Abstract
Inversion of the uterus is a rare clinical problem. It is encountered as an obstetric emergency and is a diagnostic challenge in gynaecology. Non-puerperal inversion usually results from a tumour implanted on fundus of the uterus. Treatment depends on the associated pathology and the stage of the inversion. A rare case of non-puerperal uterine inversion caused by a large fundal submucous fibroid in a 58-year-old woman resulting in lower abdominal pain and vaginal bleeding was reported. After removal of fibroid, reduction of the inversion was successful and then abdominal hysterectomy was performed.
Background
The case is important because it is easy to miss the inversion of uterus in patient with fundal fibroid, if it is not suspected clinically.
The management of uterine inversion should be early and appropriate to reduce complications.
Case presentation
A 58-year-old woman was admitted to hospital complaining of pain in her lower abdomen and per vaginal bleeding with something coming out of the vagina since 2–3 months. The patient was menopausal with previous three living issues. Operative history was insignificant. General examination was unremarkable except for the presence of anaemia. On per abdominal examination, she had tenderness in the lower abdomen. On per vaginal examination, a large and firm mass was palpated in the vagina which bled on being touched. The cervix could neither be seen nor palpated. As patient was fatty bimanual examination was not informative. Clinical diagnosis of large cervical fibroid or cervical malignancy was made.
Investigations
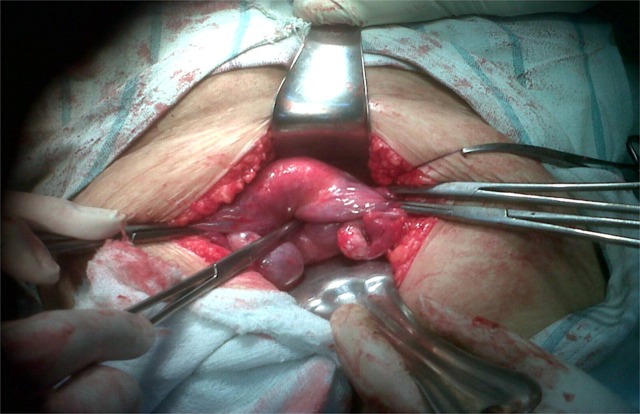
Sonography did not reveal smooth regular uterine fundal contour. Cervix was noted higher up in position. Fundus of uterus was found lying within the vagina. A 26 × 24 mm size mixed echogenic lesion was noted at fundus showing peripheral vascularity (suggestive of fibroid). There was evidence of a ‘U’-shaped depression or dimplimg at superior aspect of uterus with separation of uterine walls and cervix. On Doppler study, the vascular pedicle was noted going along the fundus within the cavity. Diagnosis of inversion of uterus with fundal fibroid was made based on sonographical features (figure 1).
Figure 1.
Showing ‘U’-shaped notch or dimpling on superior aspect of uterus with cervix noted higher in position and inverted fundus along with the fibroid noted within vagina.
Differential diagnosis
Cervical fibroid
Cervical malignancy
Cervical polyp
Treatment
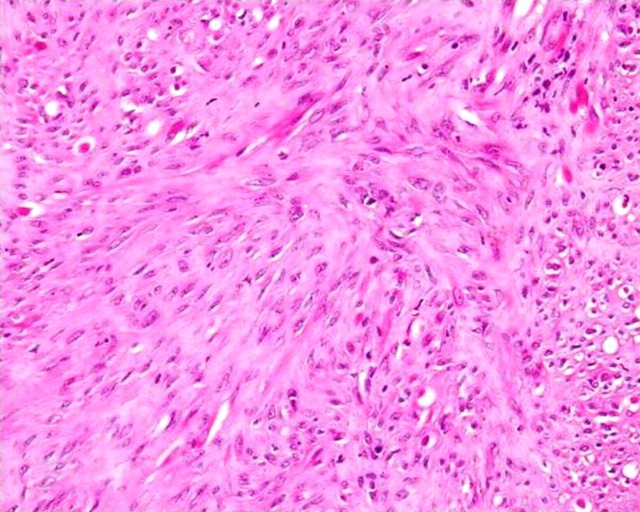
The patient was operated. Diagnosis of inversion was confirmed during operation. The fibroid was found submucous in location at fundus of uterus which was then removed vaginally and then abdominal hysterectomy was performed (figure 2).
Figure 2.
Intraoperative image confirming the diagnosis of inversion of uterus with dimple at fundus of uterus suggested by tip of forcep.
Outcome and follow-up
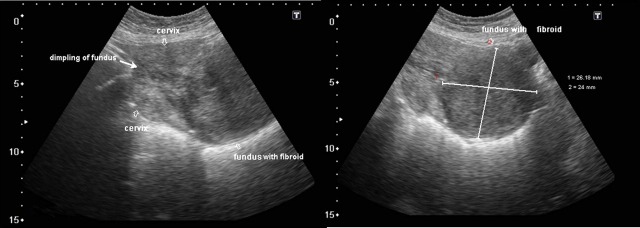
Specimen was sent for histopathological examination which showed features suggestive of fibroid (figure 3).
Figure 3.
Histopathological image showing features of fibroid-smooth muscle cells without mitoses.
Discussion
Inversion of the uterus is an unusual entity and may be classified as puerperal (obstetric) and non-puerperal (gynaecological) inversion.1
Classification according to severity:
Incomplete inversion—the uterine fundus that has inverted and lies within endometrial cavity without extending beyond external os.
Complete inversion—inverted fundus that extends beyond external os.2
Prolapsed inversion—inverted uterine fundus extends beyond vaginal introitus.3
Total inversion—inversion of uterus and vagina.2
Aetiology
Non-puerperal uterine inversion is very rare.4 5 It occurs chiefly when the uterus acts to expel a submucous leiomyoma or endometrial carcinoma or sarcoma or endometrial polyp.6 Possible explanations could be a thin uterine wall, rapid growth of the tumour, tumour size, fundal location of the tumour, tumour attachment to the uterine wall with a thin pedicle, dilatation of the cervix by distension of the uterine cavity.7
Diagnosis
Diagnosis is usually based on clinical signs and symptoms. The prominent symptoms are vaginal discharge, irregular uterine bleeding and pelvic discomfort. Bimanual palpation may reveal the absence of uterine body from its normal position. The recto-abdominal method is often most suitable, as the vagina is occupied by inverted uterus. The edge of the inversion cup can be recognised by abdominal examination especially under anaesthesia and it also helps in reduction of inversion.8
Ultrasonographical features include hyperechoic mass in the vagina with a central hypoechoic H-shaped cavity in the transverse image, while in the longitudinal image, a U-shaped depressed longitudinal groove from the uterine fundus to the centre of the inversion part is diagnostic of uterine inversion.9 10
MRI findings: on T2-weighted MRI scans, one can identify a U-shaped uterine cavity and inverted uterine fundus on a sagittal image and a ‘bulls-eye’ configuration on an axial image as indicative signs of uterine inversion are much more conspicuous.3
Treatment
In the case of non-puerperal inversion, abdominal or vaginal hysterectomy with bilateral salpingo-oophorectomy is the surgery of choice. When a uterine malignancy is associated with uterine inversion, abdominal hysterectomy with appropriate staging biopsy is usually indicated.
Learning points.
In the case of non-puerperal inversion, one should try to find out associated pathology that has led to inversion.
Even though inversion of uterus is not suspected clinically, one should consider it as a diagnosis if ultrasound shows features of inversion.
The inversion of uterus is to be diagnosed early otherwise any delay in treatment results in acute blood loss and increased risk of infection and subsequent morbidity.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Cunningham FG, MacDonald PC, Gant NF, et al. Williams Obstetrics. 20th ed Stamford, CN: Appleton & Lange, 1997:767–9. ISBN: 0-8385-9638-X. [Google Scholar]
- 2.Salomon CG, Patel SK. Computed tomography of chronic nonpuerperal uterine inversion. J Comput Assist Tomogr 1990;14:1024–6. PMID: 2229552. [DOI] [PubMed] [Google Scholar]
- 3.Lewin JS, Bryan PJ. MR imaging of uterine inversion. J Comput Assist Tomogr 1989;13:357–9. PMID: 2647797. [DOI] [PubMed] [Google Scholar]
- 4.Gomez-Lobo V, Burch W, Khanna PC. Non-puerperal uterine inversion associated with an immature teratoma of the uterus in an adolescent. Obstet Gynecol 2007;110:491–3. [DOI] [PubMed] [Google Scholar]
- 5.Lupovitch A, England ER, Chen R. Non-puerperal uterine inversion in association with uterine sarcoma: case report in a 26-year-old and review of the literature. Gynecol Oncol 2005;97:938–41. [DOI] [PubMed] [Google Scholar]
- 6.Kilpatrick CC, Chohan L, Maier RC. Chronic nonpuerperal uterine inversion and necrosis: a case report. J Med Case Reports 2010;4:381 PMID: 21108785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krenning RA, Dorr PJ, de Groot WH, et al. Non-puerperal uterine inversion: case report. Br J Obstet Gynaecol 1982;89:247–9. [DOI] [PubMed] [Google Scholar]
- 8.Gowri V. Uterine inversion and corpus malignancies: a historical review. Obstet gynecol Surv 2000;55:703–7. PMID: 11075734. [DOI] [PubMed] [Google Scholar]
- 9.Adesiyun AG. Septic postpartum uterine inversion: case report. Singapore Med J 2007;48:943–5. PMID: 17909681. [PubMed] [Google Scholar]
- 10.Hostetler DR, Bosworth MF. Uterine Inversion: a life-threatening obstetric emergency. J Am Board Fam Pract 2000;13:120–3. PMID: 10764194. [DOI] [PubMed] [Google Scholar]