Aggregate data of subspecialty graduates indicate an increasing interest in combining fellowship training in infectious diseases with critical care medicine. We explore some possible reasons for this trend and offer suggestions to encourage growth in this area of combined specialties.
Keywords: critical care, infectious disease, fellowship
Abstract
The recent rise in unfilled training positions among infectious diseases (ID) fellowship programs nationwide indicates that ID is declining as a career choice among internal medicine residency graduates. Supplementing ID training with training in critical care medicine (CCM) might be a way to regenerate interest in the specialty. Hands-on patient care and higher salaries are obvious attractions. High infection prevalence and antibiotic resistance in intensive care units, expanding immunosuppressed host populations, and public health crises such as the recent Ebola outbreak underscore the potential synergy of CCM-ID training. Most intensivists receive training in pulmonary medicine and only 1% of current board-certified intensivists are trained in ID. While still small, this cohort of CCM-ID certified physicians has continued to rise over the last 2 decades. ID and CCM program leadership nationwide must recognize these trends and the merits of the CCM-ID combination to facilitate creation of formal dual-training opportunities.
Critical care medicine (CCM) is the specialty focused on the diagnosis and management of life-threatening conditions. Intensive care units (ICUs) in the United States have historically been managed primarily by pulmonologists due to the major roles that respiratory disease and mechanical ventilation have during critical illness. However, anesthesiologists, surgeons, emergency medicine physicians, neurologists, hospitalists, and other internists comprise a growing proportion of practitioners providing intensive care today, mirroring the increasing complexity of the critically ill patient population and the diverse set of diseases that mandate ICU care. Multidisciplinary ICU care has the potential to benefit patients through access to physicians with different skill sets, and may also offer additional options for clinical practice and higher career satisfaction for physicians.
Infection maintains a conspicuous presence in ICUs worldwide. In a point prevalence study, 51% of the 13 796 patients in 1265 ICUs across 75 countries were considered infected, and 71% were receiving antibiotics [1]. The diagnosis and treatment of these infections is becoming an increasingly complicated task for the intensivist, given the alarming milieu of “bad bugs, no drugs” [2], an aging and more immunocompromised patient population, a wider array of sophisticated but complex diagnostic modalities, and a constant race against the clock for administration of appropriate antibiotics in potentially septic patients [3]. Formal training of the intensivist in ID has strong potential for synergy in patient care, clinical and epidemiologic research, and the design and execution of control strategies for pandemics and biological warfare.
In this article, we focus on historical and recent trends in CCM and ID in the United States with an emphasis on the rise in dual trained CCM-ID specialists, and discuss the merits as well as logistical issues of combined CCM-ID training. Our goal is to heighten awareness of this promising combination specialty among trainees and underscore the need for academic programs that offer formal pathways for training in CCM-ID.
THE GROWING DEMAND FOR INTENSIVISTS
The concept of CCM can trace its roots to the successful use of mechanical ventilation during the polio epidemic in Copenhagen in 1952 [4]. The concept of an ICU quickly spread around the world, due to the increase in number of mechanically ventilated patients and the higher efficiency in care achieved by placing these patients in close proximity to each other. Since the late 1960's, most US hospitals have maintained at least 1 ICU. The use of critical care services in the United States has expanded dramatically over the past several decades, outpacing the growth of most other areas of healthcare [5]. The increase in critical care services has been paralleled by a recognition that ICU patients should be cared for by physicians with special training and expertise. Within the American Board of Medical Specialties, 4 member boards (Internal Medicine, General Surgery, Pediatrics, and Anesthesiology) offer CCM certification. The American Board of Internal Medicine offered its first subspecialty exam for CCM in 1987 [6]. There is now a strong body of evidence to support the benefit of trained intensivists in caring for ICU patients, both in terms of improved patient outcomes and cost-effectiveness [7–9].
Today, the demand for intensivists continues to rise, bolstered by patient factors that include an aging and more medically complex population, as well as safety and regulatory factors such as the Leapfrog Group ICU staffing recommendations and Accreditation Council for Graduate Medical Education (ACGME) resident duty hour limitations. Many have raised concerns that these trends will lead to a relative shortage of intensivists in the near future. Indeed, the Committee on Manpower for the Pulmonary and Critical Care Societies study estimated that without an increase in the number of intensivists, there could be a 20% deficit in the supply of intensivists by 2020 [10]. As internal medicine (IM) remains the parent specialty for the majority of intensivists in this country, standardizing the training requirements for internists seeking CCM certification while allowing flexibility for dual training in other specialties has recently been the focus of a task force from the Critical Care Societies Collaborative [11].
CRITICAL CARE TRAINING PATHWAYS OFFERED THROUGH INTERNAL MEDICINE
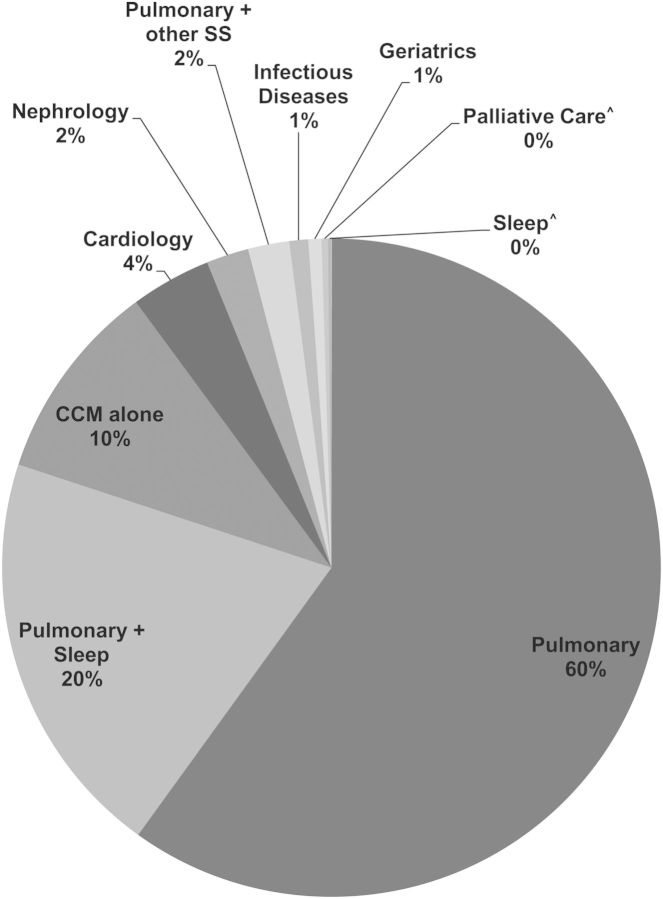
There are currently several pathways to CCM board eligibility through IM. CCM board eligibility can be obtained for physicians with IM training alone through a two-year fellowship; for IM physicians with training in another IM subspecialty, one year of CCM fellowship training is required. By far, the majority of training programs that lead to CCM board eligibility in the U.S. are the traditional three-year pulmonary/critical care medicine (PCCM) programs (see Figure 1 for the distribution of sub-specialties across new CCM graduates). For example, in 2012–2013, 138 PCCM fellowship programs comprised approximately 1500 positions with 500 graduates each year; in contrast, the 34 Internal Medicine-Critical Care Medicine (IM-CCM) programs currently have 200 positions with 100 graduates each year [12]. The IM-CCM programs are filled by a combination of trainees with background in IM alone, emergency medicine, and IM with another medical subspecialty (most commonly cardiology, nephrology, and infectious diseases).
Figure 1.
Distribution of American Board of Internal Medicine (ABIM) subspecialty (SS) certifications held by physicians newly certified in critical care medicine (CCM) (n=13 061*). *Counts represent 2014 point-prevalence estimates (courtesy ABIM); ˆSignificantly lower than one percentage.
INCREASING NUMBERS OF CCM-ID SPECIALISTS IN THE UNITED STATES
Today there are 113 physicians in the United States with active certifications in CCM and ID, where the second initial certification (referring to initial certification in ID if already CCM certified and vice versa) occurred in or after 1990. While they constitute only 1% of those who are CCM board certified, they represent 12% of the CCM certifications among those with non-pulmonary subspecialties (Figure 1). The American Board of Internal Medicine (ABIM) indicates that the number of such new second initial certifications over the following four 6-year periods was as follows: 7 in 1990–95, 22 in 1996–2001, 30 in 2002–07 and 54 in 2008–13. Although the absolute number of candidates with new second initial certifications remains small, this sustained increase over time suggests that growth in the CCM-ID graduate pool is likely to continue.
To achieve dual certification in CCM and ID, a minimum 2-year fellowship in ID and 1 year in CCM is required by the ACGME. Almost 90% of CCM-ID candidates have certified in CCM after ID training. The observed rise in CCM-ID graduates, despite a shortage of dedicated dual-training tracks, suggests that the majority of candidates are applying separately to fellowship programs for each subspecialty. It seems likely that the number of CCM-ID graduates could be even higher if this combined training pathway was as well known as PCCM and similarly obtained without the onerous task of reapplying for another fellowship during busy training years.
SYNERGY OF CCM-ID IN THE CLINICAL AND RESEARCH ARENAS
Expertise in ID is likely to benefit the practice of critical care given the prevalence of infectious conditions in the ICU and their impact on outcomes. More than half of ICU patients receive at least 1 antibiotic during their stay in the ICU [13], and it is well known that the presence of infection is a key determinant of adverse outcomes for critically ill patients [1]. In fact, overlooked nuances in presentation can greatly influence survival in sepsis, which is among the most common problems faced by an intensivist and is the leading cause of death in noncoronary ICUs [14]. Hospital-acquired infections, including ventilator-associated pneumonia, Clostridium difficile-associated diarrhea, urinary-tract infections, and catheter-related bloodstream infections, all occur at a much higher rate in the ICU than on the general wards [15]. The corollary that expertise in CCM is likely to benefit the practice of ID is also true; given that a large proportion of ID consults occur in ICU patients. In addition, as hospitals and medical systems update their preparations for large-scale highly contagious outbreaks, bioterrorism, and disaster management, hospital epidemiologists are often on the front line of making recommendations.
Furthermore, although the number of hospitalized patients with AIDS has declined, there is a growing number of other types of patients with compromised immune systems who require critical care services, many of them for complex infectious problems that involve unusual pathogens [16]. This “new age” immunocompromised population includes recipients of high-risk allogeneic hematopoietic stem cell and organ transplantation, myeloablative and cytotoxic chemotherapy, monoclonal antibodies, and other cellular and biological immunomodulating therapies. These patients may initially mask profound illness; require complicated antibiotic dosage adjustments in the setting of hypoalbuminemia, third spacing of fluid, organ failures, continuous renal replacement therapy; and need careful monitoring for severe drug-drug interactions and toxicities. The need for timely recognition and management of infection-related issues in this population has been recognized. In fact, at many centers of excellence for oncology and transplantation nationwide, the ID consultant is part of the rounding-team and offers input on each case. An ID-trained intensivist might be able to play a larger role in the ICUs at institutes like these.
No studies have explicitly examined the benefit of care from physicians dual-trained in ID and CCM, but there is strong evidence to support the benefit of ID consultation in critically ill patients with serious infections. For example, some studies have found that having an established ID consultation program in the ICU may help improve diagnosis of infection and administration of appropriate antibiotics, reduce duration of antibiotics, and improve patient outcomes such as ICU length of stay, resource utilization, and mortality [17, 18]. Recently, a much larger study using Medicare claims data found that after risk adjustment, ID intervention in patients with 11 serious but common infectious diagnoses, including septic shock, bacteremia, meningitis, and C. difficile, was associated with better outcomes and lower costs of care [19]. This study also found a significant reduction (by 3.7% fewer days) in ICU length of stay as well as 30-day hospital readmission rates, and that the benefit was highest when patients were seen by ID physicians earlier in their course. Another study found improved outcomes and healthcare costs associated with early ID consults in solid organ transplant patients admitted for infectious complications [20]. For patients with bacteremia, numerous studies have shown that ID consultation reduces morbidity and mortality as well as total cost of care, again demonstrating greatest benefit with consultation early in the course of illness [21–25].
One might argue that if ID consultative services are so readily available to intensivists, there is no need to pursue CCM-ID training. However, infection diagnosis, control, prophylaxis, and management are engrained in day-to-day ICU management, so that related questions that arise greatly exceed the average daily number of ID consultations in any given ICU. Moreover, ID consultative services are usually dependent on recognition of a problem that warrants their input by the primary providers. If the intensivist is trained in ID, missed opportunities for valuable ID input could be greatly avoided.
In addition to its clinical synergy, all of the topics discussed above are important areas for research and quality improvement. In particular, there is great interest in improving surveillance and prevention of healthcare-associated infections, especially in the current era where hospital-acquired infections are linked to reimbursement penalties. Sepsis is the target of much active research in terms of epidemiology, pathophysiology, prevention, and treatment. There is a growing recognition of the importance of antibiotic stewardship programs, particularly in the ICU where the rational use of antimicrobial agents is arguably most important [26]. The ICU has been on the frontline of emerging infectious diseases, (West Nile virus outbreak in 1999, the severe acute respiratory syndrome epidemic in 2003, the outbreak of the hypervirulent strain of C. difficile NAP1/027, the 2009 H1N1 influenza pandemic, and today's outbreak of Ebola virus disease), where often the first reports of disease biology and treatment are generated, and where research into the pathophysiology and host response to the infectious agent begin.
The recent Ebola virus disease (EVD) outbreak highlights some of the advantages of having dual trained specialists involved in both in the clinical and research arenas. Patients and healthcare workers (HCW) both benefitted from those with dual training as those specialists helped in preparing teams for the serious challenges patients with EVD present. This included preparing and training a multidisciplinary team in donning and doffing personal protective equipment (PPE), practicing invasive procedures that demand technical proficiency when dexterity is limited in full PPE, addressing the increased manpower demands of caring for a seriously ill patient with EVD, and preparing for disposal and decontamination of equipment while at the same time maximizing patient and HCW safety [27–30]. Teams of physicians from both specialties have also advanced potential research questions that might have been difficult without the participation of dual trained specialists [31].
Future pandemics will undoubtedly require expertise in both critical care and infectious diseases. While dual specialization in CCM and ID is clearly not a requirement to participate in research in any of these areas, the expertise afforded by clinical training in both fields offers unique insight into these important problems and supplies the critical thinking that is needed to formulate robust research questions in the field.
CREATING RENEWED ENTHUSIASM TO TRAIN IN ID
In recent years, ID has been declining in popularity as a specialty choice among IM residents. The 2015 fellowship match results released by the National Resident Matching Program revealed that ID and Nephrology were the only 2 subspecialties within IM that had a decline in the number of applicants [32]. The proportion of certified ID programs with unfilled positions has risen over the last 3 years from 34% in 2013 to 51% in 2015, with many programs unable to fill a single spot in the match. Interestingly, over the same period, 12.2% more programs have been certified to provide ID training despite the decline in match rate [32]. The problem is multifactorial: fewer graduates are pursuing IM, and within IM, many residents are more attracted to the procedure-oriented specialties like cardiology and gastroenterology that command higher salaries. Indeed, the salary of the average ID physician is lower than any other IM field (averaging $170 000 in 2012 compared to $185 000 for general internists and $240 000 for intensivists) [33], such that ID fellowship is essentially asking young physicians to spend more time in training for less money. This, coupled with the increasing educational debt burden of medical school graduates, may make ID as a career choice financially prohibitive.
Recognizing the declining interest among IM residents in pursuing ID training, Chandrasekar et al suggested initiatives to try to create more enthusiasm for the field, which included promotion of CCM-ID and Geriatrics-ID as combined fellowships [34]. Combining CCM and ID training could make ID more appealing overall by improving the average salary of the ID physician, increasing the diversity of practice through more procedures and “hands-on” patient care, and fostering more opportunities in research and quality improvement, while simultaneously easing the growing demand for intensivists nationwide. Whether these suggestions are incorporated into recommendations from the Task Force on ID Recruitment (recently convened by the Infectious Diseases Society of America) remains to be seen [35].
ADVANCING THE CONCEPT OF DUAL TRAINING
Given the clear synergy of CCM-ID, the growing interest among trainees, and the potential benefit to patients and hospitals, we should be considering ways to advance this promising dual specialty. We believe there are four major areas that are critical to this process. First, the creation of additional fellowship programs with a combined track in both specialties is essential. Currently, as discussed, interested IM residents may be discouraged by the need to apply to 2 separate fellowships. In addition, combining it into one streamlined program could shorten training by 1 year, especially for trainees interested in a clinical track. Second, a multidisciplinary approach among intensivist groups managing ICUs worldwide should be encouraged. This is particularly important because a lack of available jobs would stymie the field even if more CCM-ID fellows were trained. Third, the ID community should consider additional training in CCM as synergistic and recognize the importance of fostering interest in ICU and hospital-based infectious diseases. For comparison, there are approximately 50 000 new diagnoses of human immunodeficiency virus and 15 000 deaths in patients with AIDS per year in the United States [36], compared to an estimated 1 000 000 or more cases of sepsis per year and more than 200 000 sepsis-related deaths [37]. The ID community is as strong a stakeholder in the field of sepsis as intensivists and emergency physicians, and CCM-ID physicians have long been leaders in this field [3, 38, 39]. And lastly, there needs to be more funding for the important research topics that overlap CCM and ID, both from the government and from hospitals that stand to benefit from new knowledge in these areas.
POTENTIAL LIMITATIONS FROM COMBINING CCM AND ID
There may be some limitations to training in CCM-ID. The ICU is demanding, and the attention of intensivists is constantly required for many different tasks throughout their shift. This environment is less conducive to dedicating large amounts of time and attention by the primary provider to a single complex clinical ID related question, something that a separate ID consultant would likely be more inclined to do. Depending on the departmental framework, it is conceivable that ID divisions may lose revenue to CCM or pulmonary divisions if and when CCM-ID specialists manage patients with complex infections in the ICU that would have otherwise been consulted on by their ID counterparts. Finally, the job market is not flooded with customized offers for CCM-ID graduates yet. Consequently, dual-trained graduates in both community and academic settings have often had to steer their practice toward one of the 2 specialties. Universal formalization of the dual training process and heightened awareness among program and hospital leadership of the potential importance of CCM-ID could mitigate this problem considerably.
CONCLUSIONS
Critical care medicine has expanded beyond its humble origins in primarily managing respiratory failure with mechanical ventilation. Today, the complexity of ICU patients is greater than ever, and infections play a major role in precipitating critical illness leading to ICU admission, complicating the ICU course, and causing death. Despite a conspicuous dearth in training programs offering dual training in CCM and ID, there has been a sharp rise in new CCM-ID graduates over the last 2 decades, independent of the growth in overall ID graduates. Given the strong potential for synergy in clinical care and research, this combined subspecialty will likely continue to grow in the future, and provisions to foster this interest must be encouraged.
Notes
Acknowledgments. We thank the American Board of Internal Medicine for providing aggregate board certification data. We thank Kelly Byrne for assistance with formatting of the manuscript text and figure and thank Drs Anthony Suffredini and Robert Danner for reviewing the manuscript.
Financial support. This work was supported by intramural National Institutes of Health (NIH) funds.
Disclaimer. The work by the authors was done as part of US government–funded research; however, the opinions expressed are not necessarily those of the NIH or other participating institutions.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Vincent JL, Rello J, Marshall J, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA 2009; 302:2323–9. [DOI] [PubMed] [Google Scholar]
- 2.Boucher HW, Talbot GH, Bradley JS, et al. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis 2009; 48:1–12. [DOI] [PubMed] [Google Scholar]
- 3.Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006; 34:1589–96. [DOI] [PubMed] [Google Scholar]
- 4.Ibsen B. The anaesthetist's viewpoint on the treatment of respiratory complications in poliomyelitis during the epidemic in Copenhagen, 1952. Proc R Soc Med 1954; 47:72–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halpern NA, Pastores SM. Critical care medicine in the United States 2000–2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med 2010; 38:65–71. [DOI] [PubMed] [Google Scholar]
- 6.Tobin MJ. Pulmonary and critical care medicine: a peculiarly American hybrid? Thorax 1999; 54:286–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim MM, Barnato AE, Angus DC, Fleisher LA, Kahn JM. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med 2010; 170:369–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA 2002; 288:2151–62. [DOI] [PubMed] [Google Scholar]
- 9.Pronovost PJ, Needham DM, Waters H, et al. Intensive care unit physician staffing: financial modeling of the Leapfrog standard. Crit Care Med 2006; 34:S18–24. [DOI] [PubMed] [Google Scholar]
- 10.Angus DC, Kelley MA, Schmitz RJ, et al. Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA 2000; 284:2762–70. [DOI] [PubMed] [Google Scholar]
- 11.Medicine CTFoCCEPiI. Training internists to meet critical care needs in the United States: a consensus statement from the Critical Care Societies Collaborative (CCSC). Crit Care Med 2014; 42:1272–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Accreditation Council for Graduate Medical Education Data Resource Book Academic Year 2012–2013. Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/PublicationsBooks/2012-2013_ACGME_DATABOOK_DOCUMENT_Final.pdf Accessed 22 August 2014.
- 13.Warren MM, Gibb AP, Walsh TS. Antibiotic prescription practice in an intensive care unit using twice-weekly collection of screening specimens: a prospective audit in a large UK teaching hospital. J Hosp Infect 2005; 59:90–5. [DOI] [PubMed] [Google Scholar]
- 14.Mayr FB, Yende S, Angus DC. Epidemiology of severe sepsis. Virulence 2014; 5:4–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alberti C, Brun-Buisson C, Burchardi H, et al. Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med 2002; 28:108–21. [DOI] [PubMed] [Google Scholar]
- 16.Linden PK. Approach to the immunocompromised host with infection in the intensive care unit. Infect Dis Clin North Am 2009; 23:535–56. [DOI] [PubMed] [Google Scholar]
- 17.Raineri E, Pan A, Mondello P, Acquarolo A, Candiani A, Crema L. Role of the infectious diseases specialist consultant on the appropriateness of antimicrobial therapy prescription in an intensive care unit. Am J Infect Control 2008; 36:283–90. [DOI] [PubMed] [Google Scholar]
- 18.Fox BC, Imrey PB, Voights MB, Norwood S. Infectious disease consultation and microbiologic surveillance for intensive care unit trauma patients: a pilot study. Clin Infect Dis 2001; 33:1981–9. [DOI] [PubMed] [Google Scholar]
- 19.Schmitt S, McQuillen DP, Nahass R, et al. Infectious diseases specialty intervention is associated with decreased mortality and lower healthcare costs. Clin Infect Dis 2014; 58:22–8. [DOI] [PubMed] [Google Scholar]
- 20.Hamandi B, Husain S, Humar A, Papadimitropoulos EA. Impact of infectious disease consultation on the clinical and economic outcomes of solid organ transplant recipients admitted for infectious complications. Clin Infect Dis 2014; 59:1074–82. [DOI] [PubMed] [Google Scholar]
- 21.Byl B, Clevenbergh P, Jacobs F, et al. Impact of infectious diseases specialists and microbiological data on the appropriateness of antimicrobial therapy for bacteremia. Clin Infect Dis 1999; 29:60–6; discussion 7–8. [DOI] [PubMed] [Google Scholar]
- 22.Forsblom E, Ruotsalainen E, Ollgren J, Jarvinen A. Telephone consultation cannot replace bedside infectious disease consultation in the management of Staphylococcus aureus bacteremia. Clin Infect Dis 2013; 56:527–35. [DOI] [PubMed] [Google Scholar]
- 23.Fowler VG, Jr, Sanders LL, Sexton DJ, et al. Outcome of Staphylococcus aureus bacteremia according to compliance with recommendations of infectious diseases specialists: experience with 244 patients. Clin Infect Dis 1998; 27:478–86. [DOI] [PubMed] [Google Scholar]
- 24.Nathwani D, Davey P, France AJ, Phillips G, Orange G, Parratt D. Impact of an infection consultation service for bacteraemia on clinical management and use of resources. QJM 1996; 89:789–97. [DOI] [PubMed] [Google Scholar]
- 25.Valentin T, Luketina RR, Hoenigl M, Zollner-Schwetz I, Krause R. Survival of patients with Staphylococcus aureus bacteremia. Clin Infect Dis 2014; 58:599–600. [DOI] [PubMed] [Google Scholar]
- 26.Kollef MH, Micek ST. Antimicrobial stewardship programs: mandatory for all ICUs. Crit Care 2012; 16:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Decker BK, Sevransky JE, Barrett K, Davey RT, Chertow DS. Preparing for critical care services to patients with Ebola. Ann Intern Med 2014; 161:831–2. [DOI] [PubMed] [Google Scholar]
- 28.Chertow DS, Kleine C, Edwards JK, Scaini R, Giuliani R, Sprecher A. Ebola virus disease in West Africa—clinical manifestations and management. N Engl J Med 2014; 371:2054–7. [DOI] [PubMed] [Google Scholar]
- 29.Torabi-Parizi P, Davey RT, Jr, Suffredini AF, Chertow DS. Ethical and practical considerations in providing critical care to patients with Ebola virus disease. Chest 2015; doi:10.1378/chest.15-0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johnson DW, Sullivan JN, Piquette CA, et al. Lessons learned: critical care management of patients with Ebola in the United States. Crit Care Med 2015; 43:1157–64. [DOI] [PubMed] [Google Scholar]
- 31.Chertow DS, Uyeki TM, DuPont HL. Loperamide therapy for voluminous diarrhea in Ebola virus disease. J Infect Dis 2015; 211:1036–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chandrasekar PH. Bad news to worse news: 2015 Infectious Diseases (ID) Fellowship Match Results. Clin Infect Dis 2015; 60:1438. [DOI] [PubMed] [Google Scholar]
- 33.Medscape. Medscape HIV/Infectious Disease Physician Compensation Report: 2012 Results. Available at: http://www.medscape.com/features/slideshow/compensation/2012/hiv Accessed 4 September 2014.
- 34.Chandrasekar P, Havlichek D, Johnson LB. Infectious diseases subspecialty: declining demand challenges and opportunities. Clin Infect Dis 2014; 59:1593–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Calderwood SB. IDSA response to factors contributing to the decline of medical residents choosing the field of infectious diseases. Clin Infect Dis 2015; 60:1724. [DOI] [PubMed] [Google Scholar]
- 36.CDC. HIV Surveillance Report. Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/reports/ Accessed 4 September 2014.
- 37.Martin GS. Sepsis, severe sepsis and septic shock: changes in incidence, pathogens and outcomes. Expert Rev Anti Infect Ther 2012; 10:701–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cross AS, Opal SM, Palardy JE, Bodmer MW, Sadoff JC. The efficacy of combination immunotherapy in experimental Pseudomonas sepsis. J Infect Dis 1993; 167:112–8. [DOI] [PubMed] [Google Scholar]
- 39.Maki DG, Ringer M, Alvarado CJ. Prospective randomised trial of povidone-iodine, alcohol, and chlorhexidine for prevention of infection associated with central venous and arterial catheters. Lancet 1991; 338:339–43. [DOI] [PubMed] [Google Scholar]