Abstract
Objective
To evaluate changes in the trajectory of youth anxiety following the introduction of specific cognitive behavior therapy (CBT) components: relaxation training, cognitive restructuring, and exposure tasks.
Methods
488 youths ages 7–17 years (50% female; 74% ≤ 12 years) were randomly assigned to receive either CBT, sertraline (SRT), their combination (COMB), or pill placebo (PBO) as part of their participation in the Child/Adolescent Anxiety Multimodal Study (CAMS). Youths in the CBT conditions were evaluated weekly by therapists using the Clinical Global Impression Scale-Severity (CGI-S; Guy, 1976) and the Children’s Global Assessment Scale (CGAS; Schaffer et al., 1983) and every four weeks by blind independent evaluators (IEs) using the Pediatric Anxiety Ratings Scale (PARS; Rupp Study Group, 2002). Youths in SRT and PBO were included as controls.
Results
Longitudinal discontinuity analyses indicated that the introduction of both cognitive restructuring (e.g., changing self-talk) and exposure tasks significantly accelerated the rate of progress on measures of symptom severity and global functioning moving forward in treatment; the introduction of relaxation training had limited impact. Counter to expectations, no strategy altered the rate of progress in the specific domain of anxiety that it was intended to target (i.e., somatic symptoms, anxious self-talk, avoidance behavior).
Conclusions
Findings support CBT theory and suggest that cognitive restructuring and exposure tasks each make substantial contributions to improvement in youth anxiety. Implications for future research are discussed.
Keywords: cognitive behavior therapy, child anxiety, treatment components
Cognitive behavior therapy (CBT) is recognized as an efficacious treatment for child and adolescent anxiety disorders (Hollon & Beck, 2013). To date, more than 20 randomized controlled trials (RCTs) have documented its benefits, with average between-group effect sizes ranging from 0.31 to 0.44 (see Seligman & Ollendick, 2011, for review). In the Child/Adolescent Anxiety Multimodal Study (CAMS; Walkup et al 2008), the largest study of youth anxiety treatment to date, CBT (Coping Cat Program) was evaluated alone and in combination with medication (sertraline). The combined treatment produced the highest response rates (80.7%) and CBT alone produced response rates (59.7%) similar to medication (54.9%). These findings add to the existing literature (e.g., Barrett et al., 1996; Kendall et al., 2008) and elevate individual child CBT to the status of a “well-established” treatment for pediatric anxiety as defined by widely-accepted criteria (Chambless & Hollon, 1998). Among the over 500 child and adolescent therapies currently available for various forms of youth psychopathology (Kazdin, 2000), this remains a rare distinction.
Much less is known about how CBT for anxiety works. Findings from numerous trials link specific CBT protocols to favorable outcomes (Seligman & Ollendick, 2012; Walkup et al., 2008). Yet, by and large, questions about how anxiety was reduced or which intervention components were most central to success have been understudied. This gap in understanding is problematic for the field of youth anxiety where growing emphasis is on disseminating treatments previously established as efficacious. From this perspective, efforts to shed light on change processes in CBT for anxiety in youth are essential to moving the field forward.
One challenge for work in this area rests with the fact that virtually all CBT protocols involve multiple treatment components. For example, the Coping Cat Program (Kendall & Hedkte, 2006) used in CAMS employs a variety of strategies including psychoeducation, relaxation training, cognitive restructuring, and exposure tasks. Each is thought to target a specific aspect of anxiety. For instance, psychoeducation about physiological signs of anxiety and the introduction of related relaxation exercises should help youngsters to reinterpret bodily cues in a less threatening manner and to soothe somatic symptoms of anxiety. Likewise, cognitive restructuring exercises should help youth to identify and correct dysfunctional thinking patterns. Finally, exposure exercises should decrease avoidance behaviors and related functional impairment.
What is the relative potency of these components for treatment success? Cognitive behavioral theory posits that physiological arousal is a hallmark feature of anxiety. Techniques such as relaxation training are therefore thought to be useful to the extent that they soothe somatic symptoms. CBT theory also suggests that distorted thinking plays a central role in anxiety disorder, and that changes in anxiogenic thoughts (e.g., misperceptions of threat) are crucial for improvement (Beck, 1976; Rapee et al., 2000; Treadwell & Kendall, 1996). Cognitive restructuring exercises are thus thought to be a key treatment ingredient. At the same time, exposure tasks typically are viewed as a central strategy for decreasing avoidance behavior (e.g., Foa & Kozak, 1986). Reviews of the literature (e.g., Chorpita et al., 2005) suggest that exposure tasks are part of virtually all evidence-based treatment for child and adolescent anxiety. However, with rare exception (e.g., Kendall et al., 1997), few studies have examined which of these components produces significant changes in the rate of progress moving forward from its implementation.
Along related lines, the literature contains relatively little work examining the impact of specific therapeutic components on the domains of anxiety that they are meant to address. This is due in part to the fact that most RCTs for youth anxiety focus primarily on behavioral or global anxiety outcomes, even though measures of specific features of anxiety (e.g., somatic, cognitive) are available (Ronan, Kendall, & Rowe, 1996; Research Units of Pediatric Psychopharmacology; RUPP Anxiety Study Group, 2002). Another barrier stems from design considerations. The most rigorous test of the relative efficacy of specific treatment components would be a dismantling study; however, such endeavors have limitations (especially for treatments with sequenced and incremental components) and are rare. Of the existing studies, some are multiple-baselines and others are secondary analyses (see Barrios & O’Dell, 1998; David & Ollendick, 2005 for a review).
A multiple baseline study by Eisen and Silverman (1993) found that cognitive restructuring and relaxation training produced similar improvements in anxiety; however, exposure was present in all conditions and there was no exposure-only condition. Silverman et al. (1999) found that both skills training and contingency management produced similar results. Perhaps most notably, in keeping with Last et al. (1998), youngsters receiving educational support also evidenced treatment gains. More recently, Nakamura, Pestle, and Chorpita (2009) examined the timing of therapeutic changes among four youths receiving exposure and cognitive/coping skills training in a multiple-baseline design. Results varied across parent- and child-reports and outcome variables, with some indication that exposure exercises were central to treatment gains; however, the small sample size and differences in the number of sessions received across participants limit the findings.
The CAMS trial offers an opportunity to examine the relative impact and timing of specific CBT components on targeted outcomes. CAMS gathered weekly assessments throughout treatment and more extensive assessments by independent evaluators (IEs) blind to treatment status every four weeks. Measures included multiple domains of anxiety (i.e., physical symptoms, behavioral, cognitive) in addition to global severity and improvement. Importantly, CAMS involved a standardized CBT protocol (Kendall & Hedtke, 2006) that was implemented in a systematized manner. Ongoing assessment of adherence made it possible to monitor when intervention components (e.g., relaxation, cognitive restructuring) were initiated. This feature in turn permitted examination of the components and changes in the anxiety domain they were intended to tap (e.g., somatic symptoms, cognitive variables), and assessment of whether the implementation of each component was followed by significant changes in the rate of subsequent treatment progress.
The present investigation evaluates changes in treatment trajectories following the introduction of three specific CBT components. Although the focus is on participants who received CBT (either alone or in combination with medication), trajectories of participants in the two medication only treatment conditions (SRT and PBO) were also included. Direct comparisons between CBT and COMB allowed for an assessment of whether the addition of medication to CBT produced differential changes (either positively or negatively) in treatment trajectories.
Focusing on relaxation training, cognitive restructuring, and exposure tasks, we examine whether the introduction of each of these components was followed by a change in the rate of progress moving forward with respect to measures of overall anxiety symptom severity and global functioning. Because relaxation training was meant to help youth to identify signs of anxiety that might later cue them to think/act differently (thus drawing on other treatment skills), it was expected that it would have relatively limited impact on the rate of progress moving forward. Based on data indicating that changes in anxious self-talk mediate treatment outcome (Kendall & Treadwell, 2007), we expected that cognitive restructuring would be followed by significant improvement in the rate of treatment progress moving forward (i.e., steeper slope of improvement). Recognizing that exposure tasks are crucial to anxiety treatment, we expected that exposure tasks would have benefits beyond those accounted for by earlier intervention strategies and would be followed by acceleration in the rate of change.
Additional analyses evaluated whether each of these components was associated with significant decreases in the anxiety domain it was intended to tap (e.g., somatic symptoms, cognitive distortions, avoidance behavior, respectively), and whether it significantly altered the rate of change in that particular anxiety domain moving forward. We hypothesized that the initiation of relaxation training would be associated with decreases in physical symptoms of anxiety, that the initiation of cognitive restructuring would be associated with decreases in cognitive distortions related to anxiety, and that the start of exposure tasks would be linked to decreases in avoidance behavior.
Method
Participants
Children and adolescents (N=488) between the ages of 7 and 17 participated in CAMS across six sites (Compton et al., 2010; Walkup et al., 2008). To be included, participants were required to meet DSM-IV (American Psychiatric Association, 2000) criteria for one or more of the following disorders: Separation Anxiety Disorder (SAD), Social Phobia (SP), or Generalized Anxiety Disorder (GAD). Exclusion criteria included major depressive disorder (MDD), bipolar disorder, pervasive developmental disorder, and schizophrenia or schizoaffective disorder. Participants were randomly assigned to 12 weeks of treatment: cognitive behavior therapy (CBT; Coping Cat program; n=139), medication (sertraline, SRT; n=133), combined CBT + SRT, (COMB; n=140), or pill placebo (PBO; n=76). There were no significant differences between conditions with respect to demographic or clinical variables (Walkup et al., 2008; See Table 1).
Table 1.
Baseline demographic and clinical characteristics*
| Variable | COMB (N=140) |
SRT (N= 133) |
CBT (N= 139) |
PBO (N=76) |
All Subjects |
p- value |
|---|---|---|---|---|---|---|
| Demographic characteristics | ||||||
| Age | ||||||
| 7–12 year (%) | 101 (72.1) | 99 (74.4) | 108 (77.7) | 54 (71.1) | 362 (74.2) | 0.66 |
| Mean age-years | 10.7 ± 2.8 | 10.8 ± 2.8 | 10.5 ± 2.9 | 10.6 ± 2.8 | 10.7 ± 2.8 | 0.93 |
| Female sex-no. (%) | 75 (51.4) | 61 (45.9) | 72 (51.8) | 37 (48.7) | 242 (49.6) | 0.75 |
| Race or ethnic group—no. (%)+ | ||||||
| White | 116 (82.9) | 103 (77.4) | 106 (76.3) | 60 (78.9) | 385 (78.9) | 0.56 |
| Black | 11 (7.9) | 12 (9.0) | 14 (10.1) | 7 (9.2) | 44 (9.0) | 0.94 |
| Asian | 6 (4.3) | 4 (3.0) | 1 (0.7) | 1 (1.3) | 12 (2.5) | 0.23 |
| American Indian | 1 (0.7) | 2 (1.5) | 3 (2.2) | 0 | 6 (1.2) | 0.51 |
| Pacific Islander | 1 (0.7) | 0 | 0 | 1 (1.3) | 2 (0.4) | 0.40 |
| Other | 5 (3.6) | 12 (9.0) | 15 (10.8) | 7 (9.2) | 39 (8.0) | 0.14 |
| Hispanic | 16 (11.4) | 15 (11.3) | 21 (15.1) | 7 (9.2) | 59 (12.1) | 0.59 |
| Low SES-no. (%) | 35 (25.0) | 35 (26.3) | 33 (23.7) | 21 (27.6) | 124 (25.4) | 0.92 |
| Clinical characteristics | ||||||
| CGAS | 50.4 (7.2) | 51.9 (7.5) | 50.9 (7.5) | 50.5 (7.4) | 50.7 (7.1) | 0.87 |
| CGI-S | 5.1 (0.7) | 4.9 (0.7) | 5.0 (0.7) | 5.1 (0.7) | 5.0 (0.7) | 0.25 |
| NASSQ Total Score | 30.8 (17.9) | 31.7 (18.4) | 32.0 (19.3) | 29.0 (17.2) | 31.1 (18.3) | 0.68 |
| PSC | 14.7 (14.0) | 13.5 (13.9) | 13.7 (12.8) | 12.9 (11.2) | 13.8 (13.2) | 0.77 |
| PARS Avoidance | 3.5 (1.0) | 3.2 (1.1) | 3.4 (1.0) | 3.4 (1.1) | 3.4 (1.0) | 0.83 |
Note. Plus-minus values are means ±SD.
Race or ethnic group was reported by the participants. ŧLow Socioeconomic status was defined as a score of 3 or less on the Hollingshead Two-Factor Scale, which ranges from 1 to 5.
COMB= Combination of sertraline (SRT) and cognitive behavior therapy (CBT); PBO= medication management with placebo. PARS=Pediatric Anxiety Ratings Scale; CGAS=Children’s Global Assessment Scale; CGI-S=Clinician’s Global Impressions Scale-Severity; NASSQ=Negative Affect Self-Statement Questionnaire; PSC=Physical Symptom Checklist; PARS Avoidance=Pediatric Anxiety Rating Scale item 5.
Of the 488 participants, 49.6% were female, 78.9% were Caucasian, 74.2% were 12 years of age or younger, 74.9% were markedly to severely ill on the baseline Clinician Global Impressions-Severity rating scale (CGI-S; Guy, 1976), and 55.4% were recruited by project advertisements and outreach. For detailed characteristics of the CAMS youth, see Kendall et al., 2010.
Interventions
The CBT intervention in CAMS involved 14 sessions over 12 weeks (12 child sessions and 2 parent-only sessions). The Coping Cat Program (or the C.A.T. Project, a version for adolescents) includes skills training in anxiety-management followed by practice (i.e., exposure tasks) in anxiety-provoking situations tailored to the participant’s needs. Within CAMS, the protocol was standardized across sites (therapists followed the same weekly session content schedule). Although therapists were allowed “flexibility within fidelity” (Kendall et al, 2008) to tailor treatment to youth needs, they were encouraged to adhere to the schedule for introducing specific intervention components. Although not typical, components could be introduced at a different time or skipped altogether if clinically indicated. As detailed below, our data analytic approach enabled us to address these variations. Session summary forms documented the primary and secondary intervention components used during each session, and treatment fidelity was assessed across sites using a standardized adherence measure (Kendall, Gosch, Albano, Ginsburg & Compton, 2001).
The 12-week COMB condition included CBT plus SRT. The SRT condition involved eight sessions that were 30–60 minutes long and included discussion of anxiety symptom severity, treatment response, and adverse events. Psychiatrists or nurse practitioners administered SRT, and pill counts and medication diaries were used to monitor adherence. The CBT and SRT visits were scheduled on the same day when possible. For details see Walkup et al., (2008).
Timing of Assessments Relative to Timing of Treatment Content
In general, the Coping Cat Program employed in this study introduced relaxation training during week 3 of treatment, cognitive restructuring during week 5, and structured exposure tasks during week 6. With respect to exposure tasks, therapists created a fear hierarchy and typically began with low-difficulty tasks and progressed gradually to more challenging exposure tasks. Analyses herein document average start dates for relaxation training (on day 13), cognitive restructuring (on day 19), and moderate-level difficulty exposure tasks (on day 53). The onset of moderately difficult exposure tasks (defined via child SUDS ratings) was chosen because when creating a fear hierarchy, moderately difficult anxiety provoking situations are more likely to be related to situations causing functional impairment. Therefore, the onset of moderately challenging exposures was chosen as the beginning of clinically relevant and meaningful exposure-based treatment. Stated differently, low-level exposure tasks were viewed more as “practice” and time for the child to become comfortable with the procedure.
Both therapists and IEs provided outcome data for the present analyses. Dependent variables from therapists included weekly ratings on the Clinician’s Global Impressions-Severity Scale (CGI-S; Guy, 1976) and Clinician’s Global Assessment Scale (CGAS; Shaffer et al, 1983), which mapped changes in anxiety symptom severity and global functioning directly to the introduction of specific therapeutic components. Monthly ratings from IEs (the Pediatric Anxiety Ratings Scale; Rupp Study Group 2002; CGI-S, and CGAS) provided dependent variables from raters blind to treatment condition. For questions that relied upon the PARS, only the IE data were used. Notably, evidence suggests that IEs and therapists produce similar ratings of improvement on standardized outcome measures and that, when ratings diverge, therapists may be more conservative (Lewin et al., 2012). Flexibility in the assessment schedule was allowed by study design (e.g., to accommodate participant schedules). Moreover, the statistical models employed do not require evenly spaced assessments or that the assessment schedule coincide with the onset of a given treatment component. For our analyses, days since the beginning of treatment was used as the time metric for both clinician and IE assessments.
Treatment Integrity
Treatment fidelity was maintained in three ways: First, through weekly on-site supervision, second through a weekly cross-site supervision conference call involving all therapy supervisors and therapists, and third through real time evaluation of a random sample of therapy tapes. A sample of two tapes per participant was rated using a 24-item checklist to evaluate treatment integrity (adherence to specified session-by-session content), therapist proficiency, and general therapeutic competence (e.g., rapport building). On the items measuring appropriate use of cognitive restructuring techniques, 96% scored satisfactory to superior. On the items measuring appropriate use of relaxation techniques, 80% scored satisfactory or superior. On the items measuring exposure techniques, 89.5% scored satisfactory or superior. Overall inter-rater reliability was high, r=.88.
Measures
Anxiety Disorder Interview Schedule (ADIS C/P; Silverman & Albano, 1996)
Diagnostic status was determined using the child and parent versions of the ADIS, a semi-structured clinical interview that assesses a range of DSM-IV disorders in children and adolescents. The interview yields composite impairment ratings (Clinician Severity Rating; CSR) ranging from 0 to 8 for each diagnosis, with higher scores reflecting greater levels of severity. IEs underwent extensive training and supervision to maintain reliability, and multiple measures were put in place to keep them blind to study condition (see Compton et al., 2010 for detailed procedures). The intraclass correlation coefficient for the test-retest inter-rater reliability between the CAMS IEs and CAMS quality assurance (QA) raters was .88 for SAD, .85 for SoP, and .82 for GAD, respectively.
Clinical Global Impression Scale-Severity (CGI-S; Guy, 1976)
The CGI-S asks clinicians to rate the patient’s current overall level of symptom severity on a scale of 1–8 (higher scores = greater severity). Therapists completed the CGI-S weekly and IEs provided ratings at Week 0, 4, 8, and 12. Although widely used as an outcome measure in psychopharmacology trials, few studies of its psychometric properties have been published. However, in the CAMS sample, the consistency of the IE ratings of the CGI-S with the PARS total score for the same participant revealed a correlation of r=.78 suggesting both measures tap overall anxiety severity.
Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983)
The CGAS is clinician-administered and evaluates overall levels of impairment on a scale of 0–100. Higher scores indicate better functioning; scores <60 typically indicate need for treatment. The CGAS was completed weekly by therapists and weeks 0, 4, 8, and 12 by IEs. The intraclass coefficient for retest reliability was .83 (Bird, Canino, Rubio-Stipec, & Ribera, 1987).
Pediatric Anxiety Rating Scale (PARS; Research Units on Pediatric Psychopharmacology (RUPP) Anxiety Study Group, 2002)
The PARS is a clinician-administered instrument that evaluates symptoms of anxiety over the past week. Total scores range from 0–30 and are obtained by summing individual ratings of anxiety symptom severity, frequency, distress, avoidance, and interference. Higher PARS total scores reflect greater impairment, with scores above 13 suggesting clinically significant anxiety. The PARS has established psychometric properties including acceptable internal consistency, strong inter-rater reliability, and adequate retest reliability (Walkup et al., 2008). The PARS was completed by IEs at Weeks 0, 4, 8, and 12, and was the primary dimensional outcome measure in the overarching CAMS trial. Within the present analyses, total scores were used to examine overall anxiety symptom severity and the overall behavioral avoidance item was used as a measure of avoidance. The PARS has adequate internal consistency (α=.64) inter-rater reliability (r=.97), retest reliability (r=.55), and correlates significantly with several validity indicators (RUPP Anxiety Study Group, 2002).
Negative Affect Self-Statement Questionnaire (NASSQ; Ronan, Kendall, & Rowe, 1996)
The 70-item NASSQ asks youth to endorse the frequency of self-statements over the past week. It assesses both anxiogenic and depressive self-talk, requiring youth to respond on a 5-point Likert scale. The NASSQ has well-documented internal consistency, retest reliability, and concurrent validity (Sood & Kendall, 2007). Analysis of the baseline NASSQ in the CAMS sample revealed that it possessed excellent internal consistency, with α=0.95.
Physical Symptom Checklist (PSC; TADS, 2004)
The 47-item PSC is a self-report measure that includes general health problems (e.g., somatic and central nervous system symptoms). For each item, participants indicate using a 4-point Likert scale (from “not at all” to “very much”), how much they have been bothered by the symptom during the past week. The PSC was administered at baseline and weeks 4, 8, and 12. A total physical symptom score was obtained by summing items. Analysis of the baseline PSC in the CAMS sample revealed that it possessed excellent internal consistency, with α=.91.
Missing Data
Of the 488 participants randomized at baseline, 459 (94.1%) completed at least one post-baseline assessment, 396 (81.1%) completed all four IE assessments, and 440 (90.2%) completed the post-acute treatment assessment at Week 12. Study withdrawals by treatment condition were: 12 (9%) COMB, 6 (4%) CBT, 16 (12%) SRT, and 12 (16%) PBO. Of the 14 possible CBT sessions available to participants, the mean (±SD) number of sessions completed was 13.2 ±2.0 for those in CBT and 12.7 ±2.8 in COMB.
Data Analytic Plan
The statistical approach used involved a series of longitudinal multilevel discontinuity models (e.g., Singer & Willett, 2003) also known as piecewise linear regression models (e.g., Ryan & Porth, 2007). Such models can be used to evaluate whether a shift in an outcome trajectory (i.e., change in slope) occurs following the onset of an identifiable event. As implemented in the current study, longitudinal multilevel discontinuity models are used to determine whether specific CBT components are related to changes in treatment outcomes. For example, in CAMS, specific CBT sessions focused on cognitive restructuring. If helping children to cope more adaptively with their anxious thoughts is beneficial, we might expect a discontinuity in outcome trajectories (i.e., change in slopes) following the start of treatment session(s) that focus specifically on cognitive restructuring. The presence of such discontinuities would provide preliminary empirical support for the importance of a given treatment component and a better understanding of the mechanism through which treatment change might occur.
How might receipt of specific CBT components affect a participant’s outcome trajectories? To address these questions, we compared a series of discontinuous multilevel models for change that differed in both fixed effects and variance components. Specific hypotheses about the impact of the three CBT treatment components on mean change trajectories were systematically evaluated by adding relevant predictors to a “baseline” model that contained 17 parameters, 13 fixed effects and 4 variance components. The fixed effects were: (1) the intercept, (2) the main effect of time (which was modeled as DAYS since baseline), (3) the effect of site on initial status (which was modeled as 5 dummy coded indicators), (4) the effect of treatment condition on initial status (which was modeled as 3 dummy coded indicators), and (5) the effect of treatment condition on rate of change (which was modeled as a cross-level interaction between days and the 3 dummy indicators for treatment condition). The 4 variance components were: (1) the level-1 residual variance, (2) the level-2 variance on initial status (intercept), (3) the level-2 variance of rate of change (slope), and (4) the level-2 covariance between initial status and rate of change. To this “baseline model”, a series of discontinuous multilevel models for change was fitted to the data using full maximum likelihood estimation.
The specific outcome trajectory modeled (i.e., dependent variable) varied by the hypothesis under consideration. The presence or absence of a significant discontinuity was evaluated by introducing a second level-1 time-varying predictor to the “baseline model.” This predictor (POST-DAYS) was allowed to vary by participant (i.e., not all participants received a given component on the same day) and marked the onset of the treatment component. Once a participant received a given component, this predictor also marked the passage of time following receipt of the new treatment component. This second time varying predictor, if found to be significant, suggests that the average slope (i.e., rate of change) following receipt of the new treatment component was statistically different than the slope during the period preceding it. In other words, it captured the additive effect of the new treatment component on the overall average rate of change.
If a given discontinuity was statistically significant, the following level-2 predictors were evaluated to see if they moderated this new rate of change: (1) the effect of CBT-containing treatment conditions (CBT vs. COMB), (2) the effect age (children vs. adolescents), and the effect of gender (males vs. females). In each case, these level-2 predictors were modeled as a cross-level interaction between POST-DAYS and the dummy indicator for the moderator being evaluated. If a given linear discontinuity was found to be non-significant, an additional model was evaluated to determine if the impact of the treatment component had a delayed effect on outcomes. This was accomplished by adding a quadratic term to the level-1 individual growth model that already included DAYS and POST-DAYS. Additionally, to evaluate whether the magnitude of the discontinuity varied across participants, models in which POST-DAYS was treated as a random effect were evaluated. To assess whether such models resulted in a better fit to the data, the difference in the deviance statistic relative to the model excluding POST-DAYS as a random effect was used. This difference follows a chi-square distribution with dfs equal to the difference in the number of parameters between the two models. In all models, residual error terms were assumed to follow a mean-zero, normal distribution with an unstructured covariance structure used to capture the within person correlation over time. Tests were two-tailed, and p-values of less than 0.05 were considered to indicate statistical significance. Models were fit using PROC MIXED in SAS Statistical Software, Version 9.4 TS Level 1M0 (SAS Institute, Cary, NC). Finally, SRT and PBO treatment groups were included in all statistical models to control for the possibility that what was being modeled was an artifact of a rapid early response pattern, a phenomenon noted by other investigators (e.g., Ilardi & Craighead, 1994), and not due to the introduction of specific treatment components. Details of non-significant models are not reported but are available from the first author. Additional details of our analytic approach are provided in the Appendix.
Results
Outcomes Measured Weekly
The longitudinal discontinuity models evaluated in this section used therapist-rated outcomes completed following each treatment session. Changes in anxiety symptom severity were assessed using the CGI-S and changes in global functioning were measured using the CGAS.
Therapist-rated Anxiety Severity
Does the onset of relaxation training, cognitive restructuring, or exposure exercises lead to a significant difference in the average rate of change in children’s anxiety symptom severity as rated by therapists?
These questions were addressed by fitting a series of multilevel models for change to the therapist-rated CGI-S data in which the onset of each CBT component was systematically evaluated in temporal sequence. Results from this series of models are presented in Table 2. The first model presented in Table 2 is the baseline model (Model A). All subsequent models built systematically upon this model. Model B addressed the impact of relaxation training (RLX) on the mean CGI-S growth trajectories by adding a discontinuity in slope following the onset of RLX. Both fixed and random effects for RLX were included in Model B. Comparing Model B’s deviance statistic to that of Model A revealed a non-significant improvement in model fit (X2(4)=4.7, p=ns) and a non-significant estimate for the fixed effects of RLX (−0.003, p=.279). These findings suggest that the mean rate of change in CGI-S growth trajectories among those who received CBT did not change significantly before and after relaxation training. Model C evaluated whether removing the variance components associated with RLX, a simpler model, would result in a significant improvement in model fit. It did not (X2(3) =3.2, p=ns). To explore whether relaxation training might have a delayed impact on CGI-S growth curves, a quadratic change trajectory for RLX was explored. Results from this model were also non-significant (p=.397). These combined findings suggest that the mean CGI-S growth trajectories do not display an immediate or delayed change in slope following the onset of relaxation training. Given these results, the parameter RLX (both its fixed effects and variance components) was removed from all subsequent models.
Table 2.
Results from fitting a sequence of discontinuous change trajectories to CAMS clinician CGI-S data (n=488)
| n parameters for… | ||||||
|---|---|---|---|---|---|---|
| Model | Fixed effects | Variance components (in addition to ) |
Fixed effects |
Variance components |
Deviance | Comparison model: ΔDeviance(df) |
| A | Intercept, DAYS, SITE, TX, TX × DAYS | Intercept, DAYS | 13 | 4 | 8968.7 | — |
| B | Model A + RLX | Intercept, DAYS, RLX | 14 | 7 | 8964.0 | A: 4.7 (ns) (4) |
| C | Model B | Intercept, DAYS, w/o RLX | 14 | 4 | 8967.2 | B: 3.2 (ns) (3) |
| D | Model A + COG | Intercept, DAYS, COG | 14 | 7 | 8835.2 | A: 133.5** (4) |
| E | Model D | Intercept, DAYS, w/o COG | 14 | 4 | 8857.8 | D: 22.6** (3) |
| F | Model D + EXP | Intercept, DAYS, COG, EXP | 15 | 11 | 8717.1 | D: 118.1** (5) |
| G | Model F | Intercept, DAYS, COG, w/o EXP | 15 | 7 | 8794.5 | F: 77.4** (4) |
= p<.001;
CGI-S = clinical global impression – severity scale; SITE = vector of dummy coded site variables with site 6 serving as referent; TX = vector of dummy coded treatment conditions with COMB serving as referent; DAYS = days since baseline; RLX = onset of relaxation component of CBT; COG = onset of cognitive restructuring component of CBT; EXP = onset of exposure exercises component of CBT; CBT = cognitive behavior therapy.
Next we considered a model for the mean CGI-S response that allowed the rate of change in the CGI-S growth trajectories to be different before and after the onset of cognitive restructuring (COG) among those who received CBT. Model D (in Table 2) added both fixed and random effects for COG to the baseline model. Comparing the deviance statistic between Model D and the baseline model (Model A) revealed a significant improvement in model fit of (X2(4) =133.5, p<.001) and a significant fixed effects estimate for COG (−0.023, p<.001). These findings suggest that the CGI-S outcome trajectory does indeed display a linear discontinuity in slope post-COG. To determine whether the magnitude of this discontinuity varied across participants, Model E (in Table 2) removed the three variance components associated with COG. Because Model E’s fit was significantly worse (Model E – Model D; X2(3) =22.6, p<.001), these terms were retained in subsequent models. To explore potential moderators of COG, a series of models explored whether the discontinuity in COG varied by treatment condition (CBT vs. COMB), age (children vs. adolescents), or gender (boys vs. girls). Results from these models were all non-significant (all p’s >.05) and hence these parameters were not retained in subsequent models.
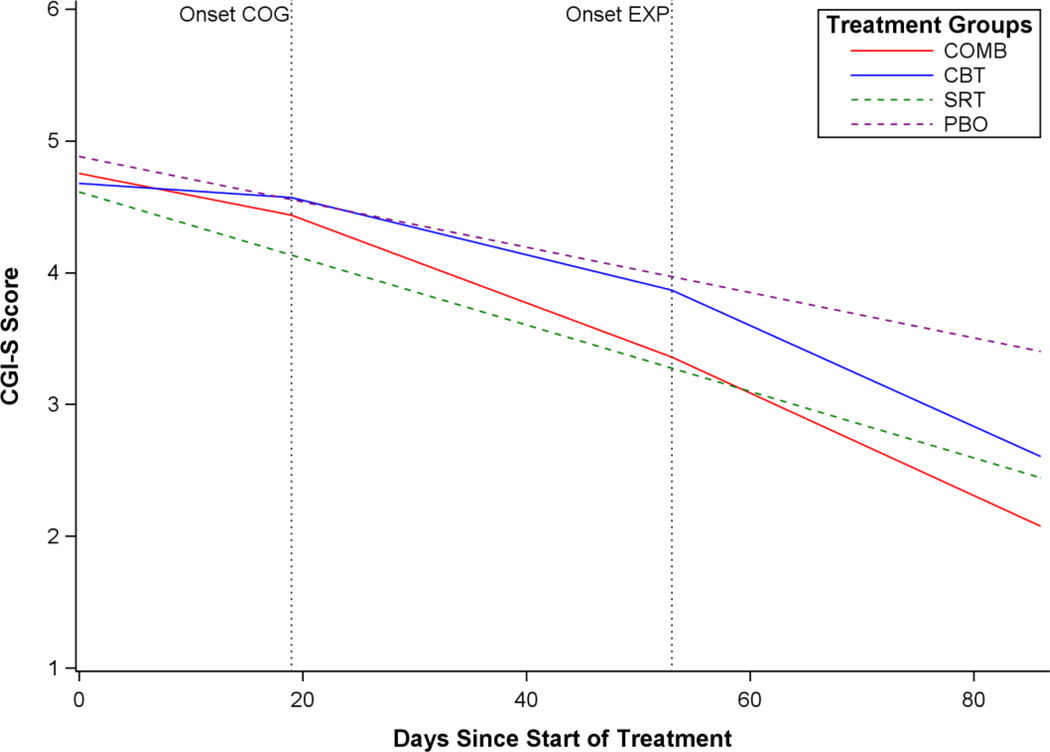
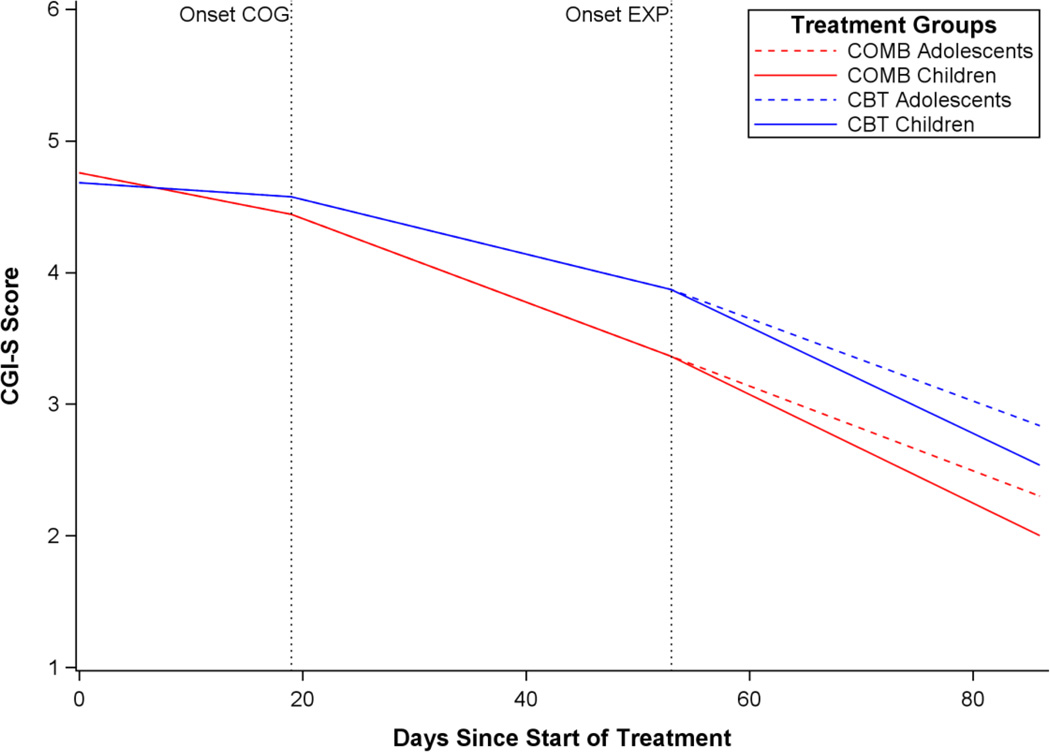
The last series of models explored the presence of a discontinuity in slope following the onset of exposure exercises (EXP) in CAMS clinician CGI-S ratings by including both fixed and random effects for EXP (Model F). Comparing the deviance statistic to the previous model (Model F - Model D) revealed a statistically significant improvement in model fit of (X2(5)=118.1, p<.001) and a significant discontinuity in slope for EXP (−0.013, p<.001). These findings indicate that the initial difference in slopes before and after cognitive restructuring (COG) is followed by a second linear discontinuity before and after the onset of exposure exercises (EXP). To evaluate whether the magnitude of this discontinuity varied significantly between participants, the next model (Model G) removed the three variance components associated with EXP. Because this model’s fit was significantly worse (X2(4) =77.4, p<.001), the terms associated with the variance components of EXP were retained in all subsequent models. Before examining Model F in more detail, additional multilevel models for change explored moderators of EXP. Results suggest that the mean post-EXP slope varied significantly by treatment condition (CBT vs. COMB; −0.010, p<.029) and participant age (child vs. adolescent; 0.009, p<.030). There were no significant differences in the post-EXP slopes between males and females (p=.315). A final model explored whether post-EXP slopes varied significantly by age within each treatment condition. This three-way interaction (i.e., EXP × TREATMENT × AGE) was not significant (p=.576). Detailed results of fitting Model F to the CAMS clinician CGI-S data (n=488), with the inclusion of two significant moderators of post-EXP slope trajectories, are available online (Supplemental Table 1). Model-based growth trajectories from 4 prototypical participants are illustrated in Figures 1 and 2. Model-based growth trajectories in all figures represent change over time for the average participant, with discontinuities in the trajectories based on the average day in which these components were introduced. Notably, trajectories would look different (i.e., the discontinuities in slope would appear earlier or later in time) for participants with earlier or later onset of the different treatment components.
Figure 1.
Estimated population mean CGI-S growth curve trajectories by CAMS treatment condition following the start of CBT cognitive restructuring and exposure exercises.
Note: Onset COG = onset of cognitive restructuring component of CBT; Onset EXP = onset of exposure exercises component of CBT.
Figure 2.
Estimated population mean CGI-S growth curve trajectories for COMB and CBT by participant age following the start of CBT exposure exercises.
Note: Onset COG = onset of cognitive restructuring component of CBT; Onset EXP = onset of exposure exercises component of CBT.
Figure 1 presents the estimated population mean CGI-S growth trajectories by each treatment condition and Figure 2 simplifies the results by focusing attention only on differences by age (i.e., children vs. adolescents) in post-EXP growth trajectories between the two CBT containing treatment conditions. The final model (see Figure 1 and Supplemental Table 1 online) suggests that before onset of cognitive restructuring, the average monthly rate of improvement on the therapist-rated CGI-S for participants in COMB was −0.51 points and −0.18 points for those in CBT alone. Upon the onset of cognitive restructuring, this average monthly rate of improvement increased to −0.96 points for those in COMB (approximately 88% faster than the corresponding rate during the previous period) and −0.63 points for those in CBT (approximately 250% faster than the corresponding rate during the previous period). Upon the onset of exposure exercises, the average monthly rate of improvement increased to −1.24 points for those in COMB (approximately 31% faster than the corresponding rate during the previous period) and −1.21 points for those in CBT (approximately 95% faster than the corresponding rate during the previous period). When compared to adolescents (see Figure 2), children showed a faster average monthly rate of improvement after the onset of exposures with an additional increase of −0.27 points on the CGI-S (children improved approximately 27% faster than adolescents across both treatment conditions). Finally, the statistically significant variance components for COG (p<.011) and EXP (p<.001) indicate that there is substantial variability in the rate of change from participant to participant following the onset of both cognitive restructuring and exposure exercises.
Does the onset of relaxation training, cognitive restructuring, or exposure exercises lead to a significant difference in the average rate of change in children’s global improvement as rated by therapists?
Similar to the discontinuity models presented on the CGI-S data, these questions were addressed by fitting a series of multilevel models for change to the weekly therapist-rated CGAS data. In these models, the onset of each CBT component was systematically evaluated in temporal sequence. Results from these models are presented in Table 3. The first model presented is the baseline model (Model A) and all subsequent models built systematically upon this model.
Table 3.
Results from fitting a sequence of discontinuous change trajectories to CAMS clinician CGAS data (n=488)
| n parameters for… | ||||||
|---|---|---|---|---|---|---|
| Model | Fixed effects | Variance components (in addition to ) |
Fixed effects |
Variance components |
Deviance | Comparison model: ΔDeviance(df) |
| A | Intercept, DAYS, SITE, TX, (TX × DAYS) | Intercept, DAYS | 13 | 4 | 25671.5 | — |
| B | Model A + RLX | Intercept, DAYS, RLX | 14 | 7 | 25662.9 | A: 8.6 (ns) (4) |
| C | Model B | Intercept, DAYS, w/o RLX | 14 | 4 | 25671.5 | B: 0.0 (ns) (3) |
| D | Model A + COG | Intercept, DAYS, COG | 14 | 7 | 25628.1 | A: 43.4** (4) |
| E | Model D | Intercept, DAYS, w/o COG | 14 | 4 | 25650.6 | D: 22.5** (3) |
| F | Model D + EXP | Intercept, DAYS, COG, EXP | 15 | 11 | 25556.8 | D: 71.3** (5) |
| G | Model F | Intercept, DAYS, COG, w/o EXP | 15 | 7 | 25619.6 | F: 62.8** (4) |
= p<.001;
CGAS = children’s global assessment scale; SITE = vector of dummy coded site variables with site 6 serving as referent; TX = vector of dummy coded treatment conditions with COMB serving as referent; DAYS = days since baseline; RLX = onset of relaxation component of CBT; COG = onset of cognitive restructuring component of CBT; EXP = onset of exposure exercises component of CBT; CBT = cognitive behavior therapy.
Model B added a discontinuity in slope following the onset of relaxation training (RLX) by including both its fixed and random effects. Comparing this model’s deviance statistic to that of the Model A revealed a non-significant improvement in model fit (X2(4) =8.6, p=ns) and a non-significant estimate for the fixed effects of RLX (−0.007, p=.776). These findings suggest that the average rate of change in CGAS growth curves did not change significantly following the onset of relaxation training. Model C evaluated whether removing the variance components associated with RLX might improve overall model fit. It did not (X2(3) = 0.0, p=ns). However, to explore the possibility that relaxation training might result in a delayed impact on CGAS growth trajectories, a quadratic change trajectory for RLX was evaluated. Results from this model were also non-significant (p=.573). These combined findings suggest that the estimated average CGAS growth trajectories do not display an immediate or delayed change in slope after the onset of relaxation training. Given these results, the parameter RLX (both its fixed effects and variance components) was removed from all subsequent models.
Model D (Table 3) evaluated whether there was a significant discontinuity in mean CGAS trajectories before and after the onset of cognitive restructuring (COG). Model D included both fixed and random effects for COG. Comparing the difference in deviance statistics between Model D and baseline model (Model A) revealed a significant improvement in model fit (X2(4) =43.4, p<.001) and a significant fixed effects estimate for COG (0.088, p<.001). These findings suggest that the CGAS outcome trajectory does indeed display a linear discontinuity in slope following the onset of cognitive restructuring. Model E explores whether the magnitude of this discontinuity varied across participants by removing the three variance components associated with COG. Because its fit was significantly worse (X2(3) = 22.5, p<.001), these terms were retained in subsequent models. A series of models explored whether the discontinuity in COG slope varied by treatment condition (CBT vs. COMB), age (children vs. adolescents), or gender (boys vs. girls). Results from these moderator analyses, were all non-significant (all p values >.05) and hence these parameters were not retained.
Model F (Table 3) added a discontinuity in slope following the onset of exposure exercises (EXP) by including both its fixed and random effects. Comparing the deviance statistic to the previous model (Model F - Model D) revealed a statistically significant improvement in model fit (X2(5) =71.3, p<.001) and a significant discontinuity in slope for EXP (0.055, p<.017). These findings indicate that the initial difference between CGAS response slopes before and after cognitive restructuring (COG) was followed by a second linear discontinuity before and after exposure exercises (EXP). To evaluate whether the magnitude of this discontinuity varied significantly between participants, the three variance components associated with EXP were removed in Model G. Because Model G’s fit was significantly worse (X2(4) =62.8, p<.001), the terms associated with EXP’s variance components were retained in all subsequent models. Additional multilevel models for change (not shown in Table 3) explored moderators of EXP and found that the mean post-EXP slopes varied significantly by treatment condition (CBT vs. COMB; 0.136, p<.001). There were no significant differences in the mean post-EXP slopes by participant age (children vs. adolescents; p=.062) or participant gender (males vs. females; p=.574).
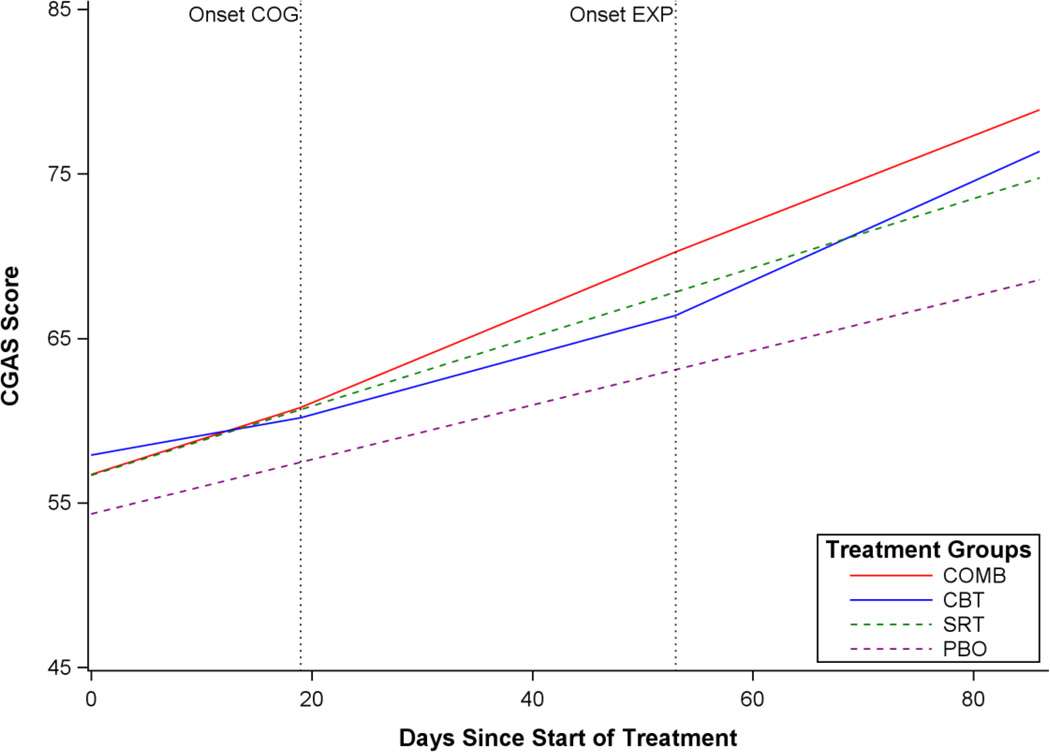
Detailed results of fitting Model F to the CAMS clinician CGAS data (n=488), with the inclusion of the significant moderator for post-EXP slope, are available in supplemental materials online (Supplemental Table 2). Figure 3 presents CGAS trajectories for four prototypical participants from each treatment condition. Before the onset of cognitive restructuring, the average monthly rate of improvement on the therapist-rated CGAS for participants in COMB was 6.4 points and 3.6 points for those in CBT. Upon the onset of cognitive restructuring, this average monthly rate of improvement increased to 8.4 points for those in COMB (approximately 30% faster than the corresponding rate during the previous period) and 5.5 points for those in CBT (approximately 53% faster than the corresponding rate during the previous period). However, upon the onset of exposure exercises, the average monthly rate of improvement decreased to 7.9 points for those in COMB (approximately 6% slower than the corresponding rate during the previous period) yet increased to 9.1 points for those in CBT (approximately 65% faster than the corresponding rate during the previous period). The statistically significant variance components for COG and EXP suggest that there is substantial variability from participant to participant in the rate of CGAS change following the onset of cognitive restructuring and exposure exercises.
Figure 3.
Estimated population mean CGAS growth curve trajectory by CAMS treatment condition following the start of CBT cognitive restructuring and exposure exercises.
Note: Onset COG = onset of cognitive restructuring component of CBT; Onset EXP = onset of exposure exercises component of CBT.
Outcomes Measured Monthly
We next present analyses of change in outcomes that are theoretically linked to specific components of CBT. Similar to the previous section, each question was addressed by fitting a series of multilevel models for change. However, outcomes assessed were those collected monthly during acute treatment and, in each model, the presence or absence of only one discontinuity was evaluated. Details from non-significant models are not presented.
Does the onset of relaxation training lead to a significant decrease in self-reported physical symptoms of anxiety?
This question was addressed by fitting a series of multilevel models for change to the monthly PSC Total Score. As in prior models, variables that contributed to improvement in model fit relative to the baseline model were retained. The first model added a discontinuity in slope following the onset of relaxation training (RLX) by including both fixed and random effects for RLX. Comparing this model’s deviance statistic to that of the baseline model revealed a non-significant improvement in model fit (X2(4) =1.2, p=.677) and a non-significant estimate for the fixed effects of RLX (−0.006, p=.69). These findings suggest that the average rate of change in PSC growth curves did not change significantly after the onset of relaxation training. To explore whether relaxation training might result in a rate of change in the mean PSC Total score that occurs later in treatment (e.g., a delayed impact on growth curves), a quadratic change trajectory was evaluated. Results from this model were also non-significant (p=.315).
Does the onset of cognitive restructuring lead to a significant difference in the average rate of change in children’s anxious self-talk?
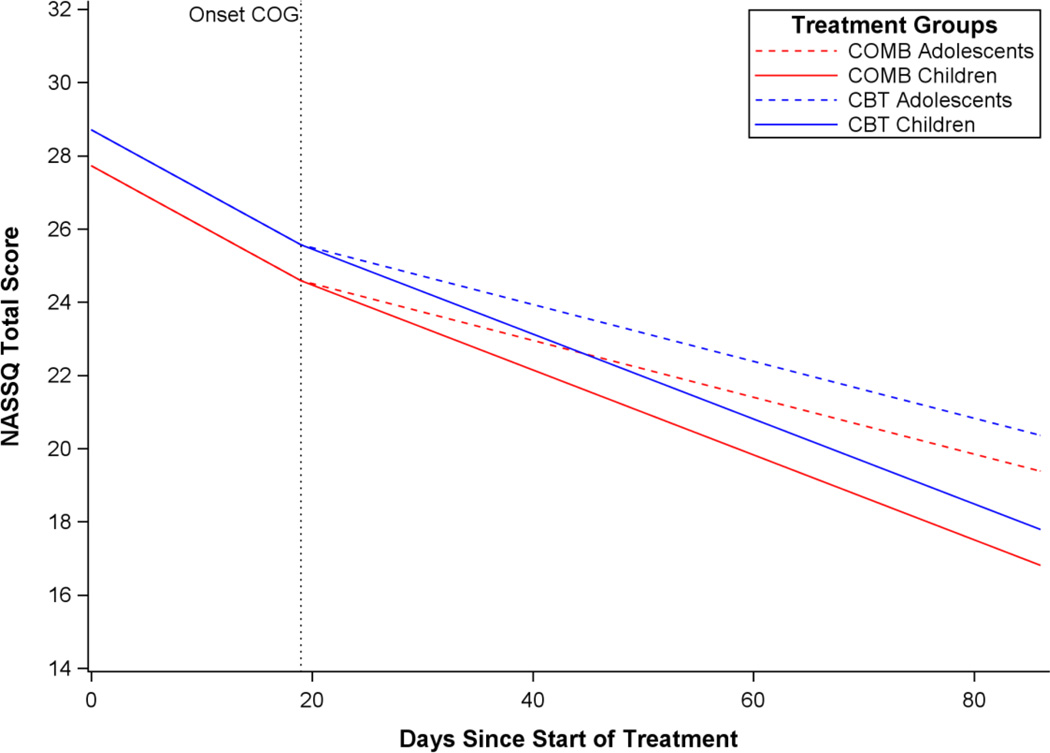
This longitudinal model for change assessed whether cognitive outcomes (i.e., NASSQ) displayed a discontinuity in slope following the introduction of the cognitive restructuring component of CBT. The first model added a discontinuity in slope following the onset of cognitive restructuring (COG) by including both fixed and random effects for COG. Comparing this model’s deviance statistic to that of the baseline model revealed a significant improvement in model fit (X2(4)=19.8, p<.001) and a significant estimate for the fixed effects of COG (0.061, p<.001). These findings suggest that the average rate of change in NASSQ growth curves does indeed display a significantly different slope following COG such that the rate of change decreased. To evaluate whether the magnitude of this discontinuity varied significantly between participants, the next model removed the three variance components associated with COG. Because this model’s fit did not change significantly (X2(3) = 0.6, p=.896), the terms associated with COG’s variance components were removed from all subsequent models. Additional models explored potential moderators of the effects of COG on NASSQ trajectories. Analyses found that the mean post-COG slope varied significantly by age (children vs. adolescents; 0.038, p<.016). There were no significant differences in the post-COG slopes between CBT containing treatment conditions (CBT vs. COMB; p=.651) and participant gender (males vs. females; p=.848).
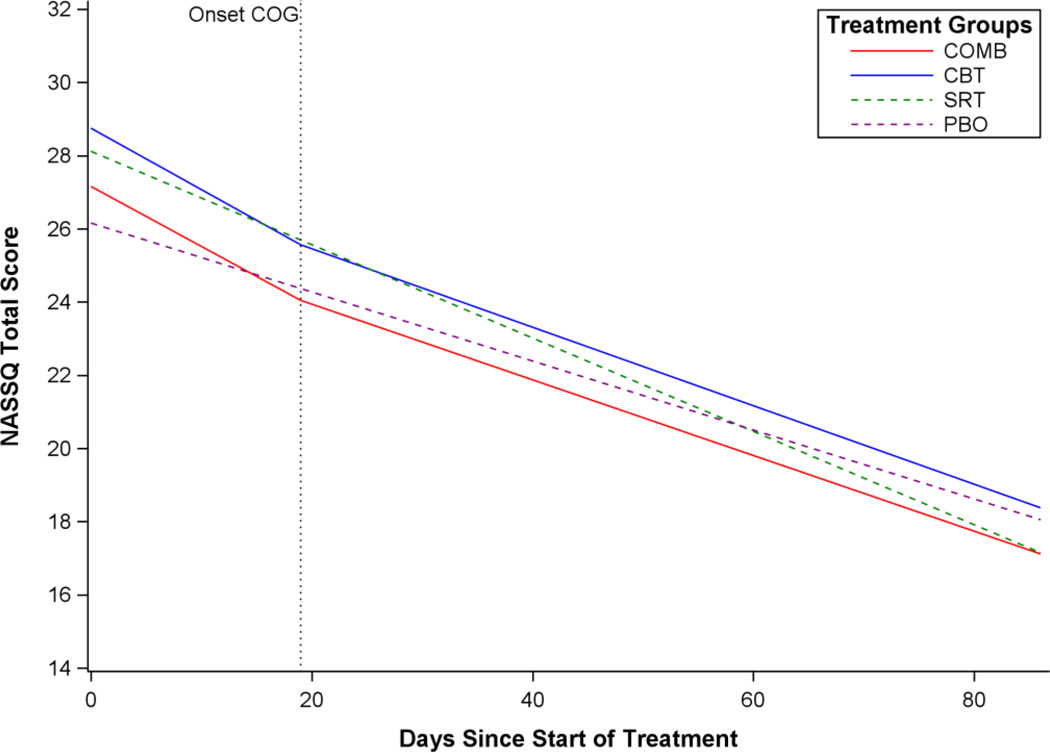
Figure 4 displays the estimated NASSQ population mean growth curve trajectory by treatment condition. Further inspection of this model suggests that before onset of cognitive restructuring, the average monthly rate of improvement on the NASSQ for participants in COMB was −4.9 points and −5.0 points for those in CBT. Upon the onset of cognitive restructuring, this average monthly rate of improvement slowed to −2.3 points for adolescents in COMB (approximately 54% slower than the corresponding rate during the previous period) and −2.4 points for adolescents in CBT (approximately 53% slower than the corresponding rate during the previous period). Children in both treatment conditions showed a less dramatic decrease in the rate of change following the onset of cognitive restructuring, with children in COMB slowing to −3.4 points per month (approximately 31% slower than the corresponding rate during the previous period) and −3.5 points per month for those in CBT (approximately 30% slower than the corresponding rate during the previous period). Counter to our expectations, these results suggest that the onset of cognitive restructuring resulted in an overall slowing of the monthly rate of change in NASSQ trajectories. However, this rate of slowing across both COMB and CBT was less pronounced in children when compared to adolescents. The statistically non-significant variance component for COG indicates that there is little variability from participant to participant in the average rate of change in NASSQ trajectories following the onset of cognitive restructuring.
Figure 4.
Estimated NASSQ population mean growth curve trajectories by CAMS treatment condition following the start of cognitive restructuring.
Note: Onset COG = onset of cognitive restructuring component of CBT.
Does the onset of exposure tasks lead to a difference in the average rate of change in children’s avoidance behavior?
This longitudinal model for change assessed whether avoidance behavior (as measured by the PARS) displayed a discontinuity in slope following the introduction of moderately challenging CBT exposure exercises. The first model explored added a discontinuity in slope to the “baseline model” following the onset of exposure exercises (EXP) by including both fixed and random effects for the regression parameter EXP. Comparing this model’s deviance statistic to that of the baseline model revealed a non-significant improvement in model fit (p=.147) and a non-significant estimate for the fixed effects of EXP (p=.247). These findings suggest that the average rate of change in avoidance scores did not display a significant discontinuity in slopes after the onset of exposure exercises. To explore whether exposure exercises might result in delayed rate of change, a quadratic change trajectory was evaluated. Results from this model were also non-significant (p=.492). These combined findings suggest that the estimated average PARS avoidance growth trajectories did not display an immediate or delayed change in slope after the onset of exposure exercises.
Discussion
Are specific components of CBT for youth anxiety followed by significant improvement in the rate of progress moving forward in treatment? The present findings indicate that two techniques make clear contributions to improvement on measures of overall anxiety symptom severity and global functioning. Indeed, the introduction of both cognitive restructuring and exposure tasks was followed by significant acceleration in the rate of progress in treatment, a finding that emerged across therapist ratings of overall symptom severity and global functioning. By contrast, the introduction of relaxation training appeared to do relatively little to alter the subsequent course of treatment. Counter to expectations, none of these techniques altered the trajectory of improvement within the specific domain of anxiety that it was intended to address (e.g., somatic symptoms, anxious self-talk, or avoidance behavior).
Taken together, these findings lend empirical support to two central aspects of cognitive behavioral theory of anxiety. First, this framework suggests that improvements in anxiety follow shifts in maladaptive thinking patterns (Beck, 1976; Kendall, 2012). The present findings support this notion, indicating that youth introduced to the practice of cognitive restructuring evidenced accelerated improvements in anxiety symptom severity and overall functioning moving forward in treatment. They converge with a prior report indicating that cognitive restructuring produced rapid decreases in both cognitive errors and overall anxiety in adolescents with panic disorder (Micco, Choate-Summers, Ehrenreich, Pincus, & Mattis, 2007), and they are consistent with data indicating that changes in self-talk (reduced negative anxious thinking) mediate therapy-produced gains (Kendall & Treadwell, 2007). Together, they buttress the evidence supporting the role of cognitive change strategies in the treatment of youth anxiety.
Exposure tasks are also central to CBT treatment, as cognitive behavioral theory also suggests that anxiety is maintained by avoidance of anxiety provoking stimuli. The present findings support the merits of exposure: across both measures of anxiety symptom severity and global impairment, the introduction of exposure tasks was followed by significant improvement in the rate of treatment progress moving forward, even when the contribution of prior treatment techniques was taken into account. Consistent with theoretical and empirical accounts (Foa & Kozak, 1986; Rapee et al., 2000; Treadwell & Kendall, 1996) and prior trials (e.g., Kendall et al., 1997) (e.g., Eisen & Silverman, 1993; Nakamura et al., 2009), improvement in CBT for child anxiety occurs following exposure tasks.
The impact of exposure on treatment trajectory was moderated by both age and treatment condition. Younger participants appeared to benefit more from exposure tasks, with steeper rates of improvement following its implementation compared to adolescents. These data are consistent with reports of impaired extinction learning in adolescence that may complicate the use of exposure during this period of development (Casey & Walkup, 2013). With respect to treatment condition, the trajectories for youth in the COMB condition demonstrated a clear advantage over the CBT, SRT, and PBO monotherapies on nearly all outcome measures, a finding that is consistent with the main CAMS efficacy findings (Walkup et al., 2008) as well as those from other clinical trials (TADS Team, 2004). However, the present findings suggest that the rate of improvement following the onset of exposure tasks was more pronounced for youth in the CBT only condition. It may be the case that, in the absence of other intervention (i.e., medication), each component of the CBT package—and exposure in particular—matters that much more. In either event, the substantial variability in slopes (i.e., the rate of improvement was not the same for all participants) following the onset of exposure tasks suggests that other moderators may be operative.
Somewhat surprisingly, we found that the introduction of exposure tasks did not alter the rate of change in avoidance behavior moving forward. It may be the case that changes in avoidance behavior occur gradually—even in the context of exposure—a notion that undergirds stepwise approaches to exposure treatment. It may also be the case that the single-item subscale used to assess avoidance behavior in this study did not adequately capture the construct or that the measurement timeline did not allow a sufficient window of time for change to occur.
Likewise, the finding that improvement in self-reported cognitive distortions slowed (rather than accelerated) following the introduction of cognitive restructuring exercises was also unexpected. One explanation is that treatment exercises geared toward helping youth to recognize anxious self-talk had the effect of making them more aware and in turn, more accurate, when completing measures of cognitive distortions at subsequent time-points. Certainly, adolescent participants demonstrated more pronounced slowing in their progress on measures of cognitive distortions compared to younger participants. These older participants, by virtue of their developmental status, may have been better poised to reflect on and identify maladaptive patterns of thinking in turn elevating their self-reported cognitive distortions.
The contribution of relaxation training appeared to be limited. Although other studies identify relaxation as a worthy intervention (Silverman et al., 1999; Piacentini et al., 2011), within the present study, relaxation training had a limited impact on the trajectory of improvement on measures of somatic symptoms, overall anxiety, or global functioning. It may be that the dose of relaxation, within a comprehensive program, is lower than that needed to make a significant impact. Alternatively, it may be the case that relaxation exercises gain further value when applied in the context of exposure tasks.
Several potential limitations deserve mention. First, CBT protocols involve an integration of multiple therapeutic components, and these analyses examined only three of them. The contribution of other strategies (e.g., problem solving) requires further investigation. Second, although the present models examined whether the onset of specific components resulted in a change in outcome trajectories, the statistical approach cannot address the unique and independent contribution of each CBT component. This is because, by design of the CBT intervention, all participants who received CBT received relaxation training, followed by cognitive restructuring, which was followed by exposure exercises, in this order. No participant received only relaxation training or only cognitive restructuring, or any other ordered combination. Thus, each participant’s trajectory reflects the combined impact of this sequence of treatments. The ability to make statements about the unique contribution of each CBT component or to compare the utility of different components will require methodology different from that employed in CAMS (e.g., MOST designs; Collins, Murphy, Nair, & Strecher, 2005). Finally, although the inclusion of therapist ratings bolsters confidence in the findings, particularly because they show a high degree of correspondence with blind IE ratings (Lewin et al., 2012) and because they could be tied directly to the introduction of treatment components; we note that their lack of blindness—along with that absence of blindness in youth reports—remains an issue.
The present findings provide a valuable glimpse into trajectories of improvement for youngsters participating in CBT for anxiety. Further research aimed at identifying the critical ingredients of multi-component therapies is needed to improve the overall potency of therapy and to promote more personalized approaches. Such work might explore strategies for selecting and sequencing intervention components in order to meet a particular child’s needs. Although most multicomponent interventions prescribe a several-month course of therapy, service use data suggest high rates of premature termination, with an average course of therapy as brief as 3–4 visits in community-based settings (Brookman-Frazee, et al, 2008). Accordingly, identification of the active ingredients of multi-component interventions may facilitate the development of more efficient, services-relevant therapies. The current results provide further support for the value of both cognitive restructuring and exposure techniques as targets for both practice and further research, and they point to the latter as a critical ingredient in successful CBT for child anxiety.
Supplementary Material
Figure 5.
Estimated NASSQ population mean growth curve trajectories for COMB and CBT by participant age.
Note: Onset COG = onset of cognitive restructuring component of CBT.
Public Health Significance.
The present findings suggest that cognitive restructuring and exposure tasks are critical components of CBT for youth anxiety but that relaxation training may have relatively less impact. These findings may be used to inform future efforts to make treatment more potent and efficient.
Acknowledgments
This research was supported by NIMH career development awards to Dr. Peris (K23 MH085058) and Dr. Compton (K23-MH075843). CAMS was supported by grants U01 MH64088, to Dr. Piacentini; U01 MH064003, to Dr. Compton; U01 MH63747, to Dr. Kendall; U01 MH64003, to Dr. Birmaher; U01 MH64092, to Dr. Albano; U01 MH64107, to Dr. March; and U01 MH064089, to Dr. Walkup from the National Institute of Mental Health (NIMH). Sertraline and matching placebo were supplied free of charge by Pfizer.
The views expressed in this article are those of the authors and do not necessarily represent the official views of the NIMH, the National Institutes of Health, or the Department of Health and Human Services.
The authors wish to acknowledge all of the therapists, interviewers, research coordinators, co-investigators and consultants who were part of this study. Special gratitude is also extended to the children and families who participated in this research.
Appendix
To answer the questions posed in this manuscript, we fit a series of growth curve models for change (time nested within individuals) that included slope deflections (based on a time-varying treatment). Each deflection marked the onset of when a particular component of CBT was introduced during the course of the trial. In CAMS, CBT participants were measured weekly by their therapist for a total of 12 possible assessment points. Participants were also assessed monthly by an independent evaluator (IE) for a total of 4 possible assessment points. The outcomes included in the present analyses were the CGI-S and CGAS (which were completed by the therapist), the PSC and NASSQ (which were self-reports and completed by each participant), and the PARS (which was completed by the IE). First, for each outcome, we fit the following growth curve model. The level-1 model (for time) was:
where DAYSij denotes days since baseline. In this level-1 model, change is a linear function of DAYS; each individual has his or her own intercept π0i (initial status) and growth π1i parameter (slope).
The level-2 models (for the individual intercept and growth parameters) were:
where SITE1, SITE2, SITE3, SITE4, and SITE5 are dummy indicators for study site (with SITE6 serving as the referent category); and CBT, SRT, and PBO are dummy indicators for the randomized treatment condition (with COMB serving as the referent category). Substituting the two level-2 equations into the level-1 equation provides the following composite (reduced-form) model:
The structural components of the level-2 submodel contain 13 fixed effects: (1) the intercept: γ00; (2) the main effect of SITE on initial status: γ01, γ02, γ03, γ04, γ05; (3) the main effect of TREATMENT CONDITION on initial status: γ06, γ07, γ08; (4) the main effect of DAYS: γ10; and (5) the effect of TREATMENT CONDITION on rates of change: γ11, γ12, γ13. The model also contains four variance components: (1) the level-1 residual variance: , (2) the level-2 variance of initial status: , (3) the level-2 variance of rate of change: , and (4) the level-2 covariance of initial status and rate of change: σ01.
Second, for each outcome, we built upon the above model in the following way. To evaluate a level-1 individual growth trajectory with a deflection in slope following the onset of a specific CBT component, we added a second time varying predictor to the level-1 model.
Before participant i receives a specific component, POST-DAYS is set to 0. On the day when the specific CBT component is introduced, this predictor remains 0. However, its values start to climb in concert with DAYS from that point forward. The modified level-1 equation still has the same intercept as the earlier equation but now it has two slopes (i.e., DAYS and POST-DAYS). The second slope term, π2i, captures the deflection in slope attributable to POST-DAYS on outcomes (measured from onset of the CBT component). Models where multiple discontinuities were evaluated were simply an extension of the above model by including a second or third time varying predictor into the level-1 model. These additional time varying predictors captured the deflection in the overall slope attributed to the onset of the new treatment component controlling for the prior component(s). Please note that for simplicity, the predictor POST-DAYS refers to the generic onset of a given CBT treatment component. In the models presented in the manuscript, the onset of CBT relaxation training was referred to at RLX, the onset of cognitive restructuring component of CBT was referred to as COG, and the onset of CBT exposure exercises was referred to as EXP.
Third, for each outcome, to assess whether the post-component slopes varied by key moderators (CBT vs. COMB, children vs. adolescents, males vs. females), subsequent models evaluated the effect of each moderator on POST-DAYS rate of change by including a cross-level interaction between the moderator in question and the post-component slope (i.e., POST-DAYS). The level-2 models (for the individual intercept and growth parameters) for models that included a moderator for the second time varying predictor were:
where MODERATOR is a dummy coded indicator for participant age (children vs. adolescent), gender (male vs. female), or CBT treatment containing condition (CBT vs. COMB). Substituting the two level-2 equations into the level-1 equation provides the following composite (reduced-form) model:
Comparisons between nested models were evaluated by assessing the significance of the change in deviance statistic (which follows a chi-square distribution with dfs associated with the difference in dfs between the two models), significance of the fixed effect parameters, and the improvement in model fit by including additional variance components.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: a controlled trial. Journal of Consulting and Clinical Psychology. 1996;64:333–342. doi: 10.1037//0022-006x.64.2.333. [DOI] [PubMed] [Google Scholar]
- Barrios BA, O'Dell SL. Fears and anxieties. In: Mash EJ, Barkley RA, editors. Treatment of childhood disorders. 2nd ed. New York: Guilford Press; 1998. pp. 249–337. [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. New York: New American Library; 1976. [Google Scholar]
- Brookman-Frazee L, Haine RA, Gabayan EN, Garland AF. Predicting frequency of treatment visits in community-based youth psychotherapy. Psychological Services. 2008;5:126–138. doi: 10.1037/1541-1559.5.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Walkup J, Drysdale AT, Hartley CA, Patwell SS, Ruberry EJ, Somerville LH, Compton SN, Lee FS. Fear and anxiety from principle to practice: Implications for when to treat youth with anxiety disorders. Biological Psychiatry. 2013;75:e19–e20. doi: 10.1016/j.biopsych.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambless DL, Hollon SD. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden E, Weisz JR. Identifying and selecting the common elements of evidence based interventions: A distillation and matching model. Mental Health Services Research. 2005;7:5–20. doi: 10.1007/s11020-005-1962-6. [DOI] [PubMed] [Google Scholar]
- Compton SN, Walkup J, Albano AM, Piacentini JC, Birmaher B, Sherrill J, Ginsburg G, Rynn M, McCracken J, Waslick B, Iyengar S, Kendall PC, March J. Child/Adolescent Anxiety Multimodal Study (CAMS): Rationale, design, and methods. Child and Adolescent Psychiatry and Mental Health. 2010;4:1–15. doi: 10.1186/1753-2000-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis TE, Ollendick TH. Empirically supported treatments for specific phobia in children: Do efficacious treatments address the components of a phobic response? Clinical Psychology: Science and Practice. 2005;12:144–160. [Google Scholar]
- Eisen AR, Silverman WK. Should I relax or change my thoughts? A preliminary examination of cognitive therapy, relaxation training, and their combination with overanxious children. Journal of Cognitive Psychotherapy. 1993;7:265–279. [Google Scholar]
- Foa E, Kozac M. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:450–472. [PubMed] [Google Scholar]
- Guy W. Clinical global impressions ECDEU assessment manual for psychopharmacology. Rockville, MD: National Institute for Mental Health; 1976. [Google Scholar]
- Ilardi SS, Craighead WE. The role of nonspecific factors in cognitive-behavior therapy for depression. Clinical Psychology: Science and Practice. 1994;1:138–156. [Google Scholar]
- Hudson JL. Mechanisms of change in cognitive behavior therapy for anxious youth. Clinical Psychology: Science and Practice. 2005;12:161–165. [Google Scholar]
- Kazdin A. Psychotherapy for children and adolescents: Directions for research and practice. New York: Oxford University Press; 2000. [Google Scholar]
- Kendall PC. Treating anxiety disorders in youth. In: Kendall PC, editor. Child and adolescent therapy: Cognitive-behavioral procedures. 4th ed. New York: Guilford Press; 2012. [Google Scholar]
- Kendall PC, Compton SN, Walkup JT, Birmaher B, Albano AM, Sherrill J, Gosch E, Keeton C, Bergman L, Sakolsky D, Suveg C, Iyengar S, March J, Piacentini J. Clinical characteristics of anxiety disordered youth. Journal of Anxiety Disorders. 2010;24:360–365. doi: 10.1016/j.janxdis.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Gosch EA, Furr JM, Sood E. Flexibility within fidelity. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:987–993. doi: 10.1097/CHI.0b013e31817eed2f. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel S, Southam-Gerow M, Henin A, Warman M. Therapy for youth with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:366–380. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hedtke KA, Aschenbrand SG. Anxiety disorders. In: Wolfe DA, Mash EJ, editors. Behavioral and Emotional Disorders in Adolescents: Nature, Assessment, and Treatment. New York: Guilford; 2006. pp. 259–299. [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76:282–297. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Treadwell K. The role of self-statements as a mediator in treatment for youth with anxiety disorders. Journal of Consulting and Clinical Psychology. 2007;75:380–389. doi: 10.1037/0022-006X.75.3.380. [DOI] [PubMed] [Google Scholar]
- Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:404–411. doi: 10.1097/00004583-199804000-00018. [DOI] [PubMed] [Google Scholar]
- Lewin AB, Peris TS, De Nadai AS, McCracken JT, Piacentini J. Agreement between therapists, parents, and independent evaluators on clinical improvement in pediatric obsessive compulsive disorder. Journal of Consulting and Clinical Psychology. 2012;80:1103–1107. doi: 10.1037/a0029991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micco JA, Choate-Summers ML, Ehrenreich JT, Pincus DB, Mattis SG. Identifying efficacious treatment components of panic control treatment for adolescents: A preliminary investigation. Child and Family Behavior Therapy. 2007;29:1–23. [Google Scholar]
- Nakamura BJ, Pestle SL, Chorpita BF. Differential sequencing of cognitive-behavioral techniques for reducing child and adolescent anxiety. Journal of Cognitive Psychotherapy. 2009;23:114–135. [Google Scholar]
- Piacentini J, Bergman RL, Chang S, Langley A, Peris T, Wood JJ, McCracken J. Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:1149–1161. doi: 10.1016/j.jaac.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM, Wignall A, Hudson JL, Schniering CA. Evidence-based treatment of child and adolescent anxiety disorders. Oakland, CA: New Harbinger; 2000. [Google Scholar]
- Ronan KR, Kendall PC, Rowe M. Negative affectivity in children: Development and validation of a self-statement questionnaire. Cognitive Therapy and Research. 1994;18:509–528. [Google Scholar]
- RUPP Anxiety Study Group. The Pediatric Anxiety Rating Scale (PARS): Development and psychometric properties. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:1061–1069. doi: 10.1097/00004583-200209000-00006. [DOI] [PubMed] [Google Scholar]
- Ryan SE, Porth LS. Gen. Tech. Rep. Fort Collins, CO: U.S. Department of Agriculture, Forest Service, Rocky Mountain Research Station; 2007. A tutorial on the piecewise regression approach applied to bedload transport data; p. 41. RMRS-GTR-189. [Google Scholar]
- Seligman LD, Ollendick TH. Cognitive-behavioral therapy for anxiety disorders in youth. Child and Adolescent Psychiatric Clinics of North America. 2011;20:217–238. doi: 10.1016/j.chc.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A children’s global assessment scale (CGAS) Archives of General Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Rabian B, Serafini LT. Contingency management, self-control, and education support in the treatment of childhood phobic disorders: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 1999;67:675–687. doi: 10.1037//0022-006x.67.5.675. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis. Oxford, UK: Oxford University Press; 2003. [Google Scholar]
- Sood ED, Kendall PC. Assessing anxious self-talk in youth: The negative affectivity self-statement questionnaire-Anxiety scale. Cognitive Therapy and Research. 2007;31:603–618. [Google Scholar]
- TADS Study Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. Journal of the American Medical Association. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- Treadwell KRH, Kendall PC. Self-talk in youth with anxiety disorders: States of mind, content specificity, and treatment outcome. Journal of Consulting and Clinical Psychology. 1996;64:941–950. doi: 10.1037//0022-006x.64.5.941. [DOI] [PubMed] [Google Scholar]
- Walkup J, Albano AM, Piacentini JC, Birmaher B, Compton S, Sherrill J. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. The New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.