Abstract
Objective:
To examine the prevalence of nightmares in people with psychosis and to describe the link between nightmares and sleep quality, psychotic, affective, and cognitive symptoms.
Methods:
Forty participants with psychotic symptoms completed an assessment of nightmares, sleep quality, positive symptoms of psychosis, affect, posttraumatic stress, social functioning, and working memory.
Results:
Among the patients, 55% reported weekly distressing nightmares. Experience of more frequent nightmares was related to poorer sleep quality and sleep efficiency. More distressing nightmares were positively associated with greater delusional severity, depression, anxiety, stress, and difficulties with working memory.
Conclusions:
Nightmares might be common in those with psychosis and are associated with increased day- and nighttime impairment. Future research should investigate treatments for nightmares, for people presenting with psychotic symptoms.
Keywords: nightmares, psychoses, psychotic symptoms, sleep, schizophrenia, affect, working memory
Abstract
Objectif :
Examiner la prévalence des cauchemars chez des personnes souffrant de psychose et décrire le lien entre les cauchemars et la qualité du sommeil, les symptômes psychotiques, affectifs, et cognitifs.
Méthodes :
Quarante participants ayant des symptômes psychotiques ont répondu à une évaluation des cauchemars, de la qualité du sommeil, des symptômes positifs de la psychose, de l’affect, du stress post-traumatique, du fonctionnement social et de la mémoire de travail.
Résultats :
Parmi les patients, 55 % ont déclaré des cauchemars troublants hebdomadaires. L’expérience de cauchemars plus fréquents était liée à une mauvaise qualité et une mauvaise efficacité du sommeil. Plus de cauchemars troublants étaient associés positivement à une gravité accrue des idées délirantes, à la dépression, à l’anxiété, au stress, et aux difficultés de la mémoire de travail.
Conclusions :
Les cauchemars peuvent être fréquents chez les personnes souffrant de psychose et ils sont associés à une incapacité accrue de jour et de nuit. La future recherche devrait se pencher sur les traitements des cauchemars pour les personnes présentant des symptômes psychotiques.
The past 5 years have drawn attention to major sleep disruption in people with psychosis.1–4 Poor sleep is a risk factor for developing first-episode psychosis5 and is predictive of the onset and maintenance of paranoid ideas,6 a poorer-quality of life,7,8 and frontal–executive task performance difficulties.4
Attempts to characterize the sleep patterns of people with psychosis have revealed various disturbances.2,9 These include increased time spent in bed, higher sleep latency, disrupted melatonin sulphate levels, circadian rhythm disruption, and lastly, more fragmented sleep.2,9 It is likely that numerous different sleep disorders account for this variety of sleep profiles, and that each requires a different treatment focus. For example, there is already evidence of increased rates of both insomnia3 and obstructive sleep apnea10 in samples with psychosis. A sleep disorder that has received little attention in this group is nightmare disorder.
Nightmares
Nightmares are typically characterized by awakening from rapid-eye movement sleep with recollection of disturbing mental activity.11 Large epidemiologic studies estimate that weekly nightmares occur in 0.9% to 6.8% of the general population.11–13 Nevertheless, for people with diagnoses such as PTSD14,15 and BPD,16 this estimated prevalence rate increases to 49% to 71%. Nightmares have been associated with increased psychological distress,16,17 worse physical health outcomes,18 and increased risk for self-harm and suicide.16,19 Whereas previously nightmares have been viewed as a symptom of other disorders, they are now regarded as a specific, comorbid, and treatable condition.18,20,21
It has been proposed that nightmares and psychotic symptoms represent a common domain with shared etiology.22 There is preliminary evidence that this may be the case. Frequent nightmares in early childhood increased the risk of later psychotic experiences in adolescents.23 Nightmare-related distress predicted levels of paranoia and psychoticism in a sample of healthy students,24 and increased frequency of nightmares have been observed in people with SSD diagnoses.22,25
Clinical Implications
Reports of nightmares should form part of a routine assessment for people with psychotic symptoms presenting with disturbed sleep.
People experiencing more distressing nightmares tend to present with more severe daytime symptomatology.
Nightmare-related distress may prove to be a novel target for psychological therapies for people experiencing symptoms of psychosis.
Limitations
A convenience sample was recruited and as such may not be representative of all people experiencing symptoms of psychosis.
Our study collected cross-sectional data, and causal statements about associations cannot be discerned.
Our study was powered to detect medium-to-large correlations, increasing the risk of type II error for some analyses.
Study Aims
Our study aimed to investigate the phenomenology of nightmares in the context of psychosis. Four key hypotheses were tested:
Nightmares will be more prevalent in the context of psychosis than in the general population.
Nightmare frequency will be associated with poorer sleep (PSQI sleep quality and sleep efficiency).
Nightmare-related distress, rather than the frequency with which they occur, will best account for the association between nightmares and daytime impairment (psychotic symptoms, affective symptoms, and daytime activities) while controlling for shared variance.
Poorer sleep quality will be associated with poorer working memory. More specifically, it is expected that a higher frequency of nightmares will be associated with poorer working memory (a cognitive deficit commonly observed in people experiencing psychosis26,27).
Method
Participants
Forty participants were recruited from in- and outpatient services in 2 south London NHS foundation trusts. Inclusion criteria were for the participant to be aged 18 or older; to have experienced symptoms of psychosis; to have proficient use of the English language for the purpose of completing questionnaires; and to be able to provide informed consent. Exclusion criteria included a primary diagnosis of alcohol or substance dependency, an organic syndrome, such as a dementia, or having a learning disability. Participants were aware that the study was investigating “sleep patterns,” but the information sheet stated the following: “whether you sleep very well, or have had sleep difficulties we would like to hear from you.”
Measures
Sociodemographic, diagnosis, prescribed medication, and alcohol and drug use data were collected. Where participants were unsure of their diagnosis, prescribed medication name and (or) dose was taken from medical notes.
The PSQI28 measured sleep quality during the month prior to assessment. The sleep efficiency (number of hours asleep divided by number of hours in bed) and overall sleep quality scales were used for analysis. The 7 PSQI component scores have good internal consistency (Cronbach α = 0.83) and yield acceptable test–retest reliability.28 The measure has previously been used in samples with psychosis.29
A retrospective dream log was adapted from Levin and Fireman.24 Participants were asked to indicate how many nightmares they estimated experiencing during the past 2 weeks (14 nights). If the participant had experienced at least 1 nightmare, they were asked to pick their worst nightmare and rate it on a 7-point Likert scale for intensity, vividness, and distress, and also to mark whether it was recurrent (yes or no). Retrospective nightmare logs measuring up to 1 month in the past are known to yield similar results to prospective measures in a sample of undergraduate students.29
The Psychotic Symptoms Rating Scale
The PSYRATS30 measured the severity of 11 dimensions of auditory hallucinations and 6 dimensions of delusions via 5-point scales (0 to 4). Evaluation of the PSYRATS delusions and hallucinations scales indicate good interrater reliability30 and concurrent validity with the Positive and Negative Syndromes Scale.31
The Depression, Anxiety and Stress Scales
The DASS-2132 provide 3 scales of these negative emotional states, derived from 21 self-report items. The scales reflect experiences during the preceding week. The 3 scales have demonstrated very good internal consistency (all Cronbach α > 0.90) and good test–retest reliability for a sample with schizophrenia.33
The Posttraumatic Diagnostic Scale
The PDS34 was administered as a self-report measure of PTSD symptomatology. The measure of symptom severity was used for analysis. It has been shown to have high internal consistency, test–retest reliability, and high diagnostic validity when compared with the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Axis I disorders35 and good sensitivity and specificity.34 The questionnaire has been used in a previous study recruiting people with psychotic symptoms.36
The Time Budget Questionnaire
The Time Budget Questionnaire37 was administered to assess use of time during the preceding week. The measure was designed specifically for people with symptoms of psychosis. Activities were rated according to complexity of activity and effort required. The measure has been shown to have convergent validity regarding activity levels and social contact.37
The Digit Span Subtest
The Digit Span subtest from the Wechsler Memory Scale, Third Edition,38 was administered to assess working memory and offered a standardized (scaled) score for each participant. The Digit Span has a reliability coefficient of 0.86.
Procedure
The study was approved by City Road and Hampstead NHS Research Ethics Committee (11/LO/2045). Informed consent was obtained, following which each participant completed the full assessment, with breaks as required.
Participants provided demographic, medication, and alcohol and drug use data. Following this, participants completed the PSYRATS for hallucinations and delusions with the researcher. The PSQI, dream log,24 and DASS-21 were completed independently but with the option of using the researcher as a scribe. Following this, the PDS, the Time Budget Questionnaire, and the Digit Span subtest were completed with the researcher. The order of assessment measures was held constant across participants. Diagnosis was confirmed by medical records from the treating psychiatrist; clinicians in the United Kingdom use the World Health Organization’s International Classification of Diseases system.
Analysis
PASW Statistics for Windows, version 18.0,39 was used to perform all inferential statistics, with the exception of 95% confidence interval for proportions, which was calculated using an online calculator by Graphpad.com.40
Because the distribution of nightmare frequency and distress data was skewed, nonparametric correlation coefficients (2-tailed Spearman rho) were used to assess hypotheses 2 and 4. Partial Spearman correlation coefficients (2-tailed) were carried out by performing partial Pearson product–moment correlation coefficient with ranked data.41 Hochberg’s improved Bonferroni procedure was used to adjust for multiple comparisons.
Results
Demographics and Clinical Characteristics of the Sample
Letters were sent to 108 people on a research register held by a specialist psychosis clinic (PICuP, SLaM). Among the 108 invitation letters sent, 28 participants were recruited. Among 21 other patients referred by their care team, 12 participants were recruited.
The first 40 participants who consented took part in the study. Twenty-five (62.5%) were male, with age ranging from 18 to 68 years (mean 41.9); 57.5% were white (British, Irish or Other), the remainder were from black and minority ethnic groups (20% Black African, 5% Black Caribbean, 2.5% Asian, and 15% Other). Four participants were inpatients, 36 were outpatients. Inpatients experienced a mean of 0 nightmares during the past 2 weeks (SD 0), while outpatients experienced 6.51 (SD 13.12). The sleep quality of inpatients revealed a mean PSQI score of 5.00 (SD 0.50), while for outpatients it was 10.00 (SD 4.08).
Clinical characteristics are outlined in Table 1. All participants experienced auditory hallucinations or delusions. Length of time experiencing positive symptoms of psychosis ranged from 3 months to 41 years. There was 1 person who had a missing value for 1 question on the PSYRATS for delusions, across all 40 participants. This score was calculated from the mean of the scores from the other 5 items for that participant.
Table 1.
Clinical characteristics of the sample, n = 40
| Characteristic | n | % | |
|---|---|---|---|
| Psychotic symptoms (week preceding assessment) | |||
| Auditory hallucinations (voices) | 27 | 67.5 | |
| Delusional belief | 35 | 87.5 | |
| Trauma | |||
| Experienced at least 1 trauma | 36 | 90.0 | |
| Experience of childhood sexual abuse | 12 | 30.0 | |
| PTSD screen (PDS) | |||
| Positive | 17 | 42.5 | |
| Negative | 20 | 50.0 | |
| Unable to categorize | 3 | 7.5 | |
| Sleep | |||
| One nightmare during past 14 nights | |||
| Yes | 28 | 70.0 | |
| No | 12 | 30.0 | |
| Sleep quality (PSQI, cut-off >5) | |||
| Poor sleepers | 34 | 85.0 | |
| Good sleepers | 6 | 15.0 | |
| Current medication | |||
| Antipsychotic | 35 | 87.5 | |
| Antidepressant | 17 | 42.5 | |
| Mood stabilizer | 7 | 17.5 | |
| Hypnotic | 5 | 12.5 | |
|
|
|||
| Nonclinical n (%) | Mild to moderate n (%) | Severe to extremely severe, n (%) | |
|
|
|||
| Affective symptoms | |||
| Depression | 7 (17.7) | 16 (40.0) | 17 (42.5) |
| Anxiety | 9 (22.5) | 10 (25.0) | 21 (52.5) |
| Stress | 12 (30.0) | 16 (40.0) | 12 (30.0) |
PDS = Posttraumatic Diagnostic Scale; PSQI = Pittsburgh Sleep Quality Index; PTSD = posttraumatic stress disorder
Thirty-six of the 40 (90%) participants had a current SSD diagnosis or bipolar affective disorder with psychotic symptoms; the remaining 4 participants all had active symptoms of psychosis and were recruited from a specialist psychosis clinic (PICuP, SLaM).
Seventeen (42.5%) participants screened positive for PTSD. Eleven of these 17 participants (65%) reported weekly nightmares. This was not significantly higher than the 10 of 20 (50%) participants who reported weekly nightmares but did not screen positive for PTSD (n = 37; χ2 = 0.81, df = 1, P > 0.05). The median nightmare distress score for participants who screened positive for PTSD was 5.00, which was not significantly different from the median (6.00) of those who screened negative for PTSD (U = 88.50, z = −0.13, P = 0.90).
Nine of the 40 participants had taken nonprescribed drugs or medications in the week prior to assessment date. Among these 9, 2 reported taking cannabis (5% of total sample). The remaining 7 took over-the-counter medications (for example, Kalms Tablets, paracetamol, and multivitamins). Median weekly alcohol intake was 0 units (range 0 to 80 units). The recommended daily intake of alcohol in the United Kingdom is 2 to 3 units for females and 3 to 4 units for males.42
The antipsychotic dose was converted into chlorpromazine equivalents using published tables.2,43,44 A medium positive correlation was found between antipsychotic dose and PSYRATS for hallucinations (rs = 0.33, df = 40, P < 0.05), sleep quality (rs = −0.40, df = 40, P < 0.05), and sleep efficiency (rs = −0.40, df = 40, P < 0.01). Analyses including these 3 variables controlled for chlorpromazine equivalent antipsychotic dose. No significant associations were found between antipsychotic dose and delusional severity, affective measures, working memory, and the time budget measure (all P > 0.05).
Hypothesis 1. Nightmares will be more prevalent in the context of psychosis than in the general population
This hypothesis was supported. Among the 40 participants with psychosis, 22 (55.0%, 95% CI 38.5% to 70.7%) experienced at least weekly nightmares (that is, 2 or more nightmares during a 2-week period). The confidence intervals from the current sample does not include the weekly prevalence rate (0.9 to 6.8) from large epidemiologic studies of the general population,11–13 which implies that the difference is statistically significant (Figure 1).
Figure 1.
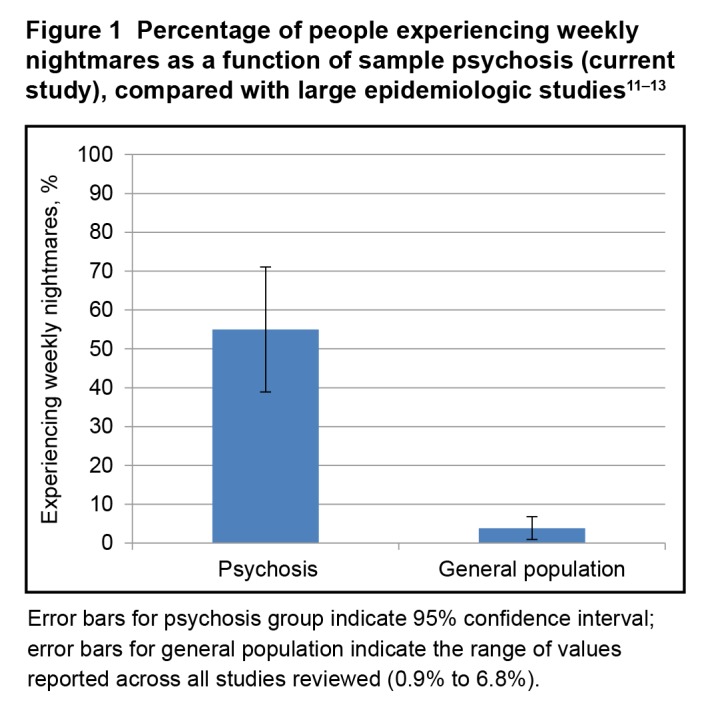
Percentage of people experiencing weekly nightmares as a function of sample psychosis (current study), compared with large epidemiologic studies11–13
Error bars for psychosis group indicate 95% confidence interval; error bars for general population indicate the range of values reported across all studies reviewed (0.9% to 6.8%).
Hypothesis 2. Nightmare frequency will be associated with poorer sleep (sleep quality and sleep efficiency)
This hypothesis was supported. A large positive correlation was found between nightmare frequency and overall (PSQI) sleep quality while controlling for antipsychotic dose (partial rs = 0.48, df = 37, P < 0.01). Nightmare frequency was also negatively correlated with sleep efficiency (hours asleep/hours spent in bed × 100) while controlling for antipsychotic dose (partial rs = −0.51, df = 37, P < 0.01).
Hypothesis 3. Nightmare-related distress, rather than the frequency with which they occur, will best account for the association between nightmares and daytime impairment (psychotic symptoms, affective symptoms, and daytime activities) while controlling for shared variance
This hypothesis was supported, as can be seen in Table 2. Nightmare distress was significantly correlated with 4 measures of daytime psychological functioning: delusional severity, depression, anxiety, and stress. In contrast, there were trends indicating that nightmare frequency was correlated with 2 measures of psychological functioning: depression and daytime activity. However, these fell short of significance after controlling for multiple comparisons.
Table 2.
Spearman partial correlations of nightmare frequency and nightmare distress to measures of daytime impairment, controlling for shared variance; correlations including PSYRATS hallucinations additionally controlled for antipsychotic dose
| Variable | Nightmare frequency Spearman ρ | Hochberg corrected P | Nightmare distress Spearman ρ | Hochberg corrected P |
|---|---|---|---|---|
| Daytime symptoms | ||||
| PSYRATS delusions (n = 25) | 0.01 | 0.97 | 0.59 | <0.001 |
| PSYRATS hallucinations (n = 24) | 0.27 | 0.90 | 0.32 | 0.36 |
| DASS-21 stress (n = 25) | 0.21 | 0.90 | 0.49 | 0.04 |
| DASS-21 anxiety (n = 25) | 0.21 | 0.90 | 0.48 | 0.04 |
| DASS-21 depression (n = 25) | 0.42 | 0.18 | 0.50 | 0.04 |
| PTSD symptom severity (PDS, n = 25) | 0.09 | 0.97 | −0.01 | 0.96 |
| Activity levels | ||||
| Daytime activity (Time Budget Questionnaire, n = 24) | −0.42 | 0.18 | −0.24 | 0.50 |
DASS-21 = Depression, Anxiety and Stress Scale, 21-item version; PDS = Posttraumatic Diagnostic Scale; PSYRATS = Psychotic Symptoms Rating Scale; PTSD = posttraumatic stress disorder
Hypothesis 4. Poorer sleep quality will be associated with poorer working memory. More specifically, it is expected that a higher frequency of nightmares will be associated with poorer working memory
This hypothesis was not supported. Overall sleep quality was not significantly correlated with working memory (partial rs = −0.06, df = 36, P = 0.70) while controlling for antipsychotic dose. Nightmare frequency was also not significantly correlated with working memory (rs = 0.02, df = 39, P = 0.90).
Exploratory analysis was undertaken to assess the link between nightmare distress and working memory. This revealed a large negative correlation between nightmare distress and working memory (rs = −0.50, df = 27, P < 0.01). This remained significant when controlling for variance in delusional severity (partial rs = −0.42, df = 24, P < 0.05) and depression (partial rs = −0.43, df = 24, P < 0.05), but not anxiety (partial rs = −0.36, df = 24, P = 0.07).
Discussion
This is the first study to investigate the occurrence of nightmares within a sample experiencing symptoms of psychosis and their relation with symptoms. The key findings are that over one-half of the sample with psychosis (55%) reported experiencing weekly distressing nightmares, reflective of moderately severe pathology.11 This is significantly higher than estimates of the prevalence rate (0.9% to 6.8%) from the general population.11–13 People with psychosis experiencing frequent nightmares tended to have poorer sleep efficiency and sleep quality. However, it was higher levels of nightmare distress that was associated with more severe delusions, depression, anxiety, stress, and poorer working memory.
The frequency of weekly nightmares in our sample was closely matched to other clinical groups, for example, PTSD (52% to 71%),14,15 and BPD (49%).16 This is an important finding; nightmares are one of the most commonly reported symptoms of PTSD45 and form part of the diagnostic criteria, yet our’s is the first study to show that nightmares are also a common problem for people with psychosis.
The finding that nightmare distress better accounts for links with daytime psychiatric symptomatology than the prevalence of nightmares extends the results of a previous study from a nonclinical, student sample.24 The finding that nightmare distress (rather than frequency) is key in determining psychological functioning also fits with investigations of the positive symptoms of psychosis. There is considerable evidence that members of the general population experience voices and unusual beliefs46–48; however, it is the distress associated with these experiences that distinguishes whether a person has a need for care.49–51
A PTSD screen revealed 42.5% of the current sample had probable PTSD, in line with high rates found in other samples with psychosis (14% to 78%).52–54 However, nightmare distress was not correlated with PTSD symptoms in this sample with psychosis, and those who screened positive for PTSD did not experience more frequent nightmares or higher nightmare distress. Given that nightmares are considered a hallmark of PTSD, this was a surprising result. It is possible that nightmares are a common problem for people with psychosis in general, irrespective of PTSD symptoms.
Our study has several limitations. The sample was a convenience sample, which may result in a sample with lower levels of functional impairment, particularly in relation to the low levels of reported substance and alcohol use. Our study used a retrospective measurement of nightmares that has not been validated for people experiencing psychosis. The study could have benefited from a matched control group. For example, a clinical control group with affective symptoms alone would allow further investigation about whether nightmares are associated purely with psychotic symptoms, or rather whether they are better related to comorbid depression or anxiety. In addition, our study was a small, initial evaluation of a previously unexplored area. It was powered to detect a medium correlation between nightmares and daytime psychopathology, as found in a previous nonclinical sample.24 A larger sample would allow for increased power to investigate the nonsignificant but promising associations between nightmare-related distress and both auditory hallucinations and activity levels, as well as controlling for the impact that individual medications (and their withdrawal) have on sleep and the emotional tone of dreams.55
Future studies may try to elucidate the direction of causality between experiencing distressing nightmares and severity of delusions. Dreaming has been theorized to play a role in fear extinction and emotion regulation.11,56–58 These models would predict that nightmares result from disrupted processing of distressing daytime experiences via usual dreaming. However, an alternative model may suggest that sleep disturbance (and therefore nightmares) are key and result in the formation and maintenance of delusional ideas.59 It is, of course, possible that the relation between nightmares and severity of daytime symptoms is bidirectional, as has been found in PTSD samples.17 A more detailed analysis of the direction of causality and mechanism linking nightmares, delusional severity, and affective symptoms was beyond the scope of our study, but would be an interesting area for further investigation.
One method to investigate the causal relation between nightmares and delusional severity, affective symptoms, and working memory would be to investigate the impact of a nightmare-specific treatment such as Imagery Rehearsal Training, which has a good evidence base for treating posttraumatic nightmares,45,60–65 and early evidence indicates that this is an acceptable treatment for people with psychotic symptoms.66
Conclusion
Nightmares may be a common clinical characteristic for people experiencing psychotic symptoms. Further, the distress associated with them is associated with worse daytime symptoms. These results support the assertion of Krakow18 that nightmares should be considered as a separate problem that can be comorbid with a range of other diagnoses, including BPD,16 primary insomnia,67 PTSD,14,15 and now psychosis.
Acknowledgments
We thank the participants who gave their time to take part in the study and the teams that facilitated recruitment within the South London and Maudsley National Health Service (NHS) Foundation Trust, particularly the Psychological Interventions Clinic for outpatients with Psychosis and Oxleas NHS Foundation Trust (Dr Marina Richards and Natalie Cook).
The authors have no conflicts of interest to report.
Abbreviations
- BPD
borderline personality disorder
- DASS-21
Depression, Anxiety and Stress Scale, 21-item version
- NHS
National Health Service
- PDS
Posttraumatic Diagnostic Scale
- PICuP
Psychological Interventions Clinic for outpatients with Psychosis
- PSQI
Pittsburgh Sleep Quality Index
- PSYRATS
Psychotic Symptoms Rating Scale
- PTSD
posttraumatic stress disorder
- SLaM
South London and Maudsley NHS Foundation Trust
- SSD
schizophrenia spectrum disorder
References
- 1.Wilson S, Argyropoulos S. Sleep in schizophrenia: time for closer attention. Br J Psychiatry. 2012;200(4):273–274. doi: 10.1192/bjp.bp.111.104091. [DOI] [PubMed] [Google Scholar]
- 2.Wulff K, Dijk D-J, Middleton B, et al. Sleep and circadian rhythm disruption in schizophrenia. Br J Psychiatry. 2012;200(4):308–316. doi: 10.1192/bjp.bp.111.096321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freeman D, Pugh K, Vorontsova N, et al. Insomnia and paranoia. Schizophr Res. 2009;108(1–3):280–284. doi: 10.1016/j.schres.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bromundt V, Köster M, Georgiev-Kill A, et al. Sleep–wake cycles and cognitive functioning in schizophrenia. Br J Psychiatry. 2011;198(4):269–276. doi: 10.1192/bjp.bp.110.078022. [DOI] [PubMed] [Google Scholar]
- 5.Ruhrmann S, Schultz-Lutter F, Salokangas R, et al. Prediction of psychosis in adolescents and young adults at high risk. Arch Gen Psychiatry. 2010;67(3):241–251. doi: 10.1001/archgenpsychiatry.2009.206. [DOI] [PubMed] [Google Scholar]
- 6.Freeman D, Stahl D, McManus S, et al. Insomnia, worry, anxiety and depression as predictors of the occurrence and persistence of paranoid thinking. Soc Psychiatry Psychiatr Epidemiol. 2012;47(8):1195–1203. doi: 10.1007/s00127-011-0433-1. [DOI] [PubMed] [Google Scholar]
- 7.Hofstetter JR, Lysaker PH, Mayeda AR. Quality of sleep in patients with schizophrenia is associated with quality of life and coping. BMC Psychiatry. 2005;5:13. doi: 10.1186/1471-244X-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ritsner M, Kurs R, Ponizovsky A, et al. Perceived quality of life in schizophrenia: relationships to sleep quality. Qual Life Res. 2004;13(4):783–791. doi: 10.1023/B:QURE.0000021687.18783.d6. [DOI] [PubMed] [Google Scholar]
- 9.Afonso P, Figueira ML, Paiva T. Sleep–wake patterns in schizophrenia patients compared to healthy controls. World J Biol Psychiatry. 2013(53):1–8. doi: 10.3109/15622975.2012.756987. [DOI] [PubMed] [Google Scholar]
- 10.Winkelman JW. Schizophrenia, obesity, and obstructive sleep apnea. J Clin Psychiatry. 2001;62(1):8–11. doi: 10.4088/jcp.v62n0103. [DOI] [PubMed] [Google Scholar]
- 11.Nielsen T, Levin R. Nightmares: a new neurocognitive model. Sleep Med Rev. 2007;11(4):295–310. doi: 10.1016/j.smrv.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Li SX, Zhang B, Li AM, et al. Prevalence and correlates of frequent nightmares: a community-based 2-phase study. Sleep. 2010;33(6):774–780. doi: 10.1093/sleep/33.6.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janson C, Gislason T, De Backer W, et al. Prevalence of sleep disturbances among young adults in three European countries. Sleep. 1995;18(7):589–597. [PubMed] [Google Scholar]
- 14.Leskin GA, Woodward SH, Young HE, et al. Effects of comorbid diagnoses on sleep disturbance in PTSD. J Psychiatr Res. 2002;36(6):449–452. doi: 10.1016/s0022-3956(02)00025-0. [DOI] [PubMed] [Google Scholar]
- 15.Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929–933. doi: 10.1176/ajp.155.7.929. [DOI] [PubMed] [Google Scholar]
- 16.Semiz UB, Basoglu C, Ebrinc S, et al. Nightmare disorder, dream anxiety, and subjective sleep quality in patients with borderline personality disorder. Psychiatry Clin Neurosci. 2008;62(1):48–55. doi: 10.1111/j.1440-1819.2007.01789.x. [DOI] [PubMed] [Google Scholar]
- 17.van Liempt S. Sleep disturbance and PTSD: a perceptual circle. Eur J Psychotraumatol. 2012;3:19142. doi: 10.3402/ejpt.v3i0.19142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krakow B. Nightmare complaints in treatment-seeking patients in clinical sleep medicine settings: diagnostic and treatment implications. Sleep. 2006;29(10):1313–1319. doi: 10.1093/sleep/29.10.1313. [DOI] [PubMed] [Google Scholar]
- 19.Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73(9):e1160–e1167. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- 20.Spoormaker VI. A cognitive model of recurrent nightmares. Int J Dream Res. 2008;1(1):15–22. [Google Scholar]
- 21.Aurora RN, Zak RS, Auerbach SH, et al. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389–401. [PMC free article] [PubMed] [Google Scholar]
- 22.Koffel E, Watson D. Unusual sleep experiences, dissociation, and schizotypy: evidence for a common domain. Clin Psychol Rev. 2009;29(6):548–559. doi: 10.1016/j.cpr.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher HL, Lereya ST, Thompson A, et al. Childhood parasomnias and psychotic experiences at age 12 years in a United Kingdom birth cohort. Sleep. 2014;37(3):475–482. doi: 10.5665/sleep.3478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levin R, Fireman G. Nightmare prevalence, nightmare distress, and self-reported psychological disturbance. Sleep. 2002;25(2):205–212. [PubMed] [Google Scholar]
- 25.Lusignan F-A, Zadra A, Dubuc M-J, et al. Dream content in chronically-treated persons with schizophrenia. Schizophr Res. 2009;112(1–3):164–173. doi: 10.1016/j.schres.2009.03.032. [DOI] [PubMed] [Google Scholar]
- 26.Schaefer J, Giangrande E, Weinberger DR, et al. The global cognitive impairment in schizophrenia: consistent over decades and around the world. Schizophr Res. 2013;150(1):42–50. doi: 10.1016/j.schres.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fatouros-Bergman H, Cervenka S, Flyckt L, et al. Meta-analysis of cognitive performance in drug-naïve patients with schizophrenia. Schizophr Res. 2014;158(1–3):156–162. doi: 10.1016/j.schres.2014.06.034. [DOI] [PubMed] [Google Scholar]
- 28.Buysse DJ, Reynolds CF, 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 29.Robert G, Zadra A. Measuring nightmare and bad dream frequency: impact of retrospective and prospective instruments. J Sleep Res. 2008;17(2):132–139. doi: 10.1111/j.1365-2869.2008.00649.x. [DOI] [PubMed] [Google Scholar]
- 30.Haddock G, McCarron J, Tarrier N, et al. Scales to measure dimensions of hallucinations and delusions: the Psychotic Symptom Rating Scales (PSYRATS) Psychol Med. 1999;29(4):879–889. doi: 10.1017/s0033291799008661. [DOI] [PubMed] [Google Scholar]
- 31.Drake R, Haddock G, Tarrier N, et al. The Psychotic Symptom Rating Scales (PSYRATS): their usefulness and properties in first episode psychosis. Schizophr Res. 2007;89(1–3):119–122. doi: 10.1016/j.schres.2006.04.024. [DOI] [PubMed] [Google Scholar]
- 32.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney (AU): Psychology Foundation; 1995. [Google Scholar]
- 33.Huppert JD, Smith TE, Apfeldorf WJ. Use of self-report measures of anxiety and depression in outpatients with schizophrenia: reliability and validity. J Psychopathol Behav Assess. 2002;24(4):275–283. [Google Scholar]
- 34.Foa EB, Cashman L, Jaycox L, et al. The validation of a self-report measure of posttraumatic stress disorder: the Posttraumatic Diagnostic Scale. Psychol Assess. 1997;9(4):445–451. [Google Scholar]
- 35.Spitzer RL, Williams JBW, Gibbon M, et al. Structured Clinican Interview for DSM-III-R Axis II Disorders (SCID-II) Washington DC: American Psychiatric Press; 1990. [Google Scholar]
- 36.Steel C, Haddock G, Tarrier N, et al. Auditory hallucinations and posttraumatic stress disorder within schizophrenia and substance abuse. J Nerv Ment Dis. 2011;199(9):709–711. doi: 10.1097/NMD.0b013e318229d6e8. [DOI] [PubMed] [Google Scholar]
- 37.Jolley S, Garety PA, Ellett L, et al. A validation of a new measure of activity in psychosis. Schizophr Res. 2006;85(1–3):288–295. doi: 10.1016/j.schres.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 38.Wechsler D. Wechsler Memory Scale. 3rd ed. London (GB): The Psychological Corporation; 1998. [Google Scholar]
- 39.SPSS Inc. PASW statistics for Windows, version 180. Chicago (IL): SPSS Inc; 2009. [Google Scholar]
- 40.Graphpad Software Inc Confidence interval of a proportion or count [Internet] [cited 2013 Feb 15]. Available from: http://www.graphpad.com/quickcalcs/confInterval1.
- 41.Reynolds HT. Nonparametric partial correlation and causal analysis. Soc Methods Res. 1974;2(3):376–392. [Google Scholar]
- 42.Department of Health NHS choices: track your drinking [Internet] 2012. [cited 2013 Feb 10]. Available from: http://www.nhs.uk/Livewell/alcohol/Pages/Alcoholtracker.aspx.
- 43.Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry. 2003;64:663–667. doi: 10.4088/jcp.v64n0607. [DOI] [PubMed] [Google Scholar]
- 44.Atkins M, Burgess A, Bottomley C, et al. Chlorpromazine equivalents: a consensus of opinion for both clinical and research applications. Psychiatr Bull. 1997;21(4):224–226. [Google Scholar]
- 45.Nappi CM, Drummond SP, Thorp SR, et al. Effectiveness of imagery rehearsal therapy for the treatment of combat-related nightmares in veterans. Behav Ther. 2010;41(2):237–244. doi: 10.1016/j.beth.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 46.Johns LC, Cannon M, Singleton N, et al. Prevalence and correlates of self-reported psychotic symptoms in the British population. Br J Psychiatry. 2004;185:298–305. doi: 10.1192/bjp.185.4.298. [DOI] [PubMed] [Google Scholar]
- 47.Freeman D, Garety PA, Bebbington PE, et al. Psychological investigation of the structure of paranoia in a nonclinical population. Br J Psychiatry. 2005;186:427–435. doi: 10.1192/bjp.186.5.427. [DOI] [PubMed] [Google Scholar]
- 48.Bentall RP, Claridge GS, Slade PD. The multidimensional nature of schizotypal traits: a factor analytic study with normal subjects. Br J Clin Psychol. 1989;28(4):363–375. doi: 10.1111/j.2044-8260.1989.tb00840.x. [DOI] [PubMed] [Google Scholar]
- 49.Peters E, Day S, McKenna J, et al. Delusional ideation in religious and psychotic populations. Br J Clin Psychol. 1999;38(1):83–96. doi: 10.1348/014466599162683. [DOI] [PubMed] [Google Scholar]
- 50.Van Os J, Verdoux H, Maurice-Tison S, et al. Self-reported psychosis-like symptoms and the continuum of psychosis. Soc Psychiatry Psychiatr Epidemiol. 1999;34(9):459–463. doi: 10.1007/s001270050220. [DOI] [PubMed] [Google Scholar]
- 51.Davies MF, Griffin M, Vice S. Affective reactions to auditory hallucinations in psychotic, evangelical and control groups. Br J Clin Psychol. 2001;40(4):361–370. doi: 10.1348/014466501163850. [DOI] [PubMed] [Google Scholar]
- 52.Andrew EM, Gray NS, Snowden RJ. The relationship between trauma and beliefs about hearing voices: a study of psychiatric and non-psychiatric voice hearers. Psychol Med. 2008;38(10):1409–1417. doi: 10.1017/S003329170700253X. [DOI] [PubMed] [Google Scholar]
- 53.Neria Y, Bromet EJ, Sievers S, et al. Trauma exposure and posttraumatic stress disorder in psychosis: findings from a first-admission cohort. J Consult Clin Psychol. 2002;70(1):246–251. doi: 10.1037//0022-006x.70.1.246. [DOI] [PubMed] [Google Scholar]
- 54.Mueser KT, Goodman LB, Trumbetta SL, et al. Trauma and posttraumatic stress disorder in severe mental illness. J Consult Clin Psychol. 1998;66(3):493–499. doi: 10.1037//0022-006x.66.3.493. [DOI] [PubMed] [Google Scholar]
- 55.Tribl GG, Wetter TC, Schredl M. Dreaming under antidepressants: a systematic review on evidence in depressive patients and healthy volunteers. Sleep Med Rev. 2013;17(2):133–142. doi: 10.1016/j.smrv.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 56.Desseilles M, Dang-Vu TT, Sterpenich V, et al. Cognitive and emotional processes during dreaming: a neuroimaging view. Conscious Cogn. 2011;20(4):998–1008. doi: 10.1016/j.concog.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 57.Gujar N, McDonald SA, Nishida M, et al. A role for REM sleep in recalibrating the sensitivity of the human brain to specific emotions. Cereb Cortex. 2011;21(1):115–123. doi: 10.1093/cercor/bhq064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nishida M, Pearsall J, Buckner RL, et al. REM sleep, prefrontal theta, and the consolidation of human emotional memory. Cereb Cortex. 2009;19(5):1158–1166. doi: 10.1093/cercor/bhn155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Freeman D, Garety PA, Kuipers E, et al. A cognitive model of persecutory delusions. Br J Clin Psychol. 2002;41(Pt 4):331–347. doi: 10.1348/014466502760387461. [DOI] [PubMed] [Google Scholar]
- 60.Krakow B, Hollifield M, Schrader R, et al. A controlled study of imagery rehearsal for chronic nightmares in sexual assault survivors with PTSD: a preliminary report. J Trauma Stress. 2000;13(4):589–609. doi: 10.1023/A:1007854015481. [DOI] [PubMed] [Google Scholar]
- 61.Davis JL, Wright DC. Randomized clinical trial for treatment of chronic nightmares in trauma-exposed adults. J Trauma Stress. 2007;20(2):123–133. doi: 10.1002/jts.20199. [DOI] [PubMed] [Google Scholar]
- 62.Davis JL, Rhudy JL, Pruiksma KE, et al. Physiological predictors of response to exposure, relaxation, and rescripting therapy for chronic nightmares in a randomized clinical trial. J Clin Sleep Med. 2011;7(6):622–631. doi: 10.5664/jcsm.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thünker J, Pietrowsky R. Effectiveness of a manualized imagery rehearsal therapy for patients suffering from nightmare disorders with and without a comorbidity of depression or PTSD. Behav Res Ther. 2012;50(9):558–564. doi: 10.1016/j.brat.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 64.Casement MD, Swanson LM. A meta-analysis of imagery rehearsal for post-trauma nightmares: effects on nightmare frequency, sleep quality, and posttraumatic stress. Clin Psychol Rev. 2012;32(6):566–574. doi: 10.1016/j.cpr.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Forbes D, Phelps AJ, McHugh AF, et al. Imagery rehearsal in the treatment of posttraumatic nightmares in Australian veterans with chronic combat-related PTSD: 12-month follow-up data. J Trauma Stress. 2003;16(5):509–513. doi: 10.1023/A:1025718830026. [DOI] [PubMed] [Google Scholar]
- 66.Sheaves B. The phenomenology of nightmares in the context of psychosis, with a case series of imagery rescripting. London (GB): King’s College London; 2013. [Google Scholar]
- 67.Ohayon MM, Morselli PL. Parasomnias prevalence of nightmares and their relationship to psychopathology and daytime functioning in insomnia subjects. Sleep. 1997;20(5):340–348. doi: 10.1093/sleep/20.5.340. [DOI] [PubMed] [Google Scholar]


