexican American women. Psychol Women Quart. 1996;20:419–435. [Google Scholar]
- 44.Goldfield GS, Moore C, Henderson K, Buchholz A, Obeid N, Flament MF. Body dissatisfaction, dietary restraint, depression, and weight status in adolescents. J Sch Health. 2010;80:186–192. doi: 10.1111/j.1746-1561.2009.00485.x. [DOI] [PubMed] [Google Scholar]
- 45.Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and Disordered Eating Behaviors from Adolescence to Young Adulthood: Findings from a 10-Year Longitudinal Study. J Am Diet Assoc. 2011;111:1004–1011. doi: 10.1016/j.jada.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Swenne I, Thurfjell B. Clinical onset and diagnosis of eating disorders in premenarcheal girls is preceded by inadequate weight gain and growth retardation. Acta Paediatrica. 2003;92:1133–1137. doi: 10.1080/08035250310005224. [DOI] [PubMed] [Google Scholar]
- 47.Health UDo, Services H. National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2004. The health consequences of smoking: a report of the Surgeon General; p. 62. [Google Scholar]
- 48.Shunk JA, Birch LL. Validity of dietary restraint among 5-to 9-year old girls. Appetite. 2004;42:241–247. doi: 10.1016/j.appet.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 49.Lowe MR, Foster GD, Kerzhnerman I, Swain RM, Wadden TA. Restrictive dieting vs. "undieting" - Effects on eating regulation in obese clinic attenders. Addict Behav. 2001;26:253–266. doi: 10.1016/s0306-4603(00)00106-4. [DOI] [PubMed] [Google Scholar]
- 50.Dhurandhar NV, Schoeller D, Brown AW, Heymsfield SB, Thomas D, Sorensen TIA, et al. Energy balance measurement: when something is not better than nothing. Int J Obes. 2014 [Google Scholar]