Abstract
Endoscopic stent placement is a common primary management therapy for benign and malignant biliary strictures. However, continuous use of stents is limited by occlusion and migration. Stent technology has evolved significantly over the past two decades to reduce these problems. The purpose of this article is to review current guidelines in managing malignant and benign biliary obstructions, current endoscopic techniques for stent placement, and emerging stent technology. What began as a simple plastic stent technology has evolved significantly to include uncovered, partially covered, and fully covered self-expanding metal stents (SEMS) as well as magnetic, bioabsorbable, drug-eluting, and antireflux stents.1
Keywords: Biliary obstruction, Stent, Hepatobiliary malignancy, Liver hilum
Introduction
Biliary obstruction can occur from both malignant and benign conditions, including pancreatic cancer, cholangiocarcinoma, metastatic disease, chronic pancreatitis, choledocolithaisis, and postoperative strictures.1 Benign biliary strictures are significant because they can cause jaundice, hepatocellular dysfunction, biliary cirrhosis, pain, pruritus, and cholangitis.3 Hepatobiliary malignancy causes obstruction in 70–90% of patients, causing similar complications.1–3 Prior to the use of stents, the primary treatment for biliary obstruction was surgery, such as cholecystojejunostomy or choledochojejunostomy.4 The endoscopic placement of biliary stents was first introduced in the early 1980s.4 There was a rapid shift from surgery towards endoscopic retrograde cholangiopancreatography (ERCP) stent placement because of its better mortality and morbidity profile.5 Palliation therapy with endoscopic stent placement can be beneficial for many patients with both distal and hilar malignant obstruction.1 In 1982, the first 10 French plastic stent was placed into a bile duct.6 In 1988, Speer et al. showed that 10F stents performed better than smaller 8F stents in malignant obstructions.7 In the late 1980s, self-expandable metal stents (SEMS) were adapted to the biliary tract to improve patency.8 These stents were also easier to place in the biliary tree, thereby increasing their popularity and use.2,4 Although plastic stents are used more frequently, especially for stone disease, SEMS have been evaluated in many other clinical situations, like benign biliary strictures, hilar obstructions, and bile leaks. In 2012, the European Society for Gastrointestinal Endoscopy (ESGE) published guidelines for clinical indications, and selection of stents (Table 1), and highlighted the strengths of individual stent types.9 The management of biliary obstruction with stenting is not always straight forward because of recent advancements in stent technology and the availability of multiple stent options.10 Here, we will review the indications for sphincterotomy before stent placement and the pros and cons of both plastic and metal stents in a variety of clinical settings. Furthermore, there are many subtypes of plastic and metal stents to choose from, including various plastic stent geometry, fully-covered SEMS (fcSEMS), partially-covered SEMS (pcSEMS), and uncovered SEMS (ucSEMS). Endoscopists need to determine the most appropriate stent suited for a variety of clinical situations, such as malignant hilar obstructions, non-malignant hilar obstructions, distal bile duct obstruction, benign biliary strictures, refractory choledocolithaisis, and biliary leaks. We will also discuss some novel stent designs, such as bioabsorbable, drug-eluting, anti-reflux, and magnetic stents, which are currently being assessed for efficacy and complications.1 With further testing and development of stents, the implementation of highly individualized therapy for both benign and malignant biliary obstructions may be possible in the near future.
Table 1. Clinical guidelines for biliary stent placement9 .
| Malignant disease | Benign disease | |||
|---|---|---|---|---|
| Sphincterotomy is not necessary for inserting a single plastic stent or a SEMS, but may facilitate more complex procedures. | Sphincterotomy is not necessary for inserting a single plastic stent or a SEMS, but may facilitate more complex procedures | |||
| Malignant hilar obstruction | Malignant non-hilar biliary obstruction | Benign biliary stricture | Biliary leak | Refractory choledocolithiasis |
| 1. CT or MRI to assess resectability of malignancy 2. Endoscopic drainage is first line therapy 3. Unilateral drainage is associated with higher mortality compared with bilateral drainage 4. Drainage >50% of the liver volume is associated with longer survival 5. If there is no definitive management decision, plastic stenting is indicated |
1. Life expectancy <4 months=plastic stents (10F Polyethyelene) 2. Life expectancy >4 months=SEMS (covered=uncovered) 3. If there is no definitive management decision, plastic stenting is indicated 4. SEMS should be considered in patients undergoing other therapies 5. Preoperative drainage of resectable hilar biliary obstruction is indicated, in acute cholangitis, or in severe pruritus with a delay in surgery |
1. Multiple plastic stents may provide longer biliary patency rates. 2. Polyethylene stents decompress better than Teflon-made stents 3. Avoid uncovered biliary SEMS 4. Covered and partially covered SEMS use still unclear |
1. ERCP should be used to locate leak 2. If no lesion can be identified, plastic biliary stent placement without sphincetrotomy is recommended 3. Remove stent within 4 to 8 weeks. At time of stent removal, cholangiography and duct cleansing should be done. |
1. If stones are irretrievable after ERCP with lithotripsy, or balloon dilatation, plastic stents are effective to drain bile ducts long term 2. Ursodeoxycholic acid or terpene can be considered for stone dissolution |
SEMS, self-expanding metal stents; CT, computed tomography; MRI, magnetic resonance imaging; ERCP, esophageal retrograde cholangiopancreatography.
Plastic and metal stents overview
Plastic stents
Plastic biliary stents are made up of polyethylene (PE), polyurethane (PU), or Teflon.11 Compared with PE stents, Teflon stents have briefer patency times but similar morbidity and mortality at 30 days.12 Cheon et al. performed a randomized trial comparing PU with PE stents in hilar biliary obstruction.13 PU stents are made with Pellethane, a soft pliable material that may adapt better to the curved bile duct for enhanced positioning and prevent distal or proximal migration.13 Results showed that migration was significantly lower with PU stents than PE stents (5% versus 29%, p=0.032).13 There was, however, no difference in median stent patency between PE and PU stents.13 Glandi et al. evaluated if systemic medical therapy could help decrease stent occlusion, and he found that ursodiol and antibiotics were ineffective in decreasing stent occlusion.14 Currently, most major manufactures use PE stents.
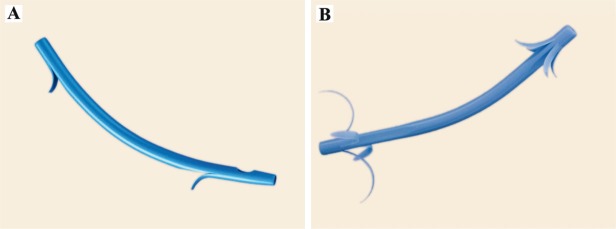
Plastic stent diameter ranges from 5F to 12F, and the length ranges from 1 to 18 cm.15 10F plastic stents need a 3.7 mm accessory channel while 11.5F stents need a 4.2 mm endoscope channel.15 Patency time is increased with stents 10F caliber and longer, but stent diameters of 11.5F or 12F have not been shown to be superior over 10F.16 There are a variety of shapes that can help facilitate anchoring, removal, and flow (Fig. 1).15 Pigtail plastic stents are coiled at one or both ends to allow for easier retrievability and more stable anchoring.15 These stents have side drainage holes. Flanged stents can be straight, angled, or curved, and they can have single or multiple flaps with side holes located both proximally and distally.15
Fig. 1. Plastic stents (Granted permission for use).
Metal stents
One limitation of plastic stents is the inability to achieve a large diameter. Larger diameter stents maintain longer patency, and self-expanding metal stents were designed for this purpose (Fig. 2).15,17 They are composed of metal alloys, such as platinol (platinum core with nitinol encasement), nitinol (combination of nickel and titanium), or stainless steel.15,18 Although nitinol is the metal of choice because of its ability to conform to the curved lumen, no one material has shown superiority.18,19 Metal stents are cylindrical in shape and have interwoven alloy wires to create enough radial force around the duct stricture to prevent collapsibility.18 The length of available SEMS range from 4 to 12 cm, and fully expanded diameters reach 6 to 10 mm.15 SEMS typically have 8.5F or less delivery systems to allow for use with most endoscopes.15 Biliary SEMS are released from preloaded through-the-scope delivery systems having diameters of 6 to 8.5F.4 The stent is deployed by removal of an outer sheath. The use of longer SEMS could increase wall pressure and damage the bile duct.4 After deployment, the stent is held in place by embedding into the tissue with expanding radial pressure.4
Fig. 2. Uncovered SEMS versus covered SEMS (Granted permission for use).
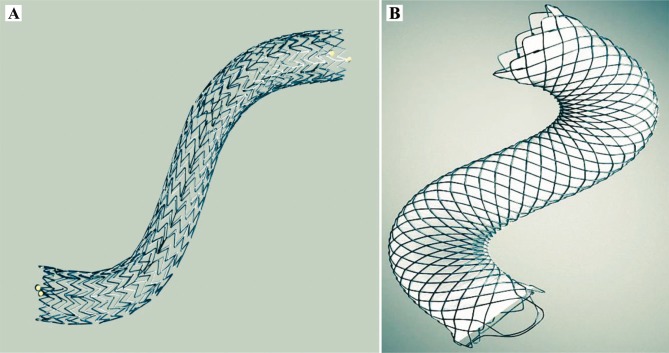
SEMS, self-expanding metal stents.
SEMS can be fully-covered, partially-covered, or uncovered. Uncovered metal stents help prevent migration, but they occlude earlier and cannot be removed due to ingrowth or overgrowth of mucosal tissue.15 However, they can be placed anywhere in the biliary tract, and they are the most commonly used metal stent. Covered SEMS (cSEMS) were introduced to decrease occlusion, but their complication is migration.15 Covering material can be made up of polytetrafluoroethylene, fluorinated ethylene propylene, or silicone membranes, all of which are effective.15 Kahaleh et al. examined 80 patients with a partially covered Wallstent for distal malignant biliary obstruction and found no stent failures from tumor ingrowth.20 In another study, Kahaleh et al. looked at 101 patients with malignant biliary strictures who received partially-covered Wallstents; only 3 cases of stent occlusion were reported at 12 months, and none were due to tumor ingrowth.21,22
SEMS can have straight ends, flanges, or anchoring flaps. Flanges were introduced to control migration, especially in covered stents.23 Park et al. compared the use of flared end versus anchoring flaps in fcSEMS in a multicenter, prospective study consisting of 43 patients with benign biliary strictures.23 After a median time of 6 months, no patients in the anchoring flaps group and six (30%) patients in the flared group had stent migration.23 Removal rate was 100% in both groups. Stricture improvement was similar in both groups.23 Very few studies are available that compare different brands of SEMS. Loew et al. compared occlusion rates in 241 patients with unresectable malignant biliary strictures receiving the 6 mm Zilver stent, 10 mm Zilver stent, or 10 mm uncovered Wallstent.24 He found that the 6 mm stent occluded more frequently than both 10 mm stents.24 Some covered metal stents have retrieval sutures attached to one or both ends to assist in extraction.15 These could potentially be helpful in biliary strictures after liver transplantation, as theses strictures are generally short and at the anastomosis.4 Hu et al. placed 13 fcSEMS with sutures for benign biliary strictures with the suture outside the papilla. Although one patient developed stent infection requiring early retrieval, the remaining patients kept the stent in place for 5.4 months without stent migration, and they were removed without complication. Stricture recurrence occurred in one patient. 22
Cost of metal versus plastic stents
In 2012, the average list price of frequently used metal stents was $1,333, while the average list price of frequently used plastic stents was $75.9 Despite the higher initial cost, the use of metal stents may reduce overall patient cost by decreasing use of medical resources like hospital stay, ERCP for stent exchanges, and treatment of cholangitis if the plastic stent occludes.25–27 When deciding between plastic and metal stents, it is important to take into account the prognosis of a given patient. If a patient is expected to outlive the patency of a plastic stent (>4 months), plastic stent replacement will be necessary.27 In this situation, the use of a metal stent may be more cost effective than having the patient undergo another procedure for plastic stent exchange.27 In the setting of uncertain life expectancy with malignant disease, our favorite strategy was highlighted by Yeoh et al. In his study, the placement of a plastic stent followed by a metal stent in long-term survivors was the most economical based on Medicare reimbursement rates in 1998.27 When performing a cost analysis, they found the most important variables affecting outcome were the cost of ERCP, followed by the cost of the metal stent, and then the probability of requiring stent exchange after the first plastic stent.27 They determined if the cost of the metal stent was less than half the cost of ERCP, then initial insertion of a metal stent would be more cost effective.27 A factor to consider when performing an ERCP is whether the diagnosis of malignant or benign biliary stricture is certain.27 If the diagnosis of malignancy is established, staging may not be complete and the patient might still be a surgical candidate where a plastic stent may be more appropriate.27 Lastly, the endoscopist may have not had the chance to discuss the advantages and disadvantages of plastic versus metal stents with the patient.27
Chen et al. advocated SEMS placement in all patients found to have pancreatic cancer. They found that it is cost-effective for the management of obstructive jaundice even when it is unknown whether they will have a pancreaticoduodenectomy.28 Distally placed SEMS do not interfere with the surgery.28 They concluded in patients undergoing ERCP before definitive cancer staging, short-length SEMS is the preferred cost-minimizing strategy.28 Data from Yoon et al. supported this conclusion. They evaluated 112 patients in Korea, where the cost of ERCP is less than those of metal stents. They concluded ERCP with metal biliary stents offers better palliation without a significant increase in cost in patients with unresectable malignant biliary obstruction ($1,488 in the metal stent group versus $1,318 in the plastic stent group p=0.422).29
Novel stents
Magnetic stents
Ryou et al. investigated in a porcine model a magnetic stent that can be retrieved by using an external hand-held magnet, thereby eliminating the need for second endoscopy for stent removal.30 This technology is especially useful in bile leak stenting post-cholecystectomy.30 The stent used was a modified 9.5 mm Geenen pancreatic stent with neodymium-iron-boron magnet extensions. In ex vivo testing, the captured distance was 10 cm. During in vivo testing, the magnetic stents were inserted and removed easily, with approximate retrieval times of 3.2 min and 33 sec, respectively.30 One concern of this novel stent system is its performance by an inexperienced user who may cause the stent to migrate proximally.30 This stent is currently being studied ex vivo, and clinical trials should not be expected soon.
Bioabsorbable stents
Bioabsorbable stents have been studied for their use in malignant and benign disease. Yamamoto et al. investigated a biodegradable 6 mm×15 mm poly-L-lactic acid Z pattern stent with platinum markers and placed them in 12 dogs.31 Cholangiography and laparotomy were performed at 1, 3, 6, and 9 months, and the stents remained patent throughout. Endothelial ingrowth into the wall was seen in nine of 12 dogs. No gross degradation was seen at 1, 3, or 6 months, but fragmentation had started at 9 months when the stents were removed.31 Haber et al. demonstrated safe deployment of a 10 mm×74 mm bioabsorbable poly-L-lactide stent in 48 of 50 patients with malignant biliary obstruction.32 Notably, radial compliance force was reduced by 60% in this stent relative to plastic stents. Outcomes of the study have not yet been published.32 More clinical studies using bioabsorbable stents need to be performed.
Drug-eluting stents
SEMS are often used for malignant biliary obstruction, but they are susceptible to occlusion from epithelial mesh overgrowth. Drug-eluting stents may improve stent patency.1 Paclitaxel, a chemotherapeutic agent that has been shown to inhibit cell proliferation in fibroblasts, pancreatic cancer, and epithelial cells in the gallbladder, has been studied for its effect on patency.33 Suk et al. investigated Niti-S Mira-Cover stents coated with paclitaxel. They inserted 21 stents in patients diagnosed with unresectable malignant biliary obstruction. Nine patients developed obstruction during the study. Four were caused by bile sludge, three had tumor overgrowth, and two had tumor ingrowth. Mean patency of drug-eluting stents were 429 days with 100% patency at 3 months, 71% patency at 5 months, and 36% patency at 12 months.34 Song et al. performed a prospective randomized pilot study comparing 24 patients with paclitaxel-eluting cSEMS and 25 patients with standard cSEMS. There was no difference in stent patency duration or survival time.35 To date, there are no randomized control trials (RCTs) comparing drug-eluting and covered metal stents. Based on the few studies available, drug-eluting stents seem to offer little, if any, benefit.
Anti-reflux stents
Stents with antireflux valves may lead to longer patency and decreased incidence of cholangitis.1 Dua et al. did a prospective randomized trial using the 10F antireflux plastic biliary stent (Tannenbaum type). Patency average was 145 days for the reflux stents and 101 days for control group plastic stents, and this difference was not statistically significant.36 Other studies have focused on metal antireflux stents. Hu et al. examined 23 patients with unresectable nonhilar malignant biliary obstruction and successfully placed antireflux metal stents in all patients.37 Stent failures occurred for a variety of reasons, including one patient with tumor ingrowth, two with tumor overgrowth, and three with stent migration. Median duration of stent patency was 425 days. At 3, 6, and 12 months, 95%, 74%, and 56% of stents, respectively, were patent.37 In 2012, Hu et al. performed another prospective randomized trial with 104 patients. Patency was 505 days in the antireflux stent group (n=52) and 301 days in the uncovered metal stent group (n=52), and the difference between the two groups was significant (p=0.031). Also, there were fewer episodes of fever in patients with antireflux stents, suggesting a reduction in cholangitis.38 Since decreasing occlusion and cholangitis episodes are two important primary outcomes, anti-reflux SEMS are worthy of further investigation.1
Sphincterotomy usage
Some endoscopists use sphincterotomy before stenting because stent placement may be easier for stent exchange during follow-up or if more than one stent will be placed.9 The loss of bile duct access is the endoscopist's biggest fear in ERCP, and many will perform a sphincterotomy to prevent this. However, several RCTs have shown that biliary sphincterotomy is not necessary when placing a single plastic or metal biliary stent.39–42 Giorgio et al. looked retrospectively at 172 patients with malignant common bile duct (CBD) obstruction and showed that sphincterotomy was not necessary for successful placement of 10F plastic stents. Half of the patients had sphincterotomy prior to the placement of stents while the other half did not. Stent insertion was successful in 96% of patients in the sphincterotomy group and 94% in the nonsphincterotomy group.40 Artifon et al. looked at sphincterotomy before SEMS in patients with malignant CBD obstruction from pancreatic cancer.39 He randomly assigned 74 patients to biliary stenting with or without sphincterotomy. cSEMS were placed in all patients. Their main outcomes included migration, occlusion, bleeding, and pancreatitis. While 48% of the patients with sphincterotomy experienced complications, only 10% of patients without sphincterotomy experienced complications.39 Banerjee et al. looked at 104 patients retrospectively that required biliary drainage for pancreaticobiliary malignancies and found that patients who underwent biliary sphincterotomy during transpapillary SEMS placement experienced more complications without increased duration in stent patency.42 Moss et al. performed a meta-analysis on 1,454 people and showed sphincterotomy-related complications in 24% of patients that underwent SEMS for obstructing pancreatic carcinoma. The most common complications were bleeding (13%) and perforation (11%).12 The above studies demonstrated that sphincterotomy has complications and provides no clear benefit to routine biliary stent placement. Sphincterotomy should be reserved to technically challenging ERCPs that need stent placement. The risks and benefits of a sphincterotomy in each case should be individually assessed.9
Management of malignant non-hilar biliary obstruction
Nonhilar biliary obstruction most often results from malignancies, including duodenal, pancreatic, and gallbladder cancers, distal cholangiocarcinoma, and metastatic disease.10 At least 66% percent of patients with distal malignant strictures are not candidates for curative resection because they cannot tolerate surgery or the lesion is unresectable or metastatic.2 Thus, palliative options for drainage include surgery or stents placed either percutaneously or endoscopically.10 The endoscopic method has become the preferred method for drainage by stent placement because of its less invasive nature and superior complication profile relative to the percutaneous route or surgery.10,43 Surgery does, however, offer more extensive palliative care options.
Plastic versus metal stents in non-hilar malignant biliary obstruction
Biliary stents are thought to provide symptomatic relief of jaundice, pruritus, and anorexia when used in malignant biliary obstruction. A meta-analysis of four RCTs showed no difference in initial insertion and early therapeutic success between SEMS and plastic stents in malignant biliary obstruction.11 Nevertheless, with SEMS, there was less stent occlusion by 4 months and decreased overall biliary obstruction relative to plastic stents.11 In general, SEMS have longer patency compared to plastic stents. In particular, they are a good choice for inoperable duodenal, biliary, and pancreatic cancer causing bile duct obstruction.44 In one meta-analysis, the average lengthened patency with SEMS was 60 days over plastic.45 In another meta-analysis of seven RCTs that included 724 patients with nonhilar malignant biliary obstruction, the risk of recurrent biliary obstruction at 4 months was decreased by 50% with SEMS compared to plastic stents.9,11 However, in patients with a prognosis of less than 4 months, plastic stents are a better choice because of lower cost and lower risk for migration and occlusion at the 3 month mark.46 A meta-analysis of five RCTs with a total of 498 patients showed no difference between plastic and SEMS at 30 days regarding jaundice, bilirubin, pruritus, and mortality.9 All these studies support the guidelines issued by ESGE in 2012 (Table 1) for nonresectable malignant biliary obstruction and show that plastic stents are a good option when patient prognosis is <4 months, while SEMS are a better option if the prognosis is >4 months.9
Covered SEMS versus uncovered SEMS
In malignancy, tumor overgrowth or ingrowth frequently causes the metal stent to obstruct.47 This led to the innovation and subsequent use of cSEMS. Isayama et al. studied cSEMS in 112 patients with nonhilar biliary malignancy. Their data showed that PU cSEMS have a longer patency than uncovered stents. Stent occlusion occurred in eight patients after 304 days in the covered group and in 21 patients after 166 days in the uncovered group.4,48 However, the cSEMS group had an increased frequency of stent migration.49 Telford et al. reconfirmed the migration issue when he compared uncovered and covered stents in malignant nonhilar obstructions. This study did not show any significant difference in mortality or recurrent biliary obstruction, but covered stents exhibited more frequent migration.50 In 400 patients in a RCT, there was no significant statistical difference in stent patency between uncovered and covered self-expandable nitinol stents in the treatment of malignant nonhilar biliary obstructions.47 Covered stents did migrate more often compared to uncovered stents, while tumor ingrowth was more frequent with uncovered stents.47 Current guidelines do not identify a benefit in cSEMS over ucSEMS in the treatment of nonhilar biliary obstructions, but further trials are being conducted to compare the two (Fig. 3).9 The precise utilization of the two types of SEMS is still an unresolved issue.
Fig. 3. Duodenal and biliary uSEMS placed for pancreatic cancer.
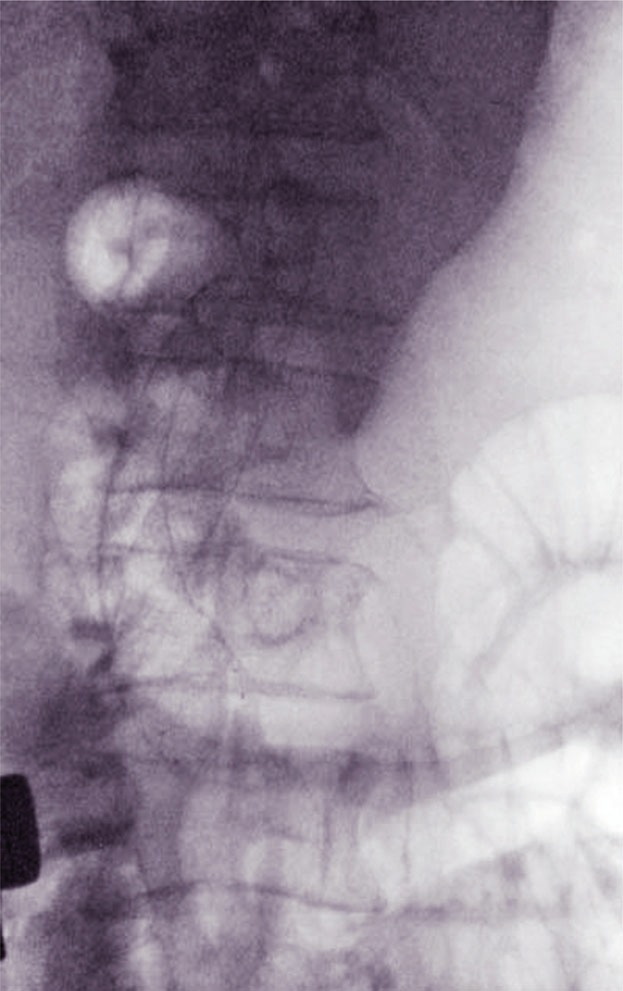
ucSEMS, uncovered self-expanding metal stents.
Management of malignant hilar biliary obstruction
The central location where the common bile duct, hepatic portal vein, and hepatic artery enter is called the hilum or porta hepatis. The duct, vein, and artery split into left and right branches to supply the right and left lobes of the liver. Approximately 55% of the liver is drained through the right hepatic duct, 35% through the left hepatic duct, and 10% through the caudate lobe.51 Cholangiocarcinoma, followed by gallbladder cancer, hepatocellular cancer, and metastatic hilar lymphadenopathy are the most common causes for hilar malignant obstructions.10 In patients with a malignant hilar CBD obstruction, preoperative biliary stent placement is an option. However, two RCTs showed an increase in overall morbidity compared with direct surgery.52,53 Lai et al. examined 87 patients assigned to either elective surgery (n=44) or endoscopic biliary drainage followed by exploration (n=43).52 Overall morbidity rate (18 patients versus 16 patients) and mortality rate (6 patients in each group) were similar in the two arms. Patients with hilar lesions had a higher incidence of cholangitis and failed drainage after stent placement.52 Van der Gaag et al. looked at preoperative biliary drainage versus surgery alone in 202 patients.53 Complications occurred in the surgery group at a rate of 39% (37 patients) and at a rate of 75% (75 patients) in the biliary drainage group (RR=0.54, 95% CI 0.41 to 0.71, p<0.001).53 Preoperative biliary drainage was successful in 94% of patients (96 patients). Mortality did not differ between the two groups.53
The benefit for preoperative drainage is uncertain in patients with malignant hilar obstruction, and more studies need to be performed. A meta-analysis of 11 studies showed no difference in death or length of stay without and with stent placement prior to any biliary surgery.54 Overall, a minority of patients with pancreatic cancer undergo resection, making SEMS with longer patency a reasonable choice.9,55,56 A multidisciplinary discussion should be made with a hepatobiliary surgeon on resectability of the tumor before any metal stent is placed, especially in hilar malignancy. Most patients with malignant hilar tumors are stenting candidates.57 Less than 20% of hilar tumors are resectable, and liver transplants are done in a very careful manner due to the known high risk of tumor reoccurrence.57
Plastic vs metal stenting
In 1993, Wagner et al. found a trend suggesting that SEMS have improved patency relative to plastic stents (although not significant). In addition, the SEMS group demonstrated decreased cholangitis and a significant decrease in reinterventions to manage stent-related problems (2.4% vs 0.4%, respectively).10,25 In a trial with 62 patients, it was shown that SEMS were statistically superior to plastic stents for hilar tumor palliation 30 days after stent placement with regard to multiple adverse outcomes, including occlusion, cholangitis, migration, and perforation.58 In another study, Raju et al. found SEMS (n=48) patency was statistically superior to that of plastic stents (n=52) with hilar cholangiocarcinoma. Median patency was 1.86 months in the plastic group and 5.56 months in the SEMS group.4,59 In a retrospective review of 52 SEMS in 35 patients by Cheng et al., five (14%) patients with SEMS had complications, including cholangitis or early stent closure when stenting unresectable hilar cholangiocarcinoma.4,60 Park et al. studied an unusual stent with similar results. He inserted a Bonastent M-Hilar SEMS with a cross wired nitinol mesh into 34 patients with unresectable malignant hilar biliary strictures of Bismuth type II or higher. Median survival was 180 days, and stent patency was 150 days. Success with placement of the newly designed metal stent was 94%.4,61 Taken together, these studies showed that SEMS are superior to plastic stents for palliation in patients with hilar malignancy.
Covered vs uncovered SEMS
The general consensus on cSEMS versus ucSEMS for malignant hilar obstruction is in favor of ucSEMS. cSEMS cover the small feeding intrahepatic biliary ducts and have migration issues and thereby have inferior outcomes in malignant hilar strictures. There is a lack of convincing data regarding this issue, mainly because the positive initial experiences with ucSEMS were so telling.
Unilateral vs bilateral stenting
The consensus for effective biliary drainage, whether unilateral or bilateral stenting is used, is to drain more than 50% of the liver volume.62 Vienne et al. proposed this after evaluating the effectiveness of any biliary drainage and found that successful drainage is a decrease in the bilirubin of more than 50% at 30 days, a standard that has been widely adopted.62 In theory, unilateral drainage may not completely reduce jaundice (especially in a cirrhotic liver) and may increase the incidence of cholangitis.10 Studies comparing the two methods are available, but the data are inconclusive. Naitoh et al. retrospectively reviewed 46 patients with malignant hilar biliary obstruction between 1997 and 2005 and compared endoscopic unilateral versus bilateral stent placement.63 There were no differences in stent insertion success with unilateral and bilateral stenting (100% vs 90%, respectively), drainage success (100% vs 96%, respectively), early complications (0% vs 10%, respectively), or late complications (65% vs 54%, respectively) between the two groups. Of note, long term stent patency was superior in the bilateral metal stenting group relative to the unilateral stenting group in cholangiocarcinoma.63 In another study, Chang et al. showed increased survival with bilateral drainage (225 days) versus unilateral drainage (80 days).64 However, one must keep in mind that it is difficult to place bilateral hilar biliary stents endoscopically due to the anatomy and angulation in the biliary system.
Bilateral side-by-side method
Typically, bilateral stenting is performed using the side-by-side technique. In this technique, two SEMS are placed parallel into the right and left hepatic ducts. If the stents become occluded, endoscopic revision can be performed through each stent, a benefit of this technique.65 Both SEMS should be placed at the same level in the CBD or in the distal ends of the duodenum to allow for easy revision if occlusion occurs.65 Tangling of the two guide wires before deployment, difficulty deploying the stent for drainage, and different stricture lengths are complications with this method.65,66 Chennat et al. tried to overcome these obstacles using a 6F endoscopic biliary SEMS in hilar malignant obstruction.67 Forty-nine Zilver SEMS were placed in 16 patients for Bismuth type II and IV lesions. Placement of stents occurred in 100% of patients. Overall, there was one early and three late stent occlusions, with successful biliary drainage occurring in 75% of patients.67
Bilateral stent-in-stent method
Bilateral stenting is usually accomplished with stents placed in a side-by-side manner. However, an alternative method is the stent-in-stent method. In this method, a SEMS is placed across the bifurcation, and a second SEMS is placed within the contralateral intrahepatic bile duct through the initial stent.61,65,68 Balloon dilation of the contralateral hepatic duct before the deployment of the first SEMS and/or in the initial SEMS has been shown to be useful.61,65,68 A stent particularly suitable for this is the Niti-S large cell D-type biliary stent developed by Taewoong Medical. It has a large 7 mm cell mesh pattern through the entire length of the stent. Kogure et al. examined the feasibility and efficacy of this large mesh stent for both unilateral and bilateral drainage of malignant hilar biliary obstruction.69 Twelve patients first underwent unilateral or bilateral drainage using a plastic stent or nasobiliary drainage tube. If jaundice improved, the plastic stent or drainage tube was replaced with a unilateral large mesh biliary stent; and if jaundice did not improve, bilateral large mesh stents were placed. Stent placement was successful in all 12 patients. Five patients had bilateral stent placement, while seven patients had unilateral placement. Six patients had stent occlusion because of tumor ingrowth (two with bilateral, two unilateral) or sludge (one with bilateral, one unilateral). Median stent patency was 202 days.69 Although the results were comparable with unilateral and bilateral side-by-side stent placement, Kogure and others have demonstrated good success with the stent-in-stent method.
Kim et al. used the stent-in-stent method with a Niti-S biliary Y-stent for malignant hilar obstruction.70 They used an open weave stent, allowing for more flexibility in aligning this area at the hilum.70 The weave is designed to tighten, thereby increasing radial force to maintain cannulation. Kim et al. showed that these stents had a stent-in-stent placement of 87%, with cholangitis reported in 1.5% of patients. The Y-stent bilateral technique is a viable option to treat malignant hilar obstruction.10,70 In 2010, Chahal et al. deployed bilateral SEMS with a stent-in-stent approach.71 They used a large mesh SEMS with deployment across the bifurcation. The second SEMS was deployed through the initial SEMS, forming a Y-shaped configuration. Bilateral drainage was established in all 21 patients attempted. One patient had an early stent occlusion, and seven patients had a late stent occlusion.51,71 The stent-in-stent method avoids excessive expansion of the bile duct compared with the side-by-side stent method and achieves more liver drainage, theoretically decreasing the rate of cholangitis.51 Many of the reported studies for stent-in-stent insertion methods have different numbers of patients, stents, and techniques. Because of the variability across studies, there is no accepted protocol or clinical situation for bilateral stent-in-stent deployment, although it may be the best therapy for cholangiocarcinoma.
Percutaneous vs endoscopic approach
If one chooses percutaneous drainage of a malignant obstruction, magnetic resonance cholangiopancreatography (MRCP) should first be done to assess biliary anatomy to guide therapy.10 A percutaneous drain is then initially placed externally and then converted days later to an internal drain with either plastic stent or SEMS.10 Reported complications of the percutaneous approach are hemothorax, pneumothorax, intraperitoneal bleeding, infection, bile leaks, ascites leak, and subcostal pain.10 The endoscopic approach is associated with fewer complications and shorter hospital stays.10 Lee et al. looked at 134 patients and compared the efficacy of endoscopic retrograde biliary drainage (ERBD), external percutaneous drainage (EPD), and internal percutaneous drainage (IPD).72 Patency for ERBD and IPD were better than EPD with Bismuth type III. IPD provided the best response for Bismuth type IV. There was no difference in the patency rate among drainage procedures for Bismuth type II. Paik et al. also evaluated 85 patients with Bismuth III or IV hilar cholangiocarcinoma. Percutaneous decompression was successful in 93% of patients versus 77% for endoscopic SEMS.73 Current data recommends that Bismuth I-III obstructions should undergo endoscopic stent placement for palliation, while Bismuth IV should undergo percutaneous stent placement.72,73
Management of benign biliary strictures
Benign biliary strictures can have multiple etiologies. Postoperative strictures can be promoted by cholecystectomy or liver transplant, and chronic inflammatory disorders like pancreatitis or primary sclerosing cholangitis can also produce strictures. Benign biliary strictures can manifest with a spectrum of clinical presentations, ranging from asymptomatic to liver failure. Current treatments include hepaticojejunostomy, percutaneous dilatation, and endoscopic dilatation with stent placement.10 Before biliary stents, cholecystectomy induced bile duct injury and strictures were treated surgically with long term patency, on the order of 10–15 years.5 There are few head-to-head studies looking at surgical versus endoscopic management of benign biliary strictures. Davids et al. looked at 66 patients treated for strictures from bile duct injuries, where 31 patients were treated with endoscopic stent placement, and 35 patients were treated surgically.5 Stents were exchanged every 3 months for 1 year. Early complications, like bacteremia, hemorrhaging, and bile leakage, were more common in the surgical group (26% vs. 8%). However, rates of stricture recurrence were similar (17%) for both patient groups at 42 months and at 50 months.5,74 Tocchi et al. showed that patency at 60 months in post-cholescystectomy biliary strictures was 77% (17 of 22) in patients treated with hepaticojejunostomy and 80% (16 of 20) in patients treated with endoscopic stent placement.74,75 Thus, both Tocchi et al. and Davids et al. showed similar outcomes with stent patency after hepaticojejunostomy and direct endoscopic stent placement. Current guidelines in the management of benign biliary strictures with stents are to use dilatation and then to insert one or more large diameter 10F plastic stents. The endoscopic method usually requires multiple ERCP sessions with balloon dilatation and stent placement every 3 months until the stricture resolves.76
Benign stricture dilation prior to stent placement
Dilation of a stricture using hydrostatic balloons or a catheter can be placed over a guide wire to facilitate single or multiple stent placement or be used as therapy alone.77 In most cases, strictures caused by surgery, primary sclerosing cholangitis, and chronic pancreatitis can be initially dilated and then stented to maintain long-term patency.77 There are not many studies examining whether endoscopic dilation alone can be used to treat benign strictures. Kaya et al. looked at 71 patients with dominant strictures caused by primary sclerosing cholangitis and compared balloon dilation to stent placement.78 Thirty-four patients were treated with dilation alone and 37 patients were treated with dilation then stent placement. The number of complications (6 vs 30, respectively p=0.001), including acute cholangitis (p=0.004), were more common in the stent group compared to balloon dilation group. There was no difference between the two groups regarding improvement of bilirubin level.78
Plastic vs metal stents
Temporary placement of multiple plastic stents is possible in >90% of patients with benign biliary strictures. Studies have shown this technique provides the longest patency, but it remains unclear if it is superior for therapy.9,79 Two systematic reviews showed a 94% success rate with placement of multiple plastic stents, 80% with cSEMS, and 60% with single plastic stents.9,79 Endoscopic success in stricture resolution for postoperative strictures is around 80% and 20% in chronic pancreatitis strictures.80 Catalano et al. showed that multiple simultaneous plastic stents are superior to single stent placement. In this study, 12 patients with biliary strictures caused by pancreatitis had multiple stents placed versus 34 patients with single stent placement. Normalization of all liver function tests only occurred in the multiple stent group.9,81 Kuzela et al. examined 43 patients with benign biliary stricture after cholecystectomy who had multiple plastic stents placed.82 The mean follow-up time was 16 months with 100% resolution of biliary strictures.82 Plastic stents in post-transplant biliary strictures were evaluated by Morelli et al. 83 Thirty-eight patients had a mean of 2.5 stents inserted over 107 days. Mean follow-up was 360 days with stricture resolution in 87% of patients.9,83 Complications after stent placement were as follows: cSEMS (40%), single plastic stents (36%), and multiple plastic stents (20%).9 ucSEMS have been looked at in benign biliary strictures, but its use is limited due to mucosal hyperplasia, making stent removal not recommended.9
Fully covered self-expanding metal stents
fcSEMS for use in benign biliary structures is an area actively being studied. Perri et al. conducted a prospective trial consisting of 17 patients examining fcSEMS in biliary strictures caused by chronic pancreatitis not responding to plastic stents.84 Initial stent placement with unflared ends had a migration rate of 100%, with 43% in stricture resolution. Patients were then given flared-end stents, showing 40% migration with stricture resolution of 90% at 6 months and 80% at 12 months.84 Irani et al. performed a retrospective study of 145 patients using cSEMS for the decompression of benign biliary strictures.85 Stricture resolution occurred in 66% of the patients with stent duration of 26 weeks. Extrinsic strictures were treated successfully in 49% of cases, with an 87% success rate in patients with intrinsic strictures. All cSEMS were able to be removed.85 Mahajan et al. used 10 mm fcSEMS with fins in 44 patients with benign biliary strictures. Resolution of the strictures was confirmed in 83% of patients, with a median post-removal follow-up of 3.8 months. Resolution was defined by normalization of liver function tests (LFTs), imaging, and symptoms.4,86 Garcia-Cano et al. performed a similar study with 20 patients and placed 8 mm fcSEMs for benign strictures.87 Stents were extracted at an average time of 4 months, and complete resolution of biliary symptoms were seen in 14 patients (70%) without any reported complications from stent removal.4,87 In 2014, a large prospective multicenter trial by Deviere et al. looked at fcSEMS in 187 patients at 13 centers across 11 countries.88 Successful endoscopic removal was achieved in 75% of patients. Eighty-one percent had stricture resolution for chronic pancreatitis, 63% for post-liver transplant, and 61% for patients that underwent cholecystectomy. Follow-up at the 20 month mark showed a stricture recurrence of 15%.88,89 Plastic stents for benign biliary strictures are the standard of care at present time. Continued long term studies need to be performed on fcSEMS to make conclusions regarding their efficacy and outcome in benign biliary strictures.
Management of biliary leaks
Stents can also be used to treat cystic or bile duct leaks after cholecystectomy, liver transplant, or liver surgery. Cholecystectomy is the most common cause of biliary leaks.9 Stents suppress the pressure gradient between the biliary tree and the duodenum to allow bile into the duodenum and for the leak to seal off.9 Most of the clinical studies in the past have evaluated plastic stents in the treatment of biliary leaks, with resolution in 70–100% of patients.15 Mavrogiannis et al. showed that a 7F stent placement for cystic duct leak post-cholecystectomy is as safe and effective as biliary stenting with sphincterotomy followed by a 10F large-diameter stent.9,90 Luigiano et al. used two fcSEMS for managing a complex bile leak after open cholecystectomy.91 A 10 mm diameter, 8 cm long fully covered Wallflex stent was initially placed, but ERCP showed the proximal end below the bile duct, causing leaks. Another 8 cm fcSEMS was placed inside the first stent, covering the area of damaged bile duct and resolving the leakage. Six weeks later, the stents were removed with confirmed resolution of the bile leak. Removal of the distal stent was complicated by sticking to the bile duct, so a 10 mm diameter controlled radial expansion balloon was used to dislodge the stent. The technique of inflating a balloon inside a stent to assist its removal had been used to remove fcSEMS.4,91 Wang et al. looked at 13 patients with complex bile leaks undergoing temporary placement of fcSEMS after cholecystectomy or liver transplantation.92 All patients had resolution of bile leaks. Ten of 11 patients had biliary debris at removal, and two patients developed a stricture below the confluence. In this study, cSEMS are less prone to migration but are associated with ulcerations, choledocholithaisis, and strictures.4,92
Management of refractory choledocolithaisis
Biliary stone removal fails 5–10% of the time after ERCP, even after the use of lithotripsy or large balloon dilatation technique. If these techniques fail or if an alternative to these approaches is needed, a stent may be inserted. The stent can help with drainage of bile and stone dissolution, which can result in eventual successful endoscopic stone removal.9 To further assist in dissolution of biliary stone, ursodeoxycholic acid with terpene has been shown to increase dissolution of the stone when a stent is in place.9,93 When sphincterotomy is contraindicated or bile duct stone extraction had been unsuccessful, stenting can be beneficial in preventing stone impaction and cholangitis both prior to surgery or before another endoscopy. Many of these patients are high risk surgical candidates, so surgery is not an option. Cerefice et al. reported 29 patients with success in stone clearance when a cSEMS was placed during initial ERCP after unsuccessful stone extraction.94
Stenting complications reviewed
Early complications
Post-ERCP biliary infection is a complication and is fatal in 8–20% of cases.9 Routine antibiotic prophylaxis is recommended in patients with liver transplant, severe neutropenia, hematological malignancy, or incomplete biliary drainage. Full antibiotics should be administered if sufficient biliary drainage is not achieved.9,95
Late complications
Occlusion of stents is the most common cause of stent failure. These stents can be occluded for a variety of reasons. When bacteria deconjugate bilirubin, bilrubinate salt is produced, which leads to obstruction of the stent.4,96 ucSEMS were found to have increased epithelial and mucosal hyperplasia, causing inflammation and requiring repeat stenting.4 cSEMS are showing the most promise with the least incidence of occlusion. Occlusion of biliary SEMS should be treated by inserting a second SEMS or a plastic stent if life expectancy < 3 months.9
Migration is a common complication with plastic stents. Five percent of plastic stents, 1% of pcSEMS, and 35% of fully covered stents have been shown to migrate.9 Most plastic stents that migrate distally are eliminated spontaneously, while most SEMS are rarely eliminated spontaneously and need to be retrieved through ERCP.9 If a SEMS migrates distally and cannot be removed by ERCP, the ends can be trimmed or a second SEMS can be inserted to help with elimination of the first stent.97 Many cSEMS are smooth, which provides little resistance to the bile duct wall, leading to the complication of migration. Anchoring flaps or flared ends help prevent migration. Mahajan et al. showed that only two of 44 cSEMS with anchoring fins migrated, but increasing incidence of ulceration and bleeding were a consequence of the fins.4,86 Because cSEMS can cover the cystic duct, cholecystitis can occur in 3–12% of cases.4 Risk factors for cholecystitis are neoplastic involvement of the cystic duct and gallbladder stones.9
Conclusions
Biliary stents have been used since the early 1980s for the treatment of malignant and benign biliary obstructions. Plastic stents were the first to be used, and there have been continued efforts to design stents to decrease migration obstruction, and complications with removal and placement. Stent technology has expanded to cSEMS and ucSEMS, which have proven to be useful in both hilar and nonhilar malignant obstructions. Postoperative or post-transplant benign strictures or strictures from chronic pancreatitis often are treated with plastic stents. Although not guideline recommended yet, interest in using fcSEMS for benign biliary disease is growing, and studies show promising outcomes. As technology advances, further development of biliary stents promotes continued research. Novel stents, including magnetic, bioabsorbable, antireflux, and drug-eluting stents, have been developed and are still undergoing evaluation. Variability in the techniques used in stent placement studies, different stent designs, and different stent manufacturers make it difficult to draw overarching conclusions regarding which stent is ideal for a given clinical situation. Endoscopists should be aware of the different indications for stent placement, options for stents, and various techniques that are currently available for use in each different clinical situation they may encounter. An informed discussion should be conducted with each patient regarding the best therapeutic options available and realistic expectations in order to optimize outcomes and quality of life.
Acknowledgements
Permission for use of plastic stents (Fig. 1) granted from Cook Medical. Permission for use of uncovered SEMS (Fig. 2) granted from Cook Medical. Permission for use of covered SEMS (Fig. 2) granted from Boston Scientific.
Abbreviations
- CBD
common bile duct
- cSEMS
covered self-expanding metal stents
- EPD
external percutaneous drainage
- ERBD
endoscopic retrograde biliary drainage
- ERCP
esophageal retrograde cholangiopancreatography
- ESGE
European Society for Gastrointestinal Endoscopy
- fcSEMS
fully-covered self-expanding metal stents
- IPD
internal percutaneous drainage
- LFTs
liver function tests
- MRCP
magnetic resonance cholangiopancreatography
- pcSEMS
partially-covered self-expanding metal stents
- PE
polyethyelene
- PU
polyurethane
- RCTs
randomized control trials
- SEMS
self-expanding metal stents
- ucSEMS
uncovered self-expanding metal stents
References
- 1.Hair CD, Sejpal DV. Future developments in biliary stenting. Clin Exp Gastroenterol. 2013;6:91–99. doi: 10.2147/CEG.S34435. 10.2147/CEG.S34435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levy MJ, Baron TH, Gostout CJ, Petersen BT, Farnell MB. Palliation of malignant extrahepatic biliary obstruction with plastic versus expandable metal stents: An evidence-based approach. Clin Gastroenterol Hepatol. 2004;2:273–285. doi: 10.1016/s1542-3565(04)00055-2. 10.1016/S1542-3565(04)00055-2. [DOI] [PubMed] [Google Scholar]
- 3.Geer RJ, Brennan MF. Prognostic indicators for survival after resection of pancreatic adenocarcinoma. Am J Surg. 1993;165:68–72. doi: 10.1016/s0002-9610(05)80406-4. 10.1016/S0002-9610(05)80406-4. ;discussion 72-63. [DOI] [PubMed] [Google Scholar]
- 4.Srinivasan I, Kahaleh M. Biliary stents in the millennium. Adv Ther. 2011;28:960–972. doi: 10.1007/s12325-011-0067-4. 10.1007/s12325-011-0067-4. [DOI] [PubMed] [Google Scholar]
- 5.Davids PH, Tanka AK, Rauws EA, van Gulik TM, van Leeuwen DJ, de Wit LT, et al. Benign biliary strictures. Surgery or endoscopy? Ann Surg. 1993;217:237–243. doi: 10.1097/00000658-199303000-00004. 10.1097/00000658-199303000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huibregtse K, Tytgat GN. Palliative treatment of obstructive jaundice by transpapillary introduction of large bore bile duct endoprosthesis. Gut. 1982;23:371–375. doi: 10.1136/gut.23.5.371. 10.1136/gut.23.5.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Speer AG, Cotton PB, MacRae KD. Endoscopic management of malignant biliary obstruction: stents of 10 French gauge are preferable to stents of 8 French gauge. Gastrointest Endosc. 1988;34:412–417. doi: 10.1016/s0016-5107(88)71407-8. 10.1016/S0016-5107(88)71407-8. [DOI] [PubMed] [Google Scholar]
- 8.Huibregtse K, Cheng J, Coene PP, Fockens P, Tytgat GN. Endoscopic placement of expandable metal stents for biliary strictures-a preliminary report on experience with 33 patients. Endoscopy. 1989;21:280–282. doi: 10.1055/s-2007-1012969. 10.1055/s-2007-1012969. [DOI] [PubMed] [Google Scholar]
- 9.Dumonceau JM, Tringali A, Blero D, Deviere J, Laugiers R, Heresbach D, et al. Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2012;44:277–298. doi: 10.1055/s-0031-1291633. 10.1055/s-0031-1291633. [DOI] [PubMed] [Google Scholar]
- 10.Sejpal D. Advancements in biliary stenting. J Clin Gastroenterol. 2012;46:191–196. doi: 10.1097/MCG.0b013e3182410367. 10.1097/MCG.0b013e3182410367. [DOI] [PubMed] [Google Scholar]
- 11.Moss AC, Morris E, Leyden J, MacMathuna P. Do the benefits of metal stents justify the costs? A systematic review and meta-analysis of trials comparing endoscopic stents for malignant biliary obstruction. Eur J Gastroenterol Hepatol. 2007;19:1119–1124. doi: 10.1097/MEG.0b013e3282f16206. [DOI] [PubMed] [Google Scholar]
- 12.Moss AC, Morris E, Mac Mathuna P. Palliative biliary stents for obstructing pancreatic carcinoma. Cochrane Database Syst Rev. 2006:Cd004200. doi: 10.1002/14651858.CD004200.pub2. 10.1002/14651858.CD004200. [DOI] [PubMed] [Google Scholar]
- 13.Cheon YK, Oh HC, Cho YD, Lee TY, Shim CS. New 10F soft and pliable polyurethane stents decrease the migration rate compared with conventional 10F polyethylene stents in hilar biliary obstruction: results of a pilot study. Gastrointest Endosc. 2012;75:790–797. doi: 10.1016/j.gie.2011.11.010. 10.1016/j.gie.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 14.Galandi D, Schwarzer G, Bassler D, Allgaier HP. Ursodeoxycholic acid and/or antibiotics for prevention of biliary stent occlusion. Cochrane Database Syst Rev. 2002:Cd003043. doi: 10.1002/14651858.CD003043. 10.1002/14651858.CD003043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pfau PR, Pleskow DK, Banerjee S, Barth BA, Bhat YM, Desilets DJ, et al. Pancreatic and biliary stents. Gastrointest Endosc. 2013;77:319–327. doi: 10.1016/j.gie.2012.09.026. 10.1016/j.gie.2012.09.026. [DOI] [PubMed] [Google Scholar]
- 16.Kadakia SC, Starnes E. Comparison of 10 French gauge stent with 11.5 French gauge stent in patients with biliary tract diseases. Gastrointest Endosc. 1992;38:454–459. doi: 10.1016/s0016-5107(92)70476-3. 10.1016/S0016-5107(92)70476-3. [DOI] [PubMed] [Google Scholar]
- 17.Cipolletta L, Rotondano G, Marmo R, Bianco MA. Endoscopic palliation of malignant obstructive jaundice: an evidence-based review. Dig Liver Dis. 2007;39:375–388. doi: 10.1016/j.dld.2006.12.016. 10.1016/j.dld.2006.12.016. [DOI] [PubMed] [Google Scholar]
- 18.Chun HJ, Kim ES, Hyun JJ, Kwon YD, Keum B, Kim CD. Gastrointestinal and biliary stents. J Gastroenterol Hepatol. 2010;25:234–243. doi: 10.1111/j.1440-1746.2009.06152.x. 10.1111/j.1440-1746.2009.06152.x. [DOI] [PubMed] [Google Scholar]
- 19.Chen YK, Jakribettuu V, Springer EW, Shah RJ, Penberthy J, Nash SR. Safety and efficacy of argon plasma coagulation trimming of malpositioned and migrated biliary metal stents: a controlled study in the porcine model. Am J Gastroenterol. 2006;101:2025–2030. doi: 10.1111/j.1572-0241.2006.00744.x. 10.1111/j.1572-0241.2006.00744.x. [DOI] [PubMed] [Google Scholar]
- 20.Kahaleh M, Tokar J, Conaway MR, Brock A, Le T, Adams RB, et al. Efficacy and complications of covered Wallstents in malignant distal biliary obstruction. Gastrointest Endosc. 2005;61:528–533. doi: 10.1016/s0016-5107(04)02593-3. 10.1016/S0016-5107(04)02593-3. [DOI] [PubMed] [Google Scholar]
- 21.Kahaleh M, Brock A, Conaway MR, Shami VM, Dumonceau JM, Northup PG, et al. Covered self-expandable metal stents in pancreatic malignancy regardless of resectability: a new concept validated by a decision analysis. Endoscopy. 2007;39:319–324. doi: 10.1055/s-2007-966263. 10.1055/s-2007-966263. [DOI] [PubMed] [Google Scholar]
- 22.Hu B, Gao DJ, Yu FH, Wang TT, Pan YM, Yang XM. Endoscopic stenting for post-transplant biliary stricture: usefulness of a novel removable covered metal stent. J Hepatobiliary Pancreat Sci. 2011;18:640–645. doi: 10.1007/s00534-011-0408-3. 10.1007/s00534-011-0408-3. [DOI] [PubMed] [Google Scholar]
- 23.Park do H, Lee SS, Lee TH, Ryu CH, Kim HJ, Seo DW, et al. Anchoring flap versus flared end, fully covered self-expandable metal stents to prevent migration in patients with benign biliary strictures: a multicenter, prospective, comparative pilot study (with videos) Gastrointest Endosc. 2011;73:64–70. doi: 10.1016/j.gie.2010.09.039. 10.1016/j.gie.2010.09.039. [DOI] [PubMed] [Google Scholar]
- 24.Loew BJ, Howell DA, Sanders MK, Desilets DJ, Kortan PP, May GR, et al. Comparative performance of uncoated, self-expanding metal biliary stents of different designs in 2 diameters: final results of an international multicenter, randomized, controlled trial. Gastrointest Endosc. 2009;70:445–453. doi: 10.1016/j.gie.2008.11.018. 10.1016/j.gie.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 25.Wagner HJ, Knyrim K, Vakil N, Klose KJ. Plastic endoprostheses versus metal stents in the palliative treatment of malignant hilar biliary obstruction. A prospective and randomized trial. Endoscopy. 1993;25:213–218. doi: 10.1055/s-2007-1010295. 10.1055/s-2007-1010295. [DOI] [PubMed] [Google Scholar]
- 26.Huibregtse K. Plastic or expandable biliary endoprostheses? Scand J Gastroenterol Suppl. 1993;200:3–7. doi: 10.3109/00365529309101567. 10.3109/00365529309101567. [DOI] [PubMed] [Google Scholar]
- 27.Yeoh KG, Zimmerman MJ, Cunningham JT, Cotton PB. Comparative costs of metal versus plastic biliary stent strategies for malignant obstructive jaundice by decision analysis. Gastrointest Endosc. 1999;49:466–471. doi: 10.1016/s0016-5107(99)70044-1. 10.1016/S0016-5107(99)70044-1. [DOI] [PubMed] [Google Scholar]
- 28.Chen VK, Arguedas MR, Baron TH. Expandable metal biliary stents before pancreaticoduodenectomy for pancreatic cancer: a Monte-Carlo decision analysis. Clin Gastroenterol Hepatol. 2005;3:1229–1237. doi: 10.1016/s1542-3565(05)00886-4. 10.1016/S1542-3565(05)00886-4. [DOI] [PubMed] [Google Scholar]
- 29.Yoon WJ, Ryu JK, Yang KY, Paik WH, Lee JK, Woo SM, et al. A comparison of metal and plastic stents for the relief of jaundice in unresectable malignant biliary obstruction in Korea: an emphasis on cost-effectiveness in a country with a low ERCP cost. Gastrointest Endosc. 2009;70:284–289. doi: 10.1016/j.gie.2008.12.241. 10.1016/j.gie.2008.12.241. [DOI] [PubMed] [Google Scholar]
- 30.Ryou M, Cantillon-Murphy P, Shaikh SN, Azagury D, Ryan MB, Lang JH, et al. Magnetic pancreaticobiliary stents and retrieval system: obviating the need for repeat endoscopy (with video) Gastrointest Endosc. 2012;75:888–892.e881. doi: 10.1016/j.gie.2011.09.051. 10.1016/j.gie.2011.09.051. [DOI] [PubMed] [Google Scholar]
- 31.Yamamoto K, Yoshioka T, Furuichi K, Sakaguchi H, Anai H, Tanaka T, et al. Experimental study of poly-L-lactic acid biodegradable stents in normal canine bile ducts. Cardiovasc Intervent Radiol. 2011;34:601–608. doi: 10.1007/s00270-010-0045-2. 10.1007/s00270-010-0045-2. [DOI] [PubMed] [Google Scholar]
- 32.Haber GB. A prospective multi-center study of a bioabsorbable biliary Wallstent in 50 patients with malignant obstructive jaundice. Gastrointest Endosc. 2001;53:AB121–AB121. [Google Scholar]
- 33.Kalinowski M, Alfke H, Kleb B, Durfeld F, Joachim Wagner H. Paclitaxel inhibits proliferation of cell lines responsible for metal stent obstruction: possible topical application in malignant bile duct obstructions. Invest Radiol. 2002;37:399–404. doi: 10.1097/00004424-200207000-00007. 10.1097/00004424-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Suk KT, Kim JW, Kim HS, Baik SK, Oh SJ, Lee SJ, et al. Human application of a metallic stent covered with a paclitaxel-incorporated membrane for malignant biliary obstruction: multicenter pilot study. Gastrointest Endosc. 2007;66:798–803. doi: 10.1016/j.gie.2007.05.037. 10.1016/j.gie.2007.05.037. [DOI] [PubMed] [Google Scholar]
- 35.Song TJ, Lee SS, Yun SC, Park do H, Seo DW, Lee SK, et al. Paclitaxel-eluting covered metal stents versus covered metal stents for distal malignant biliary obstruction: a prospective comparative pilot study. Gastrointest Endosc. 2011;73:727–733. doi: 10.1016/j.gie.2010.11.048. 10.1016/j.gie.2010.11.048. [DOI] [PubMed] [Google Scholar]
- 36.Dua KS, Reddy ND, Rao VG, Banerjee R, Medda B, Lang I. Impact of reducing duodenobiliary reflux on biliary stent patency: an in vitro evaluation and a prospective randomized clinical trial that used a biliary stent with an antireflux valve. Gastrointest Endosc. 2007;65:819–828. doi: 10.1016/j.gie.2006.09.011. 10.1016/j.gie.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 37.Hu B, Wang TT, Shi ZM, Wang SZ, Lu R, Pan YM, et al. A novel antireflux metal stent for the palliation of biliary malignancies: a pilot feasibility study (with video) Gastrointest Endosc. 2011;73:143–148. doi: 10.1016/j.gie.2010.08.048. 10.1016/j.gie.2010.08.048. [DOI] [PubMed] [Google Scholar]
- 38.Hu B, Wu J, Gao DJ, Wang TT. 144 The Role of Anti-Reflux Biliary Stent: A Prospective Randomized Study in 104 Cases. Gastrointest Endosc. 2012;75:AB122. [Google Scholar]
- 39.Artifon EL, Sakai P, Ishioka S, Marques SB, Lino AS, Cunha JE, et al. Endoscopic sphincterotomy before deployment of covered metal stent is associated with greater complication rate: a prospective randomized control trial. J Clin Gastroenterol. 2008;42:815–819. doi: 10.1097/MCG.0b013e31803dcd8a. 10.1097/MCG.0b013e31803dcd8a. [DOI] [PubMed] [Google Scholar]
- 40.Giorgio PD, Luca LD. Comparison of treatment outcomes between biliary plastic stent placements with and without endoscopic sphincterotomy for inoperable malignant common bile duct obstruction. World J Gastroenterol. 2004;10:1212–1214. doi: 10.3748/wjg.v10.i8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hui CK, Lai KC, Yuen MF, Ng M, Chan CK, Hu W, et al. Does the addition of endoscopic sphincterotomy to stent insertion improve drainage of the bile duct in acute suppurative cholangitis? Gastrointest Endosc. 2003;58:500–504. doi: 10.1067/s0016-5107(03)01871-6. 10.1067/S0016-5107(03)01871-6. [DOI] [PubMed] [Google Scholar]
- 42.Banerjee N, Hilden K, Baron TH, Adler DG. Endoscopic biliary sphincterotomy is not required for transpapillary SEMS placement for biliary obstruction. Dig Dis Sci. 2011;56:591–595. doi: 10.1007/s10620-010-1317-z. 10.1007/s10620-010-1317-z. [DOI] [PubMed] [Google Scholar]
- 43.Moss AC, Morris E, Leyden J, MacMathuna P. Malignant distal biliary obstruction: a systematic review and meta-analysis of endoscopic and surgical bypass results. Cancer Treat Rev. 2007;33:213–221. doi: 10.1016/j.ctrv.2006.10.006. 10.1016/j.ctrv.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 44.Pop GH, Richter JA, Sauer B, Rehan ME, Ho HC, Adams RB, et al. Bridge to surgery using partially covered self-expandable metal stents (PCMS) in malignant biliary stricture: an acceptable paradigm? Surg Endosc. 2011;25:613–618. doi: 10.1007/s00464-010-1231-7. 10.1007/s00464-010-1231-7. [DOI] [PubMed] [Google Scholar]
- 45.Saleem A, Leggett CL, Murad MH, Baron TH. Meta-analysis of randomized trials comparing the patency of covered and uncovered self-expandable metal stents for palliation of distal malignant bile duct obstruction. Gastrointest Endosc. 2011;74:321–327.e321-323. doi: 10.1016/j.gie.2011.03.1249. 10.1016/j.gie.2011.03.1249. [DOI] [PubMed] [Google Scholar]
- 46.Soderlund C, Linder S. Covered metal versus plastic stents for malignant common bile duct stenosis: a prospective, randomized, controlled trial. Gastrointest Endosc. 2006;63:986–995. doi: 10.1016/j.gie.2005.11.052. 10.1016/j.gie.2005.11.052. [DOI] [PubMed] [Google Scholar]
- 47.Kullman E, Frozanpor F, Soderlund C, Linder S, Sandstrom P, Lindhoff-Larsson A, et al. Covered versus uncovered self-expandable nitinol stents in the palliative treatment of malignant distal biliary obstruction: results from a randomized, multicenter study. Gastrointest Endosc. 2010;72:915–923. doi: 10.1016/j.gie.2010.07.036. 10.1016/j.gie.2010.07.036. [DOI] [PubMed] [Google Scholar]
- 48.Isayama H, Komatsu Y, Tsujino T, Sasahira N, Hirano K, Toda N, et al. A prospective randomised study of “covered” versus “uncovered” diamond stents for the management of distal malignant biliary obstruction. Gut. 2004;53:729–734. doi: 10.1136/gut.2003.018945. 10.1136/gut.2003.018945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thurnher SA, Lammer J, Thurnher MM, Winkelbauer F, Graf O, Wildling R. Covered self-expanding transhepatic biliary stents: clinical pilot study. Cardiovasc Intervent Radiol. 1996;19:10–14. doi: 10.1007/BF02560140. 10.1007/BF02560140. [DOI] [PubMed] [Google Scholar]
- 50.Telford JJ, Carr-Locke DL, Baron TH, Poneros JM, Bounds BC, Kelsey PB, et al. A randomized trial comparing uncovered and partially covered self-expandable metal stents in the palliation of distal malignant biliary obstruction. Gastrointest Endosc. 2010;72:907–914. doi: 10.1016/j.gie.2010.08.021. 10.1016/j.gie.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 51.Lee TH, Moon JH, Park SH. Bilateral metallic stenting in malignant hilar obstruction. Clin Endosc. 2014;47:440–446. doi: 10.5946/ce.2014.47.5.440. 10.5946/ce.2014.47.5.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lai EC, Mok FP, Fan ST, Lo CM, Chu KM, Liu CL, et al. Preoperative endoscopic drainage for malignant obstructive jaundice. Br J Surg. 1994;81:1195–1198. doi: 10.1002/bjs.1800810839. [DOI] [PubMed] [Google Scholar]
- 53.van der Gaag NA, Rauws EA, van Eijck CH, Bruno MJ, van der Harst E, Kubben FJ, et al. Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med. 2010;362:129–137. doi: 10.1056/NEJMoa0903230. 10.1056/NEJMoa0903230. [DOI] [PubMed] [Google Scholar]
- 54.Liu F, Li Y, Wei Y, Li B. Preoperative biliary drainage before resection for hilar cholangiocarcinoma: whether or not? A systematic review. Dig Dis Sci. 2011;56:663–672. doi: 10.1007/s10620-010-1338-7. 10.1007/s10620-010-1338-7. [DOI] [PubMed] [Google Scholar]
- 55.Mullen JT, Lee JH, Gomez HF, Ross WA, Fukami N, Wolff RA, et al. Pancreaticoduodenectomy after placement of endobiliary metal stents. J Gastrointest Surg. 2005;9:1094–1104. doi: 10.1016/j.gassur.2005.08.006. 10.1016/j.gassur.2005.08.006. ;discussion 1104-1095. [DOI] [PubMed] [Google Scholar]
- 56.Wasan SM, Ross WA, Staerkel GA, Lee JH. Use of expandable metallic biliary stents in resectable pancreatic cancer. Am J Gastroenterol. 2005;100:2056–2061. doi: 10.1111/j.1572-0241.2005.42031.x. 10.1111/j.1572-0241.2005.42031.x. [DOI] [PubMed] [Google Scholar]
- 57.Smith AC, Dowsett JF, Russell RC, Hatfield AR, Cotton PB. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstruction. Lancet. 1994;344:1655–1660. doi: 10.1016/s0140-6736(94)90455-3. 10.1016/S0140-6736(94)90455-3. [DOI] [PubMed] [Google Scholar]
- 58.Perdue DG, Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, et al. Plastic versus self-expanding metallic stents for malignant hilar biliary obstruction: a prospective multicenter observational cohort study. J Clin Gastroenterol. 2008;42:1040–1046. doi: 10.1097/MCG.0b013e31815853e0. 10.1097/MCG.0b013e31815853e0. [DOI] [PubMed] [Google Scholar]
- 59.Raju RP, Jaganmohan SR, Ross WA, Davila ML, Javle M, Raju GS, et al. Optimum palliation of inoperable hilar cholangiocarcinoma: comparative assessment of the efficacy of plastic and self-expanding metal stents. Dig Dis Sci. 2011;56:1557–1564. doi: 10.1007/s10620-010-1550-5. 10.1007/s10620-010-1550-5. [DOI] [PubMed] [Google Scholar]
- 60.Cheng JL, Bruno MJ, Bergman JJ, Rauws EA, Tytgat GN, Huibregtse K. Endoscopic palliation of patients with biliary obstruction caused by nonresectable hilar cholangiocarcinoma: efficacy of self-expandable metallic Wallstents. Gastrointest Endosc. 2002;56:33–39. doi: 10.1067/mge.2002.125364. 10.1067/mge.2002.125364. [DOI] [PubMed] [Google Scholar]
- 61.Park do H, Lee SS, Moon JH, Choi HJ, Cha SW, Kim JH, et al. Newly designed stent for endoscopic bilateral stent-in-stent placement of metallic stents in patients with malignant hilar biliary strictures: multicenter prospective feasibility study (with videos) Gastrointest Endosc. 2009;69:1357–1360. doi: 10.1016/j.gie.2008.12.250. 10.1016/j.gie.2008.12.250. [DOI] [PubMed] [Google Scholar]
- 62.Vienne A, Hobeika E, Gouya H, Lapidus N, Fritsch J, Choury AD, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc. 2010;72:728–735. doi: 10.1016/j.gie.2010.06.040. 10.1016/j.gie.2010.06.040. [DOI] [PubMed] [Google Scholar]
- 63.Naitoh I, Ohara H, Nakazawa T, Ando T, Hayashi K, Okumura F, et al. Unilateral versus bilateral endoscopic metal stenting for malignant hilar biliary obstruction. J Gastroenterol Hepatol. 2009;24:552–557. doi: 10.1111/j.1440-1746.2008.05750.x. 10.1111/j.1440-1746.2008.05750.x. [DOI] [PubMed] [Google Scholar]
- 64.Chang WH, Kortan P, Haber GB. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc. 1998;47:354–362. doi: 10.1016/s0016-5107(98)70218-4. 10.1016/S0016-5107(98)70218-4. [DOI] [PubMed] [Google Scholar]
- 65.Lee TH, Moon JH, Kim JH, Park DH, Lee SS, Choi HJ, et al. Primary and revision efficacy of cross-wired metallic stents for endoscopic bilateral stent-in-stent placement in malignant hilar biliary strictures. Endoscopy. 2013;45:106–113. doi: 10.1055/s-0032-1325928. 10.1055/s-0032-1326345. [DOI] [PubMed] [Google Scholar]
- 66.Kim JH. Endoscopic stent placement in the palliation of malignant biliary obstruction. Clin Endosc. 2011;44:76–86. doi: 10.5946/ce.2011.44.2.76. 10.5946/ce.2011.44.2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chennat J, Waxman I. Initial performance profile of a new 6F self-expanding metal stent for palliation of malignant hilar biliary obstruction. Gastrointest Endosc. 2010;72:632–636. doi: 10.1016/j.gie.2010.04.037. 10.1016/j.gie.2010.04.037. [DOI] [PubMed] [Google Scholar]
- 68.Lee TH, Park do H, Lee SS, Choi HJ, Lee JK, Kim TH, et al. Technical feasibility and revision efficacy of the sequential deployment of endoscopic bilateral side-by-side metal stents for malignant hilar biliary strictures: a multicenter prospective study. Dig Dis Sci. 2013;58:547–555. doi: 10.1007/s10620-012-2346-6. 10.1007/s10620-012-2346-6. [DOI] [PubMed] [Google Scholar]
- 69.Kogure H, Isayama H, Nakai Y, Tsujino T, Ito Y, Yamamoto K, et al. Newly designed large cell Niti-S stent for malignant hilar biliary obstruction: a pilot study. Surg Endosc. 2011;25:463–467. doi: 10.1007/s00464-010-1194-8. 10.1007/s00464-010-1194-8. [DOI] [PubMed] [Google Scholar]
- 70.Kim DU, Kang DH, Kim GH, Song GA, Kim CW, Kim S, et al. Bilateral biliary drainage for malignant hilar obstruction using the ‘stent-in-stent’ method with a Y-stent: efficacy and complications. Eur J Gastroenterol Hepatol. 2013;25:99–106. doi: 10.1097/MEG.0b013e3283590a2a. 10.1097/MEG.0b013e3283590a2a. [DOI] [PubMed] [Google Scholar]
- 71.Chahal P, Baron TH. Expandable metal stents for endoscopic bilateral stent-within-stent placement for malignant hilar biliary obstruction. Gastrointest Endosc. 2010;71:195–199. doi: 10.1016/j.gie.2009.08.006. 10.1016/j.gie.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 72.Lee SH, Park JK, Yoon WJ, Lee JK, Ryu JK, Yoon YB, et al. Optimal biliary drainage for inoperable Klatskin's tumor based on Bismuth type. World J Gastroenterol. 2007;13:3948–3955. doi: 10.3748/wjg.v13.i29.3948. 10.3748/wjg.v13.i29.3948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Paik WH, Park YS, Hwang JH, Lee SH, Yoon CJ, Kang SG, et al. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc. 2009;69:55–62. doi: 10.1016/j.gie.2008.04.005. 10.1016/j.gie.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 74.Sikora SS. Postcholecystectomy benign biliary stricture: Surgery is the gold standard. J Dig Endosc. 2012;3:36–39. 10.4103/0976-5042.95029. [Google Scholar]
- 75.Tocchi A, Mazzoni G, Liotta G, Costa G, Lepre L, Miccini M, et al. Management of benign biliary strictures: biliary enteric anastomosis vs endoscopic stenting. Arch Surg. 2000;135:153–157. doi: 10.1001/archsurg.135.2.153. 10.1001/archsurg.135.2.153. [DOI] [PubMed] [Google Scholar]
- 76.Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri V. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc. 2001;54:162–168. doi: 10.1067/mge.2001.116876. 10.1067/mge.2001.116876. [DOI] [PubMed] [Google Scholar]
- 77.Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, et al. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005;62:1–8. doi: 10.1016/j.gie.2005.04.015. 10.1016/j.gie.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 78.Kaya M, Petersen BT, Angulo P, Baron TH, Andrews JC, Gostout CJ, et al. Balloon dilation compared to stenting of dominant strictures in primary sclerosing cholangitis. Am J Gastroenterol. 2001;96:1059–1066. doi: 10.1111/j.1572-0241.2001.03690.x. 10.1111/j.1572-0241.2001.03690.x. [DOI] [PubMed] [Google Scholar]
- 79.van Boeckel PG, Vleggaar FP, Siersema PD. Plastic or metal stents for benign extrahepatic biliary strictures: a systematic review. BMC Gastroenterol. 2009;9:96. doi: 10.1186/1471-230X-9-96. 10.1186/1471-230X-9-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Farnbacher MJ, Rabenstein T, Ell C, Hahn EG, Schneider HT. Is endoscopic drainage of common bile duct stenoses in chronic pancreatitis up-to-date? Am J Gastroenterol. 2000;95:1466–1471. doi: 10.1111/j.1572-0241.2000.02078.x. 10.1111/j.1572-0241.2000.02078.x. [DOI] [PubMed] [Google Scholar]
- 81.Catalano MF, Linder JD, George S, Alcocer E, Geenen JE. Treatment of symptomatic distal common bile duct stenosis secondary to chronic pancreatitis: comparison of single vs. multiple simultaneous stents. Gastrointest Endosc. 2004;60:945–952. doi: 10.1016/s0016-5107(04)02275-8. 10.1016/S0016-5107(04)02275-8. [DOI] [PubMed] [Google Scholar]
- 82.Kuzela L, Oltman M, Sutka J, Hrcka R, Novotna T, Vavrecka A. Prospective follow-up of patients with bile duct strictures secondary to laparoscopic cholecystectomy, treated endoscopically with multiple stents. Hepatogastroenterology. 2005;52:1357–1361. [PubMed] [Google Scholar]
- 83.Morelli G, Fazel A, Judah J, Pan JJ, Forsmark C, Draganov P. Rapid-sequence endoscopic management of posttransplant anastomotic biliary strictures. Gastrointest Endosc. 2008;67:879–885. doi: 10.1016/j.gie.2007.08.046. 10.1016/j.gie.2007.08.046. [DOI] [PubMed] [Google Scholar]
- 84.Perri V, Boskoski I, Tringali A, Familiari P, Mutignani M, Marmo R, et al. Fully covered self-expandable metal stents in biliary strictures caused by chronic pancreatitis not responding to plastic stenting: a prospective study with 2 years of follow-up. Gastrointest Endosc. 2012;75:1271–1277. doi: 10.1016/j.gie.2012.02.002. 10.1016/j.gie.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 85.Irani S, Baron TH, Akbar A, Lin OS, Gluck M, Gan I, et al. Endoscopic treatment of benign biliary strictures using covered self-expandable metal stents (CSEMS) Dig Dis Sci. 2014;59:152–160. doi: 10.1007/s10620-013-2859-7. 10.1007/s10620-013-2859-7. [DOI] [PubMed] [Google Scholar]
- 86.Mahajan A, Ho H, Sauer B, Phillips MS, Shami VM, Ellen K, et al. Temporary placement of fully covered self-expandable metal stents in benign biliary strictures: midterm evaluation (with video) Gastrointest Endosc. 2009;70:303–309. doi: 10.1016/j.gie.2008.11.029. 10.1016/j.gie.2008.11.029. [DOI] [PubMed] [Google Scholar]
- 87.Garcia-Cano J, Taberna-Arana L, Jimeno-Ayllon C, Martinez-Fernandez R, Serrano-Sanchez L, Reyes-Guevara AK, et al. Use of fully covered self-expanding metal stents for the management of benign biliary conditions. Rev Esp Enferm Dig. 2010;102:526–532. doi: 10.4321/s1130-01082010000900003. [DOI] [PubMed] [Google Scholar]
- 88.Deviere J, Nageshwar Reddy D, Puspok A, Ponchon T, Bruno MJ, Bourke MJ, et al. Successful management of benign biliary strictures with fully covered self-expanding metal stents. Gastroenterology. 2014;147:385–395. doi: 10.1053/j.gastro.2014.04.043. 10.1053/j.gastro.2014.04.043. ;quiz e315. [DOI] [PubMed] [Google Scholar]
- 89.Deviere JM, Reddy DN, Puspok A, Ponchon T, Bruno MJ, Bourke MJ, et al. 147 Preliminary Results From a 187 Patient Multicenter Prospective Trial Using Metal Stents for Treatment of Benign Biliary Strictures. Gastrointest Endosc. 2012;75:AB123. [Google Scholar]
- 90.Mavrogiannis C, Liatsos C, Papanikolaou IS, Karagiannis S, Galanis P, Romanos A. Biliary stenting alone versus biliary stenting plus sphincterotomy for the treatment of post-laparoscopic cholecystectomy biliary leaks: a prospective randomized study. Eur J Gastroenterol Hepatol. 2006;18:405–409. doi: 10.1097/00042737-200604000-00014. [DOI] [PubMed] [Google Scholar]
- 91.Luigiano C, Ferrara F, Fabbri C, Bassi M, Cennamo V, D'Imperio N. Insertion of two overlapping new covered metal stents for closure of a complex biliary leak and description of a safe technique for their removal. Endoscopy. 2011;43(Suppl 2):UCTN:E211–E212. doi: 10.1055/s-0030-1256394. 10.1055/s-0030-1256394. [DOI] [PubMed] [Google Scholar]
- 92.Wang AY, Ellen K, Berg CL, Schmitt TM, Kahaleh M. Fully covered self-expandable metallic stents in the management of complex biliary leaks: preliminary data-a case series. Endoscopy. 2009;41:781–786. doi: 10.1055/s-0029-1215050. 10.1055/s-0029-1215050. [DOI] [PubMed] [Google Scholar]
- 93.Han J, Moon JH, Koo HC, Kang JH, Choi JH, Jeong S, et al. Effect of biliary stenting combined with ursodeoxycholic acid and terpene treatment on retained common bile duct stones in elderly patients: a multicenter study. Am J Gastroenterol. 2009;104:2418–2421. doi: 10.1038/ajg.2009.303. 10.1038/ajg.2009.303. [DOI] [PubMed] [Google Scholar]
- 94.Cerefice M, Sauer BG, Smith La, Javaid MA, Gosain S, Argo CK, et al. T1522: Covered Self-Expanding Metal Stents in Complex Biliary Stone Cases: Long Term Experience. Gastrointest Endosc. 2010;71:AB299. doi: 10.1016/j.gie.2011.05.026. [DOI] [PubMed] [Google Scholar]
- 95.Allison MC, Sandoe JA, Tighe R, Simpson IA, Hall RJ, Elliott TS. Antibiotic prophylaxis in gastrointestinal endoscopy. Gut. 2009;58:869–880. doi: 10.1136/gut.2007.136580. 10.1136/gut.2007.136580. [DOI] [PubMed] [Google Scholar]
- 96.Dowidar N, Kolmos HJ, Matzen P. Experimental clogging of biliary endoprostheses. Role of bacteria, endoprosthesis material, and design. Scand J Gastroenterol. 1992;27:77–80. doi: 10.3109/00365529209011171. [DOI] [PubMed] [Google Scholar]
- 97.Dumonceau JM, Heresbach D, Deviere J, Costamagna G, Beilenhoff U, Riphaus A. Biliary stents: models and methods for endoscopic stenting. Endoscopy. 2011;43:617–626. doi: 10.1055/s-0030-1256315. 10.1055/s-0030-1256315. [DOI] [PubMed] [Google Scholar]


