Abstract
Background
The quality and effectiveness of resuscitation processes may be influenced by patients' body mass index (BMI); however, the relationship between BMI and survival after in-hospital cardiac arrest has not been previously studied.
Methods and Results
We evaluated 21,237 adult patients with an in-hospital cardiac arrest within the National Registry for Cardiopulmonary Resuscitation (NRCPR). We examined the association between BMI (classified as underweight [<18.5 kg/m2], normal [18.5-24.9], overweight [25.0-29.9], obese [30.0-34.9], and very obese [≥35.0]) and survival to hospital discharge using multivariable logistic regression, after stratifying arrests by rhythm type and adjusting for patient characteristics. Of 4,499 patients with ventricular fibrillation or pulseless ventricular tachycardia as initial rhythm, 1,825 (40.6%) survived to discharge. After multivariable adjustment, compared with overweight patients, underweight (Odds Ratio [OR], 0.59 [95% CI: 0.41-0.84]; p=0.003), normal weight (OR, 0.75; [0.63-0.89]; p<.001), and very obese (OR, 0.78 [0.63-0.96]; p=0.02) had lower rates of survival, while obese patients had similar rates of survival (OR, 0.87; 95% CI, 0.72-1.06; p=0.17). In contrast, of 16,738 patients with arrests due to asystole or pulse less electrical activity, only 2,501 (14.9%) survived. After multivariable adjustment, all BMI groups had similar rates of survival except underweight patients (OR, 0.67 [0.54-0.82]; p<.001).
Conclusions
For cardiac arrests due to shockable rhythms, underweight, normal weight, and very obese patients had lower rates of survival to discharge. In contrast, for cardiac arrests due to non-shockable rhythms, survival to discharge was similar across BMI groups, except for underweight patients. Future studies are needed to clarify the extent to which BMI affects the quality and effectiveness of resuscitation measures.
Keywords: cardiopulmonary resuscitation, obesity, heart arrest, defibrillation
Introduction
While studies have linked body mass index (BMI) to worse outcomes for a wide variety of cardiovascular and non-cardiovascular conditions,1-7 the role of BMI in mediating outcomes for in-hospital cardiac arrest is unknown. In-hospital cardiac arrests are common and are associated with poor survival.8 If differences in survival exist because effective resuscitation is impaired in patients with high or low BMI, this would have important implications for the treatment of these critically ill patients.
There are several theoretical reasons why BMI could potentially affect the quality and effectiveness of resuscitation measures during an in-hospital cardiac arrest. There may be logistical delays in morbidly obese patients due to difficulties in placement of defibrillator pads, establishment of vascular access, or initiation of a viable airway. Physical and biological factors, related to a high or low BMI, could impact the quality of chest compressions, the efficacy of vasoactive drugs, or the safety of defibrillator shocks, as none of these measures are standardized to a patient's BMI or weight. Finally, it is possible that patients at each end of the BMI spectrum are treated less aggressively during the acute resuscitation. If patients with very high or low BMIs were found to have lower rates of survival after in-hospital cardiac arrests, this would prompt additional studies to determine whether this was due to hospital, patient, or physician factors.
In order to explore this gap in knowledge, we examined the association between BMI and survival for patients with in-hospital cardiac arrests within the National Registry of Cardiopulmonary Resuscitation (NRCPR). We explored differences in survival to discharge by BMI group and also examined if differences in acute resuscitation treatment (defibrillation response time, number of shocks, and resuscitation duration) varied by BMI group. The NRCPR, which is a large, multi-site quality improvement registry that prospectively collects data on consecutive in-hospital cardiac arrests,8 provides a unique resource for exploring this question.
Methods
Study Design
The design of the NRCPR has been previously described in detail.8 Briefly, the NRCPR is a large, multi-site, prospective registry of in-hospital cardiac arrest sponsored by the American Heart Association and prospectively collects data on cardiac arrests using standardized Utstein definitions.9 Specially trained research coordinators at participating hospitals abstract data on consecutive patients with an in-hospital cardiac arrest, defined as unresponsiveness, apnea, and the absence of pulse. Patients with prior Do-Not-Resuscitate orders and cardiopulmonary resuscitation events beginning outside of the hospital are excluded from registry enrollment.
In January of 2006, the NRCPR began collection of patient data on height and weight; we therefore limited our analyses to the 34,588 cardiac arrests in adult patients aged 18 years or older occurring within NRCPR from January 1, 2006 to December 31, 2007. Of these patients, 21,237 (61.4%) had available data on both height and weight from which calculations of BMI could be performed and formed the study cohort. Importantly, patients with and without information on BMI were similar in patient characteristics except that excluded patients were more likely to have a cardiac arrest in the emergency department (Appendix ). The University of Michigan Institutional Review Board granted approval for waiver of informed consent for this study.
BMI Categories
BMI was determined by the standard formula of weight (in kilograms) divided by the square of the height (in meters) and was classified using the World Health Organization (WHO) classification: underweight (<18.5 kg/m2), normal (18.5-24.9), overweight (25.0-29.9), obese (30.0-34.9), and very obese (≥35.0).10 Analyses were stratified by whether the first identifiable rhythm in a patient was shockable (pulseless ventricular tachycardia [VT] and ventricular fibrillation [VF]) or non-shockable (asystole and pulseless electrical activity [PEA] rhythm).
Study Outcomes
The primary outcome in this study was survival to hospital discharge. In order to better understand observed differences in survival to discharge, the two phases of overall survival—return of spontaneous circulation for at least 20 minutes (ROSC) and post-resuscitation survival (i.e., survival among patients with ROSC)—were evaluated as secondary outcomes. In addition, we evaluated whether defibrillation response times and resuscitation intensity (total number of defibrillations and total duration of resuscitation event) differed across BMI groups. Based on prior work,11 defibrillation response time was examined as delayed (> 2 minutes) versus not delayed (≤2 minutes).
Statistical Analysis
Baseline differences in patient characteristics across BMI groups were assessed using analysis of variance and the Kruskal-Wallis test for continuous variables, as appropriate, and chi-square (X2) tests for categorical variables. Given known differences in resuscitation measures and survival by cardiac arrest rhythm,8 we determined a priori to examine the association of BMI with survival outcomes separately among patients who presented with a shockable (VT or VF) or non-shockable (asystole and PEA) rhythm. Therefore, separate multivariable models were constructed to evaluate the independent relationship between BMI and survival outcomes for the 2 different rhythm types.
All models used the generalized estimating equations (GEE) method with an exchangeable correlation matrix to account for the potential effects of clustering of patients within hospitals. The primary models examined the relationship of BMI with survival to hospital discharge. Models adjusted for each of the following variables: age, sex, race, BMI category, initial cardiac arrest rhythm (VF vs. VT or PEA vs. asystole), cardiac arrest location (intensive care unit [ICU], telemetry unit, or nonmonitored unit), and time of cardiac arrest (work hours: 8am to 5pm, after hours: 5pm to 8am or weekend) as covariates, regardless of significance level. Additional candidate variables were selected from the following list after determining a significant univariate association (p<0.10) with survival: 1) clinical co-morbidities or conditions present prior to cardiac arrest (history of myocardial infarction, congestive heart failure, diabetes mellitus; renal, respiratory, hepatic insufficiency; metastatic or hematologic malignancy; baseline evidence of motor, cognitive, functional deficits; stroke; sepsis; hypotension; pneumonia; major trauma; requirement for hemodialysis), 2) myocardial infarction or congestive heart failure during the index admission, 3) an admitting cardiac diagnosis, 4) use of invasive therapy (mechanical ventilation, intra-aortic balloon pump, or pulmonary artery catheter) or continuous intravenous vasoactive medications (dopamine, dobutamine, norepinephrine, and phenylephrine) at the time of arrest, and 5) use of a hospital-wide cardiopulmonary arrest alert or the presence of an organized hospital code team during the resuscitation. In addition, models for VF/VT arrests included rates of delayed defibrillation time as a covariate due to its ability to influence outcomes11. In each model, we assigned the overweight patient group as the referent, based on results in other studies.12-17
We also constructed multivariable models to evaluate whether there were differences by BMI group for the secondary outcomes of ROSC and post-resuscitation survival. Finally, we examined whether there were differences in acute resuscitation treatment (defibrillation response time, number of shocks, and resuscitation duration) by BMI group. For all analyses, the null hypothesis was evaluated at a two-sided significance level of 0.05 with 95% confidence intervals (CI) calculated. Analyses were performed with SAS 9.2 (SAS Institute, Cary, NC).
Results
We identified 21,237 cardiac arrest cases at 328 hospitals. The mean age for the study population was 66.0 ± 15.6 years, of which 12,409 (58.4%) were male and 13,690 (64.5%) were non-Hispanic white. Nearly four in five patients presented with a non-shockable cardiac arrest rhythm and half the cohort was in an ICU at the time of cardiac arrest. Most patients had either normal BMI (6,935 patients; 32.7%) or were overweight (5,919 patients; 27.9%); however, 1,437 patients (6.8%) were classified as underweight, 3,412 (16.1%) were obese, and 3,534 (16.6%) were very obese.
Baseline differences in patient characteristics across the five categories of BMI are displayed in Table 1. In general, most factors were similar across the BMI groups. However, patients who were very obese were younger; more likely to have had congestive heart failure in the past or during the index admission; and more likely to have renal insufficiency and to be on mechanical ventilation at the time of cardiac arrest. Patients who were underweight were less likely to be of non-Hispanic white race; less likely to have had myocardial infarction in the past or during the index admission; more likely to have asystole as their first identified rhythm; more likely to have a pre-existing metastatic or hematologic malignancy, pneumonia, or sepsis during the index admission; and more likely to be unmonitored at the time of cardiac arrest.
Table 1. Baseline Characteristics of Study Sample by Body Mass Index Group.
[CHF, congestive heart failure; CNS, central nervous system; MI, myocardial infarction]
| PATIENT CHARACTERISTICS | Body Mass Index (Kg/m2) | P value | ||||
|---|---|---|---|---|---|---|
| Underweight | Normal | Overweight | Obese | Very Obese | ||
| < 18.5 (n=1,437) |
18.5 to 24.9 (n=6,935) |
25.0 to 29.9 (n=5,919) |
30.0 to 34.9 (n=3,412) |
≥ 35.0 (n=3,534) |
||
| ARREST RHYTHM | <.001 | |||||
| Asystole, no. (%) | 571 (39.7) | 2,595 (37.4) | 2,059 (34.8) | 1,178 (34.5) | 1,296 (36.7) | |
| Pulseless Electrical Activity, no. (%) | 645 (44.9) | 2,971 (42.8) | 2,532 (42.8) | 1,417 (41.5) | 1,474 (41.7) | |
| Ventricular fibrillation, no. (%) | 116 (8.1) | 800 (11.5) | 800 (13.5) | 486 (14.2) | 468 (13.2) | |
| Pulseless Ventricular Tachycardia, no. (%) | 105 (7.3) | 569 (8.2) | 528 (8.9) | 331 (9.7) | 296 (8.4) | |
| Age, years ± SD | 67.4 ± 16.7 | 68.6 ± 16.2 | 66.9 ± 15.2 | 64.9 ± 14.4 | 60.2 ± 14.2 | <.001 |
| Male sex, no. (%) | 739 (51.4) | 4,133 (59.6) | 3,729 (63.0) | 2,005 (58.8) | 1,803 (51.0) | <.001 |
| Race | <.001 | |||||
| White, non-Hispanic, no. (%) | 833 (58.0) | 4,448 (64.1) | 3,875 (65.5) | 2,298 (67.4) | 2,236 (63.3) | |
| Black, non-Hispanic, no. (%) | 393 (27.3) | 1,473 (21.2) | 1,172 (19.8) | 672 (19.7) | 847 (24.0) | |
| Hispanic, no. (%) | 77 (5.4) | 408 (5.9) | 393 (6.6) | 193 (5.7) | 198 (5.6) | |
| Other, no. (%) | 134 (9.3) | 606 (8.7) | 479 (8.1) | 249 (7.3) | 253 (7.2) | |
| HOSPITAL ARREST LOCATION | <.001 | |||||
| Intensive care unit, no. (%) | 644 (44.8) | 3,444 (49.7) | 2,992 (50.6) | 1,764 (51.7) | 1,832 (51.8) | |
| Telemetry unit, no. (%) | 252 (17.5) | 1,227 (17.7) | 1,008 (17.0) | 548 (16.1) | 556 (15.7) | |
| Nonmonitored unit, no. (%) | 387 (26.9) | 1,369 (19.7) | 998 (16.9) | 585 (17.2) | 621 (17.6) | |
| Procedure Suites, no. (%) | 63 (4.4) | 403 (5.8) | 438 (7.4) | 249 (7.3) | 227 (6.4) | |
| Emergency Room, no. (%) | 70 (4.9) | 414 (6.0) | 399 (1.4) | 223 (6.5) | 240 (6.8) | |
| Other, no. (%) | 21 (1.5) | 78 (1.1) | 84 (1.4) | 43 (1.3) | 58 (1.6) | |
| ARREST CHARACTERISTICS | ||||||
| Hospital-wide code blue, no. (%) | 1,213 (84.4) | 5,615 (81.0) | 4,732 (80.0) | 2,686 (78.7) | 2,773 (78.5) | <.001 |
| Time of day or week for cardiac arrest | ||||||
| Weeknight (5pm to 8am), no. (%) | 914 (63.6) | 4,290 (61.9) | 3,603 (60.9) | 2,083 (61.1) | 2,156 (61.0) | 0.32 |
| Weekend, no. (%) | 411 (28.6) | 1,874 (27.0) | 1,566 (26.5) | 883 (25.9) | 931 (26.3) | 0.33 |
| Afterhours (Nights or Weekends), no. (%) | 1,058 (73.6) | 4,986 (71.9) | 4,179 (70.6) | 2,443 (71.6) | 2,517 (71.2) | 0.18 |
| Cardiac Admitting Diagnosis, no. (%) | 1,027 (71.5) | 4,317 (62.3) | 3,361 (56.8) | 1,927 (56.5) | 2,094 (59.3) | <.001 |
| PRE-ARREST CHARACTERISTICS | ||||||
| CHF during admission, no. (%) | 209 (14.5) | 1,179 (17.0) | 1,064 (18.0) | 577 (16.9) | 734 (20.8) | <.001 |
| Prior CHF before admission, no. (%) | 216 (15.0) | 1,218 (17.6) | 5,919 (18.1) | 3,412 (18.9) | 782 (22.1) | <.001 |
| MI during admission, no. (%) | 157 (10.9) | 1,031 (14.9) | 1,088 (18.4) | 603 (17.7) | 541 (15.3) | <.001 |
| Prior MI before admission, no. (%) | 162 (11.3) | 997 (14.4) | 917 (15.5) | 546 (16.0) | 516 (14.6) | <.001 |
| Hypotension, no. (%) | 375 (26.1) | 1,809 (26.1) | 1,573 (28.2) | 934 (27.4) | 897 (25.4) | 0.41 |
| Metastatic or Hematologic Malignancy, no. (%) | 223 (15.5) | 951 (13.7) | 685 (11.6) | 375 (11.0) | 286 (8.1) | <.001 |
| Respiratory insufficiency, no. (%) | 606 (42.2) | 2,640 (38.1) | 2,239 (37.8) | 1,323 (38.9) | 1,502 (42.5) | <.001 |
| Renal insufficiency, no. (%) | 401 (27.9) | 2,089 (30.1) | 1,886 (31.9) | 1,088 (31.9) | 1,224 (34.6) | <.001 |
| Renal failure requiring hemodialysis, no. (%) | 50 (3.5) | 255 (3.7) | 239 (4.0) | 158 (4.6) | 152 (4.3) | 0.12 |
| Hepatic insufficiency, no. (%) | 89 (6.2) | 494 (7.1) | 400 (6.8) | 247 (7.2) | 256 (7.2) | 0.59 |
| Diabetes mellitus, no. (%) | 261 (18.2) | 1,509 (21.8) | 1,636 (26.8) | 1,181 (34.6) | 1,522 (43.1) | <.001 |
| Baseline CNS depression, no. (%) | 216 (15.0) | 966 (13.9) | 686 (11.6) | 382 (11.2) | 374 (10.6) | <.001 |
| Acute stroke, no. (%) | 53 (3.7) | 289 (4.2) | 244 (4.1) | 121 (3.6) | 98 (2.8) | 0.005 |
| Pneumonia, no. (%) | 258 (18.0) | 1,001 (14.4) | 687 (11.6) | 367 (10.8) | 380 (10.8) | <.001 |
| Sepsis, no. (%) | 268 (18.7) | 1,162 (16.8) | 877 (14.8) | 555 (16.3) | 592 (16.8) | 0.002 |
| Major trauma, no. (%) | 37 (2.6) | 207 (3.0) | 213 (3.6) | 104 (3.1) | 113 (3.2) | 0.19 |
| INTERVENTIONS AT TIME OF ARREST | ||||||
| Mechanical ventilation, no. (%) | 440 (30.6) | 2,205 (31.8) | 1,940 (32.8) | 3,412 (33.9) | 1,306 (37.0) | <.001 |
| Intra-aortic balloon pump, no. (%) | 4 (0.3) | 99 (1.4) | 120 (2.0) | 83 (2.4) | 52 (1.5) | <.001 |
| Pulmonary artery catheter, no. (%) | 26 (1.8) | 244 (3.5) | 237 (4.0) | 151 (4.4) | 126 (3.6) | <.001 |
| Intravenous Dopamine, no. (%) | 147 (10.2) | 848 (12.2) | 760 (12.8) | 441 (12.9) | 425 (12.0) | 0.07 |
| Intravenous Dobutamine, no. (%) | 24 (1.7) | 231 (3.3) | 213 (3.6) | 143 (4.2) | 151 (4.3) | <.001 |
| Intravenous Norephinephrine, no. (%) | 176 (12.3) | 922 (13.3) | 778 (13.1) | 479 (14.0) | 504 (14.3) | 0.25 |
| Intravenous Phenylephrine, no. (%) | 65 (4.5) | 343 (5.0) | 315 (5.3) | 176 (5.2) | 191 (5.4) | 0.63 |
Shockable Rhythms
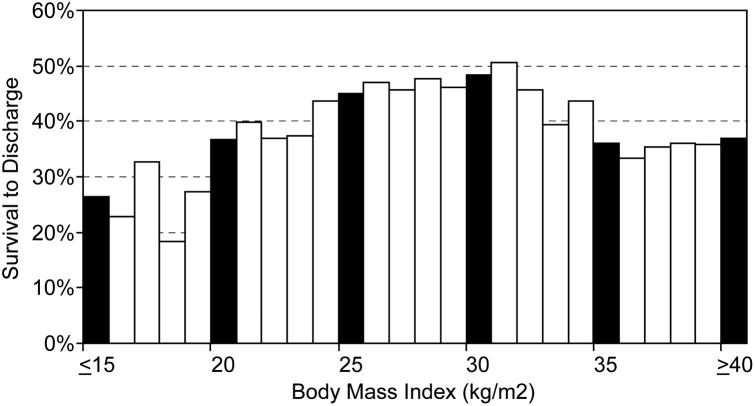
Of 4,499 patients with a pulse less arrest due to VF or VT, 1,825 (40.6%) patients survived to hospital discharge. The relationship between BMI and survival to discharge for VF and VT arrests is depicted in Figure 1. Differences were noted in overall crude rates of survival among the BMI groups, with the highest rate of survival to discharge in overweight patients (45.6% [605/1,328]) and lower survival rates in underweight (27.6% [61/221]), normal weight (36.5% [500/1,369]), obese (43.7% [357/817]), and very obese (39.5% [302/764]) patients. Moreover, while ROSC was achieved in 3,126 (69.4%) patients and 1,825 (58.4%) of these successfully resuscitated patients survived to discharge, a similar pattern of higher crude rates of ROSC and post-resuscitation survival was seen in overweight patients (Table 2).
Figure 1.
Relationship of BMI with Survival to Discharge for Cardiac Arrests due to Ventricular Fibrillation or Pulseless Ventricular Tachycardia.
Table 2. Summary of Survival Outcomes by Body Mass Index Group, Stratified by Cardiac Arrest Rhythm.
[PEA, pulseless electrical activity; ROSC, return of spontaneous circulation; VF, ventricular fibrillation; VT, ventricular tachycardia]
| Body Mass Index (kg/m2) | ||||||
|---|---|---|---|---|---|---|
| Underweight < | Normal | Overweight | Obese | Very Obese | ||
| 18.5 (n=221) |
18.5 to 24.9 (n=1,369) |
25.0 to 29.9 (n=1,328) |
30.0 to 34.9 (n=817) |
≥ 35.0 (n=764) |
P value | |
| VF AND PULSELESS VT | ||||||
|
| ||||||
| Survived to Discharge, no. (%) | 61 (27.6) | 500 (36.5) | 605 (45.6) | 357 (43.7) | 302 (39.5) | <.001 |
| ROSC, no. (%) | 131 (59.3) | 934 (68.2) | 975 (73.4) | 568 (69.5) | 518 (67.8) | <.001 |
| Post-Resuscitation Survival†, % | 46.6% | 53.5% | 62.1% | 62.9% | 58.3% | <.001 |
|
| ||||||
| (n=1,216) | (n=5,566) | (n=4,591) | (n=2,595) | (n=2,770) | p-value | |
|
| ||||||
| ASYSTOLE AND PEA | ||||||
|
| ||||||
| Survived to Discharge, no. (%) | 125 (10.3) | 769 (13.8) | 700 (15.3) | 436 (16.8) | 471 (17.0) | <.001 |
| ROSC, no. (%) | 604 (49.7) | 2,870 (51.6) | 2,348 (51.1) | 1,396 (53.8) | 1,484 (53.6) | 0.03 |
| Post-Resuscitation Survival†, % | 20.7% | 26.8% | 29.8% | 31.2% | 31.7% | <.001 |
Calculated as the number of patients surviving to discharge divided by the number achieving ROSC.
Despite differences in crude survival, rates of delayed defibrillation response times were similar across BMI groups (Table 3). However, among those who died during the initial resuscitation (i.e., no ROSC), there were differences in the total number of defibrillations administered and the total duration of the resuscitation event by BMI group. This was especially evident among underweight patients. In contrast, among those achieving ROSC, the duration of resuscitation was similar among the BMI groups.
Table 3. Defibrillation Performance and Duration of Resuscitation by Body Mass Index Group.
[PEA, pulseless electrical activity; ROSC, return of spontaneous circulation; VF, ventricular fibrillation; VT, ventricular tachycardia]
| Body Mass Index (kg/m2) | ||||||
|---|---|---|---|---|---|---|
| Underweight < 18.5 | Normal 18.5 to 24.9 | Overweight 25.0 to 29.9 | Obese 30.0 to 34.9 | Very Obese ≥ 35.0 | P value | |
| VF AND PULSELESS VT | ||||||
|
| ||||||
| Defibrillation Time >2 minutes, no. (%) | 36 (16.3) | 206 (15.1) | 182 (13.7) | 107 (13.1)) | 7 (15.5) | 0.41 |
| Shock Number | ||||||
| ROSC, median (IQR) | 1 (1,3) | 1 (1,3) | 2 (1, 3) | 2 (1, 3) | 2 (1, 3) | 0.10 |
| No ROSC, median (IQR) | 3 (2, 5) | 4 (2, 6) | 4 (2, 6) | 4 (2, 7) | 4 (3, 6) | 0.03 |
| Code Duration | ||||||
| ROSC, median (IQR) | 7 (4, 15) | 8 (3, 16) | 7 (3, 17) | 8 (3, 19) | 8 (3, 19) | 0.84 |
| No ROSC, median (IQR) | 19 (12, 30) | 23 (15, 33) | 25 (16, 34) | 23 (16, 35) | 27 (18, 38) | <.001 |
|
| ||||||
| ASYSTOLE AND PEA | ||||||
|
| ||||||
| Code Duration | ||||||
| ROSC, median (IQR) | 10 (6, 18) | 10 (5, 18) | 10 (5, 20) | 10 (5, 20) | 11 (6, 21) | 0.01 |
| No ROSC, median (IQR) | 18 (11, 26) | 20 (13, 30) | 22 (14, 32) | 23 (15, 33) | 24 (15, 34) | <.001 |
After adjustment for patient factors and rates of delayed defibrillation time, compared with overweight patients, underweight (adjusted odds ratio [OR], 0.59; 95% CI, 0.41-0.84; p=0.003), normal weight (adjusted OR, 0.75; 95% CI, 0.63-0.89; p<.001), and very obese patients (adjusted OR, 0.78; 95% CI, 0.63-0.96; p=0.02) were less likely to survive to hospital discharge, while overall survival was similar for obese patients (adjusted OR, 0.87; 95% CI, 0.72-1.06; p=0.17). These differences in overall survival by BMI group were attributable to both differences in ROSC and post-resuscitation survival (Table 4).
Table 4. Adjusted Estimates of the Association of BMI with Survival Outcomes in Patients with VF or VT Arrests*.
[BMI, body mass index; ROSC, return of spontaneous circulation; VF, ventricular fibrillation; VT, ventricular tachycardia]
| SURVIVAL TO DISCHARGE | ROSC | POST-ARREST SURVIVAL | ||||
|---|---|---|---|---|---|---|
| BMI (kg/m2) | Adjusted OR | p-value | Adjusted OR | p-value | Adjusted OR | p-value |
| <18.5 | 0.58 (0.41, 0.83) | 0.003 | 0.65 (0.48, 0.87) | 0.005 | 0.66 (0.43, 0.99) | 0.05 |
| 18.5 to 24.9 | 0.75 (0.63, 0.89) | <.001 | 0.84 (0.70, 1.00) | 0.05 | 0.80 (0.66, 0.99) | 0.04 |
| 25.0 to 29.9 | Reference | Reference | Reference | Reference | Reference | Reference |
| 30.0 to 34.9 | 0.87 (0.72, 1.06) | 0.17 | 0.80 (0.65, 0.98) | 0.03 | 0.98 (0.77, 1.25) | 0.88 |
| ≥ 35.0 | 0.78 (0.63, 0.96) | 0.02 | 0.80 (0.65, 0.99) | 0.04 | 0.90 (0.70, 1.16) | 0.42 |
Models included demographic characteristics, initial cardiac arrest rhythm (VF vs. VT or PEA vs. asystole), cardiac arrest location, and time of cardiac arrest, regardless of significance level. In addition, other variables with a univariate association (p<0.10) with each survival outcome were included in final models. These included pre-arrest characteristics (i.e., clinical comorbidities), arrest characteristics, and interventions in place prior to cardiac arrest, as outlined in Table 1.
Non-Shockable Rhythms
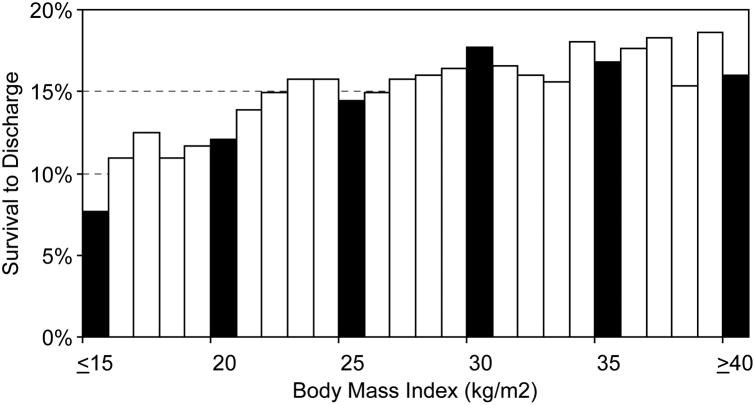
Of 16,738 patients with cardiac arrests due to asystole or PEA, 2,501 (14.9%) survived to hospital discharge. The relationship between BMI and survival to discharge for asystole and PEA arrests is depicted in Figure 2. Underweight patients had lower crude rates of survival to hospital discharge than the other BMI groups: underweight, 10.3% (125/1,216); normal weight, 13.8% (769/5,566); overweight, 15.3% (700/4591); obese, 16.8% (436/2,595); very obese, 17.0% (471/2,770) (p<.001 for differences across groups). While ROSC was achieved in 8,702 (52.0%) patients and 2,501 (28.7%) of these successfully resuscitated patients survived to discharge, a similar pattern of lower crude rates of ROSC and post-resuscitation survival was seen in underweight patients (Table 2). Finally, underweight patients were resuscitated for shorter periods, both among patients who survived with ROSC and those who died without ROSC during the initial resuscitation (Table 3).
Figure 2.
Relationship of BMI with Survival to Discharge for Cardiac Arrests due to Asystole and Pulseless Electrical Activity.
After adjustment for patient factors, compared with overweight patients, underweight patients (adjusted OR, 0.67; 95% CI, 0.54-0.82; p<.001) were less likely to survive to hospital discharge, while overall survival was similar for normal weight (adjusted OR, 0.94; 95% CI, 0.84-1.06; p=0.30), obese (adjusted OR, 1.08; 95% CI, 0.95-1.24; p=0.24) and very obese patients (adjusted OR, 0.97; 95% CI, 0.85-1.11; p=0.68). As there were no differences in adjusted rates of ROSC across the BMI groups, lower overall survival to hospital discharge in underweight patients was due to lower post-resuscitation survival (Table 5).
Table 5.
Adjusted Estimates of the Association of BMI with Survival Outcomes in Patients with Asystole and PEA Arrests.* [BMI, body mass index; PEA, pulseless electrical activity; ROSC, return of spontaneous circulation]
| SURVIVAL TO DISCHARGE | ROSC | POST-ARREST SURVIVAL | ||||
|---|---|---|---|---|---|---|
| BMI (kg/m2) | Adjusted OR | P value | Adjusted OR | P value | Adjusted OR | P value |
| <18.5 | 0.67 (0.54, 0.82) | <.001 | 0.95 (0.84, 1.08) | 0.46 | 0.63 (0.50, 0.78) | <.001 |
| 18.5 to 24.9 | 0.94 (0.84, 1.06) | 0.30 | 1.04 (0.96, 1.12) | 0.38 | 0.91 (0.80, 1.03) | 0.15 |
| 25.0 to 29.9 | Reference | Reference | Reference | Reference | Reference | Reference |
| 30.0 to 34.9 | 1.08 (0.95, 1.24) | 0.24 | 1.08 (0.98, 1.19) | 0.13 | 1.06 (0.91, 1.23) | 0.47 |
| ≥ 35.0 | 0.97 (0.85, 1.11) | 0.68 | 0.99 (0.90, 1.10) | 0.91 | 0.98 (0.84, 1.14) | 0.81 |
Models included demographic characteristics, initial cardiac arrest rhythm (VF vs. VT or PEA vs. asystole), cardiac arrest location, and time of cardiac arrest, regardless of significance level. In addition, other variables with a univariate association (p<0.10) with each survival outcome were included in final models. These included pre-arrest characteristics (i.e., clinical comorbidities), arrest characteristics, and interventions in place prior to cardiac arrest, as outlined in Table 1.
Discussion
We found that survival outcomes after in-hospital cardiac arrest differed by BMI. For cardiac arrests due to VF or VT, patients who were underweight, normal weight, and very obese had lower survival. Lower overall survival in these BMI groups was due to lower rates of both ROSC and post-resuscitation survival. While there were no differences in defibrillation response times by BMI group, underweight patients were treated for shorter durations prior to physician termination of resuscitation. In contrast, for cardiac arrests due to asystole and PEA, rates of survival to discharge were similar across BMI groups, except for underweight patients. The higher mortality seen in underweight patients was attributable to their overall lower post-resuscitation survival, as rates of acute resuscitation were similar. Collectively, these findings suggest that BMI is associated with differences in survival after in-hospital cardiac arrests and this relationship differs by cardiac arrest rhythm.
Although an inverse U- or J-shaped relationship between BMI and survival has been described in other disease states,4-6,18-21 the relationship between BMI and survival outcomes for in-hospital cardiac arrests has not previously been explored. While two small studies have evaluated the relationship between BMI and out-of-hospital cardiac arrests, these studies had limited power (combined sample size of fewer than 300 patients), were retrospective, involved single centers, and may not be generalizable to in-hospital cardiac arrests.22,23 In the NRCPR registry, we found that BMI was independently associated with survival, despite adjustment for a number of important patient factors. Given the large sample size and detailed data collection in this multi-site registry, we were able to: (1) examine the relationship of BMI separately for cardiac arrests that were shockable and non-shockable, (2) determine whether observed differences in overall survival were attributable to differences in ROSC or post-resuscitation survival, and (3) evaluate whether observed differences were associated with several key predictors of survival, such as delays in defibrillation time and duration of resuscitation.
The association of very low BMI and survival for shockable and non-shockable cardiac arrests may reflect residual confounding. While we were able to adjust for whether patients had a significant malignancy (hematologic or metastatic) and hepatic insufficiency, we did not have sufficiently detailed information on these two variables to adjust for specific types of malignancies, the extent of their metastases, malnutrition, and end-stage liver disease—all of which may be more prevalent in underweight patients and are linked to lower in-hospital survival. However, we did find that, among patients who did not survive the initial resuscitation (i.e., no ROSC), underweight patients were treated for 4 to 5 minutes shorter in both types of cardiac arrests. Moreover, underweight patients received fewer defibrillation shocks than patients in other BMI groups. Yet, it is unclear whether longer periods of resuscitation beyond the median of 19 minutes or additional defibrillation attempts beyond the median of 3 shocks in underweight patients would have meaningfully improved survival. Notably, among patients surviving the initial resuscitation, the period of time without spontaneous circulation was similar across BMI groups for patients with VF or VT arrests and shorter for underweight patients with asystole or PEA arrests. This suggests that longer times without spontaneous circulation before achieving ROSC were not responsible for the lower rates of post-resuscitation survival in underweight patients for both types of cardiac arrests.
Nonetheless, the association of underweight patients and poor survival after in-hospital cardiac arrest may have important clinical implications Malnutrition or poor functional status may explain lower survival from cardiac arrest in underweight patients. Moreover, the overall frailty of patients with low BMI, compared to other BMI categories, may account for their lower survival after cardiac arrest. These unmeasured aspects of patients' health status in our study may explain a physician's propensity to conduct a shorter resuscitation or administer fewer defibrillations in underweight patients. Alternatively, our findings may reflect a pattern of under treatment of underweight patients with cardiac arrest. This association deserves further study in cardiac arrest registries which are able to capture clinical information particular to patients with low BMI.
In contrast, there was an association between very high BMI and lower survival for VT and VF arrests, but not for asystole and PEA arrests. Because a key difference in the treatment of VT and VF arrests is the use of defibrillation, this survival finding raises several important implications. First, it suggests that the current use of fixed dose defibrillation therapy (200J, 300J, or 360J) in adult patients with VT or VF arrests may be inadequate in patients with very high BMI. In a prior study, higher thoracic impedance was associated with decreased defibrillation success,24 and BMI has previously been shown to correlate with thoracic impedance.25 While these studies are preliminary, they raise questions about whether defibrillation therapy in Advanced Cardiac Life Support protocols should be standardized to a patient's BMI. Indeed, we found in this study a trend for a higher number of required defibrillations to achieve ROSC among overweight, obese, and very obese patients with a VF or VT arrest. Given that defibrillation energy protocols for children within Pediatric Acute Life Support (PALS) are weight-based, additional animal and human studies on the optimal defibrillation energy by BMI may be warranted.
There may be other reasons why a very high BMI may be associated with worse survival outcomes after cardiac arrest. Longer times to intubation and delays in the administration of vasoactive medications in morbidly obese patients may affect the quality of resuscitation measures. Compression depth may also vary by patient BMI, which would affect the delivery of effective cardiopulmonary support during resuscitation. Preliminary studies of compression depth and the duration of interrupted cardiopulmonary resuscitation, however, do not seem to suggest that these are of lower quality in very obese patients.26 Moreover, these logistical and resuscitation issues, while plausible, would not account for the differential association of very high BMI and survival for shockable and non-shockable cardiac arrests.
Limitations
Our findings should be interpreted in the context of the following limitations. First, data on height and weight were not collected within the NRCPR until 2006, so our study includes cardiac arrests from 2006. Moreover, 38% of patients did not have assessments of height and weight and were excluded. However, patients with missing data on height and weight were not found to be meaningfully different in patient characteristics than patients included in this cohort. Second, while the NRCPR registry is the largest, prospective registry of in-hospital cardiac arrests with detailed information on many patient factors, we did not have complete information on several resuscitation factors to more fully account for the relationship between BMI and survival, such as cardiopulmonary compression quality (depth and frequency of compressions, proportion of interrupted resuscitation time), defibrillation and medication doses, and times to repeat defibrillation, vasoactive medications, and intubation. Similarly, we did not have assessments of patients' nutritional and functional status or the severity of pre-existing comorbidities to further account for the relationship between low BMI and survival. Third, our sample was drawn from a minority of U.S. hospitals (∼15% of large U.S. hospitals) that participated in a quality improvement resuscitation registry. However, we have no reason to believe that hospital participation within NRCPR would affect the relationship of BMI and survival. Finally, while we have observed a relationship between BMI and survival, this relationship should not be interpreted as causal.
Conclusion
In this large national registry of in-hospital cardiac arrests, we found that survival to discharge varied substantially by BMI. For cardiac arrests due to VT or VF, underweight, normal weight, and very obese patients had lower overall survival, despite adjustment for a number of patient factors and defibrillation response time. For asystole and PEA arrests, underweight patients had lower overall survival. Future studies are needed to determine whether the relationship between low BMI and survival is due to unmeasured differences in patient severity of illness and co-morbidity and the impact of very high BMI on defibrillation effectiveness and resuscitation quality.
Supplementary Material
What is Known
In hospital cardiac arrests are common and are associated with low rates of survival.
What this Article Adds
For in-hospital cardiac arrests, rates of survival to hospital discharge are influenced by a patient's body mass index.
For cardiac arrests due to shockable rhythms (ventricular fibrillation and pulseless ventricular tachycardia), overweight patients had the highest survival, with significantly lower rates of survival in patients who were underweight, normal weight, or very obese.
In cardiac arrests due to non-shockable rhythms (asystole and pulseless electrical activity), underweight patients had the lowest survival rate.
Acknowledgments
Funding Sources: The American Heart Association provides operational funding for the NRCPR, and the final manuscript draft was approved by the American Heart Association's Scientific Committee. Dr. Chan is supported by a Career Development Grant Award (K23HL102224) from the National Heart, Lung, And Blood Institute.
Footnotes
Conflict of Interest Disclosures: Drs. Jain, Nallamothu, and Chan report no potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Alpert MA, Lambert CR, Panayiotou H, Terry BE, Cohen MV, Massey CV, Hashimi MW, Mukerji V. Relation of duration of morbid obesity to left ventricular mass, systolic function, and diastolic filling, and effect of weight loss. Am J Cardiol. 1995;76:1194–1197. doi: 10.1016/s0002-9149(99)80338-5. [DOI] [PubMed] [Google Scholar]
- 2.Kenchaiah S, Evans JC, Levy D, Wilson PWF, Benjamin EJ, Larson MG, Kannel WB, Ramachandran SV. Obesity and the risk of heart failure. New Engl J Med. 2002;347:305–313. doi: 10.1056/NEJMoa020245. [DOI] [PubMed] [Google Scholar]
- 3.Hubert HB, Feinlab M, McNamara OM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67:968–977. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 4.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW. Body-mass index and mortality in a prospective cohort of U.S. adults. New Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 5.Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, Hollenbeck A, Leitzmann MF. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. New Engl J Med. 2006;355:764–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 6.Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, Mookadam F, Lopez-Jimenez F. Association of body weight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;268:666–678. doi: 10.1016/S0140-6736(06)69251-9. [DOI] [PubMed] [Google Scholar]
- 7.Gruberg L, Mercado N, Milo S, Boersma E, Disco C, van Es GA, Lemos PA, Ven Tzvi M, Wijns W, Unger F, Beyar R, Serruys PS Arterial Revascularization Therapies Study Investigators. Impact of body mass index on the outcome of patients with multivessel disease randomized to either coronary artery bypass grafting or stenting in the ARTS trial: the obesity paradox II? Am J of Card. 2005;95:439–444. doi: 10.1016/j.amjcard.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, Lane-Truitt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14270 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 9.Cummins RO, Chamberlin D, Hazinski MF, Nadkarni V, Kloeck W, Kramer E, Becker L, Robertson C, Koster R, Zaritsky A, Bossaert L, Ornato JP, Callanan V, Allen M, Steen P, Connolly B, Sanders A, Idris A, Cobbe S. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein’ style. Circulation. 1997;95:2213–2239. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Report of a WHO consultation on Obesity. Geneva: World Health Organization; Jun 3-5, 1997. Obesity: Preventing and Managing the Global Epidemic. WHO Technical Series No. 894. 2000. [PubMed] [Google Scholar]
- 11.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 12.Jin R, Grunkemeier GL, Furnary AP, Handy JR Providence Health System Cardiovascular Study Group. Is Obesity a Risk Factor for Mortality in Coronary Artery Bypass Surgery? Circulation. 2005;111:3359–3365. doi: 10.1161/CIRCULATIONAHA.104.489880. [DOI] [PubMed] [Google Scholar]
- 13.Zeller M, Steg PG, Ravisy J, Lorgi L, Laurent Y, Sicard P, Janin-Manificat L, Beer J, Makki H, Lagrost A, Rochette L, Cottin Y RICO Survey Working Group. Relation between body mass index, waist circumference, and death after acute myocardial infarction. Circulation. 2008;118:482–90. doi: 10.1161/CIRCULATIONAHA.107.753483. [DOI] [PubMed] [Google Scholar]
- 14.Abdullah J, Kober L, Abildstrom SZ, Christensen E, James WPT, Torp-Pedersen C. Impact of obesity as a mortality predictor in high-risk patients with myocardial infarction or chronic heart failure: a pooled analysis of five registries. Eur Heart J. 2008;29:594–601. doi: 10.1093/eurheartj/ehn010. [DOI] [PubMed] [Google Scholar]
- 15.Uretsy S, Messerli FH, Bangalore S, Champion A, Cooper-DeHoff RM, Zhou Q, Pepine CJ. Obesity paradox in patients with hypertension and coronary artery disease. Am J Med. 2007;120:863–70. doi: 10.1016/j.amjmed.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 16.Barba R, Bisbe J, Pedrajas JNA, Toril J, Monte R, Munoz-Torrero JFS, Monreal M the FRENA Investigators. Body mass index and outcome in patients with coronary, cerebrovascular, or peripheral artery disease: findings from the FRENA registry. Eur J Cardiovasc Prev Rehabil. 2009;16:457–63. doi: 10.1097/HJR.0b013e32832b1818. [DOI] [PubMed] [Google Scholar]
- 17.Lea JP, Crenshaw DO, Onufrak SJ, Newsome BB, McClellan WM. Obesity, end-stage renal disease, and survival in an elderly cohort with cardiovascular disease. Obesity. 2009;22:2216–22. doi: 10.1038/oby.2009.70. [DOI] [PubMed] [Google Scholar]
- 18.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths, associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–67. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 19.Oreopoulos A, Padwal RP, Kalantar-Sadeb K, Fonarow GC, Norris CM, McAlister FA. Body mass index and mortality in heart failure: a meta-analysis. Am Heart J. 2008;156:13–22. doi: 10.1016/j.ahj.2008.02.014. [DOI] [PubMed] [Google Scholar]
- 20.Ness AR, Gunnell D, Hughes J, Elwood PC, Davey Smith G, Burr ML. Height, body mass index, and survival in men with coronary artery disease: follow-up of the diet and reinfarction trial (DART) J Epidemiol Community Health. 2002;56:218–219. doi: 10.1136/jech.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Widlansky ME, Sesso HD, Rexrode KM, Manson JE, Gaziano JM. Body mass index and total and cardiovascular mortality in men with a history of cardiovascular disease. Arch Intern Med. 2004;164:2326–32. doi: 10.1001/archinte.164.21.2326. [DOI] [PubMed] [Google Scholar]
- 22.Bunch TJ, White RD, Lopez-Jimenez F, Thomas RJ. Association of body weight with total mortality and with ICD shocks among survivors of ventricular fibrillation out-of-hospital cardiac arrest. Resuscitation. 2008;77:351–5. doi: 10.1016/j.resuscitation.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 23.White RD, Blackwell TH, Russell JK, Jorgenson DB. Body weight does not affect defibrillation, resuscitation, or survival in patients with out-of-hospital cardiac arrest treated with a nonescalating biphasic waveform defibrillator. Crit Care Med. 2004;32:S387–S392. doi: 10.1097/01.ccm.0000139460.25406.78. [DOI] [PubMed] [Google Scholar]
- 24.Zelinka M, Buic D, Zelinka I. Comparison of five different defibrillators using recommended energy protocols. Resuscitation. 2007;74:500–7. doi: 10.1016/j.resuscitation.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 25.Fumagalli S, Boni N, Padeletti M, Gori F, Boncinelli L, Valoti P, Baldasseroni S, Di Bari M, Masotti G, Padeletti L, Barold S, Marchionni N. Determinants of thoracic electrical impedance in external electrical cardioversion of atrial fibrillation. Am J Cardiol. 2006;98:82–87. doi: 10.1016/j.amjcard.2006.01.065. [DOI] [PubMed] [Google Scholar]
- 26.Edelson DP, Abella BS, Kim S, VadenHoek TL, Becker LB. The effects of obesity on CPR quality and survival after cardiac arrest. Abstract to American Health Association Scientific Sessions 2006. Circulation. 2006;114:II_1199. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.