Abstract
Diffuse congenital hyperinsulinism in infancy (CHI-D) arises from mutations inactivating the KATP channel; however, the phenotype is difficult to explain from electrophysiology alone. Here we studied wider abnormalities in the β-cell and other pancreatic lineages. Islets were disorganized in CHI-D compared with controls. PAX4 and ARX expression was decreased. A tendency toward increased NKX2.2 expression was consistent with its detection in two-thirds of CHI-D δ-cell nuclei, similar to the fetal pancreas, and implied immature δ-cell function. CHI-D δ-cells also comprised 10% of cells displaying nucleomegaly. In CHI-D, increased proliferation was most elevated in duct (5- to 11-fold) and acinar (7- to 47-fold) lineages. Increased β-cell proliferation observed in some cases was offset by an increase in apoptosis; this is in keeping with no difference in INSULIN expression or surface area stained for insulin between CHI-D and control pancreas. However, nuclear localization of CDK6 and P27 was markedly enhanced in CHI-D β-cells compared with cytoplasmic localization in control cells. These combined data support normal β-cell mass in CHI-D, but with G1/S molecules positioned in favor of cell cycle progression. New molecular abnormalities in δ-cells and marked proliferative increases in other pancreatic lineages indicate CHI-D is not solely a β-cell disorder.
Introduction
Diffuse congenital hyperinsulinism in infancy (CHI-D) affects the entire pancreas and is characterized by persistent, inappropriate release of insulin in the presence of low blood glucose, commonly accompanied by macrosomia, indicating altered intrauterine development (1,2). Inactivating mutations in either the ABCC8 or KCNJ11 genes, which encode subunits of the KATP channel, account for approximately 90% of those cases (3,4) where hypoglycemia necessitates partial or near-total pancreatectomy (1,2). These mutations cause persistent β-cell depolarization, inappropriate calcium entry, and insulin secretion (5).
Two features of CHI-D imply more diverse pathophysiology. First, some reports have shown increased rates of β-cell proliferation by Ki67, which detects all stages of the cell-cycle except G0 (6–8). Understanding how CHI-D might promote human β-cell replication is desirable for therapeutic exploitation in diabetes. While the glucose-sensing/insulin secretion pathway can regulate β-cell proliferation (9) and an intricate array of cell cycle proteins is in place (10), normal human β-cells are recalcitrant in proliferation assays compared with their rodent counterparts (11). Second, alterations outside the β-cell lineage imply consequences from abnormal β-cells or that CHI-D directly affects other pancreatic lineages. For instance, pancreatic polypeptide (PP) cells and somatostatin-stained δ-cells have been reported as altered in CHI-D (12). Certainly, KATP channels are expressed in other islet cell types, and normal β-cell function relies on multiple intraislet interactions (5).
In this study we explored potential defects in differentiation, maturity, and proliferation of β-cells and other pancreatic lineages in CHI-D caused by mutant KATP channels.
Research Design and Methods
Human Tissue
Following ethical approval, national codes of practice, and informed consent, pancreatic tissue was received from 10 cases of CHI-D (Supplementary Table 1) or normal control samples as previously described (13). CHI-D was diagnosed from established clinical and histopathological criteria (1,2) and the identification of ABCC8 or KCNJ11 mutations (Supplementary Table 1). Postnatal control cases (2 days to 36 months [n = 16] or ≥12 years old [n = 4]) died of nonpancreatic diagnoses and showed unremarkable pancreatic histology. Fetal control material (n = 4) was obtained and processed 10 to 35 weeks post-conception (wpc) as described previously (14,15).
Immunohistochemistry, Immunofluorescence, and Cell Counting
Immunohistochemistry and immunofluorescence were performed as described previously (14,15) (Supplementary Table 2). High-content assessment of Ki67+ cells and insulin+ surface area followed digitization of slides (3D Histech Pannoramic 250 Flash II) using Pannoramic Viewer and HistoQuant software. At least 20 regions of interest were selected (free from connective tissue), and Ki67+ cells were calculated as a fraction of the total cell count. No regional differences were measured. Dual staining of Ki67 and pancreatic lineage markers was assessed from 10 randomly selected fields of view at ×200 magnification in at least two positions within each CHI-D or control pancreas or in the entire section (fetal samples; those of smaller size). Apoptosis combined immunofluorescence for insulin using a conjugated Alexa-Fluor dye (Life Technologies, Paisley, U.K.) with fluorescein isothiocyanate–labeled terminal deoxynucleotidyl TUNEL according to the manufacturer’s instructions (Trevigen, Gaithersburg, MD). DNase I treatment and omission of the terminal transferase enzyme served as positive and negative controls, respectively.
Isolation of RNA, RT-PCR, and Quantitative PCR
Total RNA was isolated from whole tissue sections using the Qiagen RNeasy FFPE kit protocol according to the manufacturer’s instructions. Quantitative RT-PCR was performed as described previously, using the ΔΔCT method standardized to HPRT and β-ACTIN and compared with age-matched controls (16,17) (primers in Supplementary Table 3).
Statistical Analysis
Cell counting data are presented as mean ± standard error. Patient and control samples were compared using the Mann-Whitney U test and correlation was assessed using the Spearman rank correlation test.
Results
Islet Structure and Hormone Colocalization in CHI-D
CHI-D α-cells and δ-cells were more diffusely scattered throughout the islet compared with a peripheral mantle location in early postnatal control tissue (Supplementary Figs. 1A–D and 2A–D). This tended to resolve to matched control tissue by the end of the first year; however, the overall islet structure remained less organized and compact in CHI-D (Supplementary Figs. 1E–F and 2E–F). In two of the CHI-D samples from early infancy 2–5% of glucagon-positive and insulin-positive cells contained both hormones, similar to fetal pancreas but not observed in any of the postnatal control samples (Supplementary Fig. 3 and Supplementary Video). Colocalization was not observed for insulin with somatostatin, ghrelin, or PP.
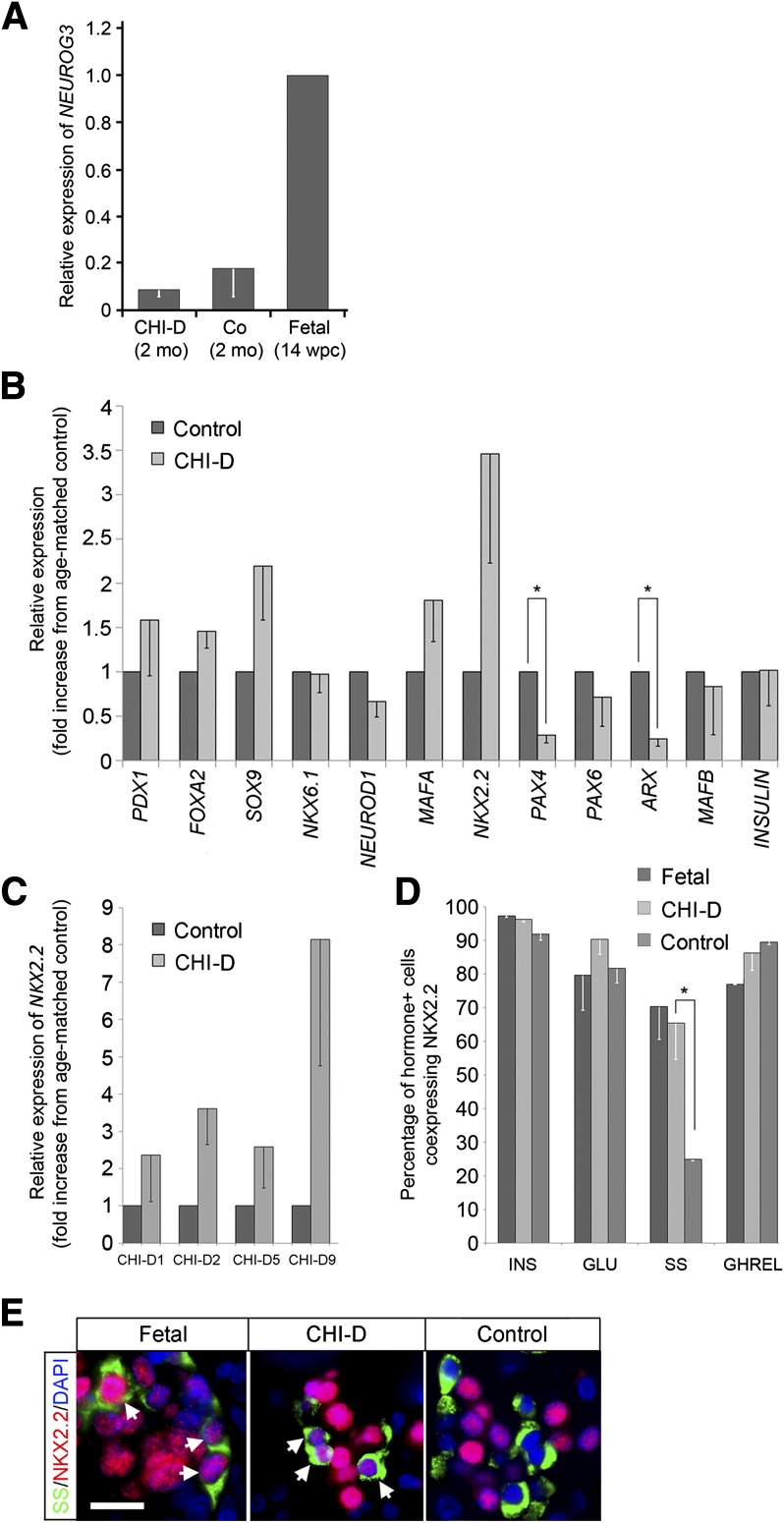
“Fetal-Like” NKX2.2 in Early Postnatal CHI-D δ-Cells
Given this potential immaturity, we looked for signs of endocrine differentiation in CHI-D. NEUROG3 detection from whole tissue sections was no higher in CHI-D than age-matched controls and much lower than when fetal NEUROG3-positive cells are most abundant (13) (Fig. 1A). We did not detect convincing NEUROG3 immunoreactivity in CHI-D or age-matched controls spanning the first year after birth (data not shown). FOXA2 (in β-cells and duct cells), NKX6.1 (β-cells), SOX9 (duct cells), and GATA4 (acinar cells) were all appropriately detected as nuclear proteins in their respective cell types in CHI-D and age-matched controls (Supplementary Fig. 4; data not shown). Mean expression of INSULIN, PDX1, FOXA2, SOX9, NKX6.1, MAFA, and MAFB from whole tissue sections was not altered in CHI-D samples (Fig. 1B). While NKX2.2 was increased before Hochberg correction, PAX4 and ARX were consistently decreased statistically (control levels of NKX2.2 were constant during the first year; Fig. 1B). This trend toward increased NKX2.2 in CHI-D reflected cases up to 6 months of age (Fig. 1C). Nuclear NKX2.2 protein was detected by immunofluorescence in virtually all β-cells, 80–90% of α-cells, and 75–90% of ghrelin-positive cells in CHI-D, fetal, and postnatal control samples. By contrast, NKX2.2 was detected in two-thirds of CHI-D and fetal δ-cells but only in 25% of age-matched control cells (Fig. 1D and E). Given this alteration, we examined nucleomegaly, another feature of CHI-D (8,16). CHI-D islet cells tended to have a slightly larger nucleus than age-matched controls, with a clear subset outside a normal distribution showing a >50% increase in nuclear diameter (Supplementary Fig. 5A). Most of the cells with these enlarged nuclei stained for insulin and β-cell transcription factors including NKX6.1 and ISL1 (PDX1 was missing occasionally; Supplementary Fig. 5B). Nucleomegaly was not observed in CHI-D cells positive for glucagon, PP, or ghrelin or in duct or acinar cells (data not shown; Supplementary Fig. 4A and G). However, 10% of nucleomegalic cells contained somatostatin, implying a δ-cell identity (Supplementary Fig. 5C).
Figure 1.
Expression of key transcription factors in CHI-D pancreas. A: Quantitative RT-PCR analysis of NEUROG3 in triplicate in CHI-D1 and CHI-D2 and age-matched controls (mean ± SEM) standardized against levels of detection in the human fetal pancreas at 14 wpc. Co, control; mo, months. B: Quantitative RT-PCR analysis of 11 transcription factors and insulin. Data from each CHI-D sample were analyzed in triplicate and standardized against their own age-matched control before displaying data as means ± SEM for all CHI-D samples. *P < 0.01 following Hochberg correction. C: Quantitative RT-PCR expression of NKX2.2 in CHI-D samples (performed in triplicate; mean ± SEM) during the first 6 months compared with their age-matched controls. D: Cell counting of dual immunofluorescence for NKX2.2 with islet hormones, insulin (INS), glucagon (GLU), somatostatin (SS), and ghrelin (GHREL) for the four CHI-D samples in C, their age-matched controls, and human fetal pancreas (two specimens at 11 and 15 wpc). Data are expressed as the mean percentage ± SEM for each hormone lineage. NKX2.2 is retained in somatostatin-positive CHI-D cells compared with age-matched controls (*P < 0.01). E: Examples (as counted in C) of dual immunofluorescence for SS and NKX2.2 counterstained with DAPI. Arrows show colocalization in fetal and CHI-D samples. Scale bar = 10 µm.
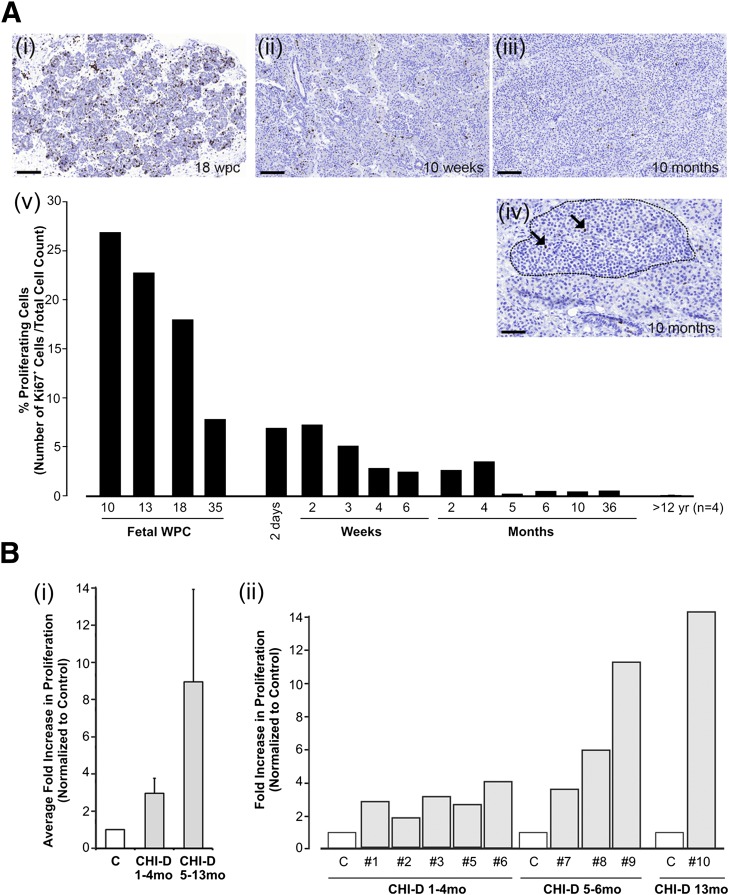
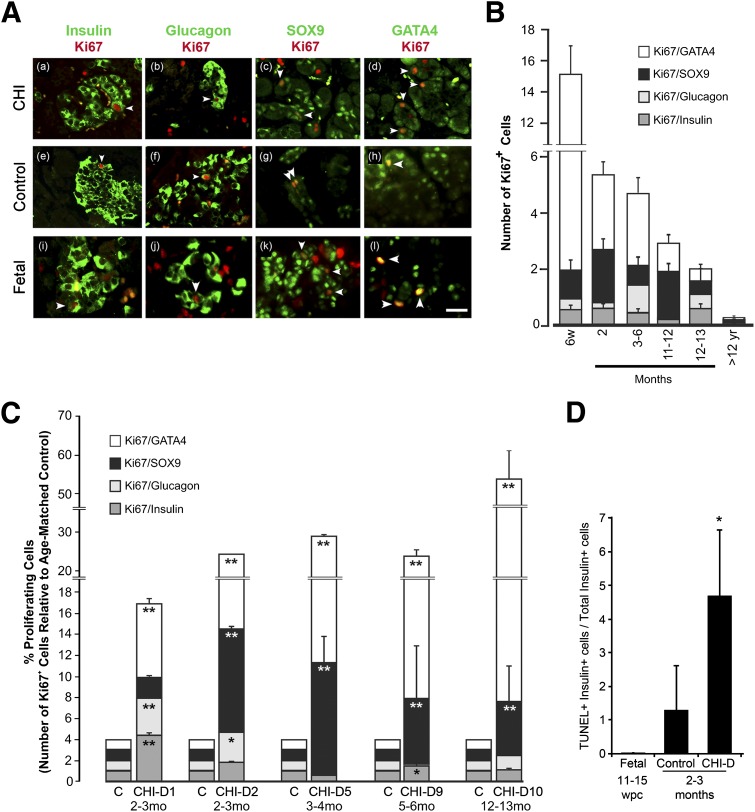
Increased Cell Proliferation in CHI-D Occurs Mostly in Exocrine Cells
Recognizing that CHI-D extended beyond β-cells, we studied proliferation in different pancreatic lineages. Total proliferation in control pancreas declined between 10 wpc and 36 months of age (Fig. 2A), with a very low rate from 12 years onward. During months 1–13, Ki67 count was increased in every CHI-D case compared with age-matched controls (Fig. 2B). This increased Ki67 count was particularly noticeable after the first 4 months, consistent with maintained proliferation in CHI-D, when replication in normal pancreas was declining. The declining proliferation in normal pancreas during the first year was largely in acinar cells (Fig. 3A and B). Very little proliferation in α-cells and β-cells was detected beyond 1 year of age. Only two of five cases studied (CHI-D 1 and CHI-D 9) showed elevated β-cell proliferation compared with their controls, the same proportion of specimens with increased α-cell proliferation (CHI-D 1 and CHI-D 2) (Fig. 3C). By contrast, four of the five cases showed increased duct cell proliferation (5- to 11-fold), whereas all five cases demonstrated increased acinar cell proliferation, which was progressively more noticeable with age. Apoptosis by TUNEL seemed negligible in exocrine tissue and α-cells. As found by Kassem et al. (6), apoptosis in β-cells was increased (Fig. 3D), raising the question of whether Ki67 truly reflected cell proliferation or, potentially, DNA damage with attempted repair. As an additional marker of proliferation analyzed in >100,000 cells, we found phosphohistone H3–positive cells were, on average, fivefold more prevalent in CHI-D (n = 2 cases) than in age-matched controls (n = 2 cases) and were most prevalent in acinar cells (Supplementary Fig. 6), similar to the data on Ki67 (Fig. 2B[i]). Also, we found no evidence of colocalization of phospho-γ-H2AX (a marker of DNA damage) with Ki67-positive cells. Furthermore, INSULIN expression was equivalent between CHI-D and controls (Fig. 1B), and the surface area of insulin staining was statistically unchanged between CHI-D (4.9 ± 0.37% [mean ± SEM] of sections; 2–13 months; n = 5) and age-matched controls (5.8 ± 0.38%; 1–10 months; n = 4). These multiple strands of evidence imply no increase of β-cell mass in CHI-D but predominant proliferation in exocrine cells.
Figure 2.
Cell proliferation is increased in CHI-D tissue. A: Proliferation in human control pancreas from 10 wpc, during the first year after birth (weeks, months), and ≥12 years (yr). All data points were gathered from individual cases, except for the data associated with ≥12 years, which are averaged from four cases. Proliferation was assessed by high-density counting from a minimum of 20,000 cells, with Ki67+ cells expressed as a percentage of the total cell count. Ai–iv: Representative images from fetal tissue at 18 wpc and postnatal pancreas at 10 weeks and 10 months. Ki67+ cells are stained brown and are clearly seen in islets (arrows in panel Aiv). Scale bars represent 100 μm in Ai–iii and 50 μm in Aiv. B: Proliferation in CHI-D tissue. Bi: Average fold increase in Ki67 count expressed relative to age-matched controls from cases up to 4 months and the older ones. Bii: Individual data from the nine cases compared with age-matched controls demonstrate particularly higher proliferation rates at older ages. C, age-matched control; mo, months; #, patient identifier.
Figure 3.
Increased proliferation in all pancreatic cell lineages in CHI-D tissue. A: Dual immunofluorescence of markers for endocrine cells (β-cells, insulin; α-cells, glucagon) and nonendocrine cells (duct cells, SOX9; acinar cells, GATA4) (green) in the pancreas with Ki67 (red) for CHI-D pancreas, postnatal control tissue, and an example of fetal tissue at 14 wpc. Arrows show examples of costained cells. Scale bar = 20 μm in all panels. B: Total counts (±SEM) for Ki67+ cells dual-stained for the markers of different pancreatic lineages in human control pancreas. Total Ki67 count was correlated inversely with age (r2 = −0.929; P < 0.01). w, weeks; yr, years. C: Fold increase (±SEM) in proliferation for each cell lineage (as defined by the markers in A) for each CHI-D sample compared with its age-matched control (C). Each bar stacks the fold increments for each cell lineage. mo, months. D: Relative counts (±SEM) for TUNEL-positive/insulin-positive cells expressed as a percentage of the total insulin-positive cells for fetal and CHI-D samples and their age-matched postnatal controls. Statistical analysis performed using Mann-Whitney U test. *P < 0.05, **P < 0.01.
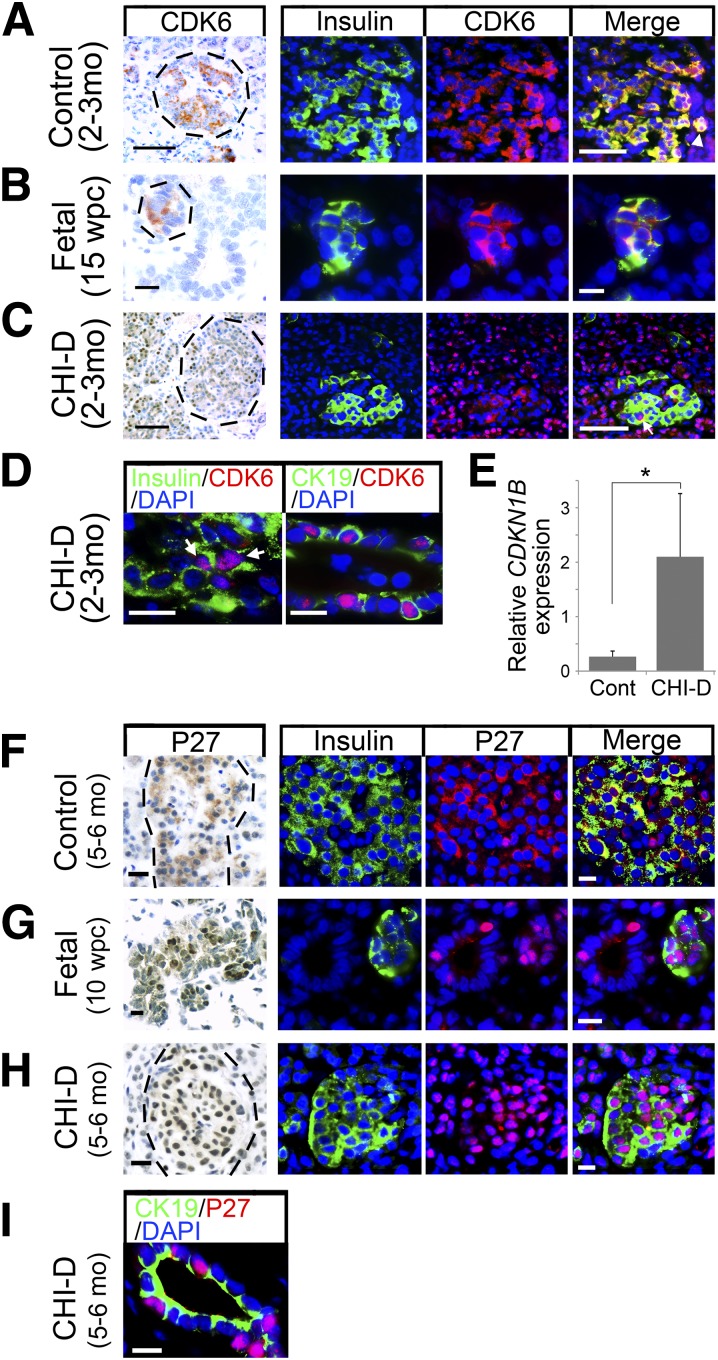
Nuclear CDK6 and P27 in CHI-D
G1/S cell cycle molecules (e.g., CDK6) tend to be cytoplasmic in adult human β-cells (17–19), but upon forced nuclear translocation, they can drive proliferation (17,18). CDK6 staining was predominantly cytoplasmic in control β-cells at 2–3 months, with occasional cells including nuclear localization (Fig. 4A, arrowhead). Staining in fetal β-cells was similarly cytoplasmic at 15 wpc (Fig. 4B). By contrast, cytoplasmic CDK6 was less noticeable in CHI-D β-cells but clearly nuclear in a proportion (Fig. 4C and D). CDK6 was also nuclear in many CHI-D CK19-positive duct cells (Fig. 4D) and acinar cells (Fig. 4C).
Figure 4.
Increased nuclear localization of CDK6 and P27 in CHI-D. Bright-field immunohistochemistry counterstained with toluidine blue and dual immunofluorescence counterstained with DAPI for CDK6 (A–D) or P27 (F–I) in postnatal control pancreas, samples of fetal pancreas, and CHI-D. Costaining is with insulin except for samples with CK19 in D and I. Hatched lines in the bright-field images encircle islets. A–D: Arrowhead in the merged panel of A points to insulin-positive cells, in which CDK6 localizes to both cytoplasm and nucleus. In C, the cytoplasmic CDK6 is very much reduced in CHI-D compared with control (Cont) or fetal β-cells, whereas the arrow in the merged panel (and arrows in D) points to clear nuclear CDK6 in insulin-positive cells. E: Quantitative RT-PCR showing increased CDKN1B expression in CHI-D (mean ± SE from five cases across the first 13 months of age) compared with age-matched controls (n = 3). *P < 0.05, Mann-Whitney U test. F–I: P27 is almost exclusively cytoplasmic in postnatal control β-cells, whereas it is almost exclusively nuclear in fetal and CHI-D β-cells and in CK-19-positive duct cells. Scale bars = 50 µm (A and C), 20 µm (B), and 10 µm (D and F–I). mo, months.
Based on these findings, we generated an interactome model of network clusters derived from a CHI microarray data set (20) (Supplementary Fig. 7A). A total of 1,288 genes were significantly altered (P < 0.05, ANOVA), which yielded 140 functional modules. When the gene most centrally associated with each module (Supplementary Fig. 7B) was ranked by its priority score as an index of centrality, the module containing CDKN1B came third (Supplementary Table 4). CDKN1B encodes P27, which can potentially inhibit proliferation or act as a chaperone for entry of the CDK6–cyclin complex into the nucleus (17–19). CDKN1B expression was increased almost eightfold in CHI-D pancreas relative to that of the age-matched control (Fig. 4E). P27 was almost entirely cytoplasmic in postnatal control β-cells but extensively nuclear in CHI-D and fetal β-cells (Fig. 4F–H). P27 also was nuclear in CHI-D duct and acinar cells (Fig. 4I; data not shown). Not all cells with these altered cell cycle proteins were nucleomegalic (Supplementary Fig. 8).
Discussion
Studying the histopathology of CHI-D cases is useful because modeling in mice with mutant Abcc8 and Kcnj11 has failed to phenocopy all aspects of the disorder. Here, islet disorganization in CHI-D was consistent with findings in Abcc8 and Kcnj11 mutant mice (21,22). While we did not observe increased PP cells (12), developmental transcription factors were altered. NKX2.2 helps maintain β-cell identity (23), and mutations cause neonatal diabetes (24). The tendency toward increased NKX2.2 in CHI-D pancreas concurs with low ARX expression, which it represses (23), and is consistent with an unexpanded PP cell population. Although CHI-D δ-cells were sparse (12), they more frequently contained NKX2.2, like fetal δ-cells, and made up 10% of endocrine cells with nucleomegaly. It is difficult to conceive that these two δ-cell alterations are secondary to inappropriate insulin from β-cells, arguing that CHI-D directly affects multiple endocrine lineages in keeping with expression of the KATP channel subunits in multiple islet cell types in mice (22). Atypical nuclei in β-cells and δ-cells might raise concern over future tumor risk; however, CHI-D is not known to predispose to islet cell tumors. Nevertheless, potential δ-cell immaturity tallies with clinical use of somatostatin analogs to inhibit insulin release in CHI-D (1), reviving the notion that the disorder could be in part a defect of δ-cells (12). By contrast, acinar and duct cells are not known to contain the KATP channel. Their augmented proliferation might therefore reflect inappropriate local insulin concentrations.
Understanding how human β-cells might be provoked into proliferation is a major therapeutic target in diabetes. CHI-D provides a distinctive opportunity to characterize β-cell proliferation in native human tissue. Our data on CDK6 intracellular localization add new weight to the model that its nuclear exclusion is a major checkpoint for human β-cell replication (10) and support P27 as its potential nuclear chaperone rather than a cell cycle inhibitor (18).
In summary, we report altered pancreatic transcription factors and cell cycle proteins in CHI-D. How these features relate to the loss of functional KATP channels, hypoglycemia, and inappropriate insulin release would now be interesting to investigate and could assist in the longer-term care of patients with CHI-D.
Supplementary Material
Article Information
Acknowledgments. Special thanks go to Roger Meadows for help with the microscopy and image analysis. The authors are grateful to the research nurses and clinical colleagues at Central Manchester University Hospitals NHS Trust and the Manchester Biomedical Research Centre.
Funding. This work was supported by the Wellcome Trust (WT088566MA and WT097820MF to N.A.H.), the Medical Research Council (R.J.S., PhD student, and R.E.J., clinical fellow), and the National Institute for Health Research (M.J.D., I.B., and K.E.C.).
Duality of Interest. No conflicts of interest relevant to this article were reported.
Author Contributions. R.J.S. and B.H. researched data and wrote the manuscript. R.E.J., A.A.B., A.S., Z.M., S.A.S., R.D.K., S.E.C., M.N., K.E.C., and K.P.H. researched data and reviewed and edited the manuscript. R.D.K., P.P.V.J., and I.B. oversaw tissue collection. M.J.D. and N.A.H. oversaw tissue collection, interpreted data, and wrote the manuscript. N.A.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Material online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db14-1202/-/DC1.
References
- 1.Glaser B. Lessons in human biology from a monogenic pancreatic β cell disease. J Clin Invest 2011;121:3821–3825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dunne MJ, Cosgrove KE, Shepherd RM, Aynsley-Green A, Lindley KJ. Hyperinsulinism in infancy: from basic science to clinical disease. Physiol Rev 2004;84:239–275 [DOI] [PubMed] [Google Scholar]
- 3.Kapoor RR, Flanagan SE, Arya VB, Shield JP, Ellard S, Hussain K. Clinical and molecular characterisation of 300 patients with congenital hyperinsulinism. Eur J Endocrinol 2013;168:557–564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Snider KE, Becker S, Boyajian L, et al. Genotype and phenotype correlations in 417 children with congenital hyperinsulinism. J Clin Endocrinol Metab 2013;98:E355–E363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashcroft FM, Rorsman P. K(ATP) channels and islet hormone secretion: new insights and controversies. Nat Rev Endocrinol 2013;9:660–669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kassem SA, Ariel I, Thornton PS, Scheimberg I, Glaser B. Beta-cell proliferation and apoptosis in the developing normal human pancreas and in hyperinsulinism of infancy. Diabetes 2000;49:1325–1333 [DOI] [PubMed] [Google Scholar]
- 7.Sempoux C, Guiot Y, Dubois D, et al. Pancreatic B-cell proliferation in persistent hyperinsulinemic hypoglycemia of infancy: an immunohistochemical study of 18 cases. Mod Pathol 1998;11:444–449 [PubMed] [Google Scholar]
- 8.Lovisolo SM, Mendonça BB, Pinto EM, Manna TD, Saldiva PH, Zerbini MC. Congenital hyperinsulinism in Brazilian neonates: a study of histology, KATP channel genes, and proliferation of β cells. Pediatr Dev Pathol 2010;13:375–384 [DOI] [PubMed] [Google Scholar]
- 9.Dadon D, Tornovsky-Babaey S, Furth-Lavi J, et al. Glucose metabolism: key endogenous regulator of β-cell replication and survival. Diabetes Obes Metab 2012;14(Suppl. 3):101–108 [DOI] [PubMed] [Google Scholar]
- 10.Fiaschi-Taesch NM, Kleinberger JW, Salim FG, et al. Human pancreatic β-cell G1/S molecule cell cycle atlas. Diabetes 2013;62:2450–2459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stewart AF. Betatrophin versus bitter-trophin and the elephant in the room: time for a new normal in β-cell regeneration research. Diabetes 2014;63:1198–1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rahier J, Fält K, Müntefering H, Becker K, Gepts W, Falkmer S. The basic structural lesion of persistent neonatal hypoglycaemia with hyperinsulinism: deficiency of pancreatic D cells or hyperactivity of B cells? Diabetologia 1984;26:282–289 [DOI] [PubMed] [Google Scholar]
- 13.Salisbury RJ, Blaylock J, Berry AA, et al. The window period of NEUROGENIN3 during human gestation. Islets 2014;6:e954436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jennings RE, Berry AA, Kirkwood-Wilson R, et al. Development of the human pancreas from foregut to endocrine commitment. Diabetes 2013;62:3514–3522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Piper K, Brickwood S, Turnpenny LW, et al. Beta cell differentiation during early human pancreas development. J Endocrinol 2004;181:11–23 [DOI] [PubMed] [Google Scholar]
- 16.Suchi M, Thornton PS, Adzick NS, et al. Congenital hyperinsulinism: intraoperative biopsy interpretation can direct the extent of pancreatectomy. Am J Surg Pathol 2004;28:1326–1335 [DOI] [PubMed] [Google Scholar]
- 17.Fiaschi-Taesch NM, Salim F, Kleinberger J, et al. . Induction of human beta-cell proliferation and engraftment using a single G1/S regulatory molecule, cdk6. Diabetes 2010;59:1926–1936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fiaschi-Taesch NM, Kleinberger JW, Salim FG, et al. Cytoplasmic-nuclear trafficking of G1/S cell cycle molecules and adult human β-cell replication: a revised model of human β-cell G1/S control. Diabetes 2013;62:2460–2470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kulkarni RN, Mizrachi EB, Ocana AG, Stewart AF. Human β-cell proliferation and intracellular signaling: driving in the dark without a road map. Diabetes 2012;61:2205–2213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Michelsen NV, Brusgaard K, Tan Q, Thomassen M, Hussein K, Christesen HT. Investigation of archived formalin-fixed paraffin-embedded pancreatic tissue with whole-genome gene expression microarray. ISRN Pathol 2011;2011:275102 [Google Scholar]
- 21.Seghers V, Nakazaki M, DeMayo F, Aguilar-Bryan L, Bryan J. Sur1 knockout mice. A model for K(ATP) channel-independent regulation of insulin secretion. J Biol Chem 2000;275:9270–9277 [DOI] [PubMed] [Google Scholar]
- 22.Seino S, Iwanaga T, Nagashima K, Miki T. Diverse roles of K(ATP) channels learned from Kir6.2 genetically engineered mice. Diabetes 2000;49:311–318 [DOI] [PubMed] [Google Scholar]
- 23.Papizan JB, Singer RA, Tschen SI, et al. Nkx2.2 repressor complex regulates islet β-cell specification and prevents β-to-α-cell reprogramming. Genes Dev 2011;25:2291–2305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Flanagan SE, De Franco E, Lango Allen H, et al. Analysis of transcription factors key for mouse pancreatic development establishes NKX2-2 and MNX1 mutations as causes of neonatal diabetes in man. Cell Metab 2014;19:146–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.