Abstract
Autoimmune hepatitis (AIH), a liver disorder affecting both children and adults, is characterized by inflammatory liver histology, elevated transaminase levels, circulating nonorganspecific autoantibodies, and increased levels of immunoglobulin G, in the absence of a known etiology. Two types of AIH are recognized according to seropositivity: smooth muscle antibody and/or antinuclear antibody define AIH type 1 and antibodies to liver-kidney microsome type 1 and/or liver cytosol type 1 define AIH type 2. AIH type 1 affects both adults and children, while AIH type 2 is mainly a paediatric disease, though it does occasionally affects young adults. AIH should be considered during the diagnostic workup of any patient with increased liver enzyme levels. AIH is exquisitely responsive to immunosuppressive treatment with prednisolone with or without azathioprine, with symptom free long-term survival for the majority of patients. For those who do not respond to standard treatment, or who are difficult-to-treat, mycophenolate mofetil and, in the absence of a response, calcineurin inhibitors should be tried in addition to steroids. The pathogenesis of AIH is not fully understood, although there is mounting evidence that genetic susceptibility, molecular mimicry and impaired immunoregulatory networks contribute to the initiation and perpetuation of the autoimmune attack. Liver damage is thought to be mediated primarily by CD4 T-cells, although recent studies support the involvement of diverse populations, including Th17 cells. A deeper understanding of the pathogenesis of AIH is likely to contribute to the development of novel treatments, such as the adoptive transfer of autologous expanded antigenspecific regulatory T-cells, which ultimately aim at restoring tolerance to liver-derived antigens.
Keywords: Autoimmune hepatitis, Autoantibodies, Immunogenetics, Regulatory T cells, Immunosuppresion
Introduction
The first decsription of autoimmune hepatitis (AIH) dates back to the 1950s, when Jan Waldenström reported a group of young women affected by severe and fluctuating persistent hepatitis associated with acneiform rashes, spider angiomas, anovulatory amenorrhea and profoundly elevated serum immunoglobulins.1 The presence of lupus erythematosus cells and of antinuclear antibody (ANA) seropositivity, subsequently led to the adoption of the term ‘‘lupoid hepatitis’’ and the idea that the condition stems from a loss of immunological tolerance.2 The positive impact of steroid therapy, first recognised in the early 1960s, resulted in the publication of three controlled clinical trials which incontrovertibly showed the life-saving value of corticosteroids in the treatment of ‘‘HBsAg-negative hepatitis’’.3–5 The recognition that ‘‘chronic active autoimmune hepatitis’’, as it was then known, constituted a distinct clinical entity followed the systematic evaluation of its clinical symptoms, laboratory features, and molecular immunopathology. During two working meetings held in the early 1990s, the International Autoimmune Hepatitis Group (IAIHG), dropped ‘chronic’ and introduced the term ‘‘autoimmune hepatitis’’, as originally suggested by Ian Mackay in 1965,6 since the disease frequently presents acutely and often has a fluctuating course, characterised by spontaneous remission, being therefore occasionally inactive. The IAIHG continues to monitor developments in the field regularly, and was responsible for the development of an initial scoring system for the diagnosis of AIH,7 subsequently revised.8 More recently, a simplified system, designed for use in clinical practice, has been proposed by the group.9
Two types of AIH are recognised, based on the serological autoantibody profile: AIH type 1 (AIH-1) is defined by positivity for ANA and/or anti-smooth muscle antibody (SMA), whereas AIH type 2 (AIH-2) is characteriszed by the presence of anti-liver kidney microsomal type 1 antibody (anti-LKM-1) or anti-liver cytosol type 1 antibody (anti-LC-1). Besides the presence of autoantibodies, AIH is associated biochemically with elevated transaminase levels, histologically with interface hepatitis, and serologically with increased levels of IgG. Immunosuppressive therapy, which remains the mainstay of treatment, should be instituted as soon as the diagnosis is made, and, generally, the response is good. If left untreated, AIH usually progresses to liver failure requiring transplantation. The etiology of AIH is unknown, though both genetic and environmental factors are likely to be involved. An immune response targeting liver autoantigens, unrestrained because of the failure of immunoregulatory mechanisms, is thought to initiate and perpetuate the liver damage.10 Here, we review recent breakthroughs in our understanding of the pathogenesis of AIH, linking them to advances in clinical practice.
Epidemiology
The actual prevalence of AIH is unknown. Few descriptive epidemiological studies are available, and the majority of them do not rely on standard criteria for patients’ inclusion, since they were performed prior to the introduction of the IAIHG scoring system, and therefore no standardized way of evaluating patients was used. Moreover, early studies did not exclude patients with chronic hepatitis C. In a study conducted in a Norwegian population, Boberg et al. found a mean annual incidence of 1.9 cases per 100,000 people per year with a prevalence of 16.9 cases per 100,000 people.11 Another study, conducted in a Spanish population, reported an annual incidence of 0.83 cases per 100,000 inhabitants in the population aged. 14 years with a prevalence of 11.6 cases per 100,000.12 It should be pointed out, however, that this was a hospital-based study, consequently limited by tertiary referral bias, which can result in an underestimation of incidence and prevalence and an overestimation of disease severity. A study that examined the prevalence of AIH in Alaskan natives reported a prevalence of definite AIH in 34.5 cases per 100,000.13 This was the first study to use the IAIHG scoring system, and the rate observed was over twice as high as that of another population based study (i.e. the Norwegian one referred to earlier). A study from the United Kingdom, conducted in a secondary care referral center, showed that the annual incidence of AIH was 3.5 per 100,000 inhabitants. 14 More recently, an epidemiological study carried out in New Zealand in which standardized inclusion criteria were deployed, reported an annual incidence of 2.0 cases of AIH per 100,000 and a point prevalence of 24.5 cases per 100,000.15 In Asia, most reports come from Japan, where AIH is considerably less frequent with an incidence estimated between 0.08 and 0.15 cases per 100,000 people per year.16,17 Similarly, AIH was long thought to be uncommon in China;18 however, with a more refined diagnostic work-up of patients, AIH has been increasingly reported in that country.19
The prevalence of AIH-2, which affects mainly children and young adults, is unknown, because the diagnosis is often overlooked. At King's College Hospital tertiary pediatric hepatology referral center, there has been a seven-fold increase in the incidence of both types of AIH over the last decade.20 AIH represents approximately 10% of some 400 new pediatric referrals per year; where two-third of the cases are AIH-1, and one-third are AIH-2.20
AIH, though characterized by a strong female preponderance (female/male 53.6/1),21 occurs in children and adults of both sexes. AIH was believed to be a disease of the young and middle aged, but it is now clear that it affects adults of all ages, including individuals older than 60.22,23
Pathogenesis
Genetics
In AIH, the strongest associations are located within the human leukocyte antigen (HLA)-DRB1 locus, with HLADRB1* 03 and HLA-DRB1*04 conferring susceptibility in European and North American populations.8 These associations have been recently confirmed in the first AIH genomewide association study.24 Susceptibility to AIH-2 is associated with HLA-DR*03 and HLA-DR*07 in the United Kingdom and Brazil.25 Non-HLA associations include CTLA-4,26 the tumor necrosis factor (TNF)a gene promoter,27 and FAS,28 an important inducer of the extrinsic apoptotic pathway.
Mechanisms of liver damage
The mechanisms leading to autoimmune liver damage have been a focus of intense investigation over the past three decades. However, the initial trigger of liver centered autoimmunity remains elusive.
The histological picture of interface hepatitis, the hallmark of the disease and composed of lymphocytes, plasma cells, and macrophages, was the first evidence to suggest that an autoaggressive cellular immune attack was the basis of this condition. Whatever the initial trigger, this massive recruitment of activated inflammatory cells is likely to cause damage. Immunohistochemical studies performed in the early 1990s identified a predominance of T lymphocytes expressing the α/β T cell receptor.29 Amongst T cells, the majority were positive for the CD4 helper/inducer phenotype and a sizable minority were positive for the CD8 cytotoxic phenotype. Lymphocytes of a non T cell lineage were fewer and included NK cells, macrophages, B cells, and plasma cells.29
Regardless of the factors triggering the autoimmune process, the pathogenic mechanism leading to liver damage is part of a complex scenario, involving the intervention of both innate and adaptive arms of the immune system. Liver damage is probably orchestrated by CD4pos lymphocytes that recognize a self-antigenic peptide. In the presence of the appropriate costimulatory signals, the autoimmune response is initiated after the peptide is embraced by an HLA class II molecule and presented by an antigen presenting cell (APC) to a naïve CD4pos T helper cell (Th0). Once activated, and depending on the type of cytokines present in the microenvironment and the nature of the antigen, Th0 cells can differentiate into: Th1, Th2, and Th17 cells. These effector cells initiate a cascade of immune reactions largely determined by the cytokines they produce: a) Th1 cells secrete mainly interleukin (IL)-2 and interferon (IFN)-γ; IFN-γ is considered the main orchestrator of tissue damage since it not only stimulates CD8 cells, enhances the expression of HLA class I, and induces expression of HLA class II molecules on hepatocytes,30,31 but also activates monocytes/macrophages, which in turn release IL-1 and TNF-α; b) Th2 cells produce IL-4, IL-10, and IL-13, cytokines that induce the maturation of B cells into plasma cells, with consequent production of autoantibodies; c) Th17 cells, which arise in the presence of transforming growth factor (TGF)-β and IL-6, produce IL-17, IL-22, TNF-α, and chemokine ligand (CCL)- 20.32 Th17 immunity has quite recently been associated in both mice and humans with autoimmune disease.33 These cells have been implicated in the pathogenesis of another autoimmune liver disease, primary biliary cirrhosis (PBC).34 Although their contribution to liver damage in AIH is still under investigation, a recent paper showed an increased number of Th17 cells in both the peripheral blood and liver of patients with AIH compared to healthy controls.35
If regulatory Tcells (Tregs) are numerically and functionally impaired in AIH, a number of effector responses, including direct action of cytotoxic T lymphocytes (CTL), cytokines released by Th1, and possibly Th17 cells and monocytes/ macrophages, and complement activation or engagement of natural killer cells by autoantibodies bound to the hepatocyte surface, perpetuate liver cell destruction (Fig. 1).36
Fig. 1. Autoimmune attack to the liver cell.
An autoantigenic peptide is presented to an uncommitted T helper (Th0) lymphocyte within the HLA class II molecule of an antigen-presenting cell (APC). Th0 cells become activated and, according to the cytokines present in the microenvironment and the nature of the antigen, differentiate into Th1, Th2, or Th17 cells, initiating a series of immune reactions determined by the cytokines they produce: Th2 secrete mainly IL-4, IL-10, and IL-13 and direct autoantibody production by B lymphocytes; Th1 secrete IL-2 and IFN-γ, which stimulate cytotoxic T lymphocytes (CTL), enhance expression of class I, and induce expression of class II HLA molecules on hepatocytes and activate macrophages; activated macrophages release IL-1 and tumor necrosis factor alpha (TNF-α). If regulatory Tcells do not oppose, a variety of effector mechanisms are triggered: liver cell destruction could derive from the action of CTL; cytokines released by Th1 and recruited macrophages; complement activation; or engagement of Fc receptor-bearing cells, such as natural killer (NK) lymphocytes, by the autoantibody bound to the hepatocyte surface. The role of the recently described Th17 cells, which arise in the presence of transforming growth factor beta (TGF-γ) and IL-6, is under investigation.
Impairment of regulatory T-cells
Several studies have reported that Tregs are numerically defective in AIH patients compared to healthy subjects (HS). A lower circulating frequency of CD4posCD25pos 37,38 or CD4posCD25high 39 Tregs has been reported in AIH patients compared to HS, and this defect is associated with lower forkhead box P3 (FOXP3) expression.39,40 Moreover, during immunosuppressive therapy, the circulating Treg frequency has been shown to increase to some extent, although not equating the levels seen in HS.37,39 In one study, however, the circulating frequency of CD4posCD25highCD127neg FOXP3pos cells was equal in AIH patients and HS, and the frequency of this population was higher in patients with active disease compared to those in remission.41
In coculture with CD4posCD25neg cells, magnetically isolated CD4posCD25pos Tregs from AIH patients were less able to generate an antiinflammatory cytokine milieu rich in TGFb, suggesting that Tregs from AIH patients are ineffective promoters of linked-suppression.40 Magnetically isolated CD4posCD25pos Tregs from AIH patients have impaired ability to suppress the proliferation of CD8pos 38 and CD4posCD25neg 39,42 cell populations compared to HS. CD4posCD25pos Tregs from AIH patients are also ineffective suppressors of IFNc production by CD8 Tcells38. Additionally, Tregs fromAIH patients, but not HS, effectively enhance the activation of proinflammatory monocytes by increasing the level of spontaneous migration, the production of TNFα, and the expression of TLR4.43 Magnetically isolated CD4posCD25posCD127neg Tregs from AIH patients were also less able to suppress proliferation in AIH compared to HS,42 although this defect was not observed in cytofluorimetrically isolated CD4posCD25highCD127neg cells.41 Tregs from AIH patients have been shown to express lower levels of galectin-9, and this defect is mirrored by reduced expression of the galectin-9 ligand, Tcell immunoglobulin, and mucin domain-3 (TIM-3) by CD4posCD25neg cells, suggesting that AIH may also be associated with effector cell resistance to Treg control.42
Diagnosis
The diagnosis of AIH is based on the presence of elevated transaminase and IgG levels, positivity for circulating autoantibodies, and a picture of interface hepatitis on histology. The criteria for the diagnosis of AIH have been established and revised by IAIHG.7,8 This diagnostic system, which includes positive and negative scores, grades clinical, laboratory, and histological features of AIH, including response to treatment. Initially, the scoring system was devised mainly for research purposes. However, it also proved to be clinically useful in assessing patients with few or atypical features of the disease.44,45 In the IAIHG scoring system, differences between a definite and probable diagnosis of AIH relate mainly to the degree of serum gamma-globulin or IgG elevation, levels of ANA, SMA, or anti-LKM-1 and exposure to alcohol, medications, or infections that can cause liver injury. Cholestatic laboratory and histological changes carry a negative score. In rare cases, the presence of autoantibodies to asialoglycoprotein receptor (anti-ASGPR), LC-1, soluble liver antigen/liver pancreas (anti-SLA/LP), and atypical perinuclear anti-neutrophil cytoplasmic antibodies supports a probable diagnosis of AIH in the absence of conventional autoantibodies. Response to steroids strengthens the diagnosis of AIH and has been incorporated into the scoring system. A definite diagnosis before steroid treatment requires a score higher than 15, while a definite diagnosis after steroid treatment requires a score greater than 17 (Table 1).
Table 1. International autoimmune hepatitis group revised diagnostic scoring system.
| Parameter | Feature | Score |
|---|---|---|
| Sex | Female | +2 |
| ALP: AST (or ALT) ratio | >3 | −2 |
| 1.5-3 | 0 | |
| 1.5 | 2 | |
| Serum globulins or IgG (times above normal) | >2.0 | +3 |
| 1.5-2.0 | +2 | |
| 1.0-1.5 | +1 | |
| <1.0 | 0 | |
| ANA, SMA or anti-LKM-1 titers | >1:80 | +3 |
| 1:80 | +2 | |
| 1:40 | +1 | |
| <1:40 | 0 | |
| AMA | Positive | −4 |
| Viral markers of active infection | Positive | −3 |
| Negative | +3 | |
| Hepatotoxic drug history | Yes | −4 |
| No | +2 | |
| Average alcohol | <25g/day | +2 |
| >60g/day | −2 | |
| Histological features | Interface hepatitis | +3 |
| Plasma cells | +1 | |
| Rosettes | +1 | |
| None of the above | −5 | |
| Biliary changesa | −3 | |
| Atypical changesb | −3 | |
| Immune diseases | Thyroiditis, colitis, other | +2 |
| HLA | DR3 or DR4 | +1 |
| Seropositivity for other autoantibodies | Anti-SLA/LP, actin, ASGPR, pANNA | +2 |
| Response to therapy | Remission | +2 |
| Relapse | +3 |
Pre-treatment score >15: definite AIH; 10–15: probable AIH; Post-treatment score >17: definite AIH; 12–17: probable AIH.
ALP, alkaline phosphatase; AST, aspartate aminotransferase; ALT, alanine aminotransferase; IgG, immunoglobulin G; ANA, anti-nuclear antibody; SMA, smooth muscle antibody; anti-LKM-1, anti-liver kidney microsomal type 1 antibodies; AMA, anti-mitochondrial antibodies; SLA/LP, soluble liver antigen/liver pancreas; ASGPR, asialoglycoprotein receptor; p-ANNA, peripheral anti-nuclear neutrophil antibody (also known as atypical pANCA); HLA, human leukocyte antigen.
Including granulomatous cholangitis concentric periductal fibrosis ductopenia marginal bile duct proliferation and cholangiolitis
Any other prominent feature suggesting a different aetiology.
Adapted from Alvarez F. et al. 8
The diagnositic criteria for children are slightly different from those of adults. In view of the fact that healthy children are very rarely positive for autoantibodies, titers as low as 1:20 for ANA and SMA and 1:10 for anti-LKM-1 are compatible with the diagnoses of AIH-1 and AIH-2, respectively. 46
Recently, a simplified scoring system has been proposed by the IAIHG.9 This system, intended to be used in the clinical practice, assesses only four criteria: autoantibodies, IgG, histology, and exclusion of viral hepatitis (Table 2).
Table 2. Simplified criteria for the diagnosis of autoimmune hepatitis.
| Variable | Cutoff | Points |
|---|---|---|
| ANA or SMA | ≥1:40 | 1 |
| ANA or SMA | ≥180 | 2a |
| Or anti-LKM-1 | ≥140 | |
| Or SLA | Positive | |
| IgG | >upper limite of normal | 1 |
| >1.10 times upper limit of normal | 2 | |
| Liver histology | Compatible with AIH | 1 |
| Typical of AIH | 2 | |
| Absence of viral hepatitis | Yes | 2 |
Score ≥6: probable AIH ≥7 definite AIH.
ANA, anti-nuclear antibody; SMA, anti-smooth muscle antibody; anti-LKM-1, anti-liver kidney microsomal antibody type 1; SLA, soluble liver antigen; IgG, immunoglobulin G; AIH, autoimmune hepatitis.
Addition of points achieved for all autoantibodies cannot exceed a maximum of 2 points.
Adapted from Hennes E.M. et al. 9
Laboratory abnormalities
AIH is characterized by elevated levels of transaminases. In general, the increase in aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels is much more striking than that of bilirubin and alkaline phosphatase (AP) levels. Nonetheless, in some patients cholestasis is present; in these cases, extra-hepatic obstruction, cholestatic forms of viral hepatitis, drug-induced disease, PBC, primary sclerosing cholangitis (PSC), and overlap syndromes must be taken into consideration.47
Another laboratory feature typical of AIH, albeit not always present, is a generalized elevation of serum globulins and particularly gamma globulins mainly due to an increase in the IgG fraction.48 The serum autoantibodies typically present include: ANA, SMA, anti-LKM-1, and anti-LC-1. Anti-mitochondrial antibodies (AMA), typically present in PBC, are occasionally present in patients with AIH.49 Since autoantibodies may also be found in other liver diseases, their presence as such is not diagnostic of AIH.
Diagnostic autoantibodies
Anti-nuclear antibodies
ANA, the first AIH-associated autoantibody,2 is readily detectable and gives a nuclear staining in the kidney, stomach, and liver sections. In most cases, its pattern, especially in the liver, is homogeneous, although a coarsely or finely speckled pattern is observed less frequently.50
Human epithelial 2 (Hep2) cells, laryngeal tumor cells characterized by prominent nuclei, should be used for a clearer definition of the nuclear pattern. However, they should not be used for screening purposes because of a high positivity rate in adult and pediatric healthy populations.51,52 In AIH, the target antigens of ANA are heterogeneous and not completely defined. ANA have been found to be reactive with single- and double-stranded deoxyribonucleic acid (DNA), small nuclear ribonucleoproteins (sn-RNPs), centromeres, histones, chromatin, and cyclin A.53–55 The advent of new techniques using recombinant nuclear antigens and immunoassays will hopefully lead to a better definition of the target antigens of ANA, of their specificity for diagnosis, and of their possible role in the pathogenesis of AIH-1.56
ANA are present not only in other autoimmune disorders, such as systemic lupus erythematosus (SLE), Sjögren syndrome and systemic sclerosis,57 but also in patients with viral hepatitis, drug-induced hepatitis, and alcoholic and nonalcoholic fatty liver disease.58,59 Thus, although ANA are considered diagnostic markers for AIH, they are not specific for AIH.
Anti-smooth muscle antibodies
SMA antibodies are detected in kidney, stomach, and liver sections, where they stain the smooth muscle contained in the wall of the arteries. In the stomach, they also stain the muscularis mucosa and the lamina propria. On the renal substrate, it is possible to visualize the vessels (V), glomeruli (G), and tubules (T) patterns.60 The VG and VGT patterns are more specific for AIH than the V pattern. The VGT pattern corresponds to the F-actin or microfilament (MF) pattern observed when cultured fibroblasts are used as substrate.61 Neither the VGT nor the antiMF patterns are, however, entirely specific for AIH. SMA are directed against components of the cytoskeleton, such as actin and non-actin components, including tubulin, vimentin, desmin, and skeletin. 58 Like ANA, SMA are not specific for AIH, since their presence has also been reported in advanced liver disease of other etiologies, infectious diseases, and rheumatic disorders. 62
Anti-Liver-kidney-microsomal type 1 antibodies
Anti-LKM-1 antibodies, the hallmark of AIH-2, stain the hepatocellular cytoplasm and the P3 portion of the renal tubules. Some confusion can occur between the immunofluorescence patterns of anti-LKM-1 and AMA because both autoantibodies stain the liver as well as the kidney.56 However, AMA stain the liver more faintly than anti-LKM-1 and mark the renal tubules more diffusely, while accentuating the distal tubules. Importantly, AMA stain gastric parietal cells while anti-KM-1 do not.63
The identification of the molecular targets of anti-LKM-1 (cytochrome P450 2D6 (CYP2D6)) and AMA (enzymes of the 2-oxo-acid dehydrogenase complexes), have led to the establishment of immune-assays based on the use of recombinant or purified antigens. Commercially available enzymelinked immunosorbent assays (ELISAs) are accurate for detection of anti-LKM-1, at least in the context of AIH-2, and for the detection of AMA. Thus, when a pattern remains difficult to interpret by immunofluorescence, the use of molecularly based immune-assays may be of help.46 Anti-LKM-1 titer is clinically relevant if equal or higher than 1/40 in adult patients and 1/10 in subjects up to the age of 18 years.64 Intriguingly, anti-LKM-1 are also present in up to 10% of patients with chronic hepatitis C virus (HCV) infection, and their titer has been found to be associated with disease activity.65
Anti-liver cytosol type 1 antibodies
Anti-LC-1 was originally described, both in combination with anti-LKM-1 and in isolation, to define a clinical entity resembling AIH-2.66 Later, anti-LC-1 was also infrequently found in association with the serological markers of AIH-167 and in patients with chronic hepatitis C virus infection.68 The molecular target has been identified as the formiminotransferase cyclodeaminase, an enzyme involved in folate metabolism and most highly expressed in the liver.69 The presence and titer of anti-LC-1 antibodies correlate with disease activity and represent a potentially useful marker of residual hepatocellular inflammation in AIH.70 The presence of anti-LC-1 in isolation scores positively towards a diagnosis of AIH-2, allowing prompt initiation of treatment.71
Anti-soluble liver antigen/liver-pancreas antigen antibodies
Anti-SLA and anti-LP, originally described as individual antibodies, share the same antigenic target and have been subsequently identified as the same autoantibody.72 The presence of anti-SLA/LP in the absence of conventional antibodies, has led to the proposal of a third type of AIH (AIH-3).73 However, early reports used a cut-off point for levels of conventional autoantibodies higher than those currently recommended for the diagnosis of AIH; therefore, the notion of AIH-3 has not been endorsed by the IAIHG. Anti-SLA/LP is highly specific for the diagnosis of AIH, and its detection at the time of presentation identifies patients with more severe disease and a worse outcome.74 Screening of cDNA expression libraries identified a UGA tRNA suppressorassociated antigenic protein (tRNP(ser)sec), more precisely Ophosphoseryl- tRNA: selecysteinil-tRNA synthase (SepSecS), as the anti-SLA target.75
Anti-neutrophil cytoplasmic antibodies
ANCA react to cytoplasmic components of neutrophils, giving a perinuclear (p-ANCA) or cytoplasmic (c-ANCA) pattern.71,76 c-ANCA mainly react with proteinase 3 and is found in Wegener granulomatosis; whereas p-ANCA react with myeloperoxidase and is frequently detected in microscopic polyangiitis. The p-ANCA detected in AIH-1, as well as those in PSC and inflammatory bowel disease (IBD), have an atypical staining pattern, being associated with peripheral nuclear membrane components, hence the name of peripheral anti-nuclear neutrophil antibody (p-ANNA).77 In contrast to AIH-1, p-ANNA is virtually absent in AIH-2. Detection of p- ANNA can aid the diagnosis of AIH, particularly in the absence of other autoantibodies.64
Anti-asialoglycoprotein receptor antibodies
Attempts to identify putative auto-antigens specifically expressed on the hepatocyte surface in AIH have led to the description of a crude liver extract preparation known as the liver specific protein (LSP) and its major component the ASGPR.78 ASGPR, also designated as hepatic lectin, is a type II transmembrane glycoprotein. It is the only known liverspecific auto-antigen and is constitutively expressed on the hepatocellular membrane. Antibodies to ASGPR are observed in 88% of all patients with AIH and co-exist with ANA, SMA, or anti-LKM-1.58 However, they are not disease specific, as they can also be found in viral hepatitis, drug-induced hepatitis, and PBC.79 In AIH, the levels of anti-ASGPR correlate with inflammatory disease activity and may be used as an additional marker to monitor treatment efficacy.80
Histology
Since transaminases and IgG levels do not reflect the extent of histological inflammatory activity or the presence or absence of cirrhosis, liver biopsy is mandatory; not only to confirm the diagnosis but also to evaluate the severity of liver damage.
Hepatitis at the portal-parenchymal interface, known as interface hepatitis (Fig. 2), is typical, but is not exclusively observed in AIH.81 This picture is characterized by a lymphoplasmacytic infiltrate crossing the limiting plate and invading the liver parenchyma. Lymphocytes, plasma cells, and histiocytes surround individual dying hepatocytes at the portal-parenchymal interface and in the lobule. Though plasma cells are usually abundant at the interface and throughout the lobule, their presence in low number does not exclude the diagnosis of AIH.71 Other lesions that may be present include hepatocyte swelling and pycnotic necrosis. Fibrosis is present in all but the mildest forms of the disease. In contrast to patients with an insidious course, those presenting with acute liver failure show tissue damage predominattly in the centrilobular area.82 However, many patients presenting with fulminant hepatic failure tend to have massive necrosis and multilobular collapse; importantly, they have less fibrosis than those presenting with a more insidious course.83
Fig. 2. Histology of autoimmune hepatitis.
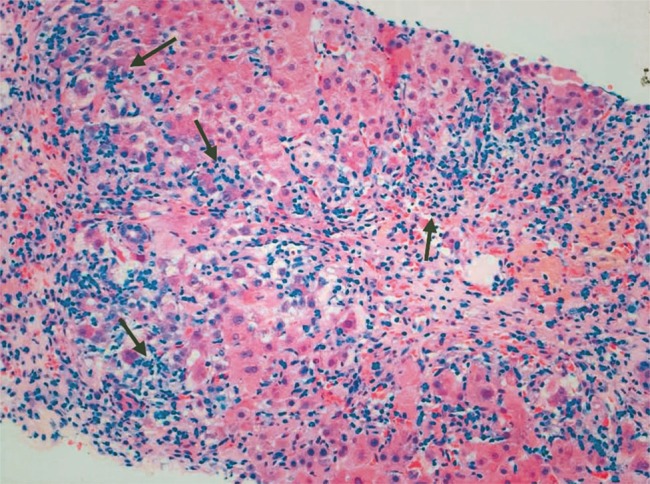
The portal and periportal inflammatory infiltrate characteristic of autoimmune hepatitis is composed of lymphocytes, monocytes/macrophages, and plasma cells (interface hepatitis, arrows). Hematoxylin & eosin staining (Picture kindly provided by Dr. Alberto Quaglia, Institute of Liver Studies, King’s College Hospital).
Despite the fact that sampling variation may occur in needle biopsy specimens, especially in the presence of cirrhosis, the severity of the histological appearance is usually of prognostic value. However, even patients with cirrhosis at presentation respond well to immunosuppressive treatment. 84
Although the characteristic portal-parenchymal lesion usually spares the biliary tree, a small proportion of patients may show inflammatory changes surrounding the bile ducts, suggesting the presence of an overlap with sclerosing cholangitis, which occurs more frequently in the pediatric setting.85
Treatment
Standard treatment
In the early 70s, three randomized clinical trials in adults with AIH provided the basis for current immunosuppressive regimens, collectively suggesting that treatment with prednisolone improves liver function tests, ameliorates symptoms, and prolongs survival.3–5 Although azathioprine did not induce remission when used on its own, it did allow for the maintenance of remission in association with a significantly reduced dose of steroids.86 Initial treatment with prednisone (or prednisolone) with or without azathioprine should be instituted as soon as the diagnosis is made (Table 3), not delayed for 6 months as suggested in the early studies.87
Table 3. Immunosuppressive treatment regimens for adults and children with autoimmune hepatitis.
| Population | Initial regimen | Maintenance |
|---|---|---|
| Adults | Prednis(ol)one 60 mg/day Or Prednis(ol)one 30–60 mg/day in combination with azathioprine 1–2 mg/kg/day |
Prednis(ol)one 10 mg/week reduction until 20 mg/day, followed by of 5 mg/week reduction until 10 mg/day and by 2.5 mg/week reduction to reach maintenance (5 mg/day) Azathioprine 1–2 mg/kg/day if in combination with prednis(ol)one or 2 mg/kg/day if alone |
| Children | Prednis(ol)one 2 mg/kg/daily (up to 60 mg/daily) decreased weekly if transaminase levels decrease. Azathioprine (1–2 mg/kg/day) added if transaminase levels plateau or increase. In the absence of jaundice, azathioprine can be started at the say time as prednisolone |
Prednis(ol)one tapered over 6–8 weeks to 0.1–0.2 mg/kg/day or 5 mg/day Azathioprine 1–2 mg/kg/day if needed or added initially |
The initial approach to therapy depends upon the histologic findings.83 Transaminase and IgG levels do not always correlate with histological damage and consequently provide limited help in respect to treatment initiation. Prompt treatment is indicated in patients with aggressive disease, usually children or young adults, and in any patient with evidence of interface hepatitis, with or without fibrosis or cirrhosis.21 In older patients with isolated portal inflammation (without interface hepatitis), institution of therapy is guided by ASTand IgG levels and/or by the presence of symptoms.47 The therapeutic approach in patients with a milder form of the disease – those who may be asymptomatic or paucisymptomatic and are detected incidentally after discovery of abnormal liver function tests – is less clear.88 In these cases, the benefit of therapy is undefined and may be so low that the risk of corticosteroid side effects might outweigh its possible benefits; this is particularly relevant when starting therapy in post-menopausal women and elderly patients.22
Although some patients may remain in remission after drug treatment is withdrawn, most require long-term maintenance therapy. Despite the absence of firm guidelines, caution must be used when attempting to withdrawal immunosuppression within 2 years of diagnosis.21 During withdrawal attempts, it is essential to closely monitor liver function tests, as relapse may be severe and even fatal. Patients who have successfully stopped immunosuppression should undergo long-term follow-up, as relapse can occur even 10 years later.88
Alternative and new treatments
In the group of patients that show failure to standard therapy and intolerance or low compliance to standard immunosuppression, alternative immunosuppressive treatments have been proposed.89 Decisions regarding the use of such regimens have to be based, however, on the basis of small series or case reports.
Mycophenolate mofetil (MMF) is a purine antagonist that selectively inhibits proliferation of activated lymphocytes.90 It has been reported to be effective in AIH patients intolerant to azathioprine.88 Therefore, in patients for whom standard immunosuppression fails to induce stable remission or who are intolerant to azathioprine, MMF, together with prednisolone, is currently the treatment of choice.21
Calcineurin inhibitors, cyclosporine and tacrolimus, have been used as a rescue treatment for difficult-to-treat cases of AIH. As no large study in this subgroup of patients has been published, these drugs should be used with caution.88
Anti-TNF-α agents, such as infliximab, are commonly used to treat immune-mediated diseases such as rheumatoid arthritis, psoriasis, and IBD. There is anecdotal evidence that inflixmab is efficacious in the management of difficult-to-treat cases of AIH.91 In the largest published retrospective series, treatment with infliximab led to a decrease in transaminase and IgG levels in 11 difficult-to-treat adult patients with AIH, although infectious complications occurred in seven of them.91 Moreover, and worryingly, infliximab therapy for other diseases has been associated with the induction of severe de novo AIH.92 Anecdotal evidence also suggestedsome benefit with the use of the anti B cell monoclonal antibody rituximab in difficult-to-treat patients.93 However, the occurrence of severe infections is an important risk-factor associated with these biological treatments.
Budesonide is a corticosteroid with very high affinity for the glucorticoid receptor and high first pass liver metabolism; hence, it is presently receiving considerable attention as an alternative to prednisone or prednisolone as primary treatment of AIH. Although initial reports were somewhat contradictory, a recent large European study found that a combination of budesonide and azathioprine induced remission in 60% of non-cirrhotic patients, while medium-dose standard steroids and azathioprine only induced remission in 39% of patients. The budesonide group had also fewer adverse effects.94 It should be noted, however, that this reported rate of remission was much lower than that seen in both adults and children (∼80%) when a higher starting dose of prednisone was used. Moreover, because budesonide cannot be used in cirrhotic patients, representing at least a third of the AIH population, its clinical utility has limitations.95
Liver transplantation
AIH accounts for 2–3% of pediatric and 4–6% of adult liver transplants (LT) performed in Europe and the United States.96 LT is indicated for AIH patients with acute liver failure who do not respond to immunosuppressive treatment, present with end-stage chronic liver disease, and have hepatocellular carcinoma that meets the transplant criteria.97,98 Although patients with a chronic presentation of AIH typically respond well to immunosuppressive treatment, approximately 10% will eventually require LT. Patients who fail to reach remission after 4 years of therapy are the most common candidates for LT.99 The indications for LT for end-stage chronic AIH are similar to those for PBC and other end-stage liver diseases. 100,101
AIH can present at times with acute or even fulminant liver failure, requiring urgent LT.102 The management of AIH patients with acute/fulminant hepatic failure is a therapeutic challenge, as experience is scarce and based on small retrospective studies. It is estimated that 8.7-19.8% of patients with AIH may have this form of presentation.102–106 According to published studies, the vast majority of them require LT, although one-third may respond to corticosteroids. Factors associated with a greater likelihood of responding to corticosteroids are: Model for End-Stage Liver Disease (MELD) at admission ≤28, absence of massive necrosis on histology, and stabilization or improvement of bilirubin levels and INR during the first 4 days of treatment. If there is no clinical or biochemichal improvement during this time frame, continued therapy with corticosteroids may be a futile exercise, as it is unlikely to change the course of the disease and may facilitate serious complications, particularly sepsis. If therapy with corticosteroids is maintained in these patients, it is imperative to pursue simultaneously assessment for LT.101
Though recurrence of AIH has been reported in between 20% and 30% of transplanted patients,101,107 a combination of prednisolone and a calcineurin inhibitor, the recommended immunosuppressive regimen after LT for AIH,107 leads to a very successful outcome with reported 5 and 10 year patient survivals of 80–90 and 75%,83 respectively, and 1 and 5 year graft survivals of 84 and 75%, respectively.83,108
Conclusions
The diagnosis of AIH should be considered during the diagnostic workup of any patient with increased liver enzyme levels. AIH is exquisitely responsive to immunosuppressive treatment, with symptom free long-term survival for the majority of patients. For patients who do not respond to standard treatment, or who are difficult-to-treat, MMF and, in the absence of a response, calcineurin inhibitors should be tried in addition to steroids. Persistent failure to respond or lack of adherence to treatment result in end-stage liver disease. These patients, and those with fulminant liver failure (encephalopathy grade II-IV) at diagnosis, will require liver transplantation. The pathogenesis of AIH is not fully understood, although there is increasing evidence that genetic susceptibility, molecular mimicry and impaired immunoregulatory networks contribute to the initiation and perpetuation of the autoimmune attack. Liver damage is thought to be mediated primarily by CD4 T cells, although recent studies support the involvement of diverse populations, including Th17 cells. Current studies are paving the way for the development of novel treatments aimed at reconstituting self-tolerance by specific immunologic maneuvers, such as adoptive transfer of autologous antigen-specific Tregs.
Abbreviations
- AIH
autoimmune hepatitis
- ALT
alanine aminotransferase
- AMA
antimitochondrial antibodies
- ANA
antinuclear antibody
- ANCA
antineutrophil cytoplasmic antibodies
- anti-ASGPR
autoantibodies to asialoglycoprotein receptor
- antiLC1
antiliver cytosol type 1 antibody
- antiLKM1
antiliver kidney microsomal type 1 antibody
- AP
alkaline phosphatase
- APC
antigen presenting cell
- AST
aspartate aminotransferase
- cANCA
cytoplasmic antineutrophil cytoplasmic antibodies
- CCL
chemokine ligand
- CTL
cytotoxic T lymphocytes
- CYP2D6
cytochrome P450 2D6
- DNA
deoxyribonucleic acid
- ELISAs
enzymelinked immunosorbent assays
- FOXP3
forkhead box P3
- HCV
hepatitis C virus
- Hep2
human epithelial 2
- HLA
human leukocyte antigen
- HS
healthy subjects
- IAIHG
international autoimmune hepatitis group
- IBD
inflammatory bowel disease
- IFN
interferon
- IgG
immunoglobulin G
- IL
interleukin
- LKM1
liverkidney microsomal type 1
- LSP
liver specific protein
- LT
liver transplant
- MELD
model for endstage liver disease
- MF
microfilament
- MMF
mycophenolate mofetil
- pANCA
perinuclear antineutrophil cytoplasmic antibodies
- PBC
primary biliary cirrhosis
- PSC
primary sclerosing cholangitis
- SLALP
soluble liver antigenliver pancreas
- SLE
systemic lupus erythematosus
- SMA
smooth muscle antibody
- snRNPs
small nuclear ribonucleoproteins
- TGF
transforming growth factor
- Th
Thelper cell
- TIM3
T cell immunoglobulin and mucin domain3
- TNF
tumor necrosis factor
- Tregs
regulatory T cells
References
- 1.Waldenstrm J. Leber Blutprotein und Nahrungseiweiss. Deutsch Z Verdau Stoffwechselkr. 1950;15:113–119. [PubMed] [Google Scholar]
- 2.Mackay IR, Cowling DC, Taft LI. Lupoid hepatitis. Lancet. 1956;271:1323–1326. doi: 10.1016/s0140-6736(56)91483-0. 10.1016/S01406736(56)914830. [DOI] [PubMed] [Google Scholar]
- 3.Cook GC, Mulligan R, Sherlock S. Controlled prospective trial of corticosteroid therapy in active chronic hepatitis. QJMed. 1971;40:159–185. doi: 10.1093/oxfordjournals.qjmed.a067264. 10.1093/oxfordjournals.qjmed.a067264. [DOI] [PubMed] [Google Scholar]
- 4.Soloway RD, Summerskill WH, Baggenstoss AH, Geall MG, Gitnik GL, Elveback IR, et al. Clinical, biochemical, and histological remission of severe chronic active liver disease: a controlled study of treatments and early prognosis. Gastroenterology. 1972;63:820–833. [PubMed] [Google Scholar]
- 5.MurrayLyon IM, Stern RB, Williams R. Controlled trial of prednisone and azathioprine in active chronic hepatitis. Lancet. 1973;1:735–737. doi: 10.1016/s0140-6736(73)92125-9. 10.1016/S01406736(73)921259. [DOI] [PubMed] [Google Scholar]
- 6.Mackay IR, Weiden S, Hasker J. Autoimmune hepatitis. Ann N Y Acad Sci. 1965;124:767–780. doi: 10.1111/j.1749-6632.1965.tb19000.x. 10.1111/j.17496632.1965.tb19000.x. [DOI] [PubMed] [Google Scholar]
- 7.Johnson PJ, McFarlane IG. Meeting report: International Autoimmune Hepatitis Group. Hepatology. 1993;18:998–1005. doi: 10.1002/hep.1840180435. 10.1002/hep.1840180435. [DOI] [PubMed] [Google Scholar]
- 8.Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;31:929–938. doi: 10.1016/s0168-8278(99)80297-9. 10.1016/S01688278(99)802979. [DOI] [PubMed] [Google Scholar]
- 9.Hennes EM, Zeniya M, Czaja AJ, Parés A, Dalekos GN, Krawitt EL, et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008;48:169–176. doi: 10.1002/hep.22322. 10.1002/hep.22322. [DOI] [PubMed] [Google Scholar]
- 10.Liberal R, Longhi MS, MieliVergani G, Vergani D. Pathogenesis of autoimmune hepatitis. Best Pract Res Clin Gastroenterol. 2011;25:653–664. doi: 10.1016/j.bpg.2011.09.009. 10.1016/j.bpg.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Boberg KM, Aadland E, Jahnsen J, Raknerud N, Stiris M, Bell H. Incidence and prevalence of primary biliary cirrhosis, primary sclerosing cholangitis, and autoimmune hepatitis in a Norwegian population. Scand J Gastroenterol. 1998;33:99–103. doi: 10.1080/00365529850166284. [DOI] [PubMed] [Google Scholar]
- 12.Primo J, Merino C, Fernandez J, Molés JR, Llorca P, Hinojosa J. [Incidence and prevalence of autoimmune hepatitis in the area of the Hospital de Sagunto (Spain)] Gastroenterol Hepatol. 2004;27:239–243. doi: 10.1016/s0210-5705(03)70452-x. 10.1016/S02105705(03)70452X. [DOI] [PubMed] [Google Scholar]
- 13.Hurlburt KJ, McMahon BJ, Deubner H, HsuTrawinski BJ, Williams JL, Kowdley KV. Prevalence of autoimmune liver disease in Alaska Natives. Am J Gastroenterol. 2002;97:2402–2407. doi: 10.1111/j.1572-0241.2002.06019.x. 10.1111/j.15720241.2002.06019.x. [DOI] [PubMed] [Google Scholar]
- 14.Whalley S, Puvanachandra P, Desai A, Kennedy H. Hepatology outpatient service provision in secondary care a study of liver disease incidence and resource costs. Clin Med. 2007;7:119–124. doi: 10.7861/clinmedicine.7-2-119. 10.7861/clinmedicine.72119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ngu JH, Bechly K, Chapman BA, Burt MJ, Barclay ML, Gearry RB, et al. Population-based epidemiology study of autoimmune hepatitis: a disease of older women? J Gastroenterol Hepatol. 2010;25:1681–1686. doi: 10.1111/j.1440-1746.2010.06384.x. 10.1111/j.14401746.2010.06384.x. [DOI] [PubMed] [Google Scholar]
- 16.Nishioka M, Morshed SA, McFarlane IG. Geographical variation in the frequency and characteristics of autoimmune liver diseases. In: Krawitt EL, Wiesner RH, Nishioka M, editors. Autoimmune liver diseases. 2nd ed. Amesterdam: Elsevier; 1998. pp. 413–424. [Google Scholar]
- 17.Toda G, Zeniya M, Watanabe F, Imawari M, Kiyosawa K, Nishioka M, et al. Present status of autoimmune hepatitis in Japan–correlating the characteristics with international criteria in an area with a high rate of HCV infection. Japanese National Study Group of Autoimmune Hepatitis. J Hepatol. 1997;26:1207–1212. doi: 10.1016/s0168-8278(97)80453-9. 10.1016/S01688278(97)804539. [DOI] [PubMed] [Google Scholar]
- 18.Lam KC, Lai CL, Wu PC, Todd D. Etiological spectrum of liver cirrhosis in the Chinese. J Chronic Dis. 1980;33:375–381. doi: 10.1016/0021-9681(80)90047-8. 10.1016/00219681(80)900478. [DOI] [PubMed] [Google Scholar]
- 19.Qiu D, Wang Q, Wang H, Xie Q, Zang G, Jiang H, et al. Validation of the simplified criteria for diagnosis of autoimmune hepatitis in Chinese patients. J Hepatol. 2011;54:340–347. doi: 10.1016/j.jhep.2010.06.032. 10.1016/j.jhep.2010.06.032. [DOI] [PubMed] [Google Scholar]
- 20.Vergani D, MieliVergani G. Rodes J, Benhamou JP, Dufour JF. Textbook of hepatology from basic science to clinical practicde. 3rd ed. London: Blackwell publishing; 2007. Autoimmune hepatitis; pp. 1089–1101. [Google Scholar]
- 21.Manns MP, Czaja AJ, Gorham JD, Krawitt EL, MieliVergani G, Vergani D, et al. Diagnosis and management of autoimmune hepatitis. Hepatology. 2010;51:2193–2213. doi: 10.1002/hep.23584. 10.1002/hep.23584. [DOI] [PubMed] [Google Scholar]
- 22.AlChalabi T, Boccato S, Portmann BC, McFarlane IG, Heneghan MA. Autoimmune hepatitis (AIH) in the elderly: a systematic retrospective analysis of a large group of consecutive patients with definite AIH followed at a tertiary referral centre. J Hepatol. 2006;45:575–583. doi: 10.1016/j.jhep.2006.04.007. 10.1016/j.jhep.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 23.Czaja AJ, Carpenter HA. Distinctive clinical phenotype and treatment outcome of type 1 autoimmune hepatitis in the elderly. Hepatology. 2006;43:532–538. doi: 10.1002/hep.21074. 10.1002/hep.21074. [DOI] [PubMed] [Google Scholar]
- 24.de Boer YS, van Gerven NM, Zwiers A, Verwer BJ, van Hoek B, van Erpecum KJ, et al. Genomewide Association Study Identifies Variants Associated with Autoimmune Hepatitis Type1. Gastroenterology. 2014;147:443–452.e5. doi: 10.1053/j.gastro.2014.04.022. 10.1053/j.gastro.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 25.DjilaliSaiah I, Fakhfakh A, Louafi H, CaillatZucman S, Debray D, Alvarez F. HLA class II influences humoral autoimmunity in patients with type 2 autoimmune hepatitis. J Hepatol. 2006;45:844–850. doi: 10.1016/j.jhep.2006.07.034. 10.1016/j.jhep.2006.07.034. [DOI] [PubMed] [Google Scholar]
- 26.Agarwal K, Czaja AJ, Jones DE, Donaldson PT. Cytotoxic T lymphocyte antigen4 CTLA4 gene polymorphisms and susceptibility to type 1 autoimmune hepatitis. Hepatology. 2000;31:49–53. doi: 10.1002/hep.510310110. 10.1002/hep.510310110. [DOI] [PubMed] [Google Scholar]
- 27.Cookson S, Constantini PK, Clare M, Underhill JA, Bernal W, Czaja AJ, et al. Frequency and nature of cytokine gene polymorphisms in type 1 autoimmune hepatitis. Hepatology. 1999;30:851–856. doi: 10.1002/hep.510300412. 10.1002/hep.510300412. [DOI] [PubMed] [Google Scholar]
- 28.Agarwal K, Czaja AJ, Donaldson PT. A functional Fas promoter polymorphism is associated with a severe phenotype in type 1 autoimmune hepatitis characterized by early development of cirrhosis. Tissue Antigens. 2007;69:227–235. doi: 10.1111/j.1399-0039.2006.00794.x. 10.1111/j.13990039.2006.00794.x. [DOI] [PubMed] [Google Scholar]
- 29.Senaldi G, Portmann B, Mowat AP, MieliVergani G, Vergani D. Immunohistochemical features of the portal tract mononuclear cell infiltrate in chronic aggressive hepatitis. Arch Dis Child. 1992;67:1447–1453. doi: 10.1136/adc.67.12.1447. 10.1136/adc.67.12.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LoboYeo A, Senaldi G, Portmann B, Mowat AP, MieliVergani G, Vergani D. Class I and class II major histocompatibility complex antigen expression on hepatocytes a study in children with liver disease. Hepatology. 1990;12:224–232. doi: 10.1002/hep.1840120208. 10.1002/hep.1840120208. [DOI] [PubMed] [Google Scholar]
- 31.Senaldi G, LoboYeo A, Mowat AP, MieliVergani G, Vergani D. Class I and class II major histocompatibility complex antigens on hepatocytes importance of the method of detection and expression in histologically normal and diseased livers. J Clin Pathol. 1991;44:107–114. doi: 10.1136/jcp.44.2.107. 10.1136/jcp.44.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bettelli E, Carrier Y, Gao W, Korn T, Strom TB, Oukka M, et al. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 2006;441:235–238. doi: 10.1038/nature04753. 10.1038/nature04753. [DOI] [PubMed] [Google Scholar]
- 33.Miossec P, Korn T, Kuchroo VK. Interleukin-17 and type 17 helper T cells. N Engl J Med. 2009;361:888–898. doi: 10.1056/NEJMra0707449. 10.1056/NEJMra0707449. [DOI] [PubMed] [Google Scholar]
- 34.Harada K, Shimoda S, Sato Y, Isse K, Ikeda H, Nakanuma Y. Periductal interleukin-17 production in association with biliary innate immunity contributes to the pathogenesis of cholangiopathy in primary biliary cirrhosis. Clin Exp Immunol. 2009;157:261–270. doi: 10.1111/j.1365-2249.2009.03947.x. 10.1111/j.13652249.2009.03947.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhao L, Tang Y, You Z, Wang Q, Liang S, Han X, et al. Interleukin-17 contributes to the pathogenesis of autoimmune hepatitis through inducing hepatic interleukin6 expression. PLoS One. 2011;6:e18909. doi: 10.1371/journal.pone.0018909. 10.1371/journal.pone.0018909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Longhi MS, Ma Y, MieliVergani G, Vergani D. Aetiopathogenesis of autoimmune hepatitis. JAutoimmun. 2010;34:7–14. doi: 10.1016/j.jaut.2009.08.010. 10.1016/j.jaut.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 37.Longhi MS, Ma Y, Bogdanos DP, Cheeseman P, MieliVergani G, Vergani D. Impairment of CD4(+)CD25(+) regulatory T-cells in autoimmune liver disease. J Hepatol. 2004;41:31–37. doi: 10.1016/j.jhep.2004.03.008. 10.1016/j.jhep.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 38.Longhi MS, Ma Y, Mitry RR, Bogdanos DP, Heneghan M, Cheeseman P, et al. Effect of CD4+ CD25+ regulatory T-cells on CD8 T-cell function in patients with autoimmune hepatitis. J Autoimmun. 2005;25:63–71. doi: 10.1016/j.jaut.2005.05.001. 10.1016/j.jaut.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 39.Ferri S, Longhi MS, De Molo C, Lalanne C, Muratori P, Granito A, et al. A multifaceted imbalance of T cells with regulatory function characterizes type 1 autoimmune hepatitis. Hepatology. 2010;52:999–1007. doi: 10.1002/hep.23792. 10.1002/hep.23792. [DOI] [PubMed] [Google Scholar]
- 40.Longhi MS, Hussain MJ, Mitry RR, Arora SK, MieliVergani G, Vergani D, et al. Functional study of CD4+CD25+ regulatory T cells in health and autoimmune hepatitis. JImmunol. 2006;176:4484–4491. doi: 10.4049/jimmunol.176.7.4484. 10.4049/jimmunol.176.7.4484. [DOI] [PubMed] [Google Scholar]
- 41.Peiseler M, Sebode M, Franke B, Wortmann F, Schwinge D, Quaas A, et al. FOXP3+ regulatory T cells in autoimmune hepatitis are fully functional and not reduced in frequency. J Hepatol. 2012;57:125–132. doi: 10.1016/j.jhep.2012.02.029. 10.1016/j.jhep.2012.02.029. [DOI] [PubMed] [Google Scholar]
- 42.Liberal R, Grant CR, Holder BS, Ma Y, MieliVergani G, Vergani D, et al. The impaired immune regulation of autoimmune hepatitis is linked to a defective galectin-9/tim-3 pathway. Hepatology. 2012;56:677–686. doi: 10.1002/hep.25682. 10.1002/hep.25682. [DOI] [PubMed] [Google Scholar]
- 43.Longhi MS, Mitry RR, Samyn M, Scalori A, Hussain MJ, Quaglia A, et al. Vigorous activation of monocytes in juvenile autoimmune liver disease escapes the control of regulatory T-cells. Hepatology. 2009;50:130–142. doi: 10.1002/hep.22914. 10.1002/hep.22914. [DOI] [PubMed] [Google Scholar]
- 44.Czaja A, Carpenter HA. Validation of scoring system for diagnosis of autoimmune hepatitis. Dig Dis Sci. 1996;41:305–314. doi: 10.1007/BF02093820. 10.1007/BF02093820. [DOI] [PubMed] [Google Scholar]
- 45.Czaja AJ, Manns MP. Advances in the diagnosis pathogenesis and management of autoimmune hepatitis. Gastroenterology. 2010;139:58–72.e4. doi: 10.1053/j.gastro.2010.04.053. 10.1053/j.gastro.2010.04.053. [DOI] [PubMed] [Google Scholar]
- 46.MieliVergani G, Heller S, Jara P, Vergani D, Chang MH, Fujisawa T, et al. Autoimmune hepatitis. J Pediatr Gastroenterol Nutr. 2009;49:158–164. doi: 10.1097/MPG.0b013e3181a1c265. 10.1097/MPG.0b013e3181a1c265. [DOI] [PubMed] [Google Scholar]
- 47.Krawitt EL. Clinical features and management of autoimmune hepatitis. World J Gastroenterol. 2008;14:3301–3305. doi: 10.3748/wjg.14.3301. 10.3748/wjg.14.3301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McFarlane IG. Definition and classification of autoimmune hepatitis. Semin Liver Dis. 2002;22:317–324. doi: 10.1055/s-2002-35702. 10.1055/s200235702. [DOI] [PubMed] [Google Scholar]
- 49.Bhat M, Guindi M, Heathcote EJ, Hirschfield GM. Transient development of anti-mitochondrial antibodies accompanies autoimmune hepatitis-sclerosing cholangitis overlap. Gut. 2009;58:152–153. doi: 10.1136/gut.2008.163220. 10.1136/gut.2008.163220. [DOI] [PubMed] [Google Scholar]
- 50.Czaja AJ, Cassani F, Cataleta M, Valentini P, Bianchi FB. Antinuclear antibodies and patterns of nuclear immunofluorescence in type 1 autoimmune hepatitis. Dig Dis Sci. 1997;42:1688–1696. doi: 10.1023/a:1018809431189. 10.1023/A1018809431189. [DOI] [PubMed] [Google Scholar]
- 51.Tan EM, Feltkamp TE, Smolen JS, Butcher B, Dawkins R, Fritzler MJ, et al. Range of antinuclear antibodies in “healthy” individuals. Arthritis Rheum. 1997;40:1601–1611. doi: 10.1002/art.1780400909. 10.1002/art.1780400909. [DOI] [PubMed] [Google Scholar]
- 52.Hilario MO, Len CA, Roja SC, Terreri MT, Almeida G, Andrade LE. Frequency of antinuclear antibodies in healthy children and adolescents. Clin Pediatr Phila. 2004;43:637–642. doi: 10.1177/000992280404300709. 10.1177/000992280404300709. [DOI] [PubMed] [Google Scholar]
- 53.Burlingame RW, Rubin RL, Rosenberg AM. Autoantibodies to chromatin components in juvenile rheumatoid arthritis. Arthritis Rheum. 1993;36:836–841. doi: 10.1002/art.1780360615. 10.1002/art.1780360615. [DOI] [PubMed] [Google Scholar]
- 54.Czaja AJ, Nishioka M, Morshed SA, Hachiya T. Patterns of nuclear immunofluorescence and reactivities to recombinant nuclear antigens in autoimmune hepatitis. Gastroenterology. 1994;107:200–207. doi: 10.1016/0016-5085(94)90078-7. [DOI] [PubMed] [Google Scholar]
- 55.Strassburg CP, Alex B, Zindy F, Gerken G, Lüttig B, Meyer zum Büschenfelde KH, et al. Identification of cyclin A as a molecular target of antinuclear antibodies (ANA) in hepatic and nonhepatic autoimmune diseases. J Hepatol. 1996;25:859–866. doi: 10.1016/s0168-8278(96)80290-x. 10.1016/S016882789680290X. [DOI] [PubMed] [Google Scholar]
- 56.Bogdanos DP, Invernizzi P, Mackay IR, Vergani D. Autoimmune liver serology: current diagnostic and clinical challenges. World J Gastroenterol. 2008;14:3374–3387. doi: 10.3748/wjg.14.3374. 10.3748/wjg.14.3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tan EM. Antinuclear antibodies: diagnostic markers for autoimmune diseases and probes for cell biology. Adv Immunol. 1989;44:93–151. doi: 10.1016/s0065-2776(08)60641-0. 10.1016/S0065277608606410. [DOI] [PubMed] [Google Scholar]
- 58.Strassburg CP, Manns MP. Autoantibodies and autoantigens in autoimmune hepatitis. Semin Liver Dis. 2002;22:339–352. doi: 10.1055/s-2002-35704. 10.1055/s200235704. [DOI] [PubMed] [Google Scholar]
- 59.Adams LA, Lindor KD, Angulo P. The prevalence of autoantibodies and autoimmune hepatitis in patients with nonalcoholic Fatty liver disease. Am J Gastroenterol. 2004;99:1316–1320. doi: 10.1111/j.1572-0241.2004.30444.x. 10.1111/j.15720241.2004.30444.x. [DOI] [PubMed] [Google Scholar]
- 60.Bottazzo GF, FlorinChristensen A, Fairfax A, Swana G, Doniach D, GroeschelStewart U. Classification of smooth muscle autoantibodies detected by immunofluorescence. J Clin Pathol. 1976;29:403–410. doi: 10.1136/jcp.29.5.403. 10.1136/jcp.29.5.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Muratori P, Muratori L, Agostinelli D, Pappas G, Veronesi L, Granito A, et al. Smooth muscle antibodies and type 1 autoimmune hepatitis. Autoimmunity. 2002;35:497–500. doi: 10.1080/0891693021000054066. 10.1080/0891693021000054066. [DOI] [PubMed] [Google Scholar]
- 62.Manns MP, Vogel A. Autoimmune hepatitis, from mechanisms to therapy. Hepatology. 2006;43:S132–S144. doi: 10.1002/hep.21059. 10.1002/hep.21059. [DOI] [PubMed] [Google Scholar]
- 63.Rizzetto M, Swana G, Doniach D. Microsomal antibodies in active chronic hepatitis and other disorders. Clin Exp Immunol. 1973;15:331–144. [PMC free article] [PubMed] [Google Scholar]
- 64.Vergani D, Alvarez F, Bianchi FB, Canado EL, Mackay IR, Manns MP, et al. Liver autoimmune serology: a consensus statement from the committee for autoimmune serology of the International Autoimmune Hepatitis Group. J Hepatol. 2004;41:677–683. doi: 10.1016/j.jhep.2004.08.002. 10.1016/j.jhep.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 65.Lenzi M, Ballardini G, Fusconi M, Cassani F, Selleri L, Volta U, et al. Type 2 autoimmune hepatitis and hepatitis C virus infection. Lancet. 1990;335:258–259. doi: 10.1016/0140-6736(90)90070-l. 10.1016/014067369090070L. [DOI] [PubMed] [Google Scholar]
- 66.Martini E, Abuaf N, Cavalli F, Durand V, Johanet C, Homberg JC. Antibody to liver cytosol (anti-LC1) in patients with autoimmune chronic active hepatitis type 2. Hepatology. 1988;8:1662–1666. doi: 10.1002/hep.1840080632. 10.1002/hep.1840080632. [DOI] [PubMed] [Google Scholar]
- 67.Han S, Tredger M, Gregorio GV, MieliVergani G, Vergani D. Anti-liver cytosolic antigen type 1 (LC1) antibodies in childhood autoimmune liver disease. Hepatology. 1995;21:58–62. [PubMed] [Google Scholar]
- 68.Lenzi M, Manotti P, Muratori L, Cataleta M, Ballardini G, Cassani F, et al. Liver cytosolic 1 antigen-antibody system in type 2 autoimmune hepatitis and hepatitis C virus infection. Gut. 1995;36:749–754. doi: 10.1136/gut.36.5.749. 10.1136/gut.36.5.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lapierre P, Hajoui O, Homberg JC, Alvarez F. Formiminotransferase cyclodeaminase is an organ-specific autoantigen recognized by sera of patients with autoimmune hepatitis. Gastroenterology. 1999;116:643–649. doi: 10.1016/s0016-5085(99)70186-1. 10.1016/S0016508599701861. [DOI] [PubMed] [Google Scholar]
- 70.Muratori L, Cataleta M, Muratori P, Lenzi M, Bianchi FB. Liver/kidney microsomal antibody type 1 and liver cytosol antibody type 1 concentrations in type 2 autoimmune hepatitis. Gut. 1998;42:721–726. doi: 10.1136/gut.42.5.721. 10.1136/gut.42.5.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vergani D, Longhi MS, Bogdanos DP, Ma Y, MieliVergani G. Autoimmune hepatitis. Semin Immunopathol. 2009;31:421–435. doi: 10.1007/s00281-009-0170-7. 10.1007/s0028100901707. [DOI] [PubMed] [Google Scholar]
- 72.Wies I, Brunner S, Henninger J, Herkel J, Kanzler S, Meyer zum Büschenfelde KH, et al. Identification of target antigen for SLA/LP autoantibodies in autoimmune hepatitis. Lancet. 2000;355:1510–1515. doi: 10.1016/s0140-6736(00)02166-8. 10.1016/S0140673600021668. [DOI] [PubMed] [Google Scholar]
- 73.Manns M, Gerken G, Kyriatsoulis A, Staritz M, Meyer zum Büschenfelde KH. Characterisation of a new subgroup of autoimmune chronic active hepatitis by autoantibodies against a soluble liver antigen. Lancet. 1987;1:292–294. doi: 10.1016/s0140-6736(87)92024-1. 10.1016/S0140673687920241. [DOI] [PubMed] [Google Scholar]
- 74.Ma Y, Okamoto M, Thomas MG, Bogdanos DP, Lopes AR, Portmann B, et al. Antibodies to conformational epitopes of soluble liver antigen define a severe form of autoimmune liver disease. Hepatology. 2002;35:658–664. doi: 10.1053/jhep.2002.32092. 10.1053/jhep.2002.32092. [DOI] [PubMed] [Google Scholar]
- 75.Costa M, Rodriguez-Sanchez JL, Czaja AJ, Gelíp C. Isolation and characterization of cDNA encoding the antigenic protein of the human tRNP(Ser)Sec complex recognized by autoantibodies from patients withtype-1 autoimmune hepatitis. Clin Exp Immunol. 2000;121:364–374. doi: 10.1046/j.1365-2249.2000.01280.x. 10.1046/j.13652249.2000.01280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hagen EC, Andrassy K, Chernok E, Daha MR, Gaskin G, Gross W, et al. The value of indirect immunofluorescence and solid phase techniques for ANCA detection. A report on the first phase of an international cooperative study on the standardization of ANCA assays. EEC/BCR Group for ANCA Assay Standardization. J Immunol Methods. 1993;159:1–16. doi: 10.1016/0022-1759(93)90136-u. 10.1016/002217599390136U. [DOI] [PubMed] [Google Scholar]
- 77.Bogdanos DP, MieliVergani G, Vergani D. Autoantibodies and their antigens in autoimmune hepatitis. Semin Liver Dis. 2009;29:241–253. doi: 10.1055/s-0029-1233533. 10.1055/s00291233533. [DOI] [PubMed] [Google Scholar]
- 78.McFarlane IG, McFarlane BM, Major GN, Tolley P, Williams R. Identification of the hepatic asialoglycoprotein receptor (hepatic lectin) as a component of liver specific membrane lipoprotein (LSP) Clin Exp Immunol. 1984;55:347–354. [PMC free article] [PubMed] [Google Scholar]
- 79.Treichel U, Gerken G, Rossol S, Rotthauwe HW, Meyer zum Büschenfelde KH, Poralla T. Autoantibodies against the human asialoglycoprotein receptor: effects of therapy in autoimmune and virusinduced chronic active hepatitis. J Hepatol. 1993;19:55–63. doi: 10.1016/s0168-8278(05)80176-x. 10.1016/S016882780580176X. [DOI] [PubMed] [Google Scholar]
- 80.Treichel U, McFarlane BM, Seki T, Krawitt EL, Alessi N, Stickel F, et al. Demographics of anti-asialoglycoprotein receptor auto-antibodies in autoimmune hepatitis. Gastroenterology. 1994;107:799–804. doi: 10.1016/0016-5085(94)90129-5. 10.1016/0016508594901295. [DOI] [PubMed] [Google Scholar]
- 81.Czaja AJ, Carpenter HA. Histological findings in chronic hepatitis C with autoimmune features. Hepatology. 1997;26:459–466. doi: 10.1002/hep.510260229. 10.1002/hep.510260229. [DOI] [PubMed] [Google Scholar]
- 82.Stravitz RT, Lefkowitch JH, Fontana RJ, Gershwin ME, Leung PS, Sterling RK, et al. Autoimmune acute liver failure: proposed clinical and histological criteria. Hepatology. 2011;53:517–526. doi: 10.1002/hep.24080. 10.1002/hep.24080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Krawitt EL. Autoimmune hepatitis. N Engl J Med. 2006;354:54–66. doi: 10.1056/NEJMra050408. 10.1056/NEJMra050408. [DOI] [PubMed] [Google Scholar]
- 84.MieliVergani G, Vergani D. Autoimmune hepatitis in children. Clin Liver Dis. 2002;6:623–634. doi: 10.1016/s1089-3261(02)00020-x. 10.1016/S108932610200020X. [DOI] [PubMed] [Google Scholar]
- 85.Gregorio GV, Portmann B, Karani J, Harrison P, Donaldson PT, Vergani D, et al. Autoimmune hepatitis/sclerosing cholangitis overlap syndrome in childhood: a 16-year prospective study. Hepatology. 2001;33:544–553. doi: 10.1053/jhep.2001.22131. 10.1053/jhep.2001.22131. [DOI] [PubMed] [Google Scholar]
- 86.Johnson PJ, McFarlane IG, Williams R. Azathioprine for longterm maintenance of remission in autoimmune hepatitis. N Engl J Med. 1995;333:958–63. doi: 10.1056/NEJM199510123331502. 10.1056/NEJM199510123331502. [DOI] [PubMed] [Google Scholar]
- 87.Lohse AW, Mieli-Vergani G. Autoimmune hepatitis. J Hepatol. 2011;55:171–182. doi: 10.1016/j.jhep.2010.12.012. 10.1016/j.jhep.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 88.Vergani D, MieliVergani G. Pharmacological management of autoimmune hepatitis. Expert Opin Pharmacother. 2011;12:607–613. doi: 10.1517/14656566.2011.524206. 10.1517/14656566.2011.524206. [DOI] [PubMed] [Google Scholar]
- 89.Yeoman AD, Longhi MS, Heneghan MA. Review article: the modern management of autoimmune hepatitis. Aliment Pharmacol Ther. 2010;31:771–87. doi: 10.1111/j.1365-2036.2010.04241.x. 10.1111/j.13652036.2010.04241.x. [DOI] [PubMed] [Google Scholar]
- 90.Heneghan MA, McFarlane IG. Current and novel immunosuppressive therapy for autoimmune hepatitis. Hepatology. 2002;35:7–13. doi: 10.1053/jhep.2002.30991. 10.1053/jhep.2002.30991. [DOI] [PubMed] [Google Scholar]
- 91.Weiler-Normann C, Schramm C, Quaas A, Wiegard C, Glaubke C, Pannicke N, et al. Infliximab as a rescue-treatment in difficult-to-treat autoimmune hepatitis. J Hepatol. 2012;58:529–534. doi: 10.1016/j.jhep.2012.11.010. 10.1016/j.jhep.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 92.Efe C, Purnak T, Ozaslan E, Wahlin S. Drug-induced autoimmune hepatitis caused by anti-tumor necrosis factor alpha agents. Hepatology. 2010;52:2246–2247. doi: 10.1002/hep.23834. 10.1002/hep.23834. [DOI] [PubMed] [Google Scholar]
- 93.Barth E, Clawson J. A Case of Autoimmune Hepatitis Treated with Rituximab. Case Rep Gastroenterol. 2010;4:502–509. doi: 10.1159/000322693. 10.1159/000322693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Manns MP, Woynarowski M, Kreisel W, Lurie Y, Rust C, Zuckerman E, et al. Budesonide induces remission more effectively than prednisone in a controlled trial of patients with autoimmune hepatitis. Gastroenterology. 2010;139:1198–1206. doi: 10.1053/j.gastro.2010.06.046. 10.1053/j.gastro.2010.06.046. [DOI] [PubMed] [Google Scholar]
- 95.Hempfling W, Grunhage F, Dilger K, Reichel C, Beuers U, Sauerbruch T. Pharmacokinetics and pharmacodynamic action of budesonide in early- and late-stage primary biliary cirrhosis. Hepatology. 2003;38:196–202. doi: 10.1053/jhep.2003.50266. 10.1053/jhep.2003.50266. [DOI] [PubMed] [Google Scholar]
- 96.Manns MP, Czaja AJ, Gorham JD, Krawitt EL, Mieli-Vergani G, Vergani D, et al. Diagnosis and management of autoimmune hepatitis. Hepatology. 2010;51:2193–2213. doi: 10.1002/hep.23584. 10.1002/hep.23584. [DOI] [PubMed] [Google Scholar]
- 97.Reich DJ, Fiel I, Guarrera JV, Emre S, Guy SR, Schwartz ME, et al. Liver transplantation for autoimmune hepatitis. Hepatology. 2000;32:693–700. doi: 10.1053/jhep.2000.16666. 10.1053/jhep.2000.16666. [DOI] [PubMed] [Google Scholar]
- 98.Mottershead M, Neuberger J. Transplantation in autoimmune liver diseases. World J Gastroenterol. 2008;14:3388–3395. doi: 10.3748/wjg.14.3388. 10.3748/wjg.14.3388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Strassburg CP, Manns MP. Treatment of autoimmune hepatitis. Semin Liver Dis. 2009;29:273–285. doi: 10.1055/s-0029-1233534. 10.1055/s00291233534. [DOI] [PubMed] [Google Scholar]
- 100.Liberal R, Grant CR, Mieli-Vergani G, Vergani D. Autoimmune hepatitis a comprehensive review. J Autoimmun. 2013;41:126–139. doi: 10.1016/j.jaut.2012.11.002. 10.1016/j.jaut.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 101.Liberal R, Zen Y, Mieli-Vergani G, Vergani D. Liver transplantation and autoimmune liver diseases. Liver Transpl. 2013;19:1065–1077. doi: 10.1002/lt.23704. 10.1002/lt.23704. [DOI] [PubMed] [Google Scholar]
- 102.Ichai P, Duclos-Vallee JC, Guettier C, Hamida SB, Antonini T, Delvart V, et al. Usefulness of corticosteroids for the treatment of severe and fulminant forms of autoimmune hepatitis. Liver Transpl. 2007;13:996–1003. doi: 10.1002/lt.21036. 10.1002/lt.21036. [DOI] [PubMed] [Google Scholar]
- 103.Kessler WR, Cummings OW, Eckert G, Chalasani N, Lumeng L, Kwo PY. Fulminant hepatic failure as the initial presentation of acute autoimmune hepatitis. Clin Gastroenterol Hepatol. 2004;2:625–631. doi: 10.1016/s1542-3565(04)00246-0. 10.1016/S1542356504002460. [DOI] [PubMed] [Google Scholar]
- 104.Potts JR, Verma S. Optimizing management in autoimmune hepatitis with liver failure at initial presentation. World J Gastroenterol. 2011;17:2070–2075. doi: 10.3748/wjg.v17.i16.2070. 10.3748/wjg.v17.i16.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Verma S, Gunuwan B, Mendler M, Govindrajan S, Redeker A. Factors predicting relapse and poor outcome in type I autoimmune hepatitis role of cirrhosis development patterns of transaminases during remission and plasma cell activity in the liver biopsy. Am J Gastroenterol. 2004;99:1510–1516. doi: 10.1111/j.1572-0241.2004.30457.x. 10.1111/j.15720241.2004.30457.x. [DOI] [PubMed] [Google Scholar]
- 106.Miyake Y, Iwasaki Y, Terada R, Onishi T, Okamoto R, Sakai N, et al. Clinical characteristics of fulminant-type autoimmune hepatitis an analysis of eleven cases. Aliment Pharmacol Ther. 2006;23:1347–1353. doi: 10.1111/j.1365-2036.2006.02894.x. 10.1111/j.13652036.2006.02894.x. [DOI] [PubMed] [Google Scholar]
- 107.Liberal R, Longhi MS, Grant CR, Mieli-Vergani G, Vergani D. Autoimmune hepatitis after liver transplantation. Clin Gastroenterol Hepatol. 2012;10:346–353. doi: 10.1016/j.cgh.2011.10.028. 10.1016/j.cgh.2011.10.028. [DOI] [PubMed] [Google Scholar]
- 108.Futagawa Y, Terasaki PI. An analysis of the OPTN/UNOS Liver Transplant Registry. Clin Transpl. 2004:315–329. [PubMed] [Google Scholar]



