Abstract
Background/Aims:
Endoscopic papillary balloon dilation (EPBD) is a possible alternative to endoscopic sphincterotomy (EST) for common bile duct (CBD) stones. To date, 10- and 8-mm EPBD have not been fully compared.
Patients and Methods:
Patients who underwent EPBD for CBD stones at two Japanese tertiary care centers between May 1994 and January 2014 were identified. Matched pairs with 10- and 8-mm EPBD were generated. Short- and long-term outcomes were compared between the two groups.
Results:
A total of 869 patients were identified (61 and 808 patients for 10- and 8-mm EPBD, respectively), and 61 well-balanced pairs were generated. The rate of complete stone removal within a single session was higher in the 10-mm EPBD group than in the 8-mm EPBD group (69% vs. 44%, P < 0.001), and use of lithotripsy was less frequent in the 10-mm EPBD group (23% vs. 56%, P < 0.001). The rates of post-ERCP pancreatitis were similar between the 10- and 8-mm EPBD groups (11% vs. 8%). Cumulative biliary complication-free rates were not statistically different between the two groups: 88% [95% confidence interval (CI): 79–97%] and 94% (95% CI: 88–100%) at 1 year and 69% (95% CI: 56–85%) and 80% (95% CI: 69–93%) at 2 years in the 10- and 8-mm EPBD groups, respectively. In the 10-mm EPBD group, ascending cholangitis was not observed, and pneumobilia was found in 5% of cases during the follow-up period.
Conclusions:
EPBD using a 10-mm balloon for CBD stones is safe and more effective than 8-mm EPBD. The sphincter function is highly preserved after 10-mm EPBD.
Keywords: Common bile duct stone, endoscopic retrograde cholangiopancreatography, lithotripsy, pancreatitis, papillary balloon dilation
Endoscopic sphincterotomy (EST) is widely utilized as a first-line treatment option for common bile duct (CBD) stones.[1,2] However, potentially fatal complications associated with EST, such as bleeding and perforation, are not uncommon.[3,4] Furthermore, EST can cause a permanent loss of the sphincter function and resultant duodenobiliary reflux, putting patients at increased risk of long-term biliary complications including biliary stone recurrence, cholecystitis, and ascending cholangitis. Endoscopic papillary balloon dilation (EPBD) is a possible alternative to EST,[5,6,7,8,9] particularly in patients with coagulopathy, for example, those on antithrombotic agents,[10,11,12] or with liver cirrhosis,[13] or chronic renal failure on hemodialysis.[14] One of the major advantages of EPBD over EST is that EPBD potentially preserves the sphincter function[15,16,17,18] and, therefore, might reduce the risk of long-term biliary complications. Recent studies have shown a lower rate of stone recurrence after EPBD as compared with EST.[19,20,21,22]
EPBD is usually carried out using a balloon dilation catheter with diameter up to 10 mm. Theoretically, the dilation of the ampulla using a larger balloon can ease the subsequent removal of CBD stones, with the expectation of a higher rate of successful stone removal with a lower rate of mechanical lithotripsy use. Conversely, larger EPBD may raise a legitimate concern of a greater injury to the ampulla, leading to an increased risk of procedure-related complications and stone recurrence. To date, the impact of the balloon diameter used in EPBD on the safety and efficacy for CBD stone extraction has been rarely investigated,[23] and the effectiveness of 10-mm EPBD remains to be elucidated.
In this retrospective study, we compared the short- and long-term outcomes of 10- and 8-mm EPBD for extraction of CBD stones. This study also included the long-term evaluation of the sphincter function after 10-mm EPBD.
PATIENTS AND METHODS
Study design
This study aimed to compare 10- and 8-mm EPBD to facilitate endoscopic removal of CBD stones, and was designed as a retrospective matched cohort study based on prospectively collected data. After matching patients receiving 10-mm EPBD with those receiving 8-mm EPBD considering important baseline characteristics, we compared technical success, procedure-related complications, and long-term outcomes between the groups.
This study was approved by the institutional review board in each institution and conducted according to the guidelines in the Helsinki Declaration.
Selection of patients and generation of matched pairs
From prospectively maintained databases, we identified consecutive patients who underwent 10- or 8-mm EPBD for CBD stones at the University of Tokyo Hospital and Japanese Red Cross Medical Center between May 1994 and January 2014. A balloon dilation catheter of 10 mm in diameter was introduced into our practice in March 2010. Exclusion criteria were as follows: (1) A history of EST or EPBD, (2) precut sphincterotomy or EST performed combined with EPBD, (3) previous gastrectomy with Billroth-II or Roux-en-Y reconstructions, (4) active pancreatitis at the time of endoscopic retrograde cholangiopancreatography (ERCP), (5) the diameter of CBD <8 mm, and 6) concomitant pancreatobiliary malignancy. Written informed consent for EPBD and follow-up evaluation was obtained from all patients before the procedure.
We matched patients receiving 10-mm EPBD one-to-one with those receiving 8-mm EPBD for age, sex, stone diameter, stone number, bile duct diameter, American Society of Anesthesiologists Physical Status Classification System score,[24] and gallbladder in situ.
Procedures of EPBD and stone removal
A side-viewing duodenoscope (JF-240, JF-260V, or TJF-260V; Olympus Optical, Tokyo, Japan) was inserted under moderate sedation. When selective biliary cannulation was achieved and CBD stones were delineated by cholangiography, the decision to perform EPBD was made. A balloon dilation catheter with a diameter of 8 or 10 mm [Eliminator; Bard Interventional Products, Billerica, MA, USA (8 mm) or Hurricane RX; Boston Scientific Corp, Natick, MA, USA (8 and 10 mm)] was inserted over the prepositioned guidewire and positioned across the papilla. Subsequently, the balloon was inflated slowly (1–2 min) with diluted contrast until the waist disappeared (the pressure was maintained not to exceed 8 atm). The pressure was maintained for 2 min initially, and thereafter, the shorter duration time of 15 s was adopted based on our previous study.[25] EPBD has been carried out with longer duration time of 5 min since its effectiveness was reported in 2010.[26]
After deflation of the balloon dilation catheter, stones were removed using a four- or eight-wire retrieval basket and/or a retrieval balloon catheter. Endoscopic mechanical lithotripsy (EML) was used to fragment large stones, as needed. Electrohydraulic lithotripsy or extracorporeal shock wave lithotripsy was used for difficult stones that could not be fragmented successfully by EML. Complete stone removal was defined as the clearance of bile duct stones confirmed by balloon-occluded cholangiography or intraductal ultrasonography.
Evaluation of short-term complications (within 30 days of EPBD)
In order to monitor procedure-related complications, each patient was routinely hospitalized at least one night after the procedure. Symptoms were continuously monitored, and a blood test including amylase was done 18–24 h after the procedure. Abdominal radiograph, ultrasound, and/or computed tomography were performed, as necessary. Short-term complications associated with EPBD were diagnosed and graded according to the consensus guidelines.[27] Therein, post-ERCP pancreatitis was defined as typical abdominal pain along with an elevated serum amylase level (≥3 times the upper limit of normal level in each institution) at more than 24 h after the procedure. The severity of pancreatitis was categorized as follows: Mild, requirement or prolongation of hospitalization for 2–3 days; moderate, hospitalization for 4–10 days; and severe, hospitalization >10 days, complicated pancreatitis, or requirement of interventions.
Evaluation of long-term outcomes (more than 30 days after EPBD)
All patients who had complete stone removal were followed up at the outpatient clinic in each institution at an interval of 6–12 months after discharge and were included in evaluation of long-term outcomes. In evaluation of long-term outcomes, the patients with failed stone removal and the corresponding matched patients were excluded. At each visit, the patients had physical examinations, blood tests, and abdominal imaging studies [ultrasonography or magnetic resonance cholangiopancreatography (MRCP)]. Other relevant examinations (e.g., endoscopic ultrasound, computed tomography, MRCP, and/or ERCP) were performed, if indicated. Biliary complications during the follow-up period were defined as a composite endpoint of bile duct stone recurrence, cholecystitis, ascending cholangitis, or liver abscess.
Pneumobilia[17] and ascending cholangitis during the follow-up period were analyzed as an indicator for the loss of the sphincter function to investigate whether larger EPBD could affect the preservation of the sphincter function.
Statistical analysis
Continuous variables are expressed as medians and interquartile ranges (IQRs), and categorical variables as numbers and percentages of patients. Variables considered in matching of patients were compared between the matched groups using the Wilcoxon rank-sum test for continuous variables and the Chi-square or Fisher's exact tests for categorical variables. All other variables were compared using the Wilcoxon signed-rank test for continuous variables and the McNemar test for categorical variables. Time to biliary complications was defined as the period between complete stone removal and biliary complications. Biliary complication-free survival was estimated using the Kaplan–Meier product-limit method and compared using the log-rank test.
All statistical analyses were performed using R software, version 2.15.1 (R Development Core Team: http://www.r-project.org) and its survival package, and matched pairs were generated based on optimal matching algorithm using its optmatch package. A two-sided P < 0.05 was considered statistically significant in all analyses.
RESULTS
Patient characteristics
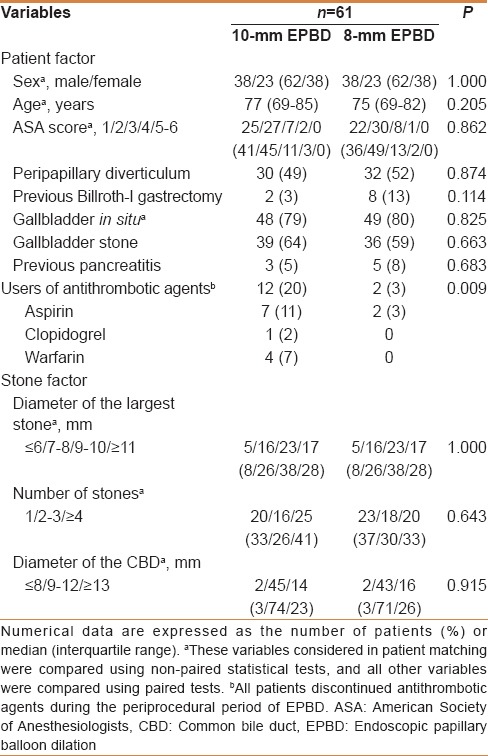
The flowchart for matching patients receiving 10-mm EPBD with those receiving 8-mm EPBD is illustrated in Figure 1. Among 1227 consecutive patients without a history of EST or EPBD who underwent EPBD for CBD stones, we selected 869 eligible patients (61 for 10-mm EPBD and 808 for 8-mm EPBD). As compared with the patients with 8-mm EPBD, those with 10-mm EPBD in this cohort were older [77 (IQR: 69–85) and 72 (IQR: 63–79) in the 10- and 8-mm EPBD groups, respectively; P < 0.001] and were associated with a larger diameter of the largest stone [10 (IQR: 8–11) and 7 (IQR: 5–10), P < 0.001] and a larger number of stones [3 (IQR: 1–6) and 2 (IQR: 1–3), P < 0.001]. These imbalances between the unmatched 8- and 10-mm EPBD groups inferred treatment selection biases. All 61 patients with 10-mm EPBD (the 10-mm EPBD group) were successfully matched with the same number of patients with 8-mm EPBD (the 8-mm EPBD group). The demographic profiles were well balanced between the matched groups, except that the 10-mm EPBD group was more likely to take antithrombotic agents as compared with the 8-mm EPBD group [Table 1].
Figure 1.
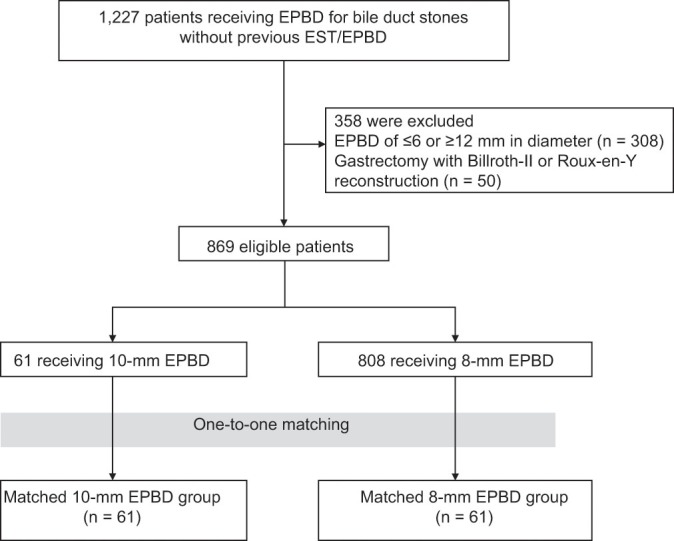
Flowchart for generating 61 matched pairs with 10- or 8-mm EPBD for extraction of bile duct stones. Patient matching was done using optimal matching algorithm with the following variables: Age, sex, stone diameter, stone number, bile duct diameter, American Society of Anesthesiologists Physical Status Classification System score and a history of cholecystectomy. EPBD, endoscopic papillary balloon dilation; EST, endoscopic sphincterotomy
Table 1.
Patient characteristics of the matched pairs with 10- and 8-mm EPBD for bile duct stone removal
Procedures of stone removal in the matched 10- and 8-mm EPBD groups
The outcomes of stone removal by EPBD are summarized in Table 2. The rate of complete stone removal did not differ significantly between the 10- and 8-mm EPBD groups (97% vs. 100%, P = 0.480). However, the rate of complete stone removal within a single session was significantly higher in the 10-mm EPBD group as compared with the 8-mm EPBD group (69% vs. 44%, P < 0.001), and the rate of requirement of lithotripsy of any type was significantly lower (23% vs. 56%, P < 0.001). As a result, a smaller number of ERCP sessions were required in the 10-mm EPBD group than in the 8-mm EPBD group [1 (IQR: 1–1.5) and 2 (IQR: 1–2), P < 0.001]. Complete stone removal failed in two patients in the 10-mm EPBD group; one underwent plastic biliary stent placement and the other underwent open choledochotomy at the patient's request after the first session of ERCP.
Table 2.
Outcomes of endoscopic removal of bile duct stones and short-term complications in the matched 10- and 8-mm EPBD groups
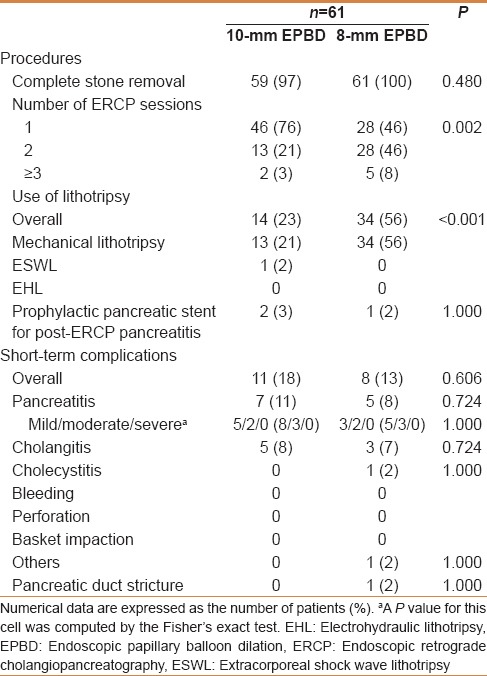
Short-term complications of the matched 10- and 8-mm EPBD groups
The short-term complications within 30 days of stone removal by EPBD are presented in Table 2. The rates of post-ERCP pancreatitis were similar in the 10- and 8-mm groups (11% vs. 8%, P = 0.724), and all patients with pancreatitis could be managed conservatively. Severe pancreatitis was not encountered in either group and the severity of pancreatitis did not depend on the treatment assignment.
No patients in both groups developed bleeding or perforation. Overall, the rates of short-term complications after EPBD were comparable (18% vs. 13% in the 10- and 8-mm EPBD groups, respectively; P = 0.606).
Long-term outcomes of the matched 10- and 8-mm EPBD groups
When evaluating long-term outcomes after EPBD, we excluded two pairs which included two patients with unsuccessful complete stone removal and, therefore, analyzed 59 pairs. Among 47 patients with gallbladder at the time of 10-mm EPBD, cholecystectomy was performed after EPBD in 17 patients (36%), gallbladder left in situ with stones in 24 (51%), and gallbladder left in situ without stones in 6 (13%). Among 49 patients with gallbladder at the time of 8-mm EPBD, cholecystectomy was performed after EPBD in 16 patients (33%), gallbladder left in situ with stones in 20 (41%), and gallbladder left in situ without stones in 13 (27%). Gallbladder left in situ with stones after EPBD was seen in 41% versus 34% patients in the 10- and 8-mm EPBD groups, respectively (P = 0.522). The median follow-up time was 2.0 (IQR: 0.7–3.1) and 2.8 (IQR: 1.3–5.3) years in the 10- and 8-mm EPBD groups, respectively (P < 0.001).
Table 3 presents the details of long-term biliary complications observed after EPBD. Overall, the rates of long-term biliary complications were not significantly different between the groups (24% vs. 20% for 10- and 8-mm EPBD, respectively; P = 0.823). Bile duct stone recurrence was observed in 12 (20%) and 10 (17%) patients in the 10- and 8-mm EPBD groups, respectively (P = 0.814). Ascending cholangitis without stone recurrence was not observed in both groups. No significant difference in biliary complication-free survival was found between the two groups (P = 0.239) [Figure 2]. The biliary complication-free rates were estimated to be 88% [95% confidence interval (CI): 79–97%] and 94% (95% CI: 88–100%) at 1 year and 69% (95% CI: 56–85%) and 80% (95% CI: 69–93%) at 2 years in the 10- and 8-mm EPBD groups, respectively. All patients with bile duct stone recurrence were successfully managed by repeated ERCP, except one patient in whom asymptomatic bile duct stones were left untreated.
Table 3.
Long-term outcomes of the patients with successful complete stone removal by 10- and 8-mm EPBD
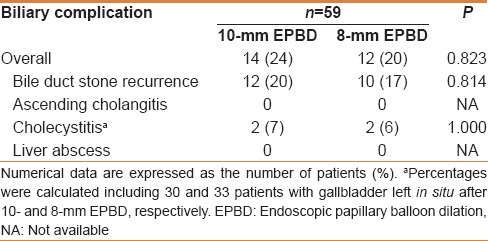
Figure 2.
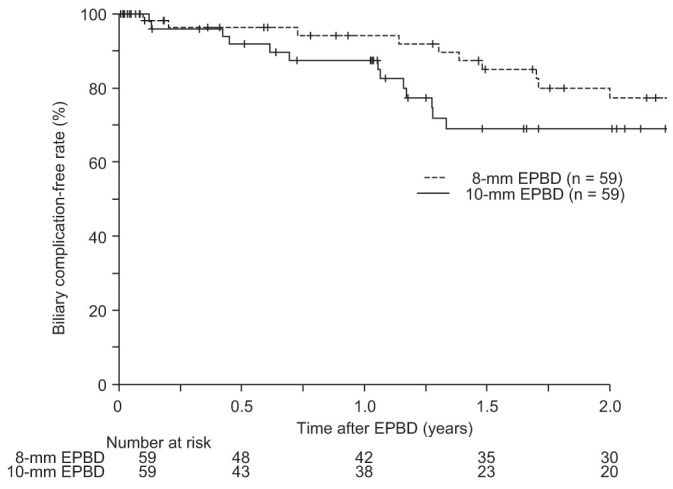
Kaplan-Meier curves showing biliary complication-free survival of the patients with successful stone removal in the matched 10- and 8-mm EPBD groups. Small vertical bars on each curve indicate censored cases. EPBD, endoscopic papillary balloon dilation
Pneumobilia was evaluated during the follow-up period. Any of the abdominal imaging studies was performed in 39 (66%) and 37 (63%) patients in the 10- and 8-mm EPBD groups, respectively. The rate of pneumobilia after 10-mm EPBD was not significantly higher than that after 8-mm EPBD (5% and 8%, P = 0.671).
DISCUSSION
In this matched cohort study based on data derived from two Japanese tertiary care centers, as compared with 8-mm EPBD, 10-mm EPBD was associated with a higher rate of complete stone removal within a single session and less frequent use of EML without increasing the risk of post-ERCP pancreatitis. Furthermore, our study demonstrated that the sphincter function could be preserved after 10-mm EPBD as after 8-mm EPBD, which ensures one of the major advantages of EPBD over EST.
EPBD is utilized as an alternative to EST for endoscopic stone extraction,[5,6,7,8,9] particularly in patients with coagulopathy. Although the efficacy of endoscopic papillary large balloon dilation (EPLBD) using a ≥12-mm balloon dilation catheter has been recently reported,[28,29,30,31] this procedure cannot be applied for small or normal bile duct and might cause a permanent loss of the sphincter function similar to EST, leading to an increased risk of stone recurrence. Taken together, EPBD can be a first-choice option for CBD stones in a subset of patients. To date, however, the outcomes of EPBD for CBD stones have not been fully investigated according to the size of a balloon dilation catheter. In a retrospective study of 208 patients, Li et al., evaluated the outcomes of EPBD with different-sized balloons (8–14 mm), which were matched for the size of the largest stone.[23] The investigators successfully removed bile duct stones in all cases regardless of the stone size, and found no significant association between the balloon size and post-ERCP pancreatitis. However, in addition to the fact that a limited EST was performed prior to EPBD, the adjustment for baseline characteristics between the groups with different-sized balloons was not done because it was not their study aim. Therefore, only limited data on comparison of 10- and 8-mm balloons in EPBD alone are currently available, considering the trade-off of technical success and complications.
The present study demonstrated the superiority of 10-mm EPBD over 8-mm EPBD as a means of sphincteroplasty to facilitate endoscopic stone extraction. Based on the promising results of several series about EPLBD without EST,[31,32,33] a highly enlarged orifice of the bile duct by a larger balloon can make subsequent procedures efficient, because it potentially eases device insertion and stone extraction. In our study, 10-mm EPBD was shown to increase the rate of complete stone removal within a single session and decrease the rate of requirement of lithotripsy. Given no increase in the short- and long-term complications in our 10-mm EPBD group as discussed below, 10-mm EPBD is considered as the more preferable sphincteroplasty than 8-mm EPBD in cases with bile duct greater than 10 mm.
Post-ERCP pancreatitis remains a serious issue associated with endoscopic extraction of bile duct stones.[34,35,36] The pathogenesis of pancreatitis after EPBD is not fully understood, but EPBD itself or subsequent stone extraction procedure might provoke papillary edema or spasm, leading to the outflow obstruction of pancreatic juice and eventually the development of pancreatitis. Although use of a larger balloon in EPBD might increase the injury to the ampulla, the rates of post-ERCP pancreatitis did not differ significantly between our 10- and 8-mm EPBD groups. We speculate that 10-mm EPBD might make stone extraction easier and could outweigh the increased damage to the ampulla.
The high rates of post-ERCP pancreatitis in our 10- and 8-mm EPBD groups needs to be discussed in context, regardless of the fact that no patients developed severe pancreatitis. EPBD is considered to be associated with a higher rate of post-ERCP pancreatitis, as compared with EST.[7,37] The relatively high rate of this complication in our study might be explained by more difficult cases referred to tertiary care centers and the involvement of trainee endoscopists. Presumably, pharmaceutical prevention[38,39] and pancreatic stent placement[40] should be administered more intensively than was done in our study, to minimize the risk of pancreatitis after EPBD. Other complications including bleeding and perforation which might be increased by the increase of balloon diameter were not observed in the 10-mm EPBD group. Taking the reported safety of EPLBD into account,[28,29,30,31,32,33] use of a larger balloon is considered acceptably safe, as far as the diameter of the balloon used does not exceed that of the lower bile duct.
The most notable advantage of EPBD is that this procedure potentially preserves the sphincter function, as opposed to EST.[15,16,17,18] Preservation of the sphincter function can prevent the duodenobiliary reflux and the recurrence of biliary stones due to bacterial colonization.[41] In terms of the preservation of the sphincter function, there is a concern about use of a larger balloon in EPBD, which might compromise the sphincter function more frequently. Li et al. found a significant correlation between increased balloon size and the rate of long-term post-ERCP pneumobilia.[23] Pneumobilia during the follow-up period was uncommon in our 10-mm EPBD group, and ascending cholangitis was not observed. There were no significant differences between the long-term biliary complications in our 10- and 8-mm EPBD groups, and a further prospective investigation is warranted about the threshold of balloon size to preserve the sphincter function after EPBD.
Several limitations should be acknowledged in the present study. The retrospective and, thus, non-randomized design was the major drawback of this study. Though patient matching was performed to control treatment selection bias, unmeasured confounding factors could not be adjusted. A relatively small number of patients and the shorter follow-up time in the 10-mm EPBD group should also be noted. Therefore, a randomized control trial with a large sample size is required to confirm the advantages of 10-mm EPBD over 8-mm EPBD. Various EPBD methods used in this study with regard to the duration of dilation and the types of balloon dilation catheters were the other limitations.
CONCLUSION
In conclusion, 10-mm EPBD is a safe procedure which allows more efficient endoscopic extraction of CBD stones, as compared with 8-mm EPBD. Furthermore, the sphincter function can be highly preserved after 10-mm EPBD, which ensures comparable long-term outcomes to 8-mm EPBD.
Footnotes
Source of Support: Nil
Conflict of Interest: The authors declare that they have no conflict of interest.
REFERENCES
- 1.Vaira D, D’Anna L, Ainley C, Dowsett J, Williams S, Baillie J, et al. Endoscopic sphincterotomy in 1000 consecutive patients. Lancet. 1989;2:431–4. doi: 10.1016/s0140-6736(89)90602-8. [DOI] [PubMed] [Google Scholar]
- 2.Cotton PB, Geenen JE, Sherman S, Cunningham JT, Howell DA, Carr-Locke DL, et al. Endoscopic sphincterotomy for stones by experts is safe, even in younger patients with normal ducts. Ann Surg. 1998;227:201–4. doi: 10.1097/00000658-199802000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson DB, Freeman ML. Major hemorrhage from endoscopic sphincterotomy: Risk factor analysis. J Clin Gastroenterol. 1994;19:283–7. doi: 10.1097/00004836-199412000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–18. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 5.Mathuna PM, White P, Clarke E, Merriman R, Lennon JR, Crowe J. Endoscopic balloon sphincteroplasty (papillary dilation) for bile duct stones: Efficacy, safety, and follow-up in 100 patients. Gastrointest Endosc. 1995;42:468–74. doi: 10.1016/s0016-5107(95)70052-8. [DOI] [PubMed] [Google Scholar]
- 6.Komatsu Y, Kawabe T, Toda N, Ohashi M, Isayama M, Tateishi K, et al. Endoscopic papillary balloon dilation for the management of common bile duct stones: Experience of 226 cases. Endoscopy. 1998;30:12–7. doi: 10.1055/s-2007-993721. [DOI] [PubMed] [Google Scholar]
- 7.Fujita N, Maguchi H, Komatsu Y, Yasuda I, Hasebe O, Igarashi Y, et al. JESED Study Group. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: A prospective randomized controlled multicenter trial. Gastrointest Endosc. 2003;57:151–5. doi: 10.1067/mge.2003.56. [DOI] [PubMed] [Google Scholar]
- 8.Tsujino T, Kawabe T, Komatsu Y, Yoshida H, Isayama H, Sasaki T, et al. Endoscopic papillary balloon dilation for bile duct stone: Immediate and long-term outcomes in 1000 patients. Clin Gastroenterol Hepatol. 2007;5:130–7. doi: 10.1016/j.cgh.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 9.Tsujino T, Yoshida H, Isayama H, Ito Y, Yashima Y, Yagioka H, et al. Endoscopic papillary balloon dilation for bile duct stone removal in patients 60 years old or younger. J Gastroenterol. 2010;45:1072–9. doi: 10.1007/s00535-010-0254-0. [DOI] [PubMed] [Google Scholar]
- 10.Ito Y, Tsujino T, Togawa O, Yamamoto N, Isayama H, Nakata R, et al. Endoscopic papillary balloon dilation for the management of bile duct stones in patients 85 years of age and older. Gastrointest Endosc. 2008;68:477–82. doi: 10.1016/j.gie.2007.10.066. [DOI] [PubMed] [Google Scholar]
- 11.Anderson MA, Ben-Menachem T, Gan SI, Appalaneni V, Banerjee S, Cash BD, et al. ASGE Standards of Practice Committee. Management of antithrombotic agents for endoscopic procedures. Gastrointest Endosc. 2009;70:1060–70. doi: 10.1016/j.gie.2009.09.040. [DOI] [PubMed] [Google Scholar]
- 12.Boustiere C, Veitch A, Vanbiervliet G, Bulois P, Deprez P, Laquiere A, et al. European Society of Gastrointestinal Endoscopy. Endoscopy and antiplatelet agents. European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2011;43:445–61. doi: 10.1055/s-0030-1256317. [DOI] [PubMed] [Google Scholar]
- 13.Park DH, Kim MH, Lee SK, Lee SS, Choi JS, Song MH, et al. Endoscopic sphincterotomy vs. endoscopic papillary balloon dilation for choledocholithiasis in patients with liver cirrhosis and coagulopathy. Gastrointest Endosc. 2004;60:180–5. doi: 10.1016/s0016-5107(04)01554-8. [DOI] [PubMed] [Google Scholar]
- 14.Takahara N, Isayama H, Sasaki T, Tsujino T, Toda N, Sasahira N, et al. Endoscopic papillary balloon dilation for bile duct stones in patients on hemodialysis. J Gastroenterol. 2012;47:918–23. doi: 10.1007/s00535-012-0551-x. [DOI] [PubMed] [Google Scholar]
- 15.Minami A, Nakatsu T, Uchida N, Hirabayashi S, Fukuma H, Morshed SA, et al. Papillary dilation vs sphincterotomy in endoscopic removal of bile duct stones. A randomized trial with manometric function. Dig Dis Sci. 1995;40:2550–4. doi: 10.1007/BF02220440. [DOI] [PubMed] [Google Scholar]
- 16.Sato H, Kodama T, Takaaki J, Tatsumi Y, Maeda T, Fujita S, et al. Endoscopic papillary balloon dilatation may preserve sphincter of Oddi function after common bile duct stone management: Evaluation from the viewpoint of endoscopic manometry. Gut. 1997;41:541–4. doi: 10.1136/gut.41.4.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yasuda I, Tomita E, Enya M, Kato T, Moriwaki H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut. 2001;49:686–91. doi: 10.1136/gut.49.5.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Isayama H, Komatsu Y, Inoue Y, Toda N, Shiratori Y, Tsujino T, et al. Preserved function of the Oddi sphincter after endoscopic papillary balloon dilation. Hepatogastroenterology. 2003;50:1787–91. [PubMed] [Google Scholar]
- 19.Yasuda I, Fujita N, Maguchi H, Hasebe O, Igarashi Y, Murakami A, et al. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010;72:1185–91. doi: 10.1016/j.gie.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 20.Doi S, Yasuda I, Mukai T, Iwashita T, Uemura S, Yamauchi T, et al. Comparison of long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation: A propensity score-based cohort analysis. J Gastroenterol. 2013;48:1090–6. doi: 10.1007/s00535-012-0707-8. [DOI] [PubMed] [Google Scholar]
- 21.Natsui M, Saito Y, Abe S, Iwanaga A, Ikarashi S, Nozawa Y, et al. Long-term outcomes of endoscopic papillary balloon dilation and endoscopic sphincterotomy for bile duct stones. Dig Endosc. 2013;25:313–21. doi: 10.1111/j.1443-1661.2012.01393.x. [DOI] [PubMed] [Google Scholar]
- 22.Lu Y, Wu JC, Liu L, Bie LK, Gong B. Short-term and long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Eur J Gastroenterol Hepatol. 2014;26:1367–73. doi: 10.1097/MEG.0000000000000218. [DOI] [PubMed] [Google Scholar]
- 23.Li NP, Liu JQ, Zhou ZQ, Ji TY, Cai XY, Zhu QY. Ampulla dilation with different sized balloons to remove common bile duct stones. World J Gastroenterol. 2013;19:903–8. doi: 10.3748/wjg.v19.i6.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dripps RD. New classification of physical status. Anesthesiology. 1963;24:111. [Google Scholar]
- 25.Tsujino T, Kawabe T, Isayama H, Sasaki T, Kogure H, Togawa O, et al. Efficacy and safety of low-pressured and short-time dilation in endoscopic papillary balloon dilation for bile duct stone removal. J Gastroenterol Hepatol. 2008;23:867–71. doi: 10.1111/j.1440-1746.2007.05267.x. [DOI] [PubMed] [Google Scholar]
- 26.Liao WC, Lee CT, Chang CY, Leung JW, Chen JH, Tsai MC, et al. Randomized trial of 1-minute versus 5-minute endoscopic balloon dilation for extraction of bile duct stones. Gastrointest Endosc. 2010;72:1154–62. doi: 10.1016/j.gie.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 27.Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, et al. Endoscopic sphincterotomy complications and their management: An attempt at consensus. Gastrointest Endosc. 1991;37:383–93. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 28.Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720–6. doi: 10.1016/j.gie.2007.02.033. quiz 768, 771. [DOI] [PubMed] [Google Scholar]
- 29.Misra SP, Dwivedi M. Large-diameter balloon dilation after endoscopic sphincterotomy for removal of difficult bile duct stones. Endoscopy. 2008;40:209–13. doi: 10.1055/s-2007-967040. [DOI] [PubMed] [Google Scholar]
- 30.Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, et al. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560–5. doi: 10.1038/ajg.2008.67. [DOI] [PubMed] [Google Scholar]
- 31.Kogure H, Tsujino T, Isayama H, Takahara N, Uchino R, Hamada T, et al. Short- and long-term outcomes of endoscopic papillary large balloon dilation with or without sphincterotomy for removal of large bile duct stones. Scand J Gastroenterol. 2014;49:121–8. doi: 10.3109/00365521.2013.848470. [DOI] [PubMed] [Google Scholar]
- 32.Jeong S, Ki SH, Lee DH, Lee JI, Lee JW, Kwon KS, et al. Endoscopic large-balloon sphincteroplasty without preceding sphincterotomy for the removal of large bile duct stones: A preliminary study. Gastrointest Endosc. 2009;70:915–22. doi: 10.1016/j.gie.2009.04.042. [DOI] [PubMed] [Google Scholar]
- 33.Chan HH, Lai KH, Lin CK, Tsai WL, Wang EM, Hsu PI, et al. Endoscopic papillary large balloon dilation alone without sphincterotomy for the treatment of large common bile duct stones. BMC Gastroenterol. 2011;11:69. doi: 10.1186/1471-230X-11-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsujino T, Isayama H, Komatsu Y, Ito Y, Tada M, Minagawa N, et al. Risk factors for pancreatitis in patients with common bile duct stones managed by endoscopic papillary balloon dilation. Am J Gastroenterol. 2005;100:38–42. doi: 10.1111/j.1572-0241.2005.40638.x. [DOI] [PubMed] [Google Scholar]
- 35.Cheng CL, Sherman S, Watkins JL, Barnett J, Freeman M, Geenen J, et al. Risk factors for post-ERCP pancreatitis: A prospective multicenter study. Am J Gastroenterol. 2006;101:139–47. doi: 10.1111/j.1572-0241.2006.00380.x. [DOI] [PubMed] [Google Scholar]
- 36.Nakai Y, Isayama H, Sasahira N, Kogure H, Sasaki T, Yamamoto N, et al. Risk factors for post-ERCP pancreatitis in wire-guided cannulation for therapeutic biliary ERCP. Gastrointest Endosc. 2015;81:119–26. doi: 10.1016/j.gie.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 37.Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: A metaanalysis of randomized, controlled trials. Am J Gastroenterol. 2004;99:1455–60. doi: 10.1111/j.1572-0241.2004.30151.x. [DOI] [PubMed] [Google Scholar]
- 38.Tsujino T, Komatsu Y, Isayama H, Hirano K, Sasahira N, Yamamoto N, et al. Ulinastatin for pancreatitis after endoscopic retrograde cholangiopancreatography: A randomized, controlled trial. Clin Gastroenterol Hepatol. 2005;3:376–83. doi: 10.1016/s1542-3565(04)00671-8. [DOI] [PubMed] [Google Scholar]
- 39.Elmunzer BJ, Scheiman JM, Lehman GA, Chak A, Mosler P, Higgins PD, et al. U.S. Cooperative for Outcomes Research in Endoscopy (USCORE). A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med. 2012;366:1414–22. doi: 10.1056/NEJMoa1111103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Choudhary A, Bechtold ML, Arif M, Szary NM, Puli SR, Othman MO, et al. Pancreatic stents for prophylaxis against post-ERCP pancreatitis: A meta-analysis and systematic review. Gastrointest Endosc. 2011;73:275–82. doi: 10.1016/j.gie.2010.10.039. [DOI] [PubMed] [Google Scholar]
- 41.Natsui M, Honma T, Genda T, Nakadaira H. Effects of endoscopic papillary balloon dilation and endoscopic sphincterotomy on bacterial contamination of the biliary tract. Eur J Gastroenterol Hepatol. 2011;23:818–24. doi: 10.1097/MEG.0b013e328348c0bf. [DOI] [PubMed] [Google Scholar]


