Abstract
Purpose of the Study:
To determine the overall effectiveness of interventions designed to increase physical activity (PA) behavior among community-dwelling older adults.
Design and Methods:
Comprehensive literature searching identified eligible PA intervention studies among community-dwelling adults aged 65 and older, or sample mean age of 70. Diverse study characteristics were extracted and outcome data were duplicate coded. Overall mean effect sizes (ESs) were synthesized using a random-effects model. Heterogeneity of effects was analyzed using Q and I 2 statistics. Moderator analyses were conducted using meta-analytic analogues of ANOVA and regression for dichotomous and continuous moderators, respectively.
Results:
ESs were calculated from 13,829 primary study subjects. The overall mean ES for two-group posttest comparisons was 0.18 (95% CI 0.10–0.26, p < .001). This represents a difference of 620 steps/day or 73min of PA/week between treatment and control groups. Significant moderators included the use of theory, how interventions were delivered, and cognitive plus behavioral-type intervention components. Non-significant moderators include the type of interventionist, delivery setting, and various measures of intervention dose.
Implications:
PA interventions significantly improved PA behavior among community-dwelling older adults. Effective PA interventions may be efficiently delivered using already available resources and personnel. Future PA intervention research should be theoretically based, incorporate more diverse subjects, and compare intervention delivery methods.
Key words: Exercise, Systematic review, Quantitative synthesis
Chronic illnesses account for 84% of all health care spending and are highly prevalent among the growing older adult population (Anderson, 2010; Centers for Medicare and Medicaid Services [CMS], 2012). Ninety percent of Americans aged 65 and older report at least one chronic illness, and 73% report two or more (Anderson, 2010; CMS, 2012). Chronically ill older adults have high rates of disability, hospitalization, and polypharmacy (Administration on Aging, 2012; Anderson, 2010). Therefore, management of chronic illness among older adults is a major public health concern. Pharmacological and medical management provide relief from some aspects of chronic disease processes; however, self-management is an important and economical component of care for the chronically ill older adult.
Physical activity (PA) is a major aspect of chronic disease self-management. PA encompasses any bodily movement that increases energy expenditure above a basal level, including structured exercise and leisure-time activities (Centers for Disease Control and Prevention, 2011). Engaging in PA is associated with numerous beneficial health outcomes related to chronic disease (Chodzko-Zajko et al., 2009). PA positively modifies cardiovascular risk factors such as hypertension, low HDL, and insulin sensitivity (Chodzko-Zajko et al., 2009; Taylor et al., 2004). Additional benefits include improving pain and physical function among arthritis patients (Conn, Hafdahl, Minor, & Nielsen, 2008; Hughes et al., 2004; Hughes et al, 2006), and decreasing depressive symptoms (Chao 2014). A recent comparative metaepidemiological study suggests exercise interventions have an important impact on mortality outcomes related to coronary artery disease, stroke, and diabetes (Naci & Ionnidis, 2013). Exercise was more effective in reducing mortality in stroke patients than some medications; furthermore, exercise interventions conferred similar mortality benefits compared to drug interventions among patients with coronary artery disease, stroke, and heart failure (Naci & Ionnidis, 2013). Thus exercise is a critically important intervention in the management of these chronic conditions. Yet only about 11% of older adults meet the current national recommendations for leisure-time aerobic and muscle strengthening activities, creating a ripe environment for PA intervention research (Federal Interagency Forum on Aging- Related Statistics, 2012).
Consequently, the number of primary PA intervention studies among older adults is rapidly accumulating. Narrative reviews of the existing literature in this area have reported considerable variability across studies’ sample characteristics, methodologies, intervention characteristics, and PA intervention effectiveness (Conn, Minor, Burks, Rantz, & Pomeroy, 2003; Cyarto, Moorhead, & Brown, 2004; Taylor et al., 2004; van der Bij, Laurant, & Wensing, 2002). A review of randomized controlled trials reported at least seven different kinds of interventions across 42 studies, including behavioral-type components and cognitive-type components (Conn et al., 2003). Behavioral-type components, such as self-monitoring, goal setting, and prompting, engage participants to actively change physical behaviors. Cognitive-type components, such as education, problem solving or counseling, promote change in cognitive processes, attitudes, or beliefs. No reviews have addressed the possible effects of these differences on PA intervention outcomes.
Meta-analyses quantitatively synthesize data across studies to calculate an overall effect size (ES) of PA interventions among older adults. Moderator analyses identify intervention characteristics linked to best outcomes. A landmark meta-analysis by Dishman and Buckworth (1996) demonstrated PA interventions had a medium effect in changing PA behavior in adults (r = 0.34). The study found larger ESs among PA interventions utilizing a behavioral focus or lasting a brief duration (Dishman & Buckworth, 1996). Recently, Conn, Hafdahl, and Mehr (2011) found a small overall mean ES (d = 0.19) of interventions to increase PA among healthy adults. Similar to Dishman and Buckworth (1996), findings revealed larger ESs among studies using behavioral-based interventions. Larger ESs were also found among studies using face-to-face delivery, and targeting individuals rather than communities (Conn, et al., 2011). Studies in these prior meta-analyses included few older adults, however. Among aging adults, Conn, Valentine, and Cooper (2002) found PA interventions to be modestly effective (d = .26) (Conn, et al., 2002). Moderator analyses demonstrated larger ESs for interventions involving self-monitoring, center-based intervention delivery, or focusing solely on PA behavior. Studies in this meta-analysis contained samples with a mean age of 65; therefore, many middle-aged subjects were included (Conn, et al., 2002). Moreover, the most recent paper included in this meta-analysis was published in 1999. Over a decade’s worth of research has yet to be synthesized.
There are no comprehensive meta-analyses addressing PA intervention effectiveness exclusively among adults aged 65 and older. Furthermore, it is not known if variables moderating intervention effectiveness among younger adults are similar to those among this population of older adults. Thus the purpose of this study is to quantitatively summarize the extant research regarding PA intervention effectiveness on measures of PA behavior among older adults.
The following research questions were used to guide this study:
1. What is the overall effect size of interventions designed to increase PA on PA behavior outcomes among adults aged 65 and older?
2. Does effectiveness of PA interventions vary based on study, sample, and intervention characteristics?
Design and Methods
Study procedures followed standard meta-analysis methods and complied with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Cooper, 2009; Moher, Liberati, Teztlaff, & Altman, 2009).
Sampling
Eligible primary studies (a) were published from 1960–2013; (b) tested PA interventions; (c) among community-dwelling older adults; (d) age 65 and older, or with a sample mean age of 70; (e) contained at least five participants; (f) reported enough data to calculate an ES; (g) and were written in English. The year 1960 was selected as a cut-off because few PA intervention studies exist prior to 1960. A comprehensive search of the existing literature from 1960–2013 was necessary to capture the breadth and depth of PA intervention research among older adults. PA interventions were conceptually defined as interventions deliberately designed to increase PA behavior. PA intervention studies involving cardiac or pulmonary rehabilitation were excluded due to their rehabilitative and therapeutic focus. Older adults were defined as aged 65 and older based on Medicare eligibility criteria. Because the goal of the literature search was to capture the cumulative body of PA intervention research, smaller studies were included. Prior meta-analysis work had set a minimum number of five participants; therefore, this project also adopted this criterium (Conn et al., 2002).
Studies utilizing both subjective (e.g., questionnaires, activity logs) and objective measures (e.g., accelerometer) of PA behavior outcomes were included. Prior research suggests that reliability and validity differences exist between various objective and subjective PA measures (Banda et al., 2010; Tucker, Welk, & Beyler, 2011; Van Poppel, Chinapaw, Mokkink, Van Mechelen, & Terwee, 2010); however, the author sought to capture information regarding all potentially eligible PA intervention studies available. Furthermore, the capabilities of collecting any PA behavior data are impacted by the population of interest (Chase, 2013; De Bruin, Hartmann, Uebelhart, Murer, & Zijlstra, 2008; Tudor-Locke, Williams, Reis, & Pluto, 2002). For example, collecting data via an interview questionnaire may be more feasible in an older population than accurately fitting participants with complex and bulky accelerometers.
The goal of the literature search associated with meta-analyses is to encompass the accumulated body of relevant research (Cooper, 2009). Cooper (2009) suggests searching direct-to-researcher channels (e.g., personal contact), quality controlled channels (e.g., peer-review journal articles), and secondary channels (e.g., bibliographies) to adequately conduct a comprehensive search. This exhaustive search should not only capture the expanse of accumulated relevant research, but also identify difficult-to-retrieve literature, such as unpublished works. If a cursory search of only a few online databases is the basis of a meta-analysis, findings may be positively skewed and not representative of the overall body of research work in an area. Comprehensive searching strengthens the validity of meta-analyses findings and reduces bias (Cooper, 2009).
A health sciences reference librarian with experience conducting searches for meta-analyses was consulted for this project. Online databases searched include: PubMed, Medline, CINAHL, SPORTDiscus, PsychInfo, Google Scholar, and Dissertation Abstracts International. Example of physical activity-related Medline search terms were: “exercise,” “physical activity,” “physical exertion,” “physical endurance,” “leisure activities,” “recreation,” “physical fitness,” “physical education and training.” The following journals were hand searched for potentially eligible studies: The Gerontologist, Journal of the American Geriatrics Society, Medicine and Science in Sport and Exercise, Journal of Aging and Physical Activity, Annals of Behavioral Medicine, Geriatric Nursing, Research in Gerontological Nursing. Years hand-searched ranged from 1960–2013, but varied for individual journals based on library availability. Additionally, eligible studies’ and relevant reviews’ bibliographies were examined. Author searches were conducted among researchers prolific in gerontological PA intervention research. Furthermore, researchers in the field were approached regarding possibly eligible current or past projects. To further identify possibly eligible unpublished reports, gerontology and interdisciplinary conference abstracts (e.g., Gerontological Society of America, Society of Behavioral Medicine) were reviewed.
Data Extraction
Data were extracted from eligible studies using a codebook developed from prior research (Abraham & Michie, 2008; Brown, Upchurch, & Acton, 2003; Conn et al., 2011; Conn et al., 2002; Michie, Johnston, Francis, Hardeman, & Eccles, 2008). Pilot testing the codebook can identify problem items and insufficient capture of study characteristics (Wilson, 2009). Thus the codebook was pilot tested on a random selection of 20 eligible studies to ensure adequate capture of relevant variables related to study design, sample, and intervention characteristics and outcome data. Coding items reported in this paper are available from the corresponding author. Considerable detail was coded about sample characteristics and intervention characteristics. Data necessary to calculate ESs were collected. Studies with alternative outcome data were included if the outcome statistics could be converted to a standardized mean difference ES (e.g. t statistic, exact p value for t statistic). Corresponding authors were contacted for any missing data. A second, doctorally-prepared researcher independently coded all outcome data. Discrepancies in coding were discussed until a consensus was achieved. A third doctorally-prepared researcher facilitated resolution of any discrepancies.
Data Analysis
Statistical analyses were performed using Comprehensive Meta-Analysis Software (Borenstein, Hedges, Higgins, & Rothstein, 2005). Standardized mean difference ESs (d) were calculated for all eligible studies. The overall mean ES is conceptually defined as the mean of the treatment group minus the mean the control group divided by a pooled standard deviation. ESs were weighted by the inverse of the variance to adjust for bias. ESs were synthesized using a random-effects model, accounting for between-study and within-study variances (Borenstein, Hedges, Higgins, & Rothstein, 2010). ESs were interpreted as small (≤0.20), medium (=0.50), or large (≥0.80) (Cohen, 1988). Statistical significance was set to alpha ≤0.05.
ESs for two-group and single-group pre-posttest studies were calculated separately. Two-group posttest comparisons provided data for the main analysis. Some reports included pre-posttest data for two-group comparisons; however, none provided correlational data necessary to link pre-posttest scores. A moderate correlation was assumed in these cases. Single group data were analyzed to supplement the more valid two-group findings. To facilitate interpretation of ES findings, the overall mean ES was converted to difference in steps per day and minutes per week of PA between treatment and control (Lipsey & Wilson, 2000). To convert the ES to steps per day, a pooled mean and standard deviation weighted by sample size were calculated for control groups in studies using this outcome measure. The difference in steps per day between treatment and control is the product of the pooled standard deviation and the overall mean ES for this meta-analysis. This value may be added to the pooled mean to determine the treatment group mean. The same calculations were completed to determine the difference in minutes per week of PA.
Homogeneity of variance across ESs was assessed using Q and I 2 statistics. The Q statistic describes the presence or absence of statistically significant heterogeneity across studies. I 2 reflects the proportion of variance due to true differences of effects across included studies. Moderator analyses were used to determine sample, study, and intervention characteristics linked with better PA outcomes. Meta-analytic analogs of ANOVA were used for dichotomous variables. Table 1 lists definitions for dichotomous variable included in the subgroup analyses. Continuous potential moderators were analyzed with meta-analytic analogues of regression. Moderator analyses were conducted on 2-group treatment versus control comparisons only, since this research design is more rigorous than single group designs.
Table 1.
Definitions of Selected Variables for Moderator Analysis
| Variable | Definition |
|---|---|
| Barriers management | The intervention encourages participants to develop ways to overcome specific barriers that prevent them from engaging in PA. The report must specifically say “barriers management.” |
| Behavioral target | Whether intervention targeted only PA behavior or PA behavior and another health behavior (e.g., diet, medication adherence). |
| Behavioral-type intervention components | Interventions that engage participants to actively change physical behaviors |
| Cognitive-type intervention components | Interventions that facilitate a change in cognitive processes, attitudes, or beliefs |
| Counseling | The intervention must involve face-to-face or mediated (e.g., telephone) verbal interaction between the interventionist/provider and participant. |
| Disease education | Education may include topics such as disease education, symptom management, PA benefits related to chronic diseases, interaction of PA and disease, self-management strategies; safety and PA. The primary focus of the education is centered around disease management and disease education. |
| Feedback | Participants are given visual or verbal feedback based on (a) a comparison to a group of similar individuals, (b) past performance data and, (c) nationally recommended amounts of PA. |
| Goal setting by the interventionist | PA behavior goals are set by the provider/interventionist/research staff or through pre-determined study protocols. |
| Goal setting by the participant | The participant/patient sets the PA behavior goals that he/she wants to achieve. |
| Health education | Education may include topics related to staying healthy and maintaining function, PA benefits related to health promotion and illness prevention. The primary focus of the education is to stay healthy and free from chronic illnesses. |
| Motivational-type intervention | Interventions that promoted independent PA behavior change, without observed and verified exercise dose by the interventionist/researcher. |
| Problem solving | The participant/patient is prompted by the provider or interventionist to identify general problems and strategies to address these issues to PA behavior. |
| Prompting | Prompting may include telephone calls, text messages, emails, calendars, reminder cues in the environment. The intervention must state that these are used to “prompt” participants. |
| Referral to community resources | Examples of community resources would include: Community centers, senior centers, gyms that may serve as places where the participant may engage in PA behavior. This item does not require referral to a specific exercise program. |
| Role modeling | This item entails involvement of an individual similar to the participant. This individual may model PA behavior for the participant. The intent of this intervention may be to motivate or increase the confidence of the subjects to perform PA behaviors. |
| Self-efficacy enhancement | The intervention intent is stated to “enhance,” “improve,” or “increase” self-efficacy. The study must state “self-efficacy” as either an intervention target or a theoretical construct. There may be a measure for exercise self-efficacy at outcome. |
| Self-monitoring | Participants are asked to keep track of their PA behavior. This may occur through different tools that are provided for the entire length of the intervention such as a pedometer, activity log/diary, calendar. |
| Supervised exercise intervention | Interventions that required observed and verified exercise dose by the interventionist/researcher. |
Note: PA = physical activity.
Results
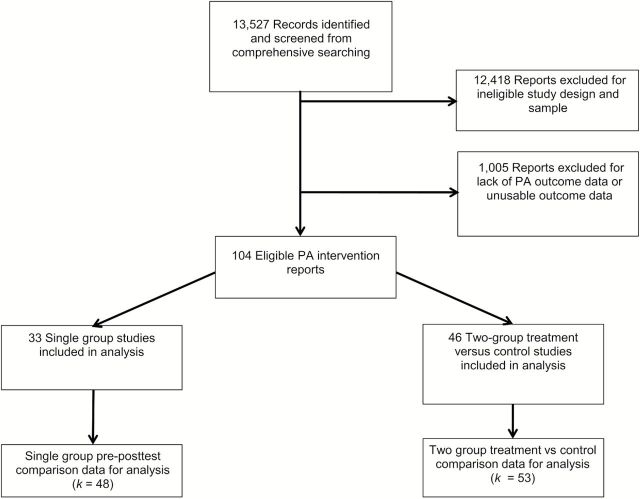
Figure 1 is a flow diagram of study selection. Comprehensive searching yielded 13,527 citations for review. A total of 104 reports were coded, describing 53 two-group, posttest comparisons and 48 single group, pre-posttest comparisons. The table of included studies has been provided in the Supplementary Appendix. ESs were calculated from a total of 13,829 subjects—10,186 subjects from two-group posttest studies and 3,643 subjects from single group pre-posttest studies.
Figure 1.
Flow diagram of report selection. 104 eligible PA reports described 46 two-group treatments versus control intervention studies and 33 single group pre-posttest intervention studies. A total of 53 two group comparisons and 48 single group comparisons were derived from reports. “Comparisons” refers to the group analyzed within a report. Some reports may have more than one comparison (e.g., multiple treatment groups). PA = physical activity; k = number of comparisons within reports for which data were available.
Study Characteristics
Table 2 lists characteristics of the included studies. Median sample size of included studies was relatively small at 39. Women were well represented in samples, whereas minorities were not. Participants tended to be overweight with a median mean body mass index (BMI) of 27kg/m2. Interventions had a median of 15 sessions, with each session lasting a median of 60min.
Table 2.
Characteristics of Reports Included in Meta-Analysis (N = 13,829 subjects)
| Characteristic | k | Minimum | Median | Maximum |
|---|---|---|---|---|
| Mean age | 101 | 68.5 | 75.35 | 88 |
| Sample size | 101 | 6 | 39 | 989 |
| Percentage women | 83 | 0 | 70 | 100 |
| Percentage minority | 53 | 0 | 15 | 100 |
| Mean BMI (kg/m2) | 45 | 21.9 | 27.7 | 40.44 |
| Mean weight | 17 | 39.89 | 65.7 | 76.9 |
| Total number of intervention sessions | 88 | 1 | 15 | 274.5 |
| Session duration (min) | 48 | 8 | 60 | 120 |
| Days over which intervention was delivered | 96 | 1 | 91.5 | 1,460 |
| Total duration of intervention (min) | 45 | 45 | 970 | 6,252 |
Note: k = number of comparisons for which data were available. “Comparison” is defined as the group analyzed within a report. Some reports may have more than one comparison (e.g., multiple treatment groups).
Physical Activity Intervention Effects
PA interventions had a significant impact on PA behaviors among community-dwelling older adults (Table 3). The overall mean ES for two-group posttest comparisons was 0.18 (p < .001). Figure 2 shows the forest plot of this main analysis. This ES is equivalent to a difference of 620 more steps per day or 73 more minutes of PA per week for the treatment group over the control group. Studies designed as two-group posttest comparisons were significantly heterogeneous (Q = 122.92, p < .001), with 57.70% of heterogeneity due to true differences in effects across studies. Figure 3 demonstrates little evidence of publication bias for this analysis.
Table 3.
Overall Effect Size of Physical Activity Interventions on Physical Activity Behavior Among Older Adults
| k | d | 95% CI LL,UL | SE | Q | I 2 | |
|---|---|---|---|---|---|---|
| Two-group, treatment versus control comparison, post-intervention | 53 | 0.18* | .10, .26 | 0.04 | 122.92* | 57.70 |
| Treatment group, within-group, pre-post intervention | 45 | 0.17* | .09, .26 | 0.04 | 102.60* | 57.11 |
| Single group, pre-post intervention | 48 | 0.23* | .15, .31 | 0.04 | 198.30* | 76.30 |
| Control group, within-group, pre-post intervention | 45 | 0.01 | −.08, .10 | 0.05 | 173.25* | 74.60 |
Note: k = number of comparisons; d = standardized mean difference calculated under random-effects model; CI = confidence interval; SE = standard error of d; Q = heterogeneity statistic; LL = lower limit; UL = upper limit;
* p < .001
Figure 2.
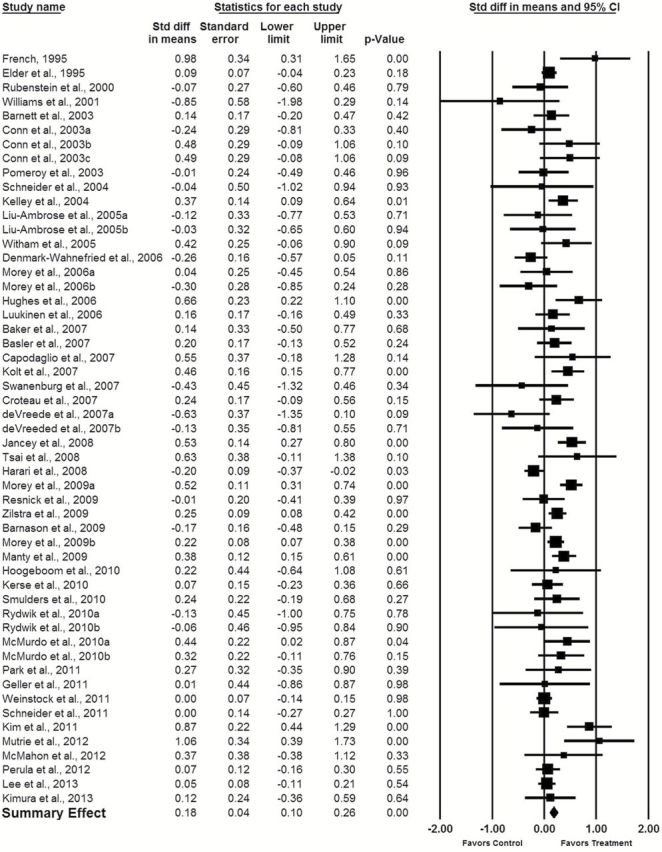
Forest plot of 2-group, posttest physical activity outcomes. Studies are listed by year of publication. Effect sizes were calculated under a random-effects model. Square areas are proportional to study weight.
Figure 3.
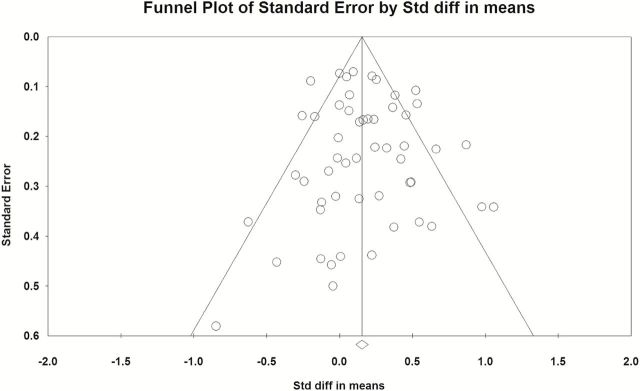
Funnel plot of 2-group posttest analysis. Publication bias is absent when studies (data points) are symmetrically distributed about the mean effect size (center line). Larger studies cluster at the top of the funnel, whereas positive studies cluster to the right of the center line. This funnel plot demonstrates little evidence of publication bias.
Forty-five two-group comparisons included pre-posttest data. The overall mean ES for these studies was 0.17 (p < .001). The overall mean ES for studies designed as single group pre-posttest comparisons was 0.23 (p < .001). The overall mean ES for control group pre-posttest comparisons was 0.01 (p = .78).
Moderator Analyses
Table 4 lists results from the moderator analyses of dichotomous variables. PA interventions tested among healthier subjects (d = 0.30) were more effective in improving PA behavior than chronically ill subjects (d = 0.11) (p = .03). Characteristics of intervention delivery impacted PA intervention effectiveness. For example, interventions delivered through audio-visual media (d = 0.48) were more effective than those that did not use this delivery method (d = 0.14) (p = .01). Delivering the intervention via mailed materials (d = 0.34) was also more effective in changing PA behavior than those interventions without this delivery mechanism (d = 0.14) (p = .03).
Table 4.
Moderator Analyses of Dichotomous Variables on Physical Activity Behavior
| Variable | k 0 a | k 1 b | d k0 a | dk1 b | Q B |
|---|---|---|---|---|---|
| Study Characteristics | |||||
| Use of true control group | 43 | 10 | 0.18 | 0.16 | 0.06 |
| European study | 34 | 19 | 0.17 | 0.19 | 0.08 |
| North American study | 27 | 26 | 0.20 | 0.15 | 0.46 |
| Objective measurement of physical activity behavior (e.g., pedometer, accelerometer data) | 42 | 11 | 0.15 | 0.28 | 1.51 |
| Sample Characteristics | |||||
| History of chronic illness | 16 | 35 | 0.30 | 0.11 | 4.98* |
| Intervention Delivery | |||||
| Exercise specialist interventionist | 33 | 20 | 0.20 | 0.14 | 0.42 |
| Use of audio-visual media | 48 | 5 | 0.14 | 0.48 | 6.78* |
| Use of written materials | 23 | 30 | 0.08 | 0.23 | 3.00 |
| Use of mailed materials | 43 | 10 | 0.14 | 0.34 | 4.66* |
| Use of discussion | 21 | 32 | 0.11 | 0.21 | 1.54 |
| Use of lecture | 32 | 21 | 0.22 | 0.11 | 1.65 |
| Phone-mediated | 34 | 19 | 0.15 | 0.21 | 0.49 |
| Face to face interaction | 9 | 44 | 0.16 | 0.18 | 0.03 |
| Delivered in more than one setting | 37 | 16 | 0.13 | 0.29 | 3.57 |
| Delivered at participant’s house | 28 | 25 | 0.16 | 0.20 | 0.25 |
| Delivered in a community setting | 38 | 15 | 0.18 | 0.17 | 0.02 |
| Delivered in a clinic setting | 45 | 8 | 0.20 | 0.09 | 1.02 |
| Group setting | 19 | 34 | 0.16 | 0.19 | 0.10 |
| Intervention Characteristics and Components | |||||
| Cognitive-type intervention components only | 48 | 5 | 0.18 | 0.03 | 1.11 |
| Behavioral-type intervention components only | 41 | 12 | 0.20 | 0.09 | 0.99 |
| Combination cognitive- and behavioral-type intervention | 17 | 36 | 0.02 | 0.23 | 4.70* |
| Motivational-type intervention | 7 | 46 | -0.15 | 0.20 | 5.4* |
| Supervised exercise intervention | 26 | 27 | 0.19 | 0.16 | 0.12 |
| Use of theory | 25 | 28 | 0.05 | 0.28 | 9.79* |
| Behavioral target | 33 | 20 | 0.16 | 0.22 | 0.51 |
| Feedback | 34 | 19 | 0.14 | 0.23 | 1.29 |
| Goal setting by the interventionist | 45 | 8 | 0.16 | 0.25 | 0.74 |
| Goal setting by the participant | 35 | 18 | 0.12 | 0.27 | 3.34 |
| Patient education | 43 | 10 | 0.15 | 0.29 | 1.76 |
| Health education | 38 | 15 | 0.17 | 0.20 | 0.09 |
| Self-efficacy enhancement | 36 | 17 | 0.13 | 0.24 | 2.16 |
| Role modeling | 47 | 6 | 0.17 | 0.25 | 0.40 |
| Prompting | 43 | 10 | 0.19 | 0.16 | 0.08 |
| Counseling | 28 | 25 | 0.14 | 0.20 | 0.55 |
| Barriers management | 33 | 20 | 0.08 | 0.30 | 9.52* |
| Problem solving | 31 | 22 | 0.08 | 0.30 | 8.56* |
| Self-monitoring | 23 | 30 | 0.10 | 0.24 | 3.20 |
| Referral to community resources | 46 | 7 | 0.19 | 0.12 | 0.46 |
Note: k = number of studies; d = standardized mean difference calculated under random-effects model; Q B = Q between.
a Refers to studies missing the variable of interest.
b Refers to studies containing the variable of interest.
* p < .05.
Studies reporting theory-based interventions (d = 0.28) had larger effects than interventions without a stated theoretical basis (d = 0.05) (p < .01). Interventions employing combination cognitive and behavioral strategies were more effective (d = 0.23) than interventions using either strategy type alone (d = 0.02) (p = .03). Studies using motivational-type interventions were more effective (d = 0.20) than studies without motivational-type interventions (d = −0.15) (p = .02). Regarding specific intervention components, problem solving techniques and barriers management, appeared more effective in changing PA behavior (Table 4). Non-significant dichotomous moderators included the type of interventionist, aspects of the delivery setting, and the use of objective measures of PA.
Table 5 lists results from the moderator analyses of continuous variables. Although the total duration of intervention delivery in minutes was statistically significant, the result is not substantively significant (B = −0.00, p = .01). PA interventions were similarly effective regardless of the year the study was conducted, subjects’ baseline BMI, or the percentage of females within the samples. PA interventions were also equally effective regardless of the number of intervention sessions delivered, the duration of each session, and the number of days over which the interventions were delivered.
Table 5.
Moderator Analyses of Continuous Variables on Physical Activity Behavior
| Variable | B | SE | p |
|---|---|---|---|
| Year of study | 0.002 | 0.01 | .82 |
| Mean age | −0.005 | 0.01 | .65 |
| Mean BMI (kg/m2) | 0.008 | 0.03 | .79 |
| Percent sample women | −0.001 | 0.00 | .62 |
| Days over which intervention delivered | 0.000 | 0.00 | .66 |
| Number of minutes per intervention session | 0.000 | 0.00 | .70 |
| Number of sessions | 0.000 | 0.00 | .58 |
| Total duration of intervention (min) | 0.000 | 0.00 | .01 |
Note: B = unstandardized meta-regression coefficient for slope; SE = standard error of B; p refers to statistical significance for B; BMI = body mass index
Discussion
Findings from this comprehensive meta-analysis suggest interventions designed to increase PA behavior among adults 65 and older are effective. Similar findings were demonstrated in prior meta-analyses studying younger populations (Dishman & Buckworth, 1996) and healthy adults (Conn et al., 2011). Although the ES is small, it represents a clinically important change in PA behavior among older adults who may be sedentary overall. Indeed, the average baseline steps/day for participants in the included studies was 4,768, which is categorized as a sedentary lifestyle (Tudor-Locke & Bassett, 2004).
These findings are similar to Conn and colleagues’ (2002) work with aging adults, although this meta-analysis differs because this study employed more comprehensive search strategies, and eligible studies contained older participants. The overall mean ES for the previous study was higher (d = 0.26) than the present study. This finding may be related to decreased PA intervention effectiveness with increased age (Dishman & Buckworth, 1996). Furthermore, the previous study demonstrated larger ESs among interventions that targeted only PA, employed self-monitoring, or were delivered in groups. These findings are contrary to the present study, suggesting that effective PA intervention strategies for young-older adults may differ from those for old-older adults. Future gerontological PA intervention research should explore these differences across the aging spectrum to tailor interventions accordingly.
Moderator analyses produced several interesting findings that advance current PA intervention research knowledge. PA interventions tested among healthier subjects had larger effects than those tested among chronically ill populations. Healthier subjects, who may experience fewer physical limitations, may be more likely to engage in PA than ill subjects. Interventions utilizing combination cognitive plus behavioral-type strategies appeared especially effective in changing PA behavior among older adults. Prior PA intervention meta-analysis findings among younger, healthy, and chronically ill samples suggested that behavioral strategies alone were more effective (Conn et al., 2011; Conn, Hafdahl, Brown, & Brown, 2008; Dishman & Buckworth, 1996). A recent narrative systematic review, however, supports combination strategies as more successful in changing PA behavior (Chase, 2013). These findings suggest older individuals may need interventions focusing not only on cognitive processes (e.g., education, counseling), but also on behavioral activities (e.g., self monitoring, goal setting) to improve PA behavior change. Future research could compare interventions employing combination cognitive plus behavioral strategies to either behavioral or cognitive strategies alone to further explore intervention effectiveness among older adults. Additionally, future research might compare varied combinations of cognitive plus behavioral interventions to determine which are most effective in older people.
Theory-based interventions were more effective than those interventions without a reported theoretical basis. The most common theories reported were the Transtheoretical Model and Social Cognitive Theory. These findings should be interpreted with caution, however. How theory is operationalized is often inadequately reported within studies, causing difficulty in connecting actual theoretical concepts with intervention components and outcome measures (Keller, Fleury, Sidani, & Ainsworth, 2009; Lippke & Ziegelmann, 2008). Future theory-driven PA intervention research should clearly explicate how theoretical concepts align with intervention components and study design, and link measured theoretical constructs with measured behavioral outcomes.
Interventions delivered via audio-visual or mailed materials were more effective in increasing PA behavior than interventions not using these delivery methods. The types of audio-visual materials used in primary studies included discs of music or exercise instruction, and exercise videos. Examples of mailed materials included informational newsletters with pictorial and descriptive examples of exercises and calendars to keep track of PA behavior. Methods of delivery that involve more than verbal information exchange may increase intervention effectiveness among older adults (Chase, 2013). For example, mailed materials provide older adults with physical resources to which they may refer repeatedly, as opposed to a one-time, face-to-face conversation. In contrast, Conn and colleagues (2002) found that these types of mediated intervention delivery did not impact PA intervention effectiveness among aging adults. Future research might compare PA interventions delivered via audio-visual or mailed mechanisms with those delivered face-to face.
This study also revealed notable non-significant moderators. For example, PA interventions were similarly effective regardless of the type of interventionist. Community lay people and diverse health care providers with consistent access to older adults are capable of delivering interventions that can impact their PA behavior. Moreover, PA interventions were equally effective regardless of delivery setting. Therefore, PA interventions may be delivered in a variety of settings, such as at home, in the community, or in the clinic, and still be successful. These findings suggest that simple and effective PA interventions may be delivered using already available resources and personnel.
Aspects of intervention dose (e.g., number of sessions, duration of sessions) were not significant moderators. These findings may be confounded by possible interactions between types of intervention strategies and aspects of intervention dose. For example, an intervention may involve multiple, hour-long counseling sessions, whereas another may involve simply providing participants with a pedometer to monitor PA behavior.
Interventions were equally effective regardless of the year the study was conducted. Few studies included in this meta-analysis were conducted prior to 2000. This may be due to the higher age inclusion criteria. As research emerged demonstrating the safety and benefits of PA among older adults, newer studies incorporating older-old participants were conducted. More recent studies did use novel interventions, such as internet- or web-based strategies (McMahon, 2012; Moy, Weston, Wilson, Hess, & Richardson, 2012; Tsai, 2008; Weinstock et al., 2011) or telehealth (Barnason, Zimmerman, Schulz, & Tu, 2009); however, there were too few eligible comparisons to conduct moderator analyses exploring their impact on intervention effectiveness. Additional research employing technology is needed to determine the efficacy of these innovative strategies among older adults.
The use of objective PA measures did not appear to be a significant moderator either. Past research suggests that objective measures of PA behavior, such as accelerometer and pedometer data, more accurately capture the quantity of PA behavior (Harris et al., 2009). Among older adults, however, these types of PA measures may be less accurate due to issues with placement and compliance (Chase, 2013; De Bruin et al., 2008; Garatachea, Torres Luque, & González Gallego, 2010). Furthermore, the type of PA behavior in which older adults engage can impact accuracy of objective data (De Bruin et al., 2008; Garatachea et al., 2010; Tudor-Locke et al., 2002). Older adults may engage in lower intensity, more stationary activities, such as gardening, household chores, yoga, and tai chi, which cannot be adequately captured by current accelerometer or pedometer technology. Subjective measures, such as questionnaires and activity logs, inquire about specific activities and time spent in these activities; thus these measures may be more attractive methods of data collection among gerontological researchers. However, overreporting of PA behavior has been documented with subjective measures (Tucker et al., 2011). Findings from this study suggest operationalization of PA behavior, either through objective or subjective means, does not affect intervention effectiveness. Thus the decision of which type of PA measure to use should take into consideration the specific characteristic of older adult PA behavior (e.g., overall quantity, type of activity, time spent in different activities) the researcher is trying to capture.
There are some limitations to this study. Although comprehensive search strategies were used to locate all available PA intervention reports, it is virtually impossible to obtain every potentially eligible study (Cooper, 2009). Additionally, meta-analyses are limited by primary study reporting. Although attempts were made to contact corresponding authors of potentially eligible primary studies with missing data, not all essential data were recovered. Thus studies that may have contributed to the main and moderator analyses were excluded due to missing data. Finally, primary study quality can impact interpretation of the results of meta-analyses. Recommendations for managing primary study quality in meta-analysis work are diverse (Conn & Rantz, 2003; Valentine, 2009). Study quality was addressed using multiple methods such as inclusion criteria (e.g., smaller studies excluded), data analysis methods (e.g., single group studies analyzed separate from two-group studies), examining aspects of study quality as potential moderators (e.g., type of control group, operationalization of PA behavior), and interpretation of findings (e.g., two-group posttest comparisons as main analysis).
Additional limitations to this study are related to general methods and scope. Meta-analyses are observational studies. Moderator analyses findings are intended to encourage future research. The samples from included primary studies demonstrated limited heterogeneity to explore in moderator analysis. Ethnic and racial diversity, which were poorly reported across studies, was low, unfortunately limiting the ability to generalize to these populations. Future PA intervention research should strive to include more diverse, older adult samples. Adapting recruitment strategies, and tailoring inclusion criteria and sampling decisions can facilitate incorporation and retention of more diverse older participants (Sullivan-Marx et al., 2011; Warren-Findlow, Prohaska, & Freedman, 2003). Additionally, the aim of this study was to examine PA intervention effects among community-dwelling older adults. Thus generalization of study findings is limited among older adults who live in more dependent settings such as nursing homes or assisted living environments.
This study has important strengths and adds to the body of research knowledge related to PA intervention effectiveness among adults aged 65 and older. Comprehensive and diverse search strategies increase the validity of this study’s findings. Meticulous and rigorous coding methods allowed for exploratory moderator analyses. These moderator analyses uncovered valuable information regarding characteristics of intervention effectiveness, suggesting areas for future research, and providing evidence for implementation in clinical practice.
The burden of chronic disease in the growing older adult population is evident. Self-management interventions, especially PA behavior change interventions, have come to the research limelight as effective and economical means of improving health outcomes and preventing disability. Improving PA behavior among older adults significantly impacts health outcomes related to chronic disease. Researchers need a comprehensive understanding of PA intervention effectiveness to advance this area of science and test future, evidence-supported interventions. Furthermore, clinicians need information related to the most effective types of PA interventions to promote healthy aging. This study has provided a comprehensive quantitative synthesis of the PA intervention literature to address these issues.
Supplementary Material
Supplementary material can be found at: http://gerontologist.oxfordjournals.org.
Funding
This work was supported by the National Institutes of Health/National Institute of Nursing Research (grant number F31NR013586) and the John A. Hartford Foundation’s National Hartford Centers of Gerontological Nursing Excellence Award Program (Patricia G. Archbold Scholarship). The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Supplementary Material
Acknowledgments
The author would like to acknowledge Drs. Vicki Conn, Lorraine Phillips, and Todd Ruppar from the Sinclair School of Nursing, University of Missouri, and Dr. Marybeth Brown from the Department of Physical Therapy, University of Missouri. As members of my doctoral committee, these individuals provided essential feedback and support during the development of this manuscript.
References
- Abraham C., Michie S. (2008). A taxonomy of behavior change techniques used in interventions. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 27, 379–387. 10.1037/0278-6133.27.3.379 [DOI] [PubMed] [Google Scholar]
- Administration on Aging. (2012. ). A profile of older Americans: 2012. Administration of Aging. Washington, DC: U.S. Department of Health and Human Services; Retrieved July 8, 2014, from http://www.aoa.gov/AoAroot/Aging_Statistics/Profile/index.aspx [Google Scholar]
- Anderson G. (2010). Chartbook, chronic conditions: Making the case for ongoing care. Baltimore, MD: Johns Hopkins University; Retrieved July 8, 2014, from http://www.rwjf.org/files/research/50968chronic.care.chartbook.pdf [Google Scholar]
- Banda J. A., Hutto B., Feeney A., Pfeiffer K. A., McIver K., Lamonte M. J., Hooker S. P. (2010). Comparing physical activity measures in a diverse group of midlife and older adults. Medicine and Science in Sports and Exercise, 42, 2251–2257. 10.1249/MSS.0b013e3181e32e9a [DOI] [PubMed] [Google Scholar]
- Barnason S., Zimmerman L., Schulz P., Tu C. (2009). Influence of an early recovery telehealth intervention on physical activity and functioning after coronary artery bypass surgery among older adults with high disease burden. Heart & Lung, 38, 459–68. http://dx.doi.org/10.1016/j.hrtlng.2009.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M., Hedges L. V., Higgins J. P. T., Rothstein H. R. (2005). Comprehensive Meta-Analysis (Version 2). Englewood, NJ: Biostat. [Google Scholar]
- Borenstein M., Hedges L. V., Higgins J. P. T., Rothstein H. R. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods, 1, 97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- Brown S. A., Upchurch S. L., Acton G. J. (2003). A framework for developing a coding scheme for meta-analysis. Western Journal of Nursing Research, 25, 205–222. 10.1177/0193945902250038 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2011). Physical activity and health: Report of the Surgeon General. Atlanta, Georgia: U.S. Department of Health and Human Services, CDC. [Google Scholar]
- Centers for Medicare and Medicaid Services. (2012). Chronic conditions among Medicare beneficiaries, Chartbook, 2012. Baltimore, MD: United States Department of Health and Human Services; Retrieved July 8, 2014, from http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/Downloads/2012Chartbook.pdf [Google Scholar]
- Chase J. D. (2013). Methodological challenges in physical activity research among older adults. Western Journal of Nursing Research, 35, 76–97. 10.1177/0193945911416829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao S.F. (2014). Changes in leisure activities and dimensions of depressive symptoms in later life: A 12-year follow-up. The Gerontologist. Advance online publication. 10.1093/geront/gnu052 [DOI] [PubMed] [Google Scholar]
- Chodzko-Zajko W. J., Proctor D. N., Fiatarone Singh M. A., Minson C. T., Nigg C. R., Salem G. J., Skinner J. S. (2009). American College of Sports Medicine position stand. Exercise and physical activity for older adults. Medicine and Science in Sports and Exercise, 41, 1510–1530. 10.1249/MSS.0b013e3181a0c95c [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Earlbaum Associates. [Google Scholar]
- Conn V. S., Hafdahl A. R., Mehr D. R. (2011). Interventions to increase physical activity among healthy adults: Meta-analysis of outcomes. American Journal of Public Health, 101, 751–758. 10.2105/AJPH.2010.194381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conn V. S., Hafdahl A. R., Minor M. A., Nielsen P. J. (2008). Physical activity interventions among adults with arthritis: Meta-analysis of outcomes. Seminars in Arthritis and Rheumatism, 37, 307–316. 10.1016/j.semarthrit.2007.07.006 [DOI] [PubMed] [Google Scholar]
- Conn V. S., Hafdahl A. R., Brown S. A., Brown L. M. (2008). Meta-analysis of patient education interventions to increase physical activity among chronically ill adults. Patient Education and Counseling, 70, 157–172. 10.1016/j.pec.2007.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conn V. S., Minor M. A., Burks K. J., Rantz M. J., Pomeroy S. H. (2003). Integrative review of physical activity intervention research with aging adults. Journal of the American Geriatrics Society, 51, 1159–1168. 10.1046/j.1532-5415.2003.51365.x [DOI] [PubMed] [Google Scholar]
- Conn V. S., Rantz M. J. (2003). Research methods: Managing primary study quality in meta-analyses. Research in Nursing & Health, 26, 322–333. 10.1002/nur.10092 [DOI] [PubMed] [Google Scholar]
- Conn V. S., Valentine J. C., Cooper H. M. (2002). Interventions to increase physical activity among aging adults: A meta-analysis. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 24, 190–200. 10.2105/AJPH.2010.194381 [DOI] [PubMed] [Google Scholar]
- Cooper H. (2009). Research synthesis and meta-analysis: A step-by-step approach (4th ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Cyarto E. V., Moorhead G. E., Brown W. J. (2004). Updating the evidence relating to physical activity intervention studies in older people. Journal of Science and Medicine in Sport / Sports Medicine Australia, 7(1 Suppl), 30–38. 10.1016/S1440-2440(04)80275-5 [DOI] [PubMed] [Google Scholar]
- De Bruin E. D., Hartmann A., Uebelhart D., Murer K., Zijlstra W. (2008). Wearable systems for monitoring mobility-related activities in older people: A systematic review. Clinical Rehabilitation, 22, 878–895. 10.1177/0269215508090675 [DOI] [PubMed] [Google Scholar]
- Dishman R. K., Buckworth J. (1996). Increasing physical activity: A quantitative synthesis. Medicine and Science in Sports and Exercise, 28, 706–719. [DOI] [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging- Related Statistics. (2012). Older Americans 2010: Key indicators of well-being Retrieved July 8, 2014, from http://www.agingstats.gov/Main_Site/Data/2012_Documents/docs/EntireChartbook.pdf
- Garatachea N., Torres Luque G., González Gallego J. (2010). Physical activity and energy expenditure measurements using accelerometers in older adults. Nutrición Hospitalaria, 25, 224–230. 10.3305/nh.2010.25.2.4439 [PubMed] [Google Scholar]
- Harris T. J., Owen C. G., Victor C. R., Adams R., Ekelund U., Cook D. G. (2009). A comparison of questionnaire, accelerometer, and pedometer: Measures in older people. Medicine and Science in Sports and Exercise, 41, 1392–1402. 10.1249/MSS.0b013e31819b3533 [DOI] [PubMed] [Google Scholar]
- Hughes S. L., Seymour R. B., Campbell R., Pollak N., Huber G., Sharma L. (2004). Impact of the fit and strong intervention on older adults with osteoarthritis. The Gerontologist, 44, 217–228. 10.1093/geront/44.2.217 [DOI] [PubMed] [Google Scholar]
- Hughes S. L., Seymour R. B., Campbell R. T., Huber G., Pollak N., Sharma L., Desai P. (2006). Long-term impact of Fit and Strong! on older adults with osteoarthritis. The Gerontologist, 46, 801–814. 10.1093/geront/46.6.801 [DOI] [PubMed] [Google Scholar]
- Keller C., Fleury J., Sidani S., Ainsworth B. (2009). Fidelity to Theory in PA Intervention Research. Western Journal of Nursing Research, 31, 289–311. 10.1177/0193945908326067 [DOI] [PubMed] [Google Scholar]
- Lippke S., Ziegelmann J. P. (2008). Theory-Based Health Behavior Change: Developing, Testing, and Applying Theories for Evidence-Based Interventions. Applied Psychology, 57, 698–716. 10.1111/j.1464-0597.2008.00339.x [Google Scholar]
- Lipsey M. W., Wilson D. B. (2000). Practical Meta-Analysis. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- McMahon S. (2012). Enhancing motivation for physical activity to reduce fall risk among community dwelling older adults (Ph.D.). Doctoral dissertation, Arizona State University, Phoenix: . Retrieved June 28, 2014, from http://search.proquest.com.proxy.mul.missouri.edu/pqdt/docview/1095138770/abstract/13F2F16B9891B12671E/82?accountid=14576 [Google Scholar]
- Michie S., Johnston M., Francis J., Hardeman W., Eccles M. (2008). From Theory to Intervention: Mapping Theoretically Derived Behavioural Determinants to Behaviour Change Techniques. Applied Psychology, 57, 660–680. 10.1111/j.1464-0597.2008.00341.x [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G; PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ (Clinical research ed.), 339, b2535. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moy M., Weston N., Wilson E., Hess M., Richardson C. (2012). A pilot study of an Internet walking program and pedometer in COPD. Respiratory Medicine, 106, 1342–1350. http://dx.doi.org/10.1016/j.rmed.2012.06.013 [DOI] [PubMed] [Google Scholar]
- Naci H., Ionnidis J. P. (2013). Comparative effectiveness of exercise and drug interventions on mortality outcomes: Metaepidemiological study. British Medical Journal, 347, 1–14. 10.1136/bmj.f5577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan-Marx E. M., Mangione K. K., Ackerson T., Sidorov I., Maislin G., Volpe S. L., Craik R. (2011). Recruitment and retention strategies among older African American women enrolled in an exercise study at a PACE program. The Gerontologist, 51(suppl 1), S73–S81. 10.1093/geront/gnr001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor A. H., Cable N. T., Faulkner G., Hillsdon M., Narici M., Van Der Bij A. K. (2004). Physical activity and older adults: A review of health benefits and the effectiveness of interventions. Journal of Sports Sciences, 22, 703–725. 10.1080/02640410410001712421 [DOI] [PubMed] [Google Scholar]
- Tsai B.-M. (2008). Feasibility and effectiveness of e-therapy on fatigue management in home-based older adults with congestive heart failure (Ph.D.). Doctoral dissertation, State University of New York at Buffalo: . Retrieved June 28, 2014, from http://search.proquest.com.proxy.mul.missouri.edu/pqdt/docview/304369596/abstract/13F2F16B9891B12671E/600?accountid=14576# [Google Scholar]
- Tucker J. M., Welk G. J., Beyler N. K. (2011). Physical activity in U.S.: Adults compliance with the Physical Activity Guidelines for Americans. American Journal of Preventive Medicine, 40, 454–461. 10.1016/j.amepre.2010.12.016 [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C., Williams J. E., Reis J. P., Pluto D. (2002). Utility of pedometers for assessing physical activity: Convergent validity. Sports Medicine (Auckland, N.Z.), 32, 795–808. 10.2165/00007256-200232120-00004 [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C., Bassett D. R, (2004). How many steps/day are enough? Preliminary pedometer indices for public health. Sports Medicine, 34(1), 1–8. 10.2165/00007256-200434010-00001 [DOI] [PubMed] [Google Scholar]
- Valentine J. C. (2009). Judging the quality of primary research. In Cooper H. M., Hedges L. V., Valentine J. C. (Eds.), The Handbook of Research Synthesis and Meta-Analysis (2nd ed., pp. 122–146). Thousand Oaks, CA: Russell Sage Foundation. [Google Scholar]
- van der Bij A. K., Laurant M. G., Wensing M. (2002). Effectiveness of physical activity interventions for older adults: A review. American Journal of Preventive Medicine, 22, 120–133. 10.1016/S0749-3797(01)00413-5 [DOI] [PubMed] [Google Scholar]
- Van Poppel M. N. M., Chinapaw M. J. M., Mokkink L. B., Van Mechelen W., Terwee C. B. (2010). Physical activity questionnaires for adults: A systematic review of measurement properties. Sports Medicine (Auckland, N.Z.), 40, 565–600. 10.2165/11531930-000000000-00000 [DOI] [PubMed] [Google Scholar]
- Warren-Findlow J., Prohaska T. R., Freedman D. (2003). Challenges and opportunities in recruiting and retaining underrepresented populations into health promotion research. The Gerontologist, 43(suppl 1), 37–46. 10.1093/geront/43.suppl_1.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock R., Brooks G., Palmas W., Morin P., Teresi J., Eimicke J., Shea S. (2011). Lessened decline in physical activity and impairment of older adults with diabetes with telemedicine and pedometer use: Results from the IDEATel study. Age & Ageing, 40, 98–105. http://dx.doi.org/10.1093/ageing/afq147 [DOI] [PubMed] [Google Scholar]
- Wilson D. (2009). Systematic coding. In Cooper H. M., Hedges L. V., Valentine J. C. (Eds.), The Handbook of Research Synthesis and Meta-Analysis (2nd ed., pp. 159–176). Thousand Oaks, CA: Russell Sage Foundation. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.