Abstract
We present an unusual case of a 54-year-old Chinese lady presenting to the ears, nose and throat clinic after family members noticed that her hearing had progressively deteriorated over the preceding weeks. She also complained of tinnitus. Examination of the ears, nose and throat was unremarkable. Flexible nasoendoscopy demonstrated swelling in the postnasal space, which, following biopsy, was shown to be pathognomonic of tuberculosis. This was successfully treated with multidisciplinary input and the patient made a complete recovery.
Background
This case demonstrates the importance of thorough examination of the ears, nose and throat as a combined entity when considering pathology of the auditory system. Furthermore, it demonstrates that a patient's ethnicity must provide the clinician with a degree of suspicion, when confronted with abnormal clinical findings, towards an associated condition. In this case, we were primarily concerned that a patient of this ethnicity may have an underlying nasopharyngeal carcinoma. This case is a rare presentation of a treatable condition, which has presented atypically compared to textbook cases of tuberculosis (TB) in other systems of the body.
Case presentation
A 54-year-old Chinese woman is referred to ears, nose and throat clinic by her general practitioner, as her family was concerned that there has been a recent deterioration in her hearing. She is struggling with the content of conversations and she reports tinnitus bilaterally.
Further questioning reveals that she is normally quite fit and well. She denies any nasal symptoms, and only very occasionally feels wheezy. There has been no recent cough or dyspnoea. She denies any weight loss or night sweats.
Her last foreign travel was to Hong Kong in 2007. She previously immigrated to the UK from Hong Kong 40 years ago. There is no history of TB. Her medical history includes asthma, non-insulin-dependent diabetes mellitus and hyperlipidaemia. Her surgical history includes an appendicectomy, two caesarean sections and a bilateral salpingo-oophorectomy. She has no allergies, and is only on metformin and simvastatin.
She quit smoking 2 years prior to her initial presentation, and smoked very occasionally before quitting. Her alcohol intake is minimal. She has no pets, and works as a cook in a Chinese restaurant.
Ear examination and anterior rhinsocopy is unremarkable. Flexible nasendoscopy demonstrates a smooth swelling to the postnasal space. The rest of the pharynx and larynx is normal. Audiometry on arrival in clinic is normal. Tympanometry was not performed.
She was consented for a biopsy of the postnasal space, primarily because of concern regarding the possibility of a nasopharyngeal carcinoma.
Following results of the biopsy, the patient was referred to the respiratory team for further investigation and treatment.
Investigations
▸Postnasal space biopsy—caseating granulomatous change.
▸ Chest X-ray—normal.
▸ High-resolution CT thorax—normal.
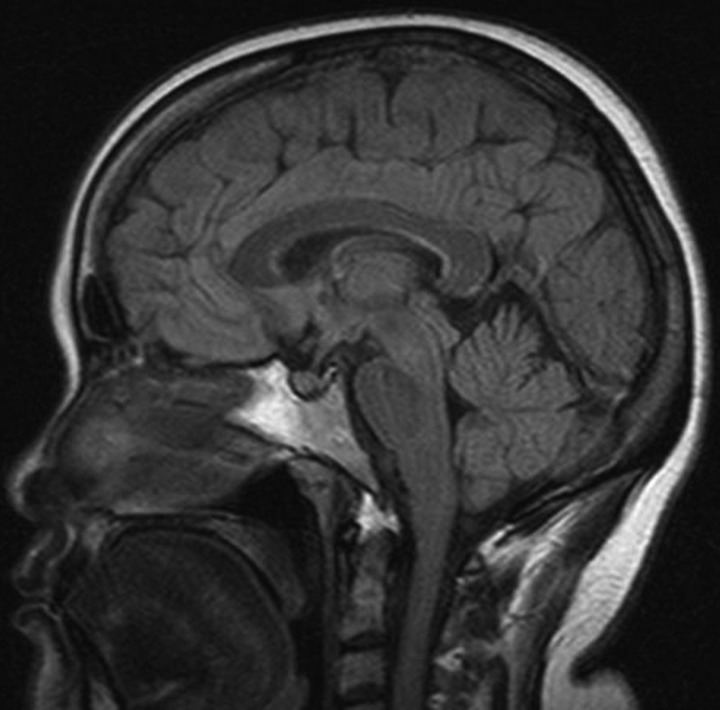
▸ MRI of the head was performed to rule out TB meningitis (figure 1).
Figure 1.
MRI head—sagittal FLAIR image demonstrating a small increase in soft tissue in the postnasal space region.
Differential diagnosis
▸ Nasopharygeal carcinoma
▸ Tuberculosis
▸ Sarcoidosis.
Treatment
Empirical treatment commenced for TB with 2 months of Rifater and Ethambutol, followed by 4 months of Rifinah.
Outcome and follow-up
Uneventful recovery after 6 months of first-line antituberculous therapy.
Discussion
Head and neck manifestations of TB are relatively common in the UK, particularly in at-risk groups. These include people of South Asian ethnicity, recent foreign travel to a high prevalence area, recent contact with an infectious person in a high-prevalence area, the immunocompromised person, those with TB in the past and a previous diagnosis of pleurisy. There is evidence to suggest that a deficiency of vitamin D may predispose to infection or reactivation of TB, due to its immunomodulatory role.1–4
Yielding TB from blood culture and fluid aspirate samples is notoriously arduous, as sensitivity is approximately 30%.5 TB also takes several weeks to grow to significant levels, and by this time, the patient's clinical condition may have changed. Alternative diagnoses may have been sought including lymphoma, as this may present with similar constitutional symptoms. Often treatment for TB has been commenced by this stage, but there may be issues regarding multidrug resistance which may not arise until several weeks of treatment have passed, and this is of particular concern in patients who have a history of foreign travel.
Biopsy is therefore the preferred method of investigation, particularly in the head and neck, where a histological diagnosis is available relatively quickly, and further investigations may help ascertain the extent of disease. It is important therefore to investigate the thorax for evidence of old or new TB. An MRI of the brain is useful to screen for intracranial TB. A lumbar puncture may then be used to confirm the presence of TB meningitis, as the treatment period is significantly longer; 12 months, compared to the traditional 6 months. Poor compliance and multidrug resistance may have catastrophic complications in TB meningitis.2 6–9
The most common presentation of TB in the head and neck is that of cervical lymphadenopathy, present in ∼90% of cases of head and neck TB. The upper respiratory tract and oral cavity are gateways for droplet-borne spread of TB.1 2 Therefore, head and neck TB is not uncommon, but its location within the head and neck may be difficult to ascertain. Patients with head and neck TB may present atypically, with a lack of constitutional symptoms such as weight loss, night sweats and respiratory symptoms. Symptoms may often be site specific, but occasionally may be a source of referred neurology.6–11
It is imperative that a thorough history includes information on travel, contact and immune status to identify at-risk individuals and plan investigation and management, after the patient is suitably risk stratified. This should be complemented with rigorous examination of the ears, nose and throat to identify a potential site of infection.
Nasopharyngeal TB is a difficult diagnosis to confirm on clinical suspicion alone. In current literature, there are 15 cases of nasopharyngeal TB, each presenting with a variety of symptoms. One case presented with diplopia, 5 with nasal symptoms and 12 had cervical masses or lymphadenopathy.
One retrospective study detailed 1315 cases of TB, of which 128 included the head and neck. In all, 87% presented with cervical lymphadenopathy, only 26% had constitutional symptoms and 20% had a co-existent site of TB.8
With particular relevance to our case, there are several interesting features which arise at various stages of presentation and investigation.
The patient's presenting complaints of tinnitus and apparent hearing loss direct the clinician to a likely otological source of disease. In the absence of otological pathology, thorough examination of the nose and throat demonstrates a lesion in the nasopharynx. Given the ethnicity of the patient in question, there is concern about the increased risk of nasopharyngeal carcinoma, and a biopsy is therefore preferred to ascertain a histological diagnosis.
This demonstrates the presence of caseating granulomata, a finding pathognomonic of TB. Non-caseating granulomata would raise the possibility of sarcoidosis. Further investigation of the respiratory tract and the brain confirmed that the disease was well localised within the nasopharynx with no evidence of respiratory or intrathecal spread. This allowed for appropriate disease management in conjunction with the local respiratory physicians, and a shorter duration of treatment, than if this patient were complicated with TB meningitis.
Learning points.
Presentations of a vestibular or auditory nature should warrant thorough examination of the nose and throat to exclude referred sources of pain and therefore underlying disease. In this case, it was necessary to rule out the possibility of hearing loss being secondary to Eustachian tube orifice compromise, thus requiring inspection of the postnasal space.
A patient's ethnicity should always be placed in the context of their symptoms in order to risk stratify the likely differential diagnoses.
Imaging should be used as an adjunct to assess the extent of distant spread of the disease to assist in planning management.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Waldron J, Van Hasselt CA, Skinner DW, et al. Tuberculosis of the nasopharynx: clinicopathological features. Clin Otolaryngol Allied Sci 1992;17:57–9. [DOI] [PubMed] [Google Scholar]
- 2.Nalini B, Vinayak S. Tuberculosis in ear, nose, and throat practice: its presentation and diagnosis. Am J Otolaryngol 2006;27:39–45. [DOI] [PubMed] [Google Scholar]
- 3.Baeke F, Takiishi T, Korf H, et al. Vitamin D: modulator of the immune system. Curr Opin Pharmacol 2010;10:482–96. [DOI] [PubMed] [Google Scholar]
- 4.Jo EK. Innate immunity to mycobacteria: vitamin D and autophagy. Cell Microbiol 2010;12:1026–35. [DOI] [PubMed] [Google Scholar]
- 5.Berger HW, Mejra E. Tuberculous pleurisy. Chest 1973;63:88–92. [DOI] [PubMed] [Google Scholar]
- 6.Hale RG, Tucker DI. Head and neck manifestations of tuberculosis. Oral Maxillofac Surg Clin North Am 2008;20:635–42. Review. [DOI] [PubMed] [Google Scholar]
- 7.Wang WC, Chen JY, Chen YK, et al. Tuberculosis of the head and neck: a review of 20 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:381–6. [DOI] [PubMed] [Google Scholar]
- 8.Menon K, Bem C, Gouldesbrough D, et al. A clinical review of 128 cases of head and neck tuberculosis presenting over a 10-year period in Bradford, UK. J Laryngol Otol 2007;121:362–8. [DOI] [PubMed] [Google Scholar]
- 9.Tang LM, Chen ST, Chang HS. Tuberculous meningitis in patients with nasopharyngeal carcinoma. Scand J Infect Dis 1996;28:195–6. [DOI] [PubMed] [Google Scholar]
- 10.Sithinamsuwan P, Sakulsaengprapha A, Chinvarun Y. Nasopharyngeal tuberculosis: a case report presenting with diplopia. J Med Assoc Thai 2005;88:1442–6. [PubMed] [Google Scholar]
- 11.Al-Serhani AM, Al-Mazrou K. Pharyngeal tuberculosis. Am J Otolaryngol 2001;22:236–40. [DOI] [PubMed] [Google Scholar]